Abstract
In most primary or continuous cell cultures infected with the Q-fever agent Coxiella burnetii, bacteria are typically sheltered in phagolysosome-like, large replicative vacuoles (LRVs). We recently reported that only a small proportion of mouse peritoneal macrophages (PMΦ) infected with a nonvirulent, phase II strain of C. burnetii developed LRVs and that their relative bacterial load increased only slowly. In the majority of infected PMΦ, the bacteria were confined to the small vesicles. We show here that nitric oxide (NO) induced by the bacteria partially accounts for the restricted development of LRVs in primary macrophages. Thus, (i) PMΦ and bone marrow-derived macrophages (BMMΦ) challenged with phase II C. burnetii produced significant amounts of NO; (ii) the NO synthase inhibitors aminoguanidine and N-methyl-l-arginine reduced the production of NO and increased the frequency of LRVs (although the relative bacterial loads of individual LRVs did not change, the estimated loads per well increased appreciably); (iii) gamma interferon (IFN-γ) or the NO donor sodium nitroprusside, added to BMMΦ prior to or after infection, reduced the development and the relative bacterial loads of LRVs and lowered the yield of viable bacteria recovered from the cultures; and (iv) these effects of IFN-γ may not be entirely dependent on the production of NO since IFN-γ also controlled the infection in macrophages from inducible NO synthase knockout mice. It remains to be determined whether NO reduced the development of LRVs by acting directly on the bacteria; by acting on the traffic, fusion, or fission of cell vesicles; or by a combination of these mechanisms.
The gram-negative, obligate intracellular bacterium Coxiella burnetii, a member of the γ-subdivision of proteobacteria, is the agent of Q fever in humans; this zoonosis has nearly worldwide distribution (4, 5, 14, 22, 32, 34, 41). Two phases of the bacterium have been described: the highly virulent, phase I organisms, which are found in infected hosts and insect vectors, and the phase II organisms, which are less virulent or devoid of virulence for mammalian hosts and are obtained by multiple passages through chicken embryos. Phase II preparations may not be free of phase I bacteria, possibly accounting for the reversions described (4, 5, 32; T. Hackstadt, Letter, Trends Microbiol. 4:341-342, 1996). Once internalized by permissive host cells, the bacteria are found in small phagosomes that shelter a few organisms and fuse with each other and with other endocytic or phagocytic vesicles; thus, after 2 or more days, most infected cells display one or more phagoylysosome-like large replicative vacuoles (LRVs) that may ultimately contain hundreds of closely packed bacteria (5, 22, 24, 33, 43, 44). Mature C. burnetii phase II LRVs are fusigenic, acidified, and (acidic) hydrolase-rich and stain for LAMPs, CD43, Rab7, and autophagic markers (2, 3, 4, 5, 6, 21, 22, 31, 36). When placed under rather harsh culture conditions, cells infected with C. burnetii can release, noncytolytically, infective bacteria into the medium (33, 37); it is not clear, however, that such release takes place under normal cell culture conditions during log-phase growth of the intracellular bacteria.
These features describe the infection with phase I or phase II C. burnetii of primary or continuous cultures of fibroblasts and epithelial, macrophage-like, or other cell types from different animal species (2, 3, 4, 5, 24, 31, 39, 43). The infection of primary macrophages, however, may depend on the animal species and strain and on the phase of the bacterium, although comparative in vitro infection assays from the same laboratory may not always be available. Thus, resident peritoneal macrophages from guinea pigs and hamsters are reported to be quite susceptible to infection with phases I and II of C. burnetii and to develop bacterium-rich large vacuoles (23, 28, 29), whereas human and mouse primary macrophages may be less permissive (16, 44). Recently, the involvement of cytokines in the control of the infection of human monocytes/macrophages by C. burnetii has been extensively examined in attempts to explain the microbicidal defects that underlie the development of chronic human infection with C. burnetii (11, 12, 16).
We recently reported that, whereas essentially all mouse peritoneal resident macrophages (PMΦ) can be infected with C. burnetii phase II, few cells develop typical LRVs; in addition, the relative bacterial loads in these vacuoles, assessed by fluorescence measurements of DAPI (4′,6′-diamidino-2-phenylindole)-stained cells, increased at a much slower rate than in mouse fibroblasts or J774 macrophage-like cells (44). We show here that small concentrations of NO, induced by C. burnetii phase II bacteria, directly or indirectly, control the formation of LRVs in mouse primary macrophages but not, apparently, the bacterial load within individual LRVs. However, higher concentrations of NO induced by gamma interferon (IFN-γ) or generated with sodium nitroprusside (SNP) can affect both the formation of LRVs and the bacterial multiplication.
MATERIALS AND METHODS
Mice.
Female BALB/c 7- to 9-week-old mice were provided by the institutional animal facility (CEDEME). C57BL/6 inducible nitric oxide synthase knockout (iNOS KO) and wild-type (WT) mice were used; the control mice were kindly provided by Elaine Rodrigues (UNIFESP).
Cell culture.
Resident macrophages (PMΦ) were collected from peritoneal washouts of mice killed by neck fracture. Cells (1.5 × 105), attached to 13-mm-diameter glass coverslips, were placed in 2-cm2 wells of 24-well tissue culture plates and kept in 0.5 ml of antibiotic-free Dulbecco modified essential medium containing 15 mM HEPES, 2 g of sodium bicarbonate/liter, 1 mM l-glutamine, and 5% (vol/vol) fetal bovine serum. Experiments were started 24 h after preparation of the PMΦ cultures.
Bone marrow-derived macrophages (BMMΦ) were generated from bone marrow stem cells cultured on 10-cm-diameter “bacteriological” plastic plates for 7 days in RPMI 1640 medium containing 15 mM of HEPES, 2 g of sodium bicarbonate/liter, and 1 mM l-glutamine and supplemented with 20% fetal bovine serum and 30% L929 cell conditioned medium (LCCM). Differentiated BMMΦ were removed from the substrate by vigorous pipetting of ice-cold phosphate-buffered saline. Cells were counted, added (1.5 × 105) to glass coverslips inserted in 24-well tissue culture plates, and cultured in RPMI supplemented with 10% fetal bovine serum and 5% LCCM. All cultures were kept at 36°C in a 5% CO2 in air atmosphere.
Bacterial preparation and infection of host cells.
Clone 4 phase II Nine Mile strain of C. burnetii bacteria, which are infective for cells but not for mammals, were provided by Ted Hackstadt (Rocky Mountain Laboratories, National Institute of Allergy and Infectious Disease, National Institutes of Health, Hamilton, Mont.) and handled in a biosafety level II facility (Hackstadt, letter). Infective inocula were obtained as described previously (43) from confluent Vero cells infected with C. burnetii for 7 days. Prior to infection, suspensions containing ∼109 infective bacteria per ml were mildly sonicated at 35 kHz for 15 min at room temperature to disrupt the aggregates. Macrophage cultures were infected with ca. 100 infective organisms per cell. After 24 h, infected cultures were vigorously washed with Hanks balanced salt solution, and the appropriate fresh medium was added.
Host cell treatments.
Unless otherwise stated, the products added to the cultures were from Sigma Chemical Co., St. Louis, Mo. NO synthesis was inhibited with 1 mM aminoguanidine hemisulfate salt (AG) or with 100 μM N G-methyl-l-arginine (NMMA). Exogenous NO was generated by adding different concentrations of SNP. Macrophages were activated with 50 ng of mouse recombinant IFN-γ (R&D Systems, Minneapolis, Minn.)/ml. The agents were added to the culture medium and kept in it until the end of the experiments.
Nitrite determination.
The concentration of nitrite (NO2−), the stable oxidized derivative of NO (25) was determined in 100-μl aliquots of cell culture supernatants transferred to 96-well plates. Then, 100 μl of Griess reagent solution (1% sulfanilamide, 0.1% naphthylene diamine dihydrochloride, 2% H3PO4) was added per well, and the absorbances were measured at 540 nm in a microplate enzyme-linked immunosorbent assay reader. Sodium nitrite diluted in culture medium was used as standard.
Cell fixation, staining, determination of the percentage of cells with LRVs, and direct counts of bacteria.
At different times after infection, cultures were fixed for 1 h in 3.5% formaldehyde containing 7.5% sucrose, stained for 15 min with 3.5 μM DAPI, washed, and mounted in 50% glycerol (vol/vol). About 500 cells in each of triplicate coverslips were scored with a ×40 objective in an inverted microscope for the presence or absence of large C. burnetii vacuoles. LRVs were defined as those with a diameter at least equal to that of the cell nucleus (∼100 μm2). Bacteria in cells devoid of LRVs were directly counted in cultures stained with DAPI (ca. 100 cells per time point) by using an epifluorescence microscopy equipped with a PlanApo ×100/NA 1.4 oil objective.
Confocal microscopy, image acquisition, and determination of relative C. burnetii load.
Images of fixed and DAPI-stained cells were acquired in a Bio-Rad 1024UV confocal system attached to a Zeiss Axiovert 100 microscope equipped with a ×40 water immersion objective NA 1.2 plan-apochromatic lens and with differential interference contrast. LaserSharp 1024 version 2.1A from Bio-Rad was used for image acquisition, and MetaMorph (Universal Imaging Corporation) version 3.5 was used for image processing. Polygons were drawn onto digitized images of infected cells, and the relative fluorescence intensity of DAPI-stained bacteria within the circumscribed areas was determined. Under the measurement conditions used, the fluorescence intensity within each polygon is assumed to be proportional to the bacterial load in the region measured as previously described (43). Between 60 and 90 vacuoles were measured in each of triplicate coverslips.
Bacterial viability.
According to the method used previously results were presented in terms of focus-forming units (FFU) (12, 24). Infected macrophages were lysed in H2O, a step that did not reduce the bacterial infectivity; lysates were sonicated, diluted, and used to infect monolayers of Vero cells, previously irradiated (1,000 rads) to block cell multiplication. Irradiated Vero cells were transferred to glass coverslips inserted in the wells of 24-well tissue culture plates and then cultured in minimal essential medium supplemented with 5% of fetal bovine serum at 37°C in a 5% CO2 atmosphere. At 4 days after infection, Vero cells were washed with PBS, fixed, and stained with DAPI as described above. An epifluorescence microscope equipped with a ×40 objective was used to score the percentage of infected cells. Dilutions chosen for counting contained ca. 10 to 80% infected cells. About 500 cells were scored per coverslip.
Statistical analysis.
Each experiment was performed with triplicate sets of wells. All tabulated or illustrated values are the averages of the triplicates from one representative experiment from at least three made. Significance of the differences between means were evaluated by either Student t test or analysis of variance, both of which were provided by the Microsoft Excel 97 statistics package. Differences were taken as statistically significant when P was <0.05 (indicated by an asterisk in the figures) or when P was <0.01 (indicated by two asterisks).
RESULTS
C. burnetii LRVs develop more frequently and contain higher bacterial loads in BMMΦ than in PMΦ.
In agreement with our previous results, only a small proportion of resident PMΦ infected with C. burnetii developed bacterium-containing typically LRVs; the remaining cells displayed a variable number of small vesicles, each enclosing a few bacteria (44). The numbers of bacteria in BMMΦ that did not develop LRVs directly counted by epifluorescence microscopy remained relatively constant between days 1 and 6 of infection. The average numbers of bacteria ± the standard errors per cell (n = ∼100 cells) were as follows: 51 ± 5 (1 day), 34 ± 3 (2 days), 47 ± 7 (4 days), and 38 ± 6 (6 days). The data suggest that the C. burnetii did not appreciably multiply in cells that did not contain LRVs and point to the importance of the vacuoles as sites of bacterial replication.
In the experiment illustrated in Fig. 1A, the proportion of cells with LRVs reached a maximum of 11% on day 6 of infection, whereas in infected BMMΦ it was significantly higher (∼19%). In this and other experiments, the maximum frequency of the LRVs in both cell types was attained by 6 days of infection.
FIG. 1.
Contrasting features of C. burnetii phase II infection of mouse PMΦ and BMMΦ. Parallel cultures of macrophages were infected for 24 h with C. burnetii phase II; at different times, the cultures were fixed and processed as described in Materials and Methods. (A) Percentage of cells with LRVs as a function of the duration of infection. Symbols: •, PMΦ; ○, BMMΦ. (B) Relative bacterial load in LRVs on days 4 and 6 after infection. Bars: □, PMΦ; ▪, BMMΦ. Data represent the mean ± the standard deviation of one representative experiment out of five with similar results. Asterisks indicate statistically significant differences between PMΦ and BMMΦ (✽, P < 0.05; ✽✽, P < 0.01). (C and D) Superimposed confocal images of DAPI fluorescence (black) and Nomarski differential interference contrast (gray) of a representative PMΦ (C) and BMMΦ (D). The arrow points to large vacuole. N, cell nuclei. Bar, 10 μm.
The relative bacterial loads in LRVs of PMΦ and BMMΦ, as assessed by fluorescence measurements, increased from days 4 to 6 (Fig. 1B). The loads attained were, however, severalfold higher in BMMΦ than in PMΦ, suggesting that the former are more permissive to the infection (Fig. 1B to D). The higher permissiveness to infection of BMMΦ has been reported for other organisms (9, 10, 19, 30).
NO is induced by C. burnetii phase II bacteria in control and IFN-γ-treated macrophages.
We next examined the net production of NO by uninfected or infected PMΦ or BMMΦ that were either treated or not treated with IFN-γ (Table 1). It can be seen that (i) in the absence of added bacteria or IFN-γ, PMΦ but not BMMΦ produced significant amounts of NO over 24 h; (ii) treatment with IFN-γ increased the production of NO by uninfected PMΦ but not by BMMΦ; (iii) in the absence of added IFN-γ, the bacteria induced net NO production in both macrophages, although PMΦ released ∼3-fold more NO than BMMΦ; and (iv) PMΦ and BMMΦ treated with both IFN-γ and bacteria produced high and statistically similar amounts of NO. Yoshiie et al. have reported that mouse lung macrophages produced NO when challenged with C. burnetii phase I (42).
TABLE 1.
Effect of IFN-γ on the production of NO by control or by C. burnetii phase II-infected BMMφ or PMφ
| Host cell | Production of NO (μM nitrite/105 macrophages/24 h ± sd)
|
|||
|---|---|---|---|---|
| Uninfected
|
Infecteda
|
|||
| No addition | With IFN-γ | No addition | With IFN-γ | |
| BMMφ | 0 | 0 | 1.8 ± 0.08 | 12.3 ± 0.20 |
| PMφ | 1.6 ± 0.04 | 4.1 ± 0.41 | 6.6 ± 0.20 | 16.9 ± 0.40 |
Macrophages were infected with C. burnetii for 24 h, and nitrite was measured in the culture supernatants. NO production was inferred from the nitrite content of culture supernatants. Cells were exposed to IFN-γ or to control medium for the duration of the infection.
Inhibitors of NO synthase increase the frequency of LRVs but not their relative bacterial loads.
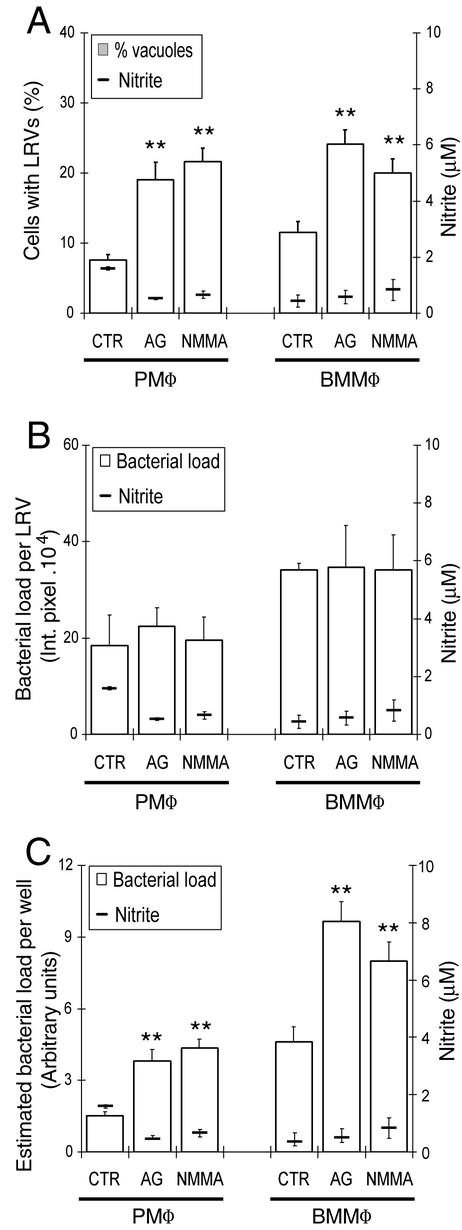
To assess the relationship of NO production to the infection pattern, we next examined the effect of NO synthase inhibitors AG or NMMA on the infection of PMΦ and BMMΦ. Figure 2A shows that the proportion of cells that developed large C. burnetii vacuoles increased in the cultures treated with the inhibitors, suggesting that NO induced by the bacteria controls the formation of LRVs. Within the sensitivity of the method, the bacterial loads in individual LRVs of cells treated with either AG or NMMA were not statistically different from those of untreated cells, suggesting that the small amounts of NO induced by the bacteria preferentially control vacuolar development rather than the relative bacterial loads in the LRVs (Fig. 2B). However, because cells with LRVs contain more bacteria than those without, the total bacterial loads in cultures treated with the synthase inhibitors were higher than in the untreated controls (Fig. 2C).
FIG. 2.
Effect of AG or NMMA on the infection of PMΦ or BMMΦ by C. burnetii phase II bacteria. Cultures were infected for 24 h, washed, and kept in AG- or NMMA-containing medium for the 6 days of the infection. (A) Percentage of cells with LRVs and nitrite production by control and AG- or NMMA-treated PMΦ and BMMΦ cultures. (B) Average of the relative bacterial load per LRV. (C) Fluorimetrically estimated total bacterial load per well in the same exper-iment shown in panels A and B. For clarity, the same nitrite data are shown in panels A, B, and C. Means ± the standard deviations of one representative experiment from three with similar results. Asterisks indicate that differences between control (CTR) and treated cultures (AG or NMMA) were statistically significant (P < 0.01).
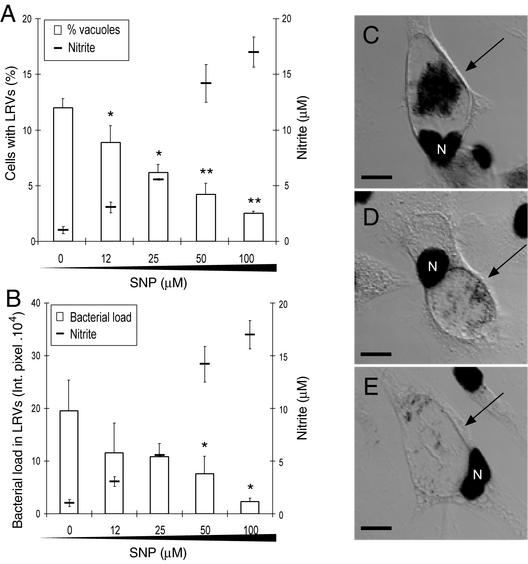
SNP added at the time of infection reduces the development of and the relative bacterial loads of LRVs.
To examine the effect of exogenous NO on the infection, SNP, an NO-generating compound, was added to BMMΦ cultures, together with the bacteria. Figure 3A and B show that the development of LRVs and their bacterial loads were both reduced by SNP in a concentration-dependent fashion. The variability associated with the measurements of rather low vacuolar fluorescence did not allow us to estimate the concentrations of SNP that could inhibit the development of LRV without affecting the bacterial loads. Confocal images of representative LRVs illustrate the markedly reduced bacterial loads in the few remaining vacuoles from cells treated with 50 or 100 μM SNP compared to an untreated control (Fig. 3C, D, and E).
FIG. 3.
Effect of SNP on the frequency of LRVs and their bacterial load in C. burnetii phase II-infected BMMΦ. SNP was added to the cultures at the time of infection and was kept in the medium until the end of experiment (6 days). The percentages of cells with LRVs (A) and the relative bacterial loads in the LRVs (B) are shown, together with the production of nitrite, as a function of the SNP concentration. The same nitrite data are shown in panels A and B as the means ± the standard deviations of one representative experiment from three with similar results. Significant differences between untreated control and treated cultures are indicated (✽, P < 0.05; ✽✽, P < 0.01). (C to E) Confocal superimposed images of DAPI fluorescence (black) and Nomarski differential interference contrast (gray). Images of representative cells illustrate the difference in bacterial loads inside the large vacuoles (arrow) of cells that were either left untreated (C) or were treated with 50 μM (D) or 100 μM (E) SNP. N, cell nuclei. Bar, 10 μm.
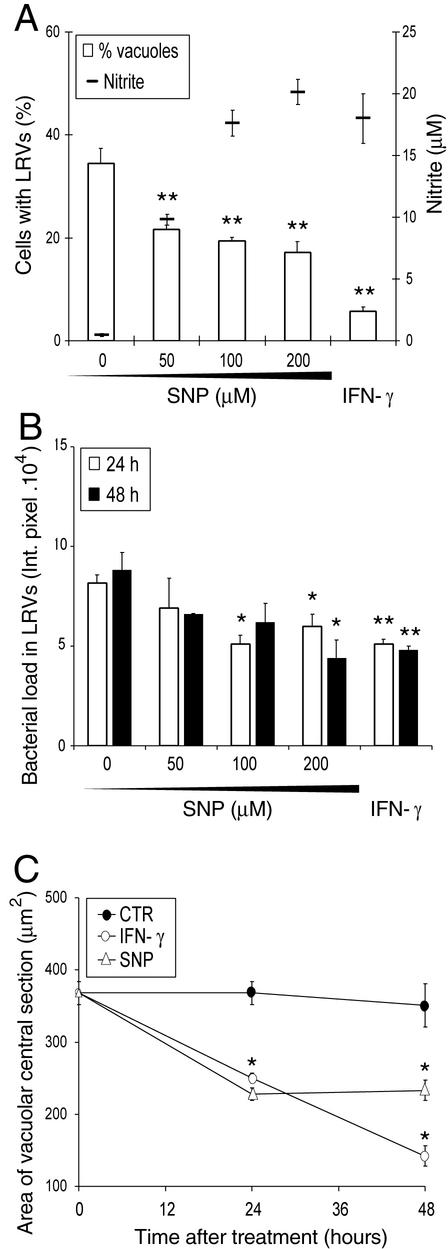
SNP or IFN-γ added to infected cultures reduce the frequency, relative bacterial loads, and sizes of the LRVs.
In this experiment BMMΦ infected for 4 days were treated for 24 or 48 h with different SNP concentrations or with a single concentration of IFN-γ. In the experiment shown, the percentages of cells with LRVs (Fig. 4A), the relative bacterial loads (Fig. 4B), and the sizes of the LRVs (Fig. 4C), estimated in the same preparations, were all significantly reduced by SNP or IFN-γ compared to the untreated controls. The shape of the concentration dependence curves suggests that the effects of SNP on the vacuoles are asymptotic. Furthermore, at low concentrations, SNP appeared to reduce the proportion of cells with LRVs to a larger extent than their relative bacterial loads. It may be of interest that IFN-γ was more active in reducing the percent of cells with LRVs than were the higher SNP concentrations, although the NO produced by the two treatments was similar (Fig. 4A). The implication seems to be that an additional NO independent mechanisms underlies the effects of IFN-γ on the infection.
FIG. 4.
Effect of SNP or IFN-γ on established infection of BMMΦ. At 4 days after C. burnetii infection, cultures were treated with SNP or IFN-γ. After 24 or 48 h, supernatants were removed for nitrite determination, and cells were processed as described in Materials and Methods. (A) Percentage of cells with LRVs and nitrite in culturesupernatants as a function of SNP concentration or IFN-γ treatment for 48 h. (B) Relative bacterial loads in LRVs of macrophages treated with SNP or IFN-γ for 24 (gray bars) or 48 h (black bars). (C) Vacuolar central optical section areas in cells treated with 100 μM SNP (▵), 50 ng of IFN-γ/ml (○), or controls (•) as a function of time. Results are expressed as the means ± standard deviations of one of two experiments. Significant differences between untreated control and treated cultures are indicated (✽, P < 0.05; ✽✽, P < 0.01)
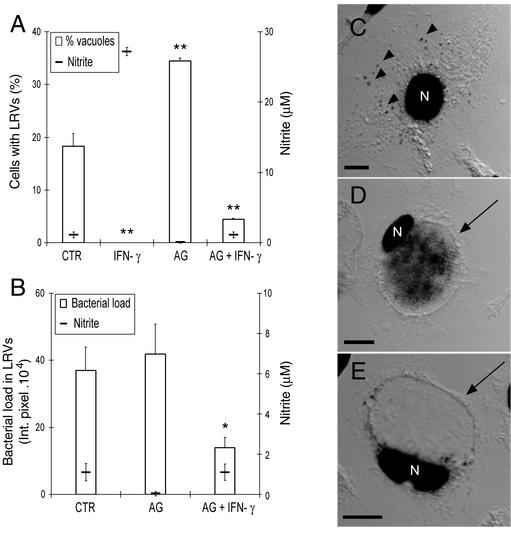
Induction of NO does not entirely account for the effects of IFN-γ on the development of LRVs and their relative bacterial loads.
Since, as shown in Fig. 3 and 4, treatment of BMMΦ with SNP or IFN-γ exerted rather similar effects on infection, it was of interest to determine the role of NO in the control of the size and bacterial load of LRVs in IFN-γ-treated cells. In the experiment shown in Fig. 5, BMMΦ were infected in the presence of AG or IFN-γ alone or both of them combined. Cultures infected in the presence of IFN-γ produced high amounts of NO and did not develop LRVs containing the bacteria (Fig. 5A); however, although LRVs did not develop, intracellular bacteria were not eliminated, since in nearly all of the cells DAPI-stained organisms were consistently found within small vacuoles dispersed throughout the cytoplasm (Fig. 5C).
FIG. 5.
Effect of IFN-γ, AG, or both on the infection of BMMΦ with C. burnetii phase II. IFN-γ, AG, or both were added to the cultures, together with the bacteria, for 24 h. At that time cells were washed and kept in fresh drug-containing medium. At 6 days after infection, supernatants were collected for nitrite determination and cells processed as described in Materials and Methods. (A) Percentage of cells with LRVs and nitrite concentration in the same cultures. (B) Relative bacterial load in LRVs and the same nitrite concentration data shown in panel A on a different scale. Results are presented as the mean ± the standard deviation of one representative experiment from three experiments with similar results. Statistically significant differences between untreated control (CTR) and treated cultures are indicated (✽, P < 0.05; ✽✽, P < 0.01). (C to E) Confocal superimposed images of DAPI fluorescence (black) and Nomarski differential interference contrast (gray). The images show cells from cultures treated with IFN-γ (C), AG (D), or AG plus IFN-γ (E). The arrowheads indicate C. burnetii dispersed through the cytoplasm; the arrows indicate the large vacuole. N, cell nucleus. Bar, 10 μm.
As shown in Fig. 2, addition of AG alone blocked the production of NO and increased the frequency of LRVs. In contrast, although they did not produce significant amounts of NO, macrophages infected in the presence of both IFN-γ and AG, developed few LRVs, with a significantly reduced bacterial load in comparison to untreated or AG-treated cells (Fig. 5A, B, D, and E).
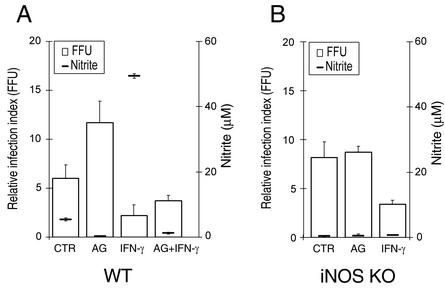
IFN-γ controls infection in BMMΦ from iNOS KO mice.
Since small amounts of NO were still being produced when the cultures were treated with IFN-γ plus AG (Fig. 5A and B), we performed an experiment with BMMΦ from iNOS KO mice and WT control mice. Cultures were infected in the presence of IFN-γ or AG either singly or in combination. At 6 days after infection, supernatants were collected for measurement of nitrite content, macrophages were lysed and lysate dilutions were plated on irradiated Vero cell monolayers to estimate bacterial viability (i.e., with regard to the FFU). As expected, WT macrophages treated with IFN-γ produced relatively large amounts of NO and reduced C. burnetii viability (Fig. 6A). Compared to untreated cells, treatment with AG alone increased the overall load of viable bacteria in WT macrophages. As expected, small amounts of NO were produced by WT cultures treated with IFN-γ plus AG, even though C. burnetii viability did not statistically differ from that of cultures treated with IFN-γ alone (P = 0.09) and was clearly reduced compared to untreated cells (Fig. 6A). In contrast to the WT macrophages, the treatment of iNOS KO macrophages with AG did not alter bacterial viability compared to untreated cultures (Fig. 6B). However, the addition of IFN-γ to iNOS KO cultures clearly reduced the bacterial viability in a situation where NO production was undetectable (Fig. 6B). Overall, these results indicate that the control of C. burnetii infection of macrophages by IFN-γ involves effector molecules other than NO.
FIG. 6.
Effect of IFN-γ, AG, or both, on C. burnetii viability in BMMΦ. IFN-γ, AG, or both were added to the cultures, together with the bacteria, for 24 h. At that time the cells were washed and kept in fresh drug-containing medium. At 6 days after infection, supernatants were collected for nitrite determination and the bacterial viability was determined as described in Materials and Methods. (A) Macrophages obtained from WT mice; (B) macrophages obtained from iNOS KO mice. The results are given as the relative infection index (FFU) as the means ± the standard errors of one representative experiment from two with similar results.
DISCUSSION
This report presents evidence that NO produced by mouse primary macrophages infected with phase II C. burnetii inhibits the development of LRVs typically found in other cell types. The main evidence for the control of LRVs by NO is the finding that the rather-specific NO synthase inhibitors AG or NMMA significantly increased the proportion of cells with LRVs (Fig. 2A). The effects were more striking in PMΦ, which, in the controls, displayed fewer LRVs and produced higher quantities of NO than BMMΦ (Fig. 1A and 2A and Table 1). However, although the relative bacterial load in individual LRVs in both macrophages was not significantly increased by the inhibitors (Fig. 2B), the total bacterial loads in the cultures treated by the inhibitors were increased (Fig. 2C). This is accounted for by the fact that the bacterial loads within LRVs appeared to be much greater and more difficult to count visually with any accuracy than those of infected cells devoid of LRV.
Oxygen reduction products may not be important in the control of C. burnetii phase II infection by untreated or IFN-γ-treated mouse primary macrophages. Our own experiments involving measurements of H2O2 or the addition of superoxide dismutase and/or catalase to infected cultures provided no support for a role for oxygen reduction products in the development and the relative bacterial loads of LRVs in untreated or IFN-γ-treated BMMΦ (data not shown). It has also been shown that isolated C. burnetii bacteria express superoxide dismutase and catalase activity (1, 20) and that IFN-γ-treated monocytes from patients with chronic granulomatous disease were able to kill C. burnetii phase I (12).
Because NO induced by the bacterium restricted the formation of LRVs without affecting the relative bacterial loads per cell, we chose to treat infected cultures with the NO generator SNP; we also treated infected or uninfected macrophages with IFN-γ, a cytokine which, among its other effects, is well known to increase the production of NO. When either SNP or IFN-γ were added with the bacteria and kept in the medium throughout, they reduced both the frequency and the relative bacterial loads of LRVs (Fig. 3A and B). However, the intracellular concentrations and the kinetics of NO generated in the normal course of infection may have differed from those in SNP- or IFN-γ-treated cells. Furthermore, since the IFN-γ effect was not fully reversed by synthase inhibitors (Fig. 5) and IFN-γ treatment reduced bacterial viability in iNOS KO macrophages (Fig. 6), mechanisms other than those involving NO may be operating in the control of C. burnetii infection by IFN-γ (15, 18, 19, 35).
The finding that NO produced by primary macrophages inhibited the development of C. burnetii-containing LRV raises two questions that should be considered in further studies. The first has to do with the mechanisms by which the bacteria trigger the production of NO by the macrophages; the second, with the mechanisms by which NO inhibits the development of LRVs in the host cells.
Induction of NO may reflect the recognition by macrophages of molecular patterns expressed on the surface of C. burnetii; the bacterial ligand could conceivably be a lipopolysaccharide known to be compositionally defective in phase II compared to (virulent) phase I organisms (22, 41; Hackstadt, letter). Such molecules might be recognized by CD14, scavenger, Toll-like, or other receptors (7, 11, 17, 26, 40). The production of NO by macrophages may be also induced or modulated by cytokines such as tumor necrosis factor alpha, IFN-α/β, or interleukin-10, of which the first and last are known to be produced by human or mouse macrophages infected with C. burnetii (12, 16, 39). It should be of interest to compare the production of NO and the development of LRVs in primary macrophages infected with phase I and phase II bacteria.
The NO triggered by the bacteria could affect vacuolar development by one or two non-mutually exclusive mechanisms: (i) NO could directly or indirectly target mechanisms of vesicle traffic, fusion, or fission and/or (ii) it could act on the bacteria inhibiting the production or the activity of putative secreted factors responsible for the development and features of the LRVs (37, 38). With regard to the first hypothesis, recent studies have shown that numerous macrophage genes can be directly or indirectly activated or repressed by NO induced by live or dead M. tuberculosis or inert particles, in control or IFN-γ-treated BMMΦ (8, 13). However, we are not aware of any evidence that NO can modulate vesicle fusion in situ or in cell-free fractions. The finding that the development of Leishmania amazonensis parasitophorous vacuoles in mouse primary macrophages was not affected by treatment with AG, SNP, or IFN-γ (D. Z. and C. Barbieri, unpublished results) is at least compatible with the hypothesis that the effect of NO on LRVs formation is primarily mediated by an effect on C. burnetii. Recently, Howe et al. (24) reported that NO inhibits C. burnetii phase II multiplication and LRV formation in L929 fibroblasts. Since L929 cells were described as highly permissive to C. burnetii (44), the results may also suggest that NO acts primarily on the bacteria.
There has been accrued interest in the mechanisms of the innate and acquired microbicidal activity of macrophages and other cells toward a variety of intracellular pathogens (7, 17, 26, 27, 40). The findings reported here indicate that alongside with its microbistatic or microbicidal activity, NO may directly or indirectly control the development of LRVs, which as in other models, are likely to provide an optimal environment for the replication of intracellular pathogens.
Acknowledgments
We thank Elaine Rodrigues for providing iNOS KO mice and CEDEME-UNIFESP for providing the other animals. The technical assistance of Regina A. de Paula is gratefully acknowledged.
This work was supported by FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo [Brazil]). D.S.Z. was supported by a doctoral fellowship from FAPESP (99/10742-5).
Editor: S. H. E. Kaufmann
REFERENCES
- 1.Akporiaye, E. T., and O. G. Baca. 1983. Superoxide anion production and superoxide dismutase and catalase activities in Coxiella burnetii. J. Bacteriol. 154:520-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akporiaye, E. T., J. D. Rowatt., A. S. Aragon, and O. G. Baca. 1983. Lysosomal response of a murine macrophage-like line persistently infected with Coxiella burnetii. Infect. Immun. 40:1152-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baca, O. G., E. T. Akporiaye, A. S. Aragon, I. L. Martinez, M. V. Robles, and N. L. Warner. 1981. Fate of phase I and phase II Coxiella burnetii in several macrophage-like tumor cell lines. Infect. Immun. 33:258-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baca, O. G., and D. Paretsky. 1983. Q fever and Coxiella burnetii: a model for host-parasite interactions. Microbiol. Rev. 46:127-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baca, O. G., Y. P. Li, and H. Kumar. 1994. Survival of the Q fever agent Coxiella burnetii in the phagolysosome. Trends Microbiol. 2:476-480. [DOI] [PubMed] [Google Scholar]
- 6.Beron, W., M. Gutierrez, M. Rabinovitch, and M. I. Colombo. 2002. Coxiella burnetii phase II localizes in a Rab7-labeled compartment with autophagic characteristics. Infect. Immun. 70:5816-5821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beutler, B. 2002. Toll-like receptors: how they work and what they do. Curr. Opin. Hematol. 8:2-10. [DOI] [PubMed] [Google Scholar]
- 8.Bogdan, C. 2001. Nitric oxide and the regulation of gene expression. Trends Cell Biol. 11:66-75. [DOI] [PubMed] [Google Scholar]
- 9.Bradbury, M. G., and C. Moreno. 1993. Effect of lipoarabinomannan and mycobacteria on tumor necrosis factor production by different populations of murine macrophages. Clin. Exp. Immunol. 94:57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buchmeier, N. A., and F. Heffron. 1989. Intracellular survival of wild-type Salmonella typhimurium and macrophage-sensitive mutants in diverse populations of macrophages. Infect. Immun. 57:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Capo, C., F. P. Lindberg, S. Meconi, Y. Zaffran, G. Tardei, E. J. Brown, D. Raoult, and J. L. Mege. 1999. Subversion of monocyte functions by Coxiella burnetii: impairment of the cross-talk between αvβ3 integrin and CR3. J. Immunol. 163:6078-6085. [PubMed] [Google Scholar]
- 12.Dellacasagrande, J., C. Capo, D. Raoult, and J. L. Mege. 1999. IFN-γ-mediated control of Coxiella burnetii survival in monocytes: the role of cell apoptosis and TNF. J. Immunol. 162:2259-2265. [PubMed] [Google Scholar]
- 13.Ehrt, S., D. Schnappinger, S. Bekiranov, J. Drenkow, S. Shi, T. R. Gingeras, T. Gaasterland, G. Schoolnik, and C. Nathan. 2001. Reprogramming of the macrophage transcriptome in response to interferon-gamma and Mycobacterium tuberculosis: signaling roles of nitric oxide synthase-2 and phagocyte oxidase. J. Exp. Med. 194:1123-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Franz, D. R., P. B. Jahrling, A. M. Friedlander, D. J. McClain, D. L. Hoover, W. R. Bryne, J. A. Pavlin, G. W. Christopher, and E. M. Eitzen, Jr. 1997. Clinical recognition and management of patients exposed to biological warfare agents. JAMA 278:399-411. [DOI] [PubMed] [Google Scholar]
- 15.Gebran, S. J., Y. Yamamoto, C. Newton, T. W. Klein, and H. Friedman. 1994. Inhibition of Legionella pneumophila growth by gamma interferon in permissive A/J mouse macrophages: role of reactive oxygen species, nitric oxide, tryptophan, and iron(III). Infect. Immun. 62:3197-3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghigo, E., C. Capo, D. Raoult, and J. L. Mege. 2001. Interleukin-10 stimulates Coxiella burnetii replication in human monocytes through tumor necrosis factor downmodulation: role in microbicidal defect of Q fever. Infect. Immun. 69:2345-2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Girardin, S. E., P. J. Sansonetti, and D. J. Philpott. 2002. Intracellular versus extracellular recognition of pathogens: common concepts in mammals and flies. Trends Microbiol. 10:193-199. [DOI] [PubMed] [Google Scholar]
- 18.Halonen, S. K., G. A. Taylor, and L. M. Weiss. 2001. Gamma interferon-induced inhibition of Toxoplasma gondii in astrocytes is mediated by IGTP. Infect. Immun. 69:5573-5576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamrick, T. S., E. A. Havell, J. R. Horton, and P. E. Orndorff. 2000. Host and bacterial factors involved in the innate ability of mouse macrophages to eliminate internalized unopsonized Escherichia coli. Infect. Immun. 68:125-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heinzen, R. A., M. E. Frazier, and L. P. Mallavia. 1992. Coxiella burnetii superoxide dismutase gene: cloning, sequencing, and expression in Escherichia coli. Infect. Immun. 60:3814-3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heinzen, R. A., M. A. Scidmore, D. D. Rockey, and T. Hackstadt. 1996. Differential interaction with endocytic and exocytic pathways distinguish parasitophorous vacuoles of Coxiella burnetii and Chlamydia trachomatis. Infect. Immun. 64:796-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heinzen, R. A., T. Hackstadt, and J. E. Samuel. 1999. Developmental biology of Coxiella burnetii. Trends Microbiol. 7:149-154. [DOI] [PubMed] [Google Scholar]
- 23.Hinrichs, D. J., and T. R. Jerrells. 1976. In vitro evaluation of immunity to Coxiella burnetii. J. Immunol. 117:996-1003. [PubMed] [Google Scholar]
- 24.Howe, D., L. F. Barrows, N. M. Lindstrom, and R. A. Heinzen. 2002. Nitric oxide inhibits Coxiella burnetii replication and parasitophorous vacuole maturation. Infect. Immun. 70:5140-5147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ignarro, L. J., J. M. Fukuto, J. M. Griscavage, N. E. Rogers, and R. E. Byrns. 1993. Oxidation of nitric oxide in aqueous solution to nitrite but not nitrate: comparison with enzymatically formed nitric oxide from l-arginine. Proc. Natl. Acad. Sci. USA 90:8103-8107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janeway, C. A., Jr., and R. Medzhitov. 2002. Innate immune recognition. Annu. Rev. Immunol. 20:197-216. [DOI] [PubMed] [Google Scholar]
- 27.Kaiser, V., and G. Diamond. 2000. Expression of mammalian defensin genes. J. Leukoc. Biol. 68:779-784. [PubMed] [Google Scholar]
- 28.Kishimoto, R. A., and J. S. Walker. 1976. Interaction between Coxiella burnetii and guinea pig peritoneal macrophages. Infect. Immun. 14:416-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kishimoto, R. A., B. J. Veltri, P. G. Canonico, F. G. Shirey, and J. S. Walker. 1976. Electron microscopic study on the interaction between normal guinea pig peritoneal macrophages and Coxiella burnetii. Infect. Immun. 14:1087-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leary, K., J. R. Connor, and P. S. Morahan. 1985. Comparison of herpes simplex virus type 1 DNA replication and virus production in murine bone marrow-derived and resident peritoneal macrophages. J. Gen. Virol. 66:1123-1129. [DOI] [PubMed] [Google Scholar]
- 31.Maurin, M., A. M. Benoliel, P. Bongrand, and D. Raoult. 1992. Phagolysosomes of Coxiella burnetii-infected cell lines maintain an acidic pH during persistent infection. Infect. Immun. 60:5013-5016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maurin, M., and D. Raoult. 1999. Q fever. Clin. Microbiol. Rev. 14:518-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCaul, T. F., J. C. Williams, and H. A. Thompson. 1991. Electron microscopy of Coxiella burnetii in tissue culture. Induction of cell types as products of developmental cycle. Acta Virol. 35:545-560. [PubMed] [Google Scholar]
- 34.Norlander, L. 2000. Q fever epidemiology and pathogenesis. Microbes Infect. 2:417-424. [DOI] [PubMed] [Google Scholar]
- 35.Polsinelli, T., M. S. Meltzer, and A. H. Fortier. 1994. Nitric oxide-independent killing of Francisella tularensis by IFN-γ stimulated murine alveolar macrophages. J. Immunol. 153:1238-1245. [PubMed] [Google Scholar]
- 36.Rabinovitch, M., E. Freymuller, R. A. de Paula, P. Manque, W. K. Andreoli, and R. A. Mortara. 1999. Cell coinfections with nonviral pathogens and the construction of doubly infected phagosomes, p. 349-371. In S. Gordon (ed.), Phagocytosis and pathogens. JAI Press, Stamford, Conn.
- 37.Redd, T., and H. A. Thompson. 1995. Secretion of proteins by Coxiella burnetii. Microbiology 141:363-369. [DOI] [PubMed] [Google Scholar]
- 38.Sexton, J. A., and J. P. Vogel. 2002. Type IVB secretion by intracellular pathogens. Traffic 3:178-185. [DOI] [PubMed] [Google Scholar]
- 39.Tujulin, E., B. Lilliehook, A. Macellaro, A. Sjostedt, and L. Norlander. 1999. Early cytokine induction in mouse P388D1 macrophages infected by Coxiella burnetii. Vet. Immunol. Immunopathol. 68:159-168. [DOI] [PubMed] [Google Scholar]
- 40.Vasselon, T., and P. A. Detmers. 2002. Toll receptors: a central element in innate immune responses. Infect. Immun. 70:1033-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams, J. C., and H. A. Thompson (ed.). 1991. Q fever: the biology of Coxiella burnetii. CRC Press, Inc., Boca Raton, Fla.
- 42.Yoshiie, K., S. Matayoshi, T. Fujimura, N. Maeno, and H. Oda. 1999. Induced production of nitric oxide and sensitivity of alveolar macrophages derived from mice with different sensitivity to Coxiella burnetii. Acta Virol. 43:273-278. [PubMed] [Google Scholar]
- 43.Zamboni, D. S., R. A. Mortara, and M. Rabinovitch. 2001. Infection of Vero cells with Coxiella burnetii phase II: relative intracellular bacterial load and distribution estimated by confocal laser scanning microscopy and morphometry. J. Microbiol. Methods 43:223-232. [DOI] [PubMed] [Google Scholar]
- 44.Zamboni, D. S., E. Freymuller, R. A. Mortara, and M. Rabinovitch. 2002. Mouse resident peritoneal macrophages partially control in vitro infection with Coxiella burnetii phase II. Microbes Infect. 4:591-598. [DOI] [PubMed] [Google Scholar]