Abstract
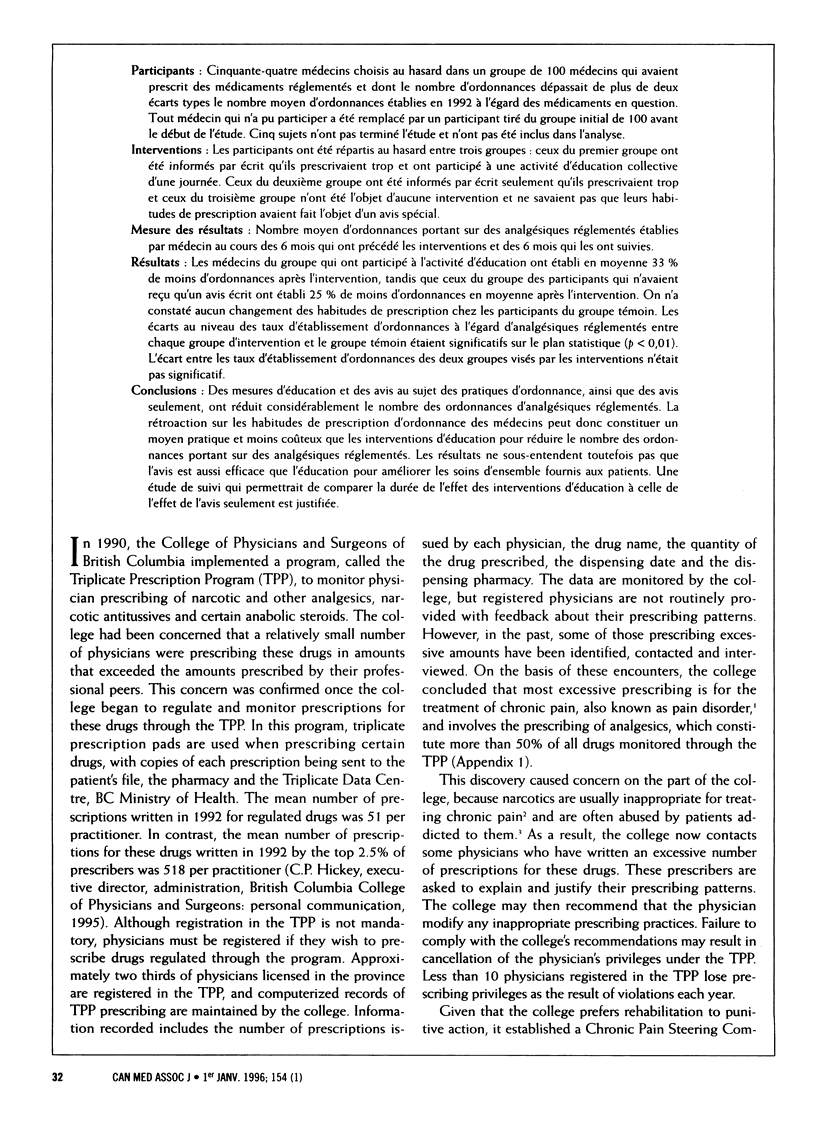
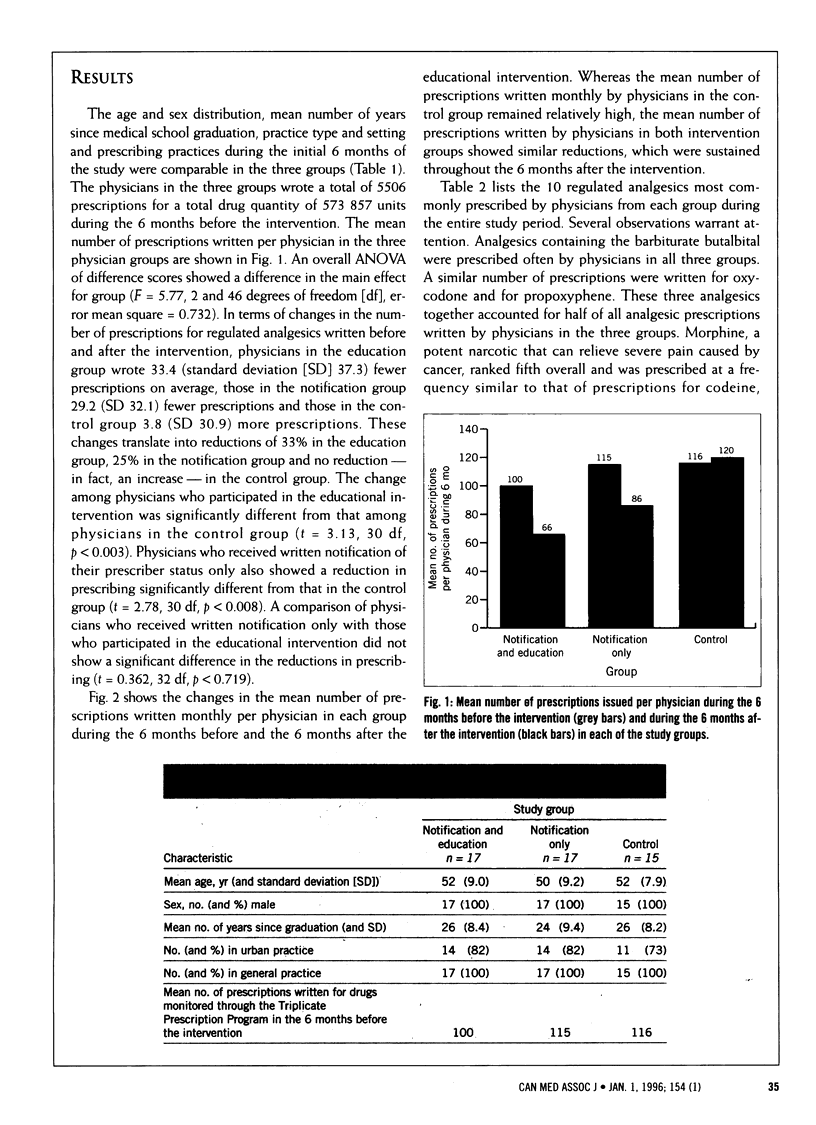
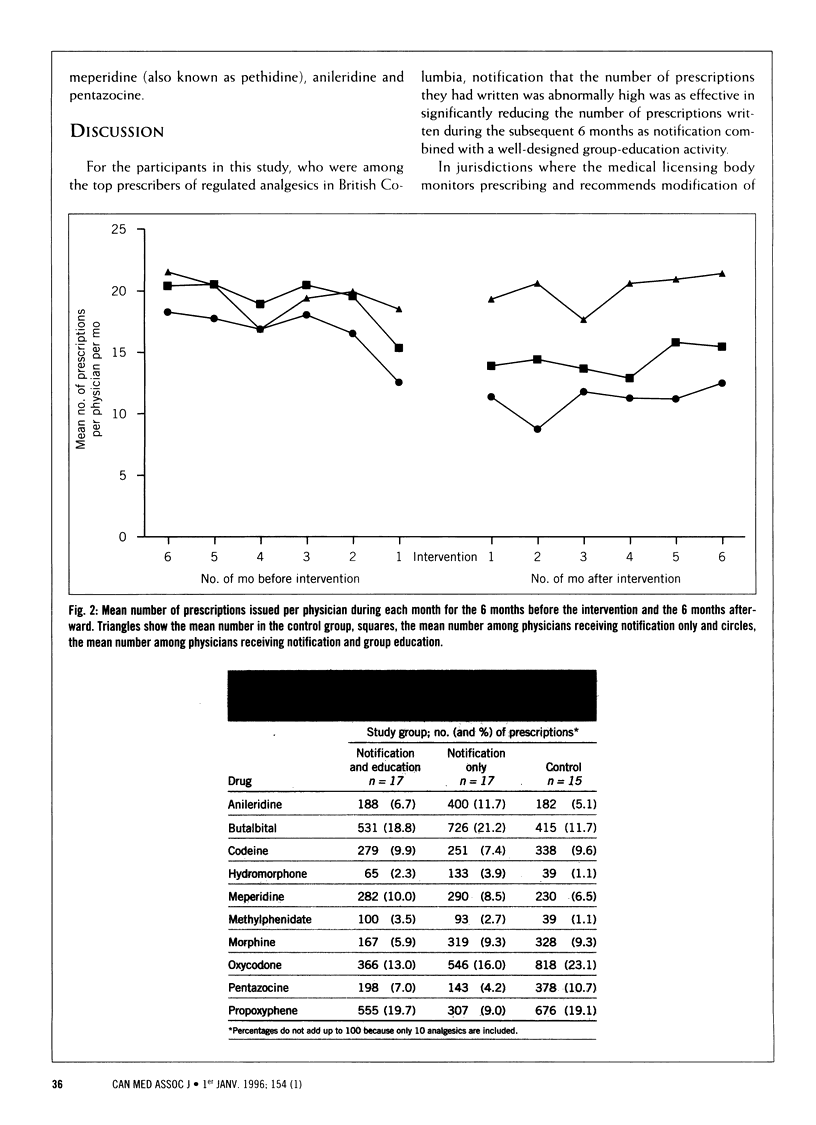
OBJECTIVE: To compare the effectiveness of group education and notification with that of notification alone in modifying prescribing of regulated analgesics. DESIGN: Randomized controlled trial conducted from Dec. 1, 1992, to Dec. 31, 1993. SETTING: Nonacademic primary care practices in British Columbia. PARTICIPANTS: Fifty-four physicians randomly selected from a group of 100 physicians who had written a number of prescriptions for regulated drugs more than than two standard deviations above the mean number of prescriptions written for such drugs in 1992. Any physician who was unable to participate was replaced from the original group of 100 before the study began. Five subjects did not complete the study and were not included in the analysis. INTERVENTIONS: Participants were randomly assigned to three groups: those in the first group received a written notification of excessive prescribing and attended a 1-day group-education activity, those in the second group received a written notification of excessive prescribing only and those in the third group were not subject to any intervention and were unaware that their prescribing had received special notice. OUTCOME MEASURE: Mean number of prescriptions for regulated analgesics issued per physician in the 6 months before and the 6 months after the interventions. RESULTS: Physicians in the group that attended the education intervention wrote, on average, 33% fewer prescriptions after the intervention, whereas physicians in the group that received only written notification wrote 25% fewer prescriptions, on average, after the intervention. No change in prescribing was shown in the control group. The differences in rates of prescribing of regulated analgesics between each intervention group and the control group were statistically significant (p < 0.01). The difference in the rate of prescribing between the two intervention groups was not significant. CONCLUSIONS: Group education and notification of prescriber status as well as notification alone significantly reduced prescribing of regulated analgesics. Hence, feedback on a physician's prescribing pattern may be a practical and less costly alternative to direct educational intervention in moderating the prescribing of regulated analgesics. The results do not, however, imply that notification is as effective as education in improving overall patient care. A follow-up study comparing the duration of the effect of the educational intervention with that of notification alone is warranted.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aronoff G. M., Wagner J. M., Spangler A. S., Jr Chemical interventions for pain. J Consult Clin Psychol. 1986 Dec;54(6):769–775. doi: 10.1037//0022-006x.54.6.769. [DOI] [PubMed] [Google Scholar]
- Avorn J., Soumerai S. B. Improving drug-therapy decisions through educational outreach. A randomized controlled trial of academically based "detailing". N Engl J Med. 1983 Jun 16;308(24):1457–1463. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- Bingle G. J., O'Connor T. P., Evans W. O., Detamore S. The effect of 'detailing' on physicians' prescribing behavior for postsurgical narcotic analgesia. Pain. 1991 May;45(2):171–173. doi: 10.1016/0304-3959(91)90185-Z. [DOI] [PubMed] [Google Scholar]
- Davis D. A., Thomson M. A., Oxman A. D., Haynes R. B. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. JAMA. 1992 Sep 2;268(9):1111–1117. [PubMed] [Google Scholar]
- Everitt D. E., Soumerai S. B., Avorn J., Klapholz H., Wessels M. Changing surgical antimicrobial prophylaxis practices through education targeted at senior department leaders. Infect Control Hosp Epidemiol. 1990 Nov;11(11):578–583. doi: 10.1086/646098. [DOI] [PubMed] [Google Scholar]
- Gehlbach S. H., Wilkinson W. E., Hammond W. E., Clapp N. E., Finn A. L., Taylor W. J., Rodell M. S. Improving drug prescribing in a primary care practice. Med Care. 1984 Mar;22(3):193–201. doi: 10.1097/00005650-198403000-00002. [DOI] [PubMed] [Google Scholar]
- Gottlieb H., Alperson B. L., Schwartz A. H., Beck C., Kee S. Self-management for medication reduction in chronic low back pain. Arch Phys Med Rehabil. 1988 Jun;69(6):442–448. [PubMed] [Google Scholar]
- Grimm R. H., Jr, Shimoni K., Harlan W. R., Jr, Estes E. H., Jr Evaluation of patient-care protocol use by various providers. N Engl J Med. 1975 Mar 6;292(10):507–511. doi: 10.1056/NEJM197503062921005. [DOI] [PubMed] [Google Scholar]
- Inui T. S., Yourtee E. L., Williamson J. W. Improved outcomes in hypertension after physician tutorials. A controlled trial. Ann Intern Med. 1976 Jun;84(6):646–651. doi: 10.7326/0003-4819-84-6-646. [DOI] [PubMed] [Google Scholar]
- Ives T. J., Frey J. J., Furr S. J., Bentz E. J. Effect of an educational intervention on oral cephalosporin use in primary care. Arch Intern Med. 1987 Jan;147(1):44–47. [PubMed] [Google Scholar]
- Kroenke K., Pinholt E. M. Reducing polypharmacy in the elderly. A controlled trial of physician feedback. J Am Geriatr Soc. 1990 Jan;38(1):31–36. doi: 10.1111/j.1532-5415.1990.tb01593.x. [DOI] [PubMed] [Google Scholar]
- Long D. M. Will your prescribing habits cost your license? Md Med J. 1988 Feb;37(2):127–131. [PubMed] [Google Scholar]
- McConnell T. S., Cushing A. H., Bankhurst A. D., Healy J. L., McIlvenna P. A., Skipper B. J. Physician behavior modification using claims data: tetracycline for upper respiratory infection. West J Med. 1982 Nov;137(5):448–450. [PMC free article] [PubMed] [Google Scholar]
- McPhee J. A., Wilgosh C. P., Roy P. D., Miller D. M., Knox M. G. Effect of pharmacy-conducted education on prescribing of postoperative narcotics. Am J Hosp Pharm. 1991 Jul;48(7):1484–1487. [PubMed] [Google Scholar]
- Meyer T. J., Van Kooten D., Marsh S., Prochazka A. V. Reduction of polypharmacy by feedback to clinicians. J Gen Intern Med. 1991 Mar-Apr;6(2):133–136. doi: 10.1007/BF02598309. [DOI] [PubMed] [Google Scholar]
- Pozen M. W., Gloger H. The impact on house officers of educational and administrative interventions in an outpatient department. Soc Sci Med. 1976 Sep-Oct;10(9-10):491–495. doi: 10.1016/0037-7856(76)90117-7. [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., DiClemente C. C., Norcross J. C. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992 Sep;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Ray W. A., Schaffner W., Federspiel C. F. Persistence of improvement in antibiotic prescribing in office practice. JAMA. 1985 Mar 22;253(12):1774–1776. [PubMed] [Google Scholar]
- Reuler J. B., Girard D. E., Nardone D. A. The chronic pain syndrome: misconceptions and management. Ann Intern Med. 1980 Oct;93(4):588–596. doi: 10.7326/0003-4819-93-4-588. [DOI] [PubMed] [Google Scholar]
- Schaffner W., Ray W. A., Federspiel C. F., Miller W. O. Improving antibiotic prescribing in office practice. A controlled trial of three educational methods. JAMA. 1983 Oct 7;250(13):1728–1732. [PubMed] [Google Scholar]
- Soumerai S. B., Avorn J. Principles of educational outreach ('academic detailing') to improve clinical decision making. JAMA. 1990 Jan 26;263(4):549–556. [PubMed] [Google Scholar]
- Soumerai S. B., Lipton H. L. Computer-based drug-utilization review--risk, benefit, or boondoggle? N Engl J Med. 1995 Jun 15;332(24):1641–1645. doi: 10.1056/NEJM199506153322411. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., McLaughlin T. J., Avorn J. Improving drug prescribing in primary care: a critical analysis of the experimental literature. Milbank Q. 1989;67(2):268–317. [PubMed] [Google Scholar]
- Spengler D. M. Chronic low back pain. The team approach. Clin Orthop Relat Res. 1983 Oct;(179):71–76. [PubMed] [Google Scholar]
- Tennant F. S., Jr Drug abuse in the US Army, Europe. JAMA. 1972 Sep 4;221(10):1146–1149. [PubMed] [Google Scholar]



