Abstract
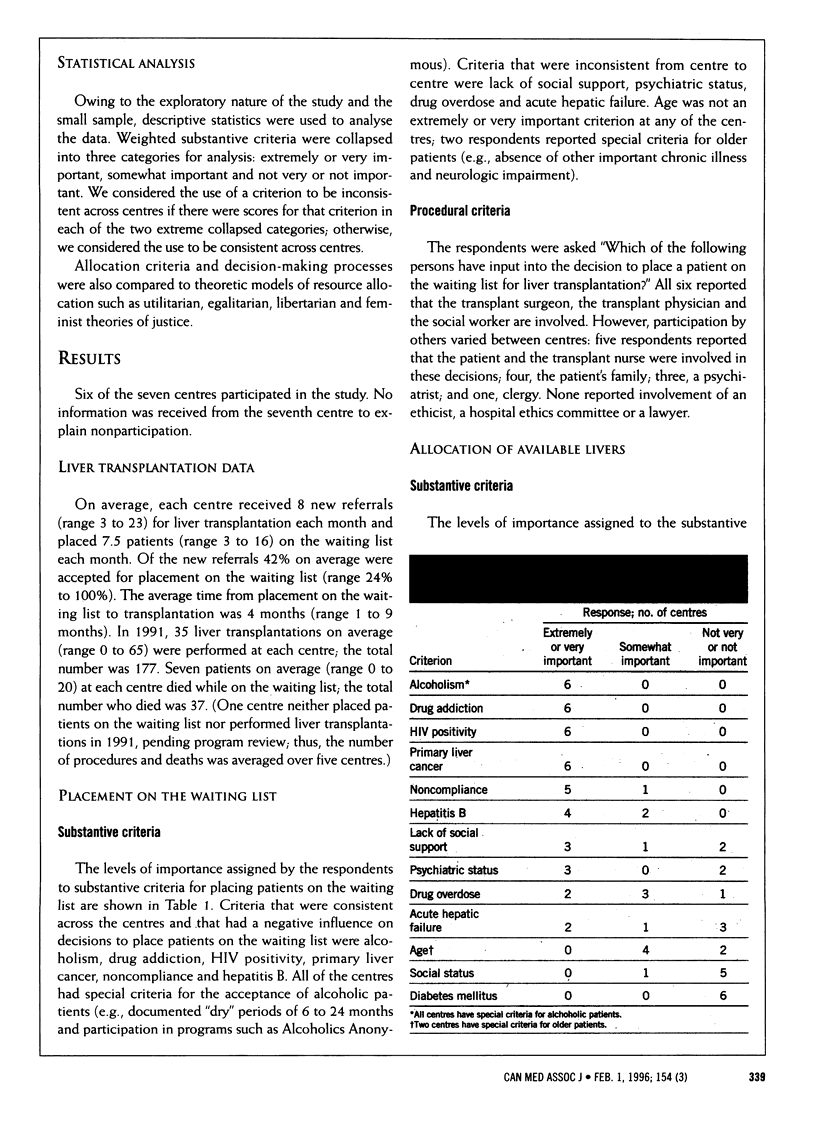
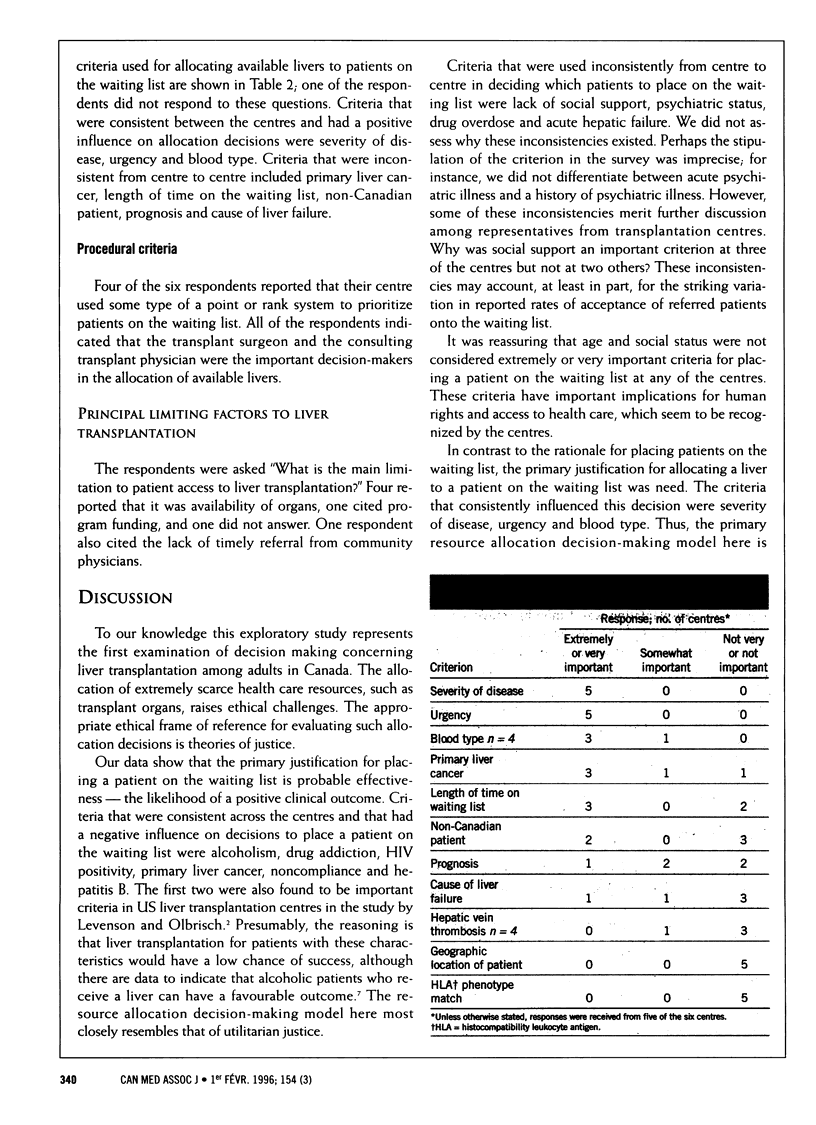
OBJECTIVES: To describe the substantive and procedural criteria used for placing patients on the waiting list for liver transplantation and for allocating available livers to patients on the waiting list; to identify principal decision-makers and the main factors limiting liver transplantation in Canada; and to examine how closely cadaveric liver allocation resembles theoretic models of source allocation. DESIGN: Mailed survey. PARTICIPANTS: Medical directors of all seven Canadian adult liver transplantation centres, or their designates. Six of the questionnaires were completed. OUTCOME MEASURES: Relative importance of substantive and procedural criteria used to place patients in the waiting list for liver transplantation and to allocate available livers. Identification of principal decision-makers and main limiting factors to adult liver transplantation. RESULTS: Alcoholism, drug addiction, HIV positivity, primary liver cancer, noncompliance and hepatitis B were the most important criteria that had a negative influence on decisions to place patients on the waiting list for liver transplantation. Severity of disease and urgency were the most important criteria used for selecting patients on the waiting list for transplantation. Criteria that were inconsistent across the centres included social support (for deciding who is placed on the waiting list) and length of time on the waiting list (for deciding who is selected from the list). Although a variety of people were reported as being involved in these decisions, virtually all were reported to be health to be health care professionals. Thirty-seven patients died while waiting for liver transplantation in 1991; the scarcity of cadaveric livers was the main limiting factor. CONCLUSIONS: Criteria for resource allocation decisions regarding liver transplantation are generally consistent among the centres across Canada, although some important inconsistencies remain. Because patients die while on the waiting list and because the primary limiting factor is organ supply, increased organ acquisition efforts are needed.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bird G. L., O'Grady J. G., Harvey F. A., Calne R. Y., Williams R. Liver transplantation in patients with alcoholic cirrhosis: selection criteria and rates of survival and relapse. BMJ. 1990 Jul 7;301(6742):15–17. doi: 10.1136/bmj.301.6742.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levenson J. L., Olbrisch M. E. Psychosocial evaluation of organ transplant candidates. A comparative survey of process, criteria, and outcomes in heart, liver, and kidney transplantation. Psychosomatics. 1993 Jul-Aug;34(4):314–323. doi: 10.1016/S0033-3182(93)71865-4. [DOI] [PubMed] [Google Scholar]
- Singer P. A. A review of public policies to procure and distribute kidneys for transplantation. Arch Intern Med. 1990 Mar;150(3):523–527. [PubMed] [Google Scholar]
- Spital A. The shortage of organs for transplantation. Where do we go from here? N Engl J Med. 1991 Oct 24;325(17):1243–1246. doi: 10.1056/NEJM199110243251710. [DOI] [PubMed] [Google Scholar]


