A proximal femoral or hip fracture is the most common reason for admission to an acute orthopaedic ward. About 86 000 such fractures occur each year in the United Kingdom.w1 Global numbers were reported as 1.3 million in 1990, and depending on secular trends could be 7-21 million by 2050.1
In developed countries, the treatment of a hip fracture requires a wide range of disciplines, as the patient will present to the ambulance service and the accident and emergency unit, then pass through departments of radiology, anaesthetics, orthopaedic surgery, medicine, and rehabilitation. Medical and social services in the community may be needed when the patient leaves hospital.
Mortality associated with a hip fracture is about 5-10% after one month. One year after fracture about a third of patients will have died, compared with an expected annual mortality of about 10% in this age group.2,3 w2 Thus, only a third of deaths are directly attributable to the hip fracture itself, but patients and relatives often think that the fracture has played a crucial part in the final illness.w2
More than 10% of survivors will be unable to return to their previous residence. Most of the remainder will have some residual pain or disability.2,3
Search strategy
The musculoskeletal Cochrane review group has identified all randomised controlled trials on hip fractures and most are summarised in Cochrane reviews (www.Cochrane.org) and in Clinical Evidence articles.4
For aspects of hip fracture that cannot or have not been subject to randomised controlled trials, we looked at systematic review articles, the evidence based guidelines identified on this topic, and our personal libraries of hip fracture references based on annual Medline searches.5-7
Who fractures their hip?
The average age of patients with hip fracture is over 80, and nearly 80% are women.2 The annual risk of hip fracture is age related and reaches 4% in women over 85.w3
Most hip fractures result from a fall or stumble—only about 5% of cases have no history of injury.w4-w8
Injuries have a multifactorial origin, and they reflect increased tendency to fall, loss of protective reflexes, and reduced bone strength. Rates of hip fracture are three times higher among people living in care homes than in those of the same age living in the community.w9
How is the fracture diagnosed and classified?
Most hip fractures are readily diagnosed by a history of a fall that led to a painful hip, inability to walk, or an externally rotated limb, and plain radiographs of the hip that confirm the diagnosis. In about 15% of cases, the hip fracture is undisplaced, and radiographic changes may be minimalw10; in a further 1% of cases the fracture will not be visible on plain radiographs, and other investigations will be needed. Magnetic resonance imaging is currently the investigation of choice in this situation.w11 w12
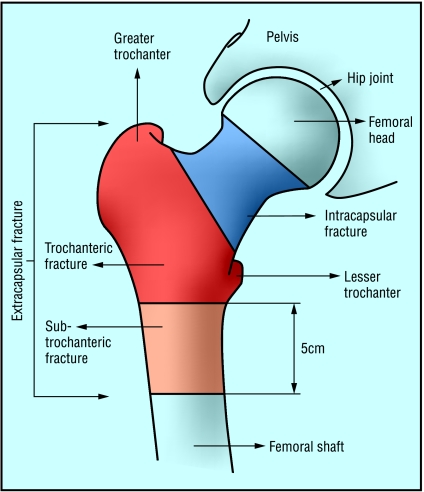
Fractures can be classified radiographically into intracapsular and extracapsular fractures (figure). These may be further subdivided, depending on the level of the fracture and the presence or absence of displacement and comminution.w13-w15
Figure 1.
Classification of hip fractures. Fractures in the blue area are intracapsular and those in the red and orange areas are extracapsular
Healing of intracapsular fractures is complicated by the tenuous blood supply to the femoral head—the retinacular vessels that pass up the femoral capsule may be damaged, especially if the fracture is displaced. This problem does not occur in extracapsular fractures, but up to one litre of blood may be lost from fractures at this site, so fluid replacement and blood transfusion may be needed.
Treatment
The first step is to decide between a surgical or conservative approach. Conservative treatment is now rarely used because of poor outcome and prolonged hospital stay. Conservative treatment of a displaced intracapsular fracture leads to a painful functionless hip. An undisplaced intracapsular fracture can be managed with analgesia, a few days rest, then gentle mobilisation, but the risk of subsequent displacement of the fracture is high, and internal fixation is preferable.w16-w19
Extracapsular fractures can be managed with traction, but this must be maintained for one to two months. The frail older people who typically sustain this injury are poorly equipped to cope with prolonged immobilisation, which may result in loss of mobility and independence.w19 w20 This may precipitate placement into a long term care home—an outcome that some perceive as worse than death.w21 Thus, most hip fractures are treated by surgery.
Intracapsular fractures may be treated by fixing the fracture and preserving the femoral head.w22 Preservation of the femoral head is appropriate for undisplaced fractures and for displaced fractures in “younger” patients (under 70). In frail or older people, displaced intracapsular fractures may be treated by reduction and fixation, but the incidence of non-union and avascular necrosis is 30-50% for this procedure, so the femoral head is replaced in most patients.w23 w24 The approach may be hemiarthroplasty, where just the femoral head is replaced, or a total hip replacement, where both sides of the joint are replaced. Cementing the prosthesis in place results in less pain and better mobility (figs A and B on bmj.com).w25
Various types of plates, screws, and nails are available for fixing extracapsular fractures. At present, the sliding hip screw is the most effective device.w26 Subtrochanteric fractures may also be fixed with a sliding hip screw, but these are increasingly being treated with an intramedullary nail (figs C and D on bmj.com). With current implants and surgical techniques, most patients with hip fracture can be allowed to bear weight on the injured limb, and hip movements should not be restricted after surgery.
Perioperative care
Traction to the limb before surgery seems to be of no benefit.w27 Spinal anaesthesia may be marginally better than general anaesthesia.w28 w29 Box 1 lists aspects of good practice that have been recommended for the care of patients with hip fracture.5-7
Thromboembolic prophylaxis is a contentious issue. People who sustain a hip fracture are at high risk of thromboembolic complications but are also at risk of the adverse effects of prophylactic drugs. The incidence of thromboembolic complications has fallen as a result of the measures listed in box 2, and the adverse effects of prophylaxis may outweigh the benefits. A systematic review of heparins and a large randomised trial of low dose aspirin noted a reduction in thromboembolic complications with prophylaxis, but at the expense of increased bleeding complications.w37 w42
Box 1 Recommended components of care for patients with hip fracture
From admission
Adequate, appropriate analgesia
Supplementary nerve blocks for pain reliefw30
Intravenous fluid replacement
Monitoring of fluid balance
Assessment of associated injuries and medical conditions
Fast tracking through the casualty departmentw31
Use of defined clinical pathwaysw32
Pressure area assessment and carew33 w34
On the ward
Help with eating in the early postoperative periodw35
Nutritional supportw36
Thromboembolic prophylaxisw37
At surgery
Surgery within 48 hours of admissionw38-w40
Perioperative antibiotic prophylaxisw41
Perioperative supplementary oxygen5
After surgery
Mobilisation the day after surgery
Early rehabilitation and planning for discharge
Cyclical leg compression or foot pump devices can reduce thromboembolic complications but are time consuming and costly, and the effectiveness of graduated compression stockings is unclear in these patients.5 w37 None of these approaches to thromboembolic prophylaxis have been shown to reduce overall mortality after hip fracture.
Rehabilitation
Rehabilitation should start from the time of admission. It is important for the patient and the family to outline a proposed plan of treatment, along with provisional dates for discharge. This helps them make necessary arrangements, such as getting a bed downstairs.
Many patients who sustain a hip fracture fear that it will result in death or disability, and it is important to set reasonable expectations to restore their morale. However, over optimistic reassurance about the success of surgery may lead to disappointment if rehabilitation is slow. Assessment must be comprehensive in order to identify impediments to recovery, set realistic goals, and coordinate appropriate rehabilitation.
Box 2 Recommended measures to reduce the risk of thromboembolic complications
Avoidance of dehydration
Early surgery
Avoidance of prolonged surgery
Avoidance of over transfusion
Early mobilisation
Box 3 Approaches to rehabilitation
Traditional care on the orthopaedic ward, with variable degrees of input from geriatricians
Initial treatment on the orthopaedic ward, with subsequent transfer to a hospital based geriatric-orthopaedic rehabilitation unitw43
Initial treatment on the orthopaedic ward, with subsequent transfer to a skilled nursing facility in the community for assessment and rehabilitationw44
Shared care on a ward that combines orthopaedic surgical care with geriatric medical assessment and rehabilitation until dischargew45
Care on an orthopaedic ward and early discharge home with the support of a community rehabilitation teamw46
Box 4 Recommended plan for assessing and preventing falls
Clinical assessment to determine the cause of any falls
Assessment of mental state
Medication review
Management of osteoporosis
Visual assessment and correction if possible
Assessment of continence
Assessment of gait and balance disorders
Mobility improvement and strength training for inpatients
Provision of appropriate walking aids and footwear
Home assessment and modification of environmental hazards
Access to strength and balance training after discharge
Five broad categories of rehabilitation have been described (box 3).8
The National Service Framework for Older People in England recommends that each hospital should have at least one “orthogeriatric” ward.9 The optimum model of care is unknown—randomised trials have produced conflicting results and no clear consensus.10
Can further fractures be prevented?
Multidisciplinary assessment of the reason for the fall will reduce the risk of further fractures, and the components of such assessments are well described.11,12 Nearly all patients with hip fracture meet the criteria for such an assessment, which should be performed routinely as part of inpatient rehabilitation care (box 4). A medical cause for the fall should be sought; specifically, hypotension, postural hypotension, arrhythmia, vasovagal syncope, and carotid sinus hypersensitivity. Examination should include lying and standing blood pressure and a 12 lead electrocardiogram.
About 3% of hip fractures are related to localised bone weakness at the fracture site, secondary to tumour, bone cysts, or Paget's disease. More than half of the remaining patients have osteoporosis, and nearly all are osteopenic. Over the age of 80, a woman with normal bone mineral density for her age will have a T score of around - 2.5 (the diagnostic threshold for osteoporosis). Thus, assessment of bone density is probably not necessary in older age groups, and current UK guidelines only recommend a dual energy x ray absorptiometry scan for women under the age of 75.13
In men and younger women, routine preoperative blood counts and basic biochemistry may need to be accompanied by tests for causes of bone fragility. Malnutrition, low body weight, alcoholism, and deficiency of calcium or vitamin D are common and important at all ages. Treatment with steroids, renal failure, liver disease, hyperthyroidism, hyperparathyroidism, and hypogonadism are other potential causes of bone fragility.
Pharmacological prevention of hip fracture is controversial. An early study showed a benefit of calcium and vitamin D supplementation in residents of care homes. A similar regimen was therefore adopted among people recovering from hip fracture, but this approach has not been supported by later studies.14,15 w47, w48
Oral bisphosphonates are widely recommended for secondary prevention of fragility fractures; UK guidelines advocate them for all women over 75 and for younger women with confirmed osteoporosis.16 The effectiveness of bisphosphonates in the very elderly is not known, although no reason exists to doubt their efficacy in this situation.17 Careful explanation and counselling are crucial to the effective use of these drugs. Pre-existing gastrointestinal problems raise concern over upper gastrointestinal intolerance, and some frailer patients may have difficulty adhering to the dosing regimen.
Strontium may be an effective and convenient alternative in frailer patients.w49 Suggestions that strontium may predispose patients to thromboembolism have not been confirmed, but prescription should be delayed until the patient is mobile. Calcium and vitamin D status should be optimised in patients taking bisphosphonates or strontium.
Hormone replacement therapy and selective oestrogen receptor antagonists should be avoided in women recovering from hip fractures, as they greatly increase the risk of thromboembolism.18,19 Early reports of hip protectors, which absorb or spread the energy of a fall, were promising, but recent studies have questioned their effectiveness.20,21
Current and future directions for research
New designs and developments in surgical implants
Assessment of many aspects of perioperative care
Definition of the optimum method of rehabilitation
Evaluation of proposed methods for reducing the risk of further fractures
Additional educational resources
Further reading
Parker MJ, Handoll HHG. Hip fracture. Clinical evidence. BMJ Publishing, 20054
Scottish Intercollegiate Guidelines Network (SIGN). Prevention and management of hip fractures in older people. SIGN Publication No 56. (www.sign.ac.uk/guidelines/fulltext/56/index.html)5
Cochrane Database of Systematic Reviews (www.cochrane.org/reviews/clibaccess.htm)
Patient resources
National Osteoporosis Society, PO Box 10, Bath BA3 3YB (www.nos.org.uk)
Summary points
Hip fracture is the most common cause of acute orthopaedic admission in older people
Treatment is generally surgical to replace or repair the broken bone
Mortality is 5-10% after one month and about 30% after one year
Some loss of function is to be expected in most patients
Multidisciplinary rehabilitation is needed for the patient to return home
Ways to reduce the risk of further fracture should be considered
Conclusions
Hip fracture is the most common disabling injury and cause of accidental death in older people. The incidence and the public health and economic consequences of this injury have risen as the population has aged, and this is expected to continue for the foreseeable future.
The prevention and management of hip fractures involves a wide range of disciplines, and most people who sustain the injury require surgery followed by a period of rehabilitation. The complexity of care needed for hip fractures makes the condition a real test and a useful marker of the integration and effectiveness of modern health care.
Supplementary Material
 Extra references w1-w49 and figures A-D appear on bmj.com
Extra references w1-w49 and figures A-D appear on bmj.com
Competing interests: None declared by MP. AJ received reimbursement of conference expenses and fees for non-promotional lecturing from the manufacturers of various oral bisphosphonates.
References
- 1.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporosis Int 1997;7: 407-13. [DOI] [PubMed] [Google Scholar]
- 2.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fracture. BMJ 1993;307: 1248-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roche JJW, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2006;331: 1374-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parker MJ, Handoll HHG. Hip fracture. Clinical evidence. BMJ Publishing, 2005. [PubMed]
- 5.Scottish Intercollegiate Guidelines Network (SIGN). Prevention and management of hip fractures in older people. SIGN Publication No 56. Edinburgh: SIGN. 2002. www.sign.ac.uk/guidelines/fulltext/56/index.html (last accessed 6 Jun 2006).
- 6.New Zealand Guidelines Group. Acute management and immediate rehabilitation after hip fracture amongst people aged 65 years and over. 2003. www.nzgg.org.nz/guidelines/dsp_guideline_popup.cfm?guidelineCatID=32&guidelineID=7 (last accessed 6 Jun 2006).
- 7.March LM, Chamberlain AC, Cameron ID, Cumming RG, Brnabic AJM, Finnegan TP, et al. How best to fix the broken hip. Med J Aust 1999;170: 489-94. [PubMed] [Google Scholar]
- 8.Cameron I, Crotty M, Curry C, Finnegan T, Gillespie L, Gillespie W, et al. Geriatric rehabilitation following fractures in older people: a systematic review. Health Technol Assess 2000;4(2): i-iv, [PubMed] [Google Scholar]; 1-111.
- 9.Department of Health. National service framework for older people. London: DoH, 2001 www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4003066&chk=wg3bg0 (last accessed 8 Jun 2006).
- 10.Cameron ID, Handoll HHG, Finnegan TP, Madhok R, Langhorne P. Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures. Cochrane Database Syst Rev 2001;(3): CD000106. [DOI] [PubMed]
- 11.Gillespie LD, Gillespie WJ, Cumming R, Lamb SE, Rowe BH. Interventions for preventing falls in the elderly. Cochrane Database Syst Rev 2003;(4): CD000340. [DOI] [PubMed]
- 12.American Geriatrics Society, British Geriatrics Society, American Academy of Orthopaedic Surgeons. National guidelines for the prevention of falls in older persons. 2001. http://www.americangeriatrics.org/products/positionpapers/Falls.pdf (last accessed 6 Jun 2006). [PubMed]
- 13.National Institute for Health and Clinical Assessment. Clinical practice guideline for the assessment and prevention of falls in older people. London: NICE, 2004. www.nice.org.uk/page.aspx?o=cg021fullguideline (last accessed 6 Jun 2006).
- 14.Chapuy MC, Arlot ME, Delmas PD, Meunier PJ. Effect of calcium and cholecalciferol treatment for 3 years on hip fractures in elderly women. BMJ 1994;308: 1081-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avenell A, Gillespie WJ, Gillespie LD, O'Connell DL. Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev 2005;(3): CD000227. [DOI] [PubMed]
- 16.National Institute for Health and Clinical Excellence. Bisphosphonates (alendronate, etidronate, risedronate), selective oestrogen receptor modulators (raloxifene) and parathyroid hormone (teriparatide) for the secondary prevention of osteoporotic fragility fractures in postmenopausal women. London: NICE, 2005. www.nice.org.uk/pdf/TA087guidance.pdf (last accessed 6 Jun 2006).
- 17.Boonen S, McClung MR, Eastell R, Fuleihan GE-H, Barton IP, Delmas P. Safety and efficacy of risedronate in reducing fracture risk in osteoporotic women aged 80 and older: implications for use of antiresorptive agents in the old and oldest old. J Am Geriatr Soc 2004;52: 1836-9. [DOI] [PubMed] [Google Scholar]
- 18.Writing Group for the Women's Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results for the Women's health initiative randomized controlled trial. JAMA 2002;288: 321-33. [DOI] [PubMed] [Google Scholar]
- 19.Cummings SR, Eckert S, Krueger KA, Grady D, Powles TJ, Cauley JA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple outcomes of raloxifene evaluation. JAMA 1999;281: 2189-97. [DOI] [PubMed] [Google Scholar]
- 20.Parker MJ, Gillespie LD, Gillespie WJ. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev 2005;(3): CD001255. [DOI] [PubMed]
- 21.Parker MJ, Gillespie L, Gillespie W. Hip protectors for preventing hip fractures in the elderly: the evolution of a systematic review of randomised controlled trials. BMJ 2006;332: 571-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.