Abstract
Infections due to Coxiella burnetii, the causative agent of Q fever, are uncommon in the United States. Cases of chronic Q fever are extremely rare and most often manifest as culture-negative endocarditis in patients with underlying valvular heart disease. We describe a 31-year-old farmer from West Virginia with a history of congenital heart disease and recurrent fevers for 14 months who was diagnosed with Q fever endocarditis based on an extremely high antibody titer against Coxiella burnetii phase I antigen. Despite treatment with doxycycline, he continued to have markedly elevated Coxiella burnetii phase I antibody titers for 10 years after the initial diagnosis. To our knowledge, this case represents the longest follow-up period for a patient with chronic Q fever in the United States. We review all cases of chronic Q fever reported in the United States and discuss important issues pertaining to epidemiology, diagnosis, and management of this disease.
CASE REPORT
A 31-year-old farmer from West Virginia was admitted in June 1995 because of recurrent episodes of fever as high as 39°C, night sweats, paroxysmal coughing, chest pressure, decreased appetite, fatigue, and an 11-kg involuntary weight loss over the preceding 14 months. He had been treated several times for presumed bronchitis with various antibiotics, but his complaints had worsened since December 1994. His past medical history was significant for congenital heart disease, including dextrocardia, a double-outlet right ventricle, a ventricular septal defect, and severe pulmonary stenosis. As an infant, he had undergone operative placement of a right Blalock-Taussig shunt, and at age 12, he underwent surgery for closure of a ventricular septal defect and placement of a conduit between the right ventricle and pulmonary artery. At age 26, he underwent surgery for replacement with a 22-mm Hancock conduit. He participated in birthing his calves, one of which was stillborn around the time of the onset of his illness. He was treated empirically with penicillin, gentamicin, and vancomycin, and his fevers resolved.
On physical examination, he was a thin, chronically ill-appearing white male. His vital signs were within normal limits, and he was afebrile. Cardiac examination revealed a grade 3/6 harsh systolic ejection murmur heard maximally at the right upper sternal border without radiation. The chest examination was normal. There was no hepatosplenomegaly, enlarged lymph nodes, or peripheral stigmata of endocarditis. Laboratory studies revealed the following results: hematocrit level was 41%; white blood cell count was 7.3 × 109 white blood cells/liter, with a differential cell count of 35% segmented neutrophils, 5% bands, and 54% lymphocytes; platelets were aggregated and uncountable; electrolyte panel and urinalysis were normal; erythrocyte sedimentation rate was 34 mm/h; and alkaline phosphatase, aspartate aminotransferase, and alanine aminotransferase levels were elevated at 198 U/liter, 244 U/liter, and 196 U/liter, respectively. Serologies for hepatitis A, B, and C viruses were negative. The patient was positive for human immunodeficiency virus by enzyme-linked immunosorbent assay, but confirmatory Western blot analysis was negative. Multiple blood cultures were negative for bacteria and fungi. Tuberculin skin test was negative with a positive anergy panel. Serology studies for Brucella species, Legionella species, Borrelia burgdorferi, Chlamydia species, Blastomyces dermatitidis, Coccidioides immitis, and Histoplasma capsulatum were negative. Coxiella burnetii phase I titers by microimmunofluorescence using antigens and the technique of the WHO Collaborative Center for Rickettsial Reference and Research (D. Raoult, Marseille, France) were 163,840 (immunoglobulin G [IgG]) and 40,960 (IgM), and phase II titers were ≥327,680 (IgG) and 81,920 (IgM). A bone marrow biopsy (Fig. 1) and liver biopsy revealed granulomas, and special stains for bacteria, fungi, and acid-fast bacilli were negative. Routine bacterial, fungal, and acid-fast cultures were negative. Immunohistological staining of the bone marrow and liver biopsy specimens were negative for C. burnetii.
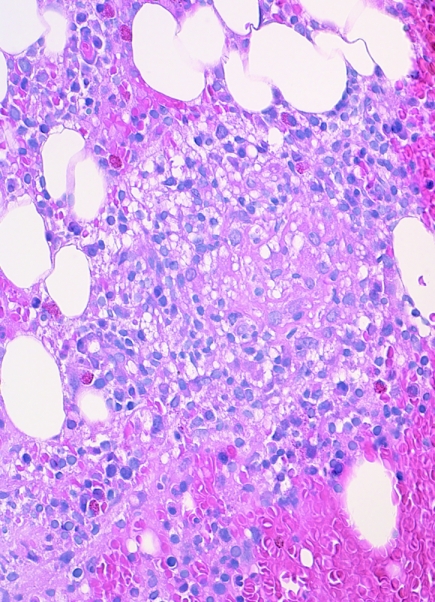
FIG. 1.
Noncaseating granuloma in the bone marrow of a 31-year-old farmer with chronic Q fever (hematoxylin and eosin stain; original magnification, ×100).
Computed tomography of the chest, abdomen, and pelvis were unrevealing. Transthoracic and transesophageal echocardiography revealed no evidence of intracardiac vegetation. Doxycycline and rifampin treatment were initiated to treat Coxiella burnetii infection, and the patient rapidly defervesced. Ciprofloxacin was subsequently substituted for rifampin, and the patient was advised that replacement of the conduit would likely be required to achieve a microbiological cure. However, he declined further surgery, and the antibiotic combination of doxycycline and ciprofloxacin was prescribed indefinitely for presumed Q fever prosthetic endocarditis.
During the 10 years following his initial diagnosis of chronic Q fever, he had seven transthoracic echocardiograms and three cardiac magnetic resonance imaging studies, all of which were negative for intracardiac vegetations. Early in his course of therapy, the patient stopped taking ciprofloxacin and maintained variable adherence with his doxycycline regimen, discontinuing the antibiotic on average once to twice per year between 1995 and 2005. Within several weeks after each discontinuation trial, he developed persistent fevers, weight loss, and generalized fatigue, which resolved with reinstitution of the medication. He refused to take hydroxychloroquine because of concern for ocular toxicity. The patient's C. burnetii titers during the 10-year follow-up period are shown in Table 1.
TABLE 1.
C. burnetii serology of a patient with chronic Q fever
| Date (mo/day/yr) | Microimmunofluorescence titer
|
|||
|---|---|---|---|---|
| Anti-phase I
|
Anti-phase II
|
|||
| IgG | IgM | IgG | IgM | |
| 6/13/1995 | 163,840 | 40,960 | 327,680 | 81,920 |
| 4/25/1996 | 163,840 | 10,240 | 327,680 | 40,960 |
| 5/25/1996 | 81,920 | 20,480 | 163,840 | 40,960 |
| 11/21/1996 | 20,480 | 5,120 | 81,920 | 10,240 |
| 9/18/1997 | 10,240 | 640 | 81,920 | 2,560 |
| 4/18/1998 | 10,240 | 640 | 40,960 | 1,280 |
| 4/23/2005 | 3,200 | 50 | 6,400 | 100 |
Q fever is a zoonosis caused by Coxiella burnetii, a small obligate intracellular gram-negative bacterium that is prevalent throughout the world. Domesticated ungulates, including cattle, sheep, and goats, are considered the primary reservoirs for human infection, but pets such as cats and dogs as well as ticks and other arthropods may also transmit infection (23). Infected mammals are typically asymptomatic but shed C. burnetii in their urine, feces, milk, and birth products, and most human Q fever infections are acquired through the inhalation of contaminated aerosols, often generated during parturition events (31). Therefore, persons at highest risk for Q fever include farmers, veterinarians, abattoir workers, those in contact with dairy products, and laboratory personnel working with C. burnetii (23). C. burnetii is highly resistant to desiccation and environmental degradation and can be disseminated by wind (35). Thus, Q fever may occur in patients without any direct contact with animals (4). Its highly infectious nature and aerosol route of transmission make C. burnetii a potential agent of bioterrorism, and the organism has been classified as a group B agent by the Centers for Disease Control and Prevention (20). Human Q fever became a nationally notifiable disease in the United States in 1999 (4).
Epidemiology of C. burnetii infection.
The reported seroprevalence of bovine Q fever in the United States varies widely from state to state, but seroepidemiologic studies suggest that C. burnetii infection has increased in U.S. cattle during the last several decades (12). The highest rates of infection have been reported in California, where a 98% herd infection rate was reported in the 1950s (18), and another survey in the 1970s revealed that 100% of herds in 17 counties contained seropositive cattle (82% of 1,052 specific cattle from the herds were seropositive) (2). A survey of 787 herds of cattle in the Milwaukee area showed that the incidence of bovine Q fever increased from 32% in 1957 to 61% in 1959 and 73% in 1962, and a random sample of 50 C. burnetii-positive herds found that 84% of the cattle were shedding the organism in their milk (38). Recently, a real-time PCR assay targeting the IS1111 sequence, which is unique to C. burnetii, detected the organism in 94.3% of bulk tank milk samples from U.S. dairy herds tested during a 3-year period (12), with little regional or temporal variation, suggesting that C. burnetii infection in cattle is very common and persistent throughout the United States.
Despite the rising prevalence of C. burnetii infection in U.S. cattle, the passively reported prevalence of Q fever among the United States human population remains exceedingly low. Transmission of C. burnetii from cattle to humans may be reduced by the pasteurization process of commercial milk, but persons with significant contact with cattle and other domestic animals remain at increased risk for infection. The first major Q fever outbreaks in the United States were reported in 1946 and involved 55 stock handlers and slaughterhouse workers in Amarillo, Texas (36), and 33 employees of a sheep- and calf-killing department of a large packing house in Chicago, Illinois (34). Between 1948 and 1977, 1,164 human Q fever cases were optionally reported to the Center for Disease Control, with the majority of cases (67%) occurring in California (5). Fewer than 30 cases were reported annually between 1978 and 1986 (33), and 48 cases were reported to the Centers for Disease Control and Prevention between 2000 and 2001 (4). A Q fever outbreak involving 15 family members who had attended a family reunion and were exposed to a parturient cat occurred in 1989 in eastern Maine. Interestingly, parturient cats have also been implicated in C. burnetii transmission in neighboring Nova Scotia, Canada (14, 15), suggesting a common wildlife reservoir, such as small rodents (19).
Clinical manifestations.
The clinical manifestations of Q fever vary widely. Up to 60% of infected individuals develop no symptoms (31). Acute Q fever, which develops after an incubation period of 2 to 5 weeks, is usually characterized by a nonspecific febrile illness, pneumonitis, or hepatitis. Other less common clinical manifestations of acute Q fever include myocarditis, pericarditis, skin rash, and meningoencephalitis (23). Chronic Q fever may develop many months to years after initial infection, manifesting as bacterial culture-negative endocarditis in up to 75% of cases (10). Chronic Q fever occurs almost exclusively in patients with predisposing conditions, including those with heart valve lesions, vascular abnormalities, and immunosuppression (7). In addition to endocarditis, chronic Q fever less frequently presents as vascular infections, osteoarticular infections, chronic hepatitis, chronic pulmonary infections, and chronic fatigue syndrome (23). Over 90% of Q fever endocarditis cases occur in persons with underlying heart disease, which may be congenital, rheumatic, degenerative, or syphilitic or may involve prosthetic valves (23). Whereas C. burnetii accounts for 3% of all endocarditis cases diagnosed in England and Wales (26) and at least 5% of cases in France (29), there have been only seven reported cases of Q fever endocarditis in the United States, including the patient presented here (1, 4, 10, 13, 27). However, the true number of chronic Q fever cases in the United States is unknown and is likely underrepresented in the literature, since many cases may have occurred prior to the advent of national reporting in 1999. In addition, patients with endocarditis may have received multiple antibiotics prior to valve replacement, making isolation of the organism from infected tissue less likely.
Demographic analysis of the chronic Q fever cases reported in the United States reveals that 100% of patients (seven of seven) were male (Table 2), consistent with the male predominance reported in other countries, including France, where the male-to-female ratio for C. burnetii infection is 2.45 in adults (31). Their average age at the time of diagnosis was 53 ± 20 years (median age, 49 years). This finding corroborates observations that advanced age appears to be associated with an increased risk of C. burnetii infection (31) and that patients with chronic Q fever tend to be older than those who develop acute Q fever (32). The duration of symptoms prior to diagnosis in patients with chronic Q fever in the United States was 5.6 ± 4.4 months, ranging from 1 month (patient 6) to 14 months (our patient). Six of seven patients for whom information was available had direct farm exposure, while the other patient had no exposure to farm animals but hunted deer, bear, and pheasant in Minnesota (10), which may have placed him at increased risk for C. burnetii infection from a wildlife reservoir (19). Three of seven patients, including our patient, had congenital cardiac anomalies, one patient had a history of mitral and aortic valve replacements, and three of seven patients had no evidence of cardiac anomalies. All seven patients were diagnosed with culture-negative endocarditis, and six of the seven patients had direct evidence of cardiac involvement by either echocardiography or pathology. Our patient (patient 4) did not have definitive evidence of cardiac involvement, with repeatedly negative echocardiograms and cardiac magnetic resonance imaging results, but he was presumed to have culture-negative endocarditis in the setting of congenital heart disease and an intracardiac conduit. In all six patients, the aortic valve was affected, requiring aortic valve replacement in four cases. No patients had involvement of any other heart valves. Our patient represents the only case of chronic Q fever reported in the United States with documented pathological involvement of extracardiac sites (bone marrow and liver).
TABLE 2.
C. burnetii serologies of patients with chronic Q fevera
| Patient (reference) | Yr of diagnosis | Age (yr) | Gender | State of residence | Direct farm exposure | Duration of illness before diagnosis (mos) | Underlying cardiac anomaly | Clinical manifestation | Embolic phenomena | Affected valve | Valve replaced during present illness | Antibody reciprocal titer (phase I IgG) at time of diagnosis | Antibody titer technique |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (17) | 2004 | 40 | M | MN | N | 2 | Con, AVR | CNE | − | A | N | 40,960 | IFA |
| 2 (4) | 2001 | 49 | M | TN | Y | 6 | Con | CNE | + | A | Y | >512 | IFA |
| 3 (4) | 2000 | 90 | M | PA | Y | 4 | CNE | − | A | Y | >524,288 | IFA | |
| 4b | 1995 | 31 | M | WV | Y | 14 | Con | CNE | − | NA | N | >327,680 | IFA |
| 5 (23) | 1984 | 65 | M | AL | Y | 8 | MVR, AVR | CNE | − | A | Y | 32,768 | IFA |
| 6 (21) | 1977 | 39 | M | NA | NA | 1 | CNE | + | A | Nc | 32d | CF | |
| 7 (22) | 1976 | 54 | M | OR | Y | 4 | CNE | + | A | Y | 4,096 | CF |
M, male; N, no; Y, yes; Con, congenital heart disease; AVR, aortic valve replacement; MVR, mitral valve replacement; CNE, culture-negative endocarditis; IFA, immunofluorescence assay; CF, complement fixation; NA, not available; −, absence of embolic phenomena; +, presence of embolic phenomena; A, aorta.
Current case.
Patient died.
No phase reported.
Diagnosis of chronic Q fever.
As witnessed in these seven cases, the diagnosis of chronic Q fever may be delayed by many months because of the lack of specific signs and symptoms. Fever may be absent in more than 18% of cases, and vague constitutional symptoms, congestive heart failure, or valvular dysfunction may predominate (10). Peripheral manifestations of endocarditis including digital clubbing, purpuric rash, hepatomegaly, splenomegaly, immune complex glomerulonephritis, and embolic phenomena are common (21). Cardiac vegetations are visible by echocardiography in as few as 12% of patients (23), as these vegetations tend to be smaller and located beneath endothelial surfaces (10). The organism may be cultured under special conditions, but isolation of C. burnetii by culture is generally not performed because of the high risk of infectivity to laboratory workers and the lack of sensitivity of the technique (25). Instead, serologic testing remains the most widely used diagnostic method. The specific techniques commonly used include complement fixation, indirect immunofluorescence assay or microimmunofluorescence, enzyme-linked immunosorbent assay, and microagglutination (23). C. burnetii exhibits antigenic phase variation (phases I and II), which is highly valuable in differentiating between acute and chronic Q fever. Acute Q fever is characterized by antibodies against phase II antigens, whereas chronic Q fever is characterized by the presence of anti-phase I antibodies, usually in the presence of anti-phase II antibodies (9). An IgG anti-phase I antibody titer of ≥800 is considered diagnostic of Q fever endocarditis (6, 32). High C. burnetii IgA titers were previously thought to correlate with chronic Q fever endocarditis, but a more recent study has shown that such reactions are not specific to this form of the infection (23).
Recently, a molecular detection approach for testing of patient sera using a nested PCR assay demonstrated an optimal sensitivity of 64% and specificity of 100% for the diagnosis of chronic Q fever, but the assay's sensitivity was dramatically reduced if serum samples were stored at −20°C or if IgG phase I titers were greater than 25,600 (8). Pathological features of affected cardiac valves are nonspecific, characterized by significant fibrosis and calcifications, slight inflammation and vascularization, and small or absent vegetations (16), although the presence of foamy or “empty” macrophages may be suggestive of C. burnetii infection (3). C. burnetii may be detected in cardiac tissue by immunohistochemical analysis, culture, or PCR even after prolonged antibiotic treatment (3, 9, 16, 24, 37).
Therapy and prevention of chronic Q fever.
Chronic Q fever is a severe illness for which the spontaneous death rate may exceed 65% (23). With appropriate antibiotic therapy, chronic Q fever-associated mortality may be significantly reduced, but the organism is difficult to eradicate, and a prolonged course of antibiotic treatment is necessary. In vitro data have shown that the pH within the acidified phagosomal compartment in which intracellular C. burnetii resides may be responsible for the lack of bactericidal activity of many antibiotics (22). C. burnetii is inherently resistant to β-lactam compounds and aminoglycosides, but the organism is generally susceptible to tetracycline derivatives, cotrimoxazole, rifampin, and the fluoroquinolones. Monotherapy with each of these drugs may be effective in reducing the symptoms associated with chronic Q fever, but relapses are frequent upon cessation of antibiotics, prompting the development of combination regimens (17, 30). Although the combination of doxycycline and rifampin appears to be more effective than doxycycline alone, the use of rifampin is limited by drug-related interactions, especially with anticoagulant agents, which are often prescribed to patients with cardiac valve defects or prosthetic valves (28).
In a retrospective multicenter study involving 16 patients with Q fever endocarditis treated with fluoroquinolones and doxycycline, the combination regimen led to a statistically significant difference in mortality compared to doxycycline monotherapy (17). However, based on clinical, serological, and valve tissue culture results, neither therapy was able to cure Q fever endocarditis within 2 years, and those authors recommended a minimum duration of 3 years of therapy with doxycycline and fluoroquinolones.
Hydroxychloroquine, an alkalinizing agent of phagolysosomes, in combination with doxycycline has been shown to have in vitro bactericidal activity against C. burnetii (22). In a clinical study involving 35 patients with Q fever endocarditis, the addition of hydroxychloroquine to doxycycline was found to reduce the median duration of treatment by 2 years compared to treatment with doxycycline and ofloxacin, and there were no relapses after 18 months of therapy in the group that received hydroxychloroquine-doxycycline (30). The mortality rate for both regimens was 5%, and the major complication associated with each regimen was hypersensitivity to sunlight. Adverse effects of hydroxychloroquine include photosensitivity and retinal accumulation, but only 1 of 21 patients in the doxycycline-hydroxychloroquine group developed retinal toxicity that required the discontinuation of hydroxychloroquine treatment (30).
Although the optimal duration of therapy is unknown, based on these findings, the current recommendations for the treatment of chronic Q fever are 100 mg of doxycycline by mouth twice daily with 600 mg of hydroxychloroquine by mouth once daily for at least 18 months. Serologic testing is recommended on a regular basis during therapy, and the main predictive criterion of clinical cure is a decrease of phase I IgG antibody titers to <200 (28).
Because Q fever is an occupational hazard, vaccination has been advocated for exposed populations, including livestock handlers, abattoir workers, persons in contact with unpasteurized dairy products, veterinarians, and laboratory personnel working with C. burnetii (23). Although clinical data are lacking, vaccination should also be considered for persons who are not professionally exposed but who are at higher risk for development of chronic Q fever, including those with cardiac valve defects or prostheses, those with vascular aneurysms, and immunocompromised patients. Currently available vaccines, which are produced from phase I whole-cell C. burnetii isolates, are effective in protecting humans against infection, but vaccination of people with preexisting immunity can induce severe local and occasional systemic reactions (39). Existing Q fever vaccines for humans and animals are not commercially available in the United States.
For unclear reasons, C. burnetii infection is less commonly recognized in the United States than in other developed countries, and cases of chronic Q fever are extremely rare. However, recent seroepidemiologic studies indicate that this infection is highly prevalent among U.S. cattle (12), and a recent national survey of infectious disease experts reported that as many as 75% of diagnosed Q fever cases are not reported, and many cases are likely not diagnosed (10). Since Q fever became reportable nationally in 1999, there has been a linear increase in the numbers of human cases identified, with 21, 26, 61, 71, and 70 cases in each year from 2000 through 2004 (11). As of August 2005, 65 cases of Q fever were diagnosed in the United States in 2005, extrapolated to 110 cases over the entire year. Thus, it is likely that the prevalence of Q fever in the United States is not dissimilar to that observed in other countries where it is considered a significant and frequent cause of disease. Because affected patients may have nonspecific symptoms with no history of direct farm exposure and atypical echocardiographic findings, the diagnosis of chronic Q fever should be considered for all individuals with heart valve lesions or immunosuppression who present with unexplained fever.
Acknowledgments
We thank H. Moriuchi, K. Kotloff, and J. M. Baffa for their initial clinical evaluation of the patient at the University of Maryland, Baltimore. We are also grateful to D. Raoult, Unité des Rickettsies, WHO Collaborative Center for Rickettsial Reference and Research, Marseille, France, for the patient's most recent C. burnetii serology studies.
There was no conflict of interest.
REFERENCES
- 1.Applefeld, M. M., L. M. Billingsley, H. J. Tucker, and P. Fiset. 1977. Q fever endocarditis—a case occurring in the United States. Am. Heart J. 93:669-670. [PubMed] [Google Scholar]
- 2.Biberstein, E. L., D. E. Behymer, R. Bushnell, G. Crenshaw, H. P. Riemann, and C. E. Franti. 1974. A survey of Q fever (Coxiella burnetii) in California dairy cows. Am. J. Vet. Res. 35:1577-1582. [PubMed] [Google Scholar]
- 3.Brouqui, P., J. S. Dumler, and D. Raoult. 1994. Immunohistologic demonstration of Coxiella burnetii in the valves of patients with Q fever endocarditis. Am. J. Med. 97:451-458. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 2002. Q fever—California, Georgia, Pennsylvania, and Tennessee, 2000-2001. Morb. Mortal. Wkly. Rep. 51:924-927. [PubMed] [Google Scholar]
- 5.D'Angelo, L. J., E. F. Baker, and W. Schlosser. 1979. From the Center for Disease Control: Q fever in the United States, 1948-1977. J. Infect. Dis. 139:613-615. [DOI] [PubMed] [Google Scholar]
- 6.Dupont, H. T., X. Thirion, and D. Raoult. 1994. Q fever serology: cutoff determination for microimmunofluorescence. Clin. Diagn. Lab. Immunol. 1:189-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fenollar, F., P. E. Fournier, M. P. Carrieri, G. Habib, T. Messana, and D. Raoult. 2001. Risks factors and prevention of Q fever endocarditis. Clin. Infect. Dis. 33:312-316. [DOI] [PubMed] [Google Scholar]
- 8.Fenollar, F., P. E. Fournier, and D. Raoult. 2004. Molecular detection of Coxiella burnetii in the sera of patients with Q fever endocarditis or vascular infection. J. Clin. Microbiol. 42:4919-4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fournier, P. E., T. J. Marrie, and D. Raoult. 1998. Diagnosis of Q fever. J. Clin. Microbiol. 36:1823-1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gami, A. S., V. S. Antonios, R. L. Thompson, H. P. Chaliki, and N. M. Ammash. 2004. Q fever endocarditis in the United States. Mayo Clin. Proc. 79:253-257. [DOI] [PubMed] [Google Scholar]
- 11.Hopkins, R. S., R. A. Jajosky, P. A. Hall, D. A. Adams, F. J. Connor, P. Sharp, W. J. Anderson, R. F. Fagan, J. J. Aponte, D. A. Nitschke, C. A. Worsham, N. Adekoya, and M. H. Chang. 2005. Summary of notifiable diseases—United States, 2003. Morb. Mortal. Wkly. Rep. 52:1-85. [PubMed] [Google Scholar]
- 12.Kim, S. G., E. H. Kim, C. J. Lafferty, and E. Dubovi. 2005. Coxiella burnetii in bulk tank milk samples, United States. Emerg. Infect. Dis. 11:619-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kimbrough, R. C., III, R. A. Ormsbee, M. Peacock, W. R. Rogers, R. W. Bennetts, J. Raaf, A. Krause, and C. Gardner. 1979. Q fever endocarditis in the United States. Ann. Intern. Med. 91:400-402. [DOI] [PubMed] [Google Scholar]
- 14.Kosatsky, T. 1984. Household outbreak of Q-fever pneumonia related to a parturient cat. Lancet ii:1447-1449. [DOI] [PubMed]
- 15.Langley, J. M., T. J. Marrie, A. Covert, D. M. Waag, and J. C. Williams. 1988. Poker players' pneumonia. An urban outbreak of Q fever following exposure to a parturient cat. N. Engl. J. Med. 319:354-356. [DOI] [PubMed] [Google Scholar]
- 16.Lepidi, H., P. Houpikian, Z. Liang, and D. Raoult. 2003. Cardiac valves in patients with Q fever endocarditis: microbiological, molecular, and histologic studies. J. Infect. Dis. 187:1097-1106. [DOI] [PubMed] [Google Scholar]
- 17.Levy, P. Y., M. Drancourt, J. Etienne, J. C. Auvergnat, J. Beytout, J. M. Sainty, F. Goldstein, and D. Raoult. 1991. Comparison of different antibiotic regimens for therapy of 32 cases of Q fever endocarditis. Antimicrob. Agents Chemother. 35:533-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luoto, L. 1960. Report on the nationwide occurrence of Q fever infections in cattle. Public Health Rep. 75:135-140. [PMC free article] [PubMed] [Google Scholar]
- 19.Madariaga, M. G. 2005. Q fever wildlife reservoir. Emerg. Infect. Dis. 11:776-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madariaga, M. G., K. Rezai, G. M. Trenholme, and R. A. Weinstein. 2003. Q fever: a biological weapon in your backyard. Lancet Infect. Dis. 3:709-721. [DOI] [PubMed] [Google Scholar]
- 21.Marrie, T. J. 2000. Coxiella burnetii (Q fever), p. 2043-2050. In R. Dolin (ed.), Mandell, Douglas, and Bennett's principles and practice of infectious diseases, 5th ed., vol. 2. Churchill Livingstone, Philadelphia, Pa. [Google Scholar]
- 22.Maurin, M., A. M. Benoliel, P. Bongrand, and D. Raoult. 1992. Phagolysosomal alkalinization and the bactericidal effect of antibiotics: the Coxiella burnetii paradigm. J. Infect. Dis. 166:1097-1102. [DOI] [PubMed] [Google Scholar]
- 23.Maurin, M., and D. Raoult. 1999. Q fever. Clin. Microbiol. Rev. 12:518-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muhlemann, K., L. Matter, B. Meyer, and K. Schopfer. 1995. Isolation of Coxiella burnetii from heart valves of patients treated for Q fever endocarditis. J. Clin. Microbiol. 33:428-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Musso, D., and D. Raoult. 1995. Coxiella burnetii blood cultures from acute and chronic Q-fever patients. J. Clin. Microbiol. 33:3129-3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palmer, S. R., and S. E. Young. 1982. Q-fever endocarditis in England and Wales, 1975-81. Lancet ii:1448-1449. [DOI] [PubMed] [Google Scholar]
- 27.Pierce, M. A., M. S. Saag, W. E. Dismukes, and C. G. Cobbs. 1986. Q fever endocarditis. Am. J. Med. Sci. 292:104-106. [DOI] [PubMed] [Google Scholar]
- 28.Raoult, D. 1993. Treatment of Q fever. Antimicrob. Agents Chemother. 37:1733-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raoult, D., J. Etienne, P. Massip, S. Iaocono, M. A. Prince, P. Beaurain, S. Benichou, J. C. Auvergnat, P. Mathieu, and P. Bachet. 1987. Q fever endocarditis in the south of France. J. Infect. Dis. 155:570-573. [DOI] [PubMed] [Google Scholar]
- 30.Raoult, D., P. Houpikian, H. T. Dupont, J. M. Riss, J. Arditi-Djiane, and P. Brouqui. 1999. Treatment of Q fever endocarditis: comparison of 2 regimens containing doxycycline and ofloxacin or hydroxychloroquine. Arch. Intern. Med. 159:167-173. [DOI] [PubMed] [Google Scholar]
- 31.Raoult, D., T. Marrie, and J. Mege. 2005. Natural history and pathophysiology of Q fever. Lancet Infect. Dis. 5:219-226. [DOI] [PubMed] [Google Scholar]
- 32.Raoult, D., H. Tissot-Dupont, C. Foucault, J. Gouvernet, P. E. Fournier, E. Bernit, A. Stein, M. Nesri, J. R. Harle, and P. J. Weiller. 2000. Q fever 1985-1998. Clinical and epidemiologic features of 1,383 infections. Medicine (Baltimore) 79:109-123. [DOI] [PubMed] [Google Scholar]
- 33.Sawyer, L. A., D. B. Fishbein, and J. E. McDade. 1988. Q fever in patients with hepatitis and pneumonia: results of laboratory-based surveillance in the United States. J. Infect. Dis. 158:497-498. [DOI] [PubMed] [Google Scholar]
- 34.Shepard, C. C. 1947. An outbreak of Q fever in a Chicago packing house. Am. J. Hyg. 46:185-192. [DOI] [PubMed] [Google Scholar]
- 35.Tissot-Dupont, H., S. Torres, M. Nezri, and D. Raoult. 1999. Hyperendemic focus of Q fever related to sheep and wind. Am. J. Epidemiol. 150:67-74. [DOI] [PubMed] [Google Scholar]
- 36.Topping, N. H., and C. C. Shepard. 1947. Q fever in the United States. JAMA 133:813-815. [DOI] [PubMed] [Google Scholar]
- 37.Turck, W. P., G. Howitt, L. A. Turnberg, H. Fox, M. Longson, M. B. Matthews, and R. Das Gupta. 1976. Chronic Q fever. Q. J. Med. 45:193-217. [PubMed] [Google Scholar]
- 38.Wisniewski, H. J., and E. R. Krumbiegel. 1970. Q fever in the Milwaukee area. I. Q fever in Milwaukee area cattle. Arch. Environ. Health 21:58-62. [DOI] [PubMed] [Google Scholar]
- 39.Zhang, G., and J. E. Samuel. 2004. Vaccines against Coxiella infection. Exp. Rev. Vaccines 3:577-584. [DOI] [PubMed] [Google Scholar]