Abstract
A novel PCR-based reverse hybridization method Genotype MTBDR assay (Hain Lifescience GmbH, Nehren, Germany) was evaluated for rapid detection of rifampin (RIF) and isoniazid (INH) resistance in Turkish Mycobacterium tuberculosis isolates. The Genotype MTBDR assay is designed to detect mutations within the 81-bp hotspot region of rpoB and mutations at katG codon 315. A total of 41 RIF-resistant M. tuberculosis isolates with rpoB mutations that were previously tested by the INNO-LiPA Rif.TB kit and also characterized by DNA sequencing were included in the study. Thirty-seven of these isolates were also resistant to INH. RIF resistance was correctly identified in 39 of 41 isolates (95.1%) with the Genotype MTBDR assay probes specific for these mutations. One isolate with a Gln-490-His mutation and another one with a CGG insertion between codons 514 and 515 were identified as RIF sensitive by the Genotype MTBDR assay. While the INNO-LiPA Rif.TB kit was able to determine the CGG insertion between codons 514 and 515, the Gln-490-His mutation outside the 81-bp hotspot region was not detected by the INNO-LiPA Rif.TB kit. These isolates had MICs of ≥32 μg/ml for RIF. The Genotype MTBDR assay also correctly identified 27 of 37 INH-resistant isolates (73%) with mutations in katG codon 315. In conclusion, the Genotype MTBDR assay may be useful for the rapid diagnosis of the most common mutations found in multidrug-resistant M. tuberculosis strains. However, the test results should always be confirmed with phenotypic methods.
Mycobacterium tuberculosis remains one of the most significant causes of death from an infectious agent. The incidence of pulmonary tuberculosis in Turkey is nearly 30 per 100,000 population (2, 26). In the Aegean region, 8.2% of M. tuberculosis strains isolated between 1999 and 2001 were found to be resistant to rifampin (RIF). During the same period, the incidence of resistance to both RIF and isoniazid (INH) was 6.8% (8).
Collectively, DNA sequencing studies demonstrate that more than 95% of RIF-resistant M. tuberculosis strains have a mutation within the 81-bp hotspot region of the rpoB gene (5, 12, 25). In contrast, the mutations causing INH resistance are located in several regions (28). Approximately, 34.6 to 94.3% of INH-resistant strains have been found to contain mutations in codon 315 of the katG gene (9, 10, 15, 18, 27), 2.9 to 21.5% contain mutations in the inhA promoter region (9, 10, 18, 27), and an additional 2 to 11.5% have mutations in the ahpC-oxyR intergenic region (9, 10, 27).
Several molecular methods have been developed in recent years to evaluate the rpoB and katG genes for RIF and INH resistance, including DNA sequencing, line probe assay, and analysis with DNA microarrays. Molecular assays have been established to allow the prediction of drug resistance in clinical M. tuberculosis isolates within one working day and potentially are the most rapid methods for the detection of drug resistance (5, 6, 9, 11, 12). The Genotype MTBDR assay (Hain Lifescience GmbH, Nehren, Germany) is a novel kit-based method for the detection of the most common mutations in the M. tuberculosis katG and rpoB genes (9, 11).
The aim of this study was to determine the performance of the Genotype MTBDR assay for rapid detection of RIF and INH resistance in Turkish M. tuberculosis isolates of known rpoB sequence and INNO-LiPA Rif.TB patterns. In the first step, rpoB and katG mutations were determined by the Genotype MTBDR assay. The results obtained by the Genotype MTBDR assay were then compared with the results obtained by DNA sequencing, INNO-LiPA Rif.TB, and phenotypic susceptibility testing.
MATERIALS AND METHODS
M. tuberculosis isolates.
A total of 41 RIF-resistant M. tuberculosis isolates, 37 of which were multidrug resistant, were included in the study. Mycobacterium tuberculosis strains were obtained from patients living in the Aegean region of Turkey between 2000 and 2004. Drug susceptibility testing (DST) for RIF, INH, streptomycin, and ethambutol had been previously performed with the proportional method on 7H10 medium according to the criteria of the CLSI (formerly NCCLS) (17). Mutations in the rpoB gene for each isolate had also been determined by DNA sequencing and INNO-LiPA Rif.TB previously.
Determination of MICs for RIF and INH.
All isolates resistant to 1 μg of RIF per ml and resistant to 0.2 μg of INH per ml were tested on 7H10 medium, with 2-, 4-, 8-, 16-, and 32-μg/ml concentrations of RIF and with 1-, 2-, and 4-μg/ml concentrations of INH, respectively.
Genotypic characterization.
DNA sequencing was performed with an automated DNA sequencer (model 310; Applied Biosystems, Foster City, Calif.). The katG and inhA genes were amplified by PCR using primers described previously and then sequenced by using the same primers (18, 24).
INNO-LiPA Rif.TB assay.
The INNO-LiPA Rif.TB (Innogenetics N.V., Ghent, Belgium) test was used according to the instructions of the manufacturer. The RIF resistance-determining region of the rpoB gene was amplified with specific biotin-labeled primers. The biotinylated PCR product was then denatured and hybridized to a strip with 10 specific oligonucleotide probes. M. tuberculosis was detected in a sample by use of the M. tuberculosis complex-specific probe. The reactivities of an amplified fragment with the S-type probes for the wild type (probes S1 through S5) were used to detect the mutations that lead to RIF resistance in M. tuberculosis. Furthermore, four probes (R-type probes) were specifically designed to hybridize to the sequences of the four most frequently observed mutations: R2 (D516V), R4a (H526Y), R4b (H526D), and R5 (S531L).
In conclusion, when all of the wild-type S probes gave a positive signal and all the R probes reacted negatively, the M. tuberculosis isolate was considered susceptible to RIF. When at least one negative signal was obtained with the wild-type S probes, the isolate was considered RIF resistant (INNO-LiPA Rif.TB S patterns). When the resistance to RIF was due to one of the four most frequently observed mutations described above, a positive reaction was obtained with one of the four R probes and was always accompanied by a negative reaction with the corresponding S probe (INNO-LiPA Rif.TB R patterns).
Genotype MTBDR assay.
The Genotype MTBDR assay (Hain Lifescience GmbH, Nehren, Germany) was used according to the instructions of the manufacturer. Briefly, for DNA preparation, 0.5 ml of actively growing (1 to 2 weeks old) liquid cultures (MB/BacT; bioMérieux, Marcy l'Etoile, France) was used. Liquid cultures were centrifuged at 10,000 × g for 15 min. Supernatants were discarded and suspended in 100 μl of distilled water, boiled for 20 min, sonicated for 15 min, and then centrifuged at 10,000 × g for 5 min. Supernatants were used for PCR amplification. For amplification, 35 μl of primer-nucleotide mix (provided with the kit), amplification buffer containing 2.5 mM MgCl2, 1.25 U of FastStart Taq polymerase (Roche Molecular Diagnostics, Mannheim, Germany), and 5 μl of supernatant in a final volume of 50 μl were used. The amplification protocol consisted of 10 min of denaturing at 95°C; 10 cycles of 30 s at 95°C and 120 s at 58°C; 20 additional cycles of 25 s at 95°C, 40 s at 53°C, and 40 s at 70°C; and a final extension at 70°C for 8 min. PCR products were analyzed in 1.5% agarose gel for the control of incomplete or marginal amplification. The biotinylated PCR products were then denatured and hybridized to a strip with specific oligonucleotide probes. Hybridization and detection were performed in an automated washing and shaking device (TwinCubator; Hain Lifescience GmbH, Nehren, Germany). The program was started after 20 μl of the amplification products was mixed with 20 μl of denaturing reagent (provided with the kit) for 5 min in separate troughs of a plastic well. Following the addition of 1 ml of prewarmed hybridization buffer, membrane strips were placed in each trough. The hybridization procedure is performed at 45°C for 0.5 h and is followed by two washing steps. For colorimetric detection of hybridized amplicons, streptavidin conjugated with alkaline phosphatase and substrate buffer was added. After final washing, strips were air dried.
Each strip contains 17 probes, including amplification and hybridization controls. M. tuberculosis was detected in a sample by the use of the M. tuberculosis complex-specific probe. The rpoB- and katG-specific regions were detected by rpoB and katG control probes, respectively. The reactivities of an amplified fragment with the five rpoB wild-type probes (rpoB WT1 through rpoB WT5) and one katG wild-type probe were used to detect the mutations that lead to RIF and INH resistance in M. tuberculosis. Furthermore, six probes (mutant probes) were specifically designed to hybridize to the sequences of the four most frequently observed rpoB and two katG mutations: rpoB D516V, rpoB H526Y, rpoB H526D, rpoB S531L, katG S315T1, and katG S315T2.
In conclusion, when all of the wild-type probes gave a positive signal and all of the mutant probes reacted negatively, the M. tuberculosis isolate was considered susceptible to RIF and INH. When at least one negative signal was obtained with the rpoB wild-type probes, the isolate was considered resistant to RIF, and same was true for the katG wild-type probe. When the resistance to RIF or INH was due to one of the six most frequently observed mutations described above, a positive reaction was obtained with at least one of the six mutant probes and was always accompanied by a negative reaction with the corresponding wild-type probe.
RESULTS AND DISCUSSION
Rifampin resistance was correctly identified in 22 of 41 isolates (53.7%) with the Genotype MTBDR assay's rpoB mutant probes specific for these mutations. Seventeen of 41 RIF-resistant isolates (41.5%) yielded hybridization patterns, with at least one negative signal obtained with the wild-type rpoB probes. The codons most frequently involved in mutations were codon 531 (56.1%) and codon 526 (17.1%). Nineteen (46.3%) isolates carried the most common mutation, Ser-531-Leu. Two RIF-resistant isolates were identified as RIF sensitive by the Genotype MTBDR assay. Compared to conventional DST, the rate of concordance of the Genotype MTBDR assay results for the detection of RIF resistance was 95.1% (Table 1).
TABLE 1.
Comparison of Genotype MTBDR test results with DNA sequencing data, INNO-LiPA Rif.TB profiles, and the MICs of RIF in Turkish RIF-resistant isolates (n = 41) of M. tuberculosisa
| Nucleotide/amino acid change(s) | MTBDR profile/result | LiPA profile/result | MIC (μg/ml) (no. of isolates) | No. (%) of isolates |
|---|---|---|---|---|
| 531-TCG→TTG/Ser→Leu | Mut3/resistant | R5/resistant | >32 (17), 32 (2) | 19 (46.3) |
| 531-TCG→TGG/Ser→Trp | ΔWT5/resistant | ΔS5/resistant | >32 (4) | 4 (9.8) |
| 533-CTG→CCG/Leu→Pro | ΔWT5/resistant | ΔS5/resistant | 4 (1) | 1 (2.4) |
| 526-CAC→TAC/His→Tyr | Mut2a/resistant | R4a/resistant | >32 (2) | 2 (4.9) |
| 526-CAC→CGC/His→Arg | ΔWT4/resistant | ΔS4/resistant | >32 (4) | 4 (9.8) |
| 526-CAC→TGC/His→Cys | ΔWT4/resistant | ΔS4/resistant | 8 (1) | 1 (2.4) |
| 522-TCG→TGG/Ser→Trp | ΔWT3/resistant | ΔS3/resistant | >32 (2) | 2 (4.9) |
| 516-GAC→GTC/Asp→Val | Mut1/resistant | R2/resistant | 8 (1) | 1 (2.4) |
| 516-GAC→TAC/Asp→Tyr | ΔWT2/resistant | ΔS2/resistant | 8 (2) | 2 (4.9) |
| 513-CAA→CCA/Gln→Pro | ΔWT1/resistant | ΔS1/resistant | >32 (1) | 1 (2.4) |
| 513-CAA→GAA/Gln→Glu | ΔWT1/resistant | ΔS1/resistant | >32 (1) | 1 (2.4) |
| 515-ATG→ATC/Met→Ile | ΔWT2, ΔWT5/resistant | ΔS2, ΔS5/resistant | 8 (1) | 1 (2.4) |
| 533 CTG→CCG/Leu→Pro | ||||
| CGG insertion between 514 and 515/Arg | S/sensitive | ΔS1, ΔS2/resistant | 32 (1) | 1 (2.4) |
| 490-CAG→CAT/Gln→His | S/sensitive | S/sensitive | >32 (1) | 1 (2.4) |
Mut1, Mut2a, Mut3, R2, R4a, and R5 indicate the specific point mutation patterns in the Genotype MTBDR and INNO-LiPA Rif.TB assays, respectively. Δ indicates the negative signal at any of the wild-type probes without a positive signal at the corresponding mutant probe.
Of the two isolates incorrectly identified as RIF sensitive by the Genotype MTBDR assay, one had an Gln-490-His mutation and the other isolate had a CGG insertion between codons 514 and 515. While the Gln-490-His mutation, which was outside the 81-bp hotspot region, was not detected by either Genotype MTBDR or INNO-LiPA Rif.TB, the CGG insertion between codons 514 and 515 was detected by INNO-LiPA Rif.TB. This isolate gave a negative signal with the wild-type rpoB probes S1 and S2 and four mutant probes, R2, R4a, R4b, and R5, but was positive with the wild-type rpoB probes S3, S4, and S5 by INNO-LiPA Rif.TB. The Genotype MTBDR assay has a gap between the wild-type 1 and wild-type 2 probes, possibly lacking the codon 514 and 515. In contrast, INNO-LiPA Rif.TB has a overlapping region between the wild-type probes S1 and S2, including codon 514 and 515. The reason for this problem may be the gap between the wild-type 1 and wild-type 2 probes of the Genotype MTBDR assay. This isolate also had an ACA mutation in codon 315 of the katG gene and was detected correctly by the katG T2 (S315T2) probe of the Genotype MTBDR assay (Table 1 and Fig. 1 and 2). One isolate with a double mutation at codon 515 and codon 533 gave negative signals with the wild-type rpoB probes S2 and S5 by both assays. It is known that marginal or incomplete amplification could cause especially more than one negative signal, however, in the present study, the two isolates which had two negative signals with the wild-type rpoB probes also showed DNA sequencing profiles consistent with the Genotype MTBDR assay and/or INNO-LiPA Rif.TB assay pattern.
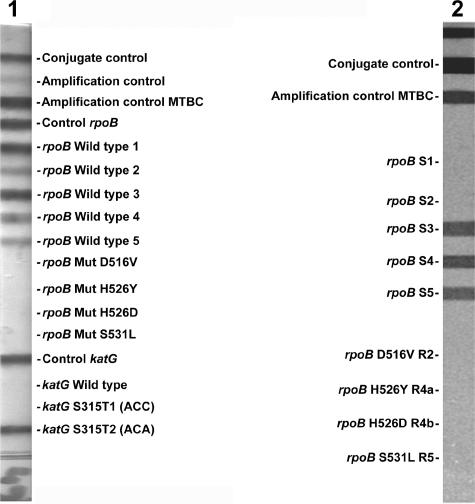
FIG. 1.
Locations of Genotype MTBDR and INNO-LiPA Rif.TB probes within the 81-bp hotspot cluster of the rpoB gene.
FIG. 2.
Representative results for patterns of the isolate which had a CGG insertion between codons 514 and 515 obtained with the Genotype MTBDR assay and INNO-LiPA Rif.TB assay. The positions of the oligonucleotides and the marker lines are given. The specificity and targeted genes of the lines are shown from top to bottom as follows. The Genotype MTBDR assay (lane 1): conjugate control; amplification control (23S rRNA); M. tuberculosis complex-specific control (23S rRNA); control for rpoB amplification; rpoB wild-type probes located in the 81-bp hotspot region 5 to 9; rpoB mutant (Mut) probes with mutations in codons 516, 526, and 531; control for katG amplification; katG codon 315 wild-type probe; katG codon 315 mutation probes (sequences in parentheses). The INNO-LiPA Rif.TB assay (lane 2): conjugate control; M. tuberculosis complex-specific control; rpoB wild-type probes located in the 81-bp hotspot region 3 to 7; rpoB mutant probes with mutations in codons 516, 526, and 531. In lane 1, the isolate was positive with the control probes, wild-type rpoB probes, and katG S315T2 (ACA) probe and evaluated as RIF sensitive and INH resistant by the Genotype MTBDR assay. In lane 2, the isolate was positive with the control probes and wild-type rpoB probes S3, S4, and S5 but negative with the wild-type rpoB probes S1 and S2 and evaluated as RIF resistant by INNO-LiPA Rif.TB assay.
The DNA sequencing studies demonstrate that more than 95% of RIF-resistant strains have a mutation in a hotspot region of the rpoB gene. Moreover, previous studies have generally revealed a strong correlation between certain rpoB mutations and the MICs of RIF (3, 14). In concordance with previous reports, in this study, it was found that the isolates with MICs of RIF of ≤8 μg/ml had Asp516Val or Asp516Tyr substitutions, whereas isolates with MICs of RIF of ≥32 μg/ml had Ser531Leu, His526Tyr, or His526Arg mutations (Table 1). These findings suggest that the detection of mutation in the rpoB gene is not only a useful strategy for diagnosis of drug resistance to RIF in the M. tuberculosis complex but also a useful tool for the detection of the level of RIF resistance.
With regard to INH resistance, a mutation in katG codon 315 was detected in 27 of the 37 INH-resistant isolates (73%) but in none of the four susceptible strains. All distinct nucleotide exchanges in katG codon 315 of INH-resistant strains could be verified by hybridization to the oligonucleotide probe targeting the particular mutations: 25 strains carried the ACC (S315T1) mutation and two carried the ACA (S315T2) mutation. Ten of the 37 INH-resistant strains showed a wild-type hybridization pattern in the Genotype MTBDR assay (Table 2). Sequencing analysis revealed that one of these had mutations (C→T) in the ribosome-binding site region of inhA.
TABLE 2.
Comparison of Genotype MTBDR test results with DNA sequencing data and the MICs of INH in Turkish INH-resistant isolates of M. tuberculosis (n = 37)
| Nucleotide/amino acid change(s) | MTBDR profile/result | MIC (μg/ml) (no. of isolates) | No. (%) of isolates |
|---|---|---|---|
| katG 315-AGC→ACC/Ser→Thr | katG T1/resistant | >4 (25) | 25 (67.6) |
| katG 315-AGC→ACA/Ser→Thr | katG T2/resistant | >4 (2) | 2 (5.4) |
| inhA 209 C→T | katG WTa/sensitive | >4 (1) | 1 (2.7) |
| No mutation | katG WT/sensitive | >4 (2), 2 (1), <1 (6) | 9 (24.3) |
WT, wild type.
Presumably, the remaining nine strains carry a mutation in other genomic regions not analyzed in this investigation, such as ahpC, kasA, iniA, iniB, iniC, efpA, furA, or ndh (20, 27).
Of the 37 INH-resistant isolates, 31 had MICs of INH of >1 μg/ml. Of these 31 isolates, 27 (87.1%) had a mutation in katG codon 315 (Table 2). The previous studies suggest that mutations in katG codon 315 are associated with high levels (>1 μg/ml) of INH resistance (1, 4, 13, 27), which was also observed in our study. Mutations in the upstream region of inhA result in an increase of InhA expression, thereby elevating the drug target levels and producing INH resistance via a titration mechanism associated with various levels of INH resistance (19). In the current study, one strain had an inhA C→T mutation with a MIC of INH of >4 μg/ml. Compared to DST, the rate of concordance of the Genotype MTBDR assay results for the detection of low (0.2 μg/ml ≤ MIC < 1 μg/ml) and high levels of INH resistance were 73% and 87.1%, respectively.
Recently, novel molecular diagnostic methods based on the PCR and a reverse hybridization procedure, such as INNO-LiPA Rif.TB assay and Genotype MTBDR assay, have been evaluated for the detection of rpoB mutations (5-7, 9, 11, 23). Both the Genotype MTBDR and INNO-LiPA Rif.TB have been proven to be robust and reproducible, and the results are easy to interpret without the extensive expert knowledge required for the interpretation of real-time PCR data or DNA sequencing data. Furthermore, they can easily be implemented in routine workflows (21, 22). The INNO-LiPA Rif.TB assay is restricted to the detection of RIF resistance. In contrast, the Genotype MTBDR assay allows the rapid and specific detection of the most frequent mutations leading to INH and RIF resistance in clinical M. tuberculosis isolates. However, because of the probe design, the Genotype MTBDR cannot detect some rare mutations, such as the CGG insertion between codons 514 and 515 within the 81-bp region of the rpoB gene.
In earlier reports (9, 11), sensitivities of the Genotype MTBDR were reported as 99% (102 of 103) and 96.4% (27 of 28) in RIF-resistant strains and 88.4% (91 of 103) and 84.4% (27 of 32) in INH-resistant strains, respectively. While Hillemann et al. (9) detected a mutation outside the 81-bp rpoB region, Makinen et al. (11) detected a mutation in the 81-bp rpoB region in RIF-resistant isolates incorrectly identified as RIF sensitive by the Genotype MTBDR. In concordance with previous reports, in the present study, the Genotype MTBDR was also able to detect a genetic alteration in 39 (95.1%) of the 41 RIF-resistant strains and 27 (87.1%) of the 31 high-level INH-resistant strains. The INNO-LiPA Rif.TB assay and Genotype MTBDR assay could incorrectly identify silent or neutral mutations that are phenotypically sensitive as resistant. However, such mutations are unlikely to be a common problem and these assays are highly sensitive and specific for the detection of RIF and INH resistance (9, 11, 16). In conclusion, both assays may be useful for the rapid screening of M. tuberculosis isolates obtained from patients suspected of having multidrug-resistant tuberculosis, but the Genotype MTBDR assay has the advantage of being able to detect resistance to both INH and RIF simultaneously. However, the test results must always be confirmed by the phenotypic methods.
Acknowledgments
We thank Makro Corp. for providing the Genotype MTBDR assay.
REFERENCES
- 1.Abate, G., S. E. Hoffner, V. O. Thomsen, and H. Miorner. 2001. Characterization of isoniazid-resistant strains of Mycobacterium tuberculosis on the basis of phenotypic properties and mutations in katG. Eur. J. Clin. Microbiol. Infect. Dis. 20:329-333. [DOI] [PubMed] [Google Scholar]
- 2.Aktas, E., R. Durmaz, D. Yang, and Z. Yang. 2005. Molecular characterization of isoniazid and rifampin resistance of Mycobacterium tuberculosis clinical isolates from Malatya, Turkey. Microb. Drug Resist. 11:94-99. [DOI] [PubMed] [Google Scholar]
- 3.Bodmer, T., G. Zurcher, P. Imboden, and A. Telenti. 1995. Mutation position and type of substitution in the β-subunit of the RNA polymerase influence in-vitro activity of rifamycins in rifampicin-resistant Mycobacterium tuberculosis. J. Antimicrob. Chemother. 35:345-348. [DOI] [PubMed] [Google Scholar]
- 4.Cardoso, R. F., R. C. Cooksey, G. P. Morlock, P. Barco, L. Cecon, F. Forestiero, C. Q. Leite, D. N. Sato, M. de Lourdes Shikama, E. M. Mamizuka, R. D. Hirata, and M. H. Hirata. 2004. Screening and characterization of mutations in isoniazid-resistant Mycobacterium tuberculosis isolates obtained in Brazil. Antimicrob. Agents Chemother. 48:3373-3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavusoglu, C., S. Hilmioglu, S. Guneri, and A. Bilgic. 2002. Characterization of rpoB mutations in rifampin-resistant clinical isolates of Mycobacterium tuberculosis from Turkey by DNA sequencing and line probe assay. J. Clin. Microbiol. 40:4435-4438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cirillo, D. M., F. Piana, L. Frisicale, M. Quaranta, A. Riccabone, V. Penati, P. Vaccarino, and G. Marchiaro. 2004. Direct rapid diagnosis of rifampicin-resistant Mycobacterium tuberculosis infection in clinical samples by line probe assay (INNO LiPA Rif.TB). New Microbiol. 27:221-227. [PubMed] [Google Scholar]
- 7.Cooksey, R. C., G. P. Morlock, S. Glickman, and J. T. Crawford. 1997. Evaluation of a line probe assay kit for characterization of rpoB mutations in rifampin-resistant Mycobacterium tuberculosis isolates from New York City. J. Clin. Microbiol. 35:1281-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guneri, S., I. Unsal, A. Oztop, M. Erkut, V. Avkan Oguz, and R. Cakmak. 2002. Antituberculosis drug resistance in Aegean Region. Toraks Derg. 3:77-78. [PubMed] [Google Scholar]
- 9.Hillemann, D., M. Weizenegger, T. Kubica, E. Richter, and S. Niemann. 2005. Use of the Genotype MTBDR assay for rapid detection of rifampin and isoniazid resistance in Mycobacterium tuberculosis complex isolates. J. Clin. Microbiol. 43:3699-3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim, S. Y., Y. J. Park, W. I. Kim, S. H. Lee, C. Ludgerus Chang, S. J. Kang, and C. S. Kang. 2003. Molecular analysis of isoniazid resistance in Mycobacterium tuberculosis isolates recovered from South Korea. Diagn. Microbiol. Infect. Dis. 47:497-502. [DOI] [PubMed] [Google Scholar]
- 11.Makinen, J., H. J. Marttila, M. Marjamaki, M. K. Viljanen, and H. Soini. 2006. Comparison of two commercially available DNA line probe assays for detection of multidrug-resistant Mycobacterium tuberculosis. J. Clin. Microbiol. 44:350-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mani, C., N. Selvakumar, S. Narayanan, and P. R. Narayanan. 2001. Mutations in the rpoB gene of multidrug-resistant Mycobacterium tuberculosis clinical isolates from India. J. Clin. Microbiol. 39:2987-2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marttila, H. J., H. Soini, E. Eerola, E. Vyshnevskaya, B. I. Vyshnevskiy, T. F. Otten, A. V. Vasilyef, and M. K. Viljanen. 1998. A Ser315Thr substitution in KatG is predominant in genetically heterogeneous multidrug-resistant Mycobacterium tuberculosis isolates originating from the St. Petersburg area in Russia. Antimicrob. Agents Chemother. 42:2443-2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moghazeh, S. L., X. Pan, T. Arain, C. K. Stover, J. M. Musser, and B. N. Kreiswirth. 1996. Comparative antimycobacterial activities of rifampin, rifapentine, and KRM-1648 against a collection of rifampin-resistant Mycobacterium tuberculosis isolates with known rpoB mutations. Antimicrob. Agents Chemother. 40:2655-2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mokrousov, I., O. Narvskaya, T. Otten, E. Limeschenko, L. Steklova, and B. Vyshnevskiy. 2002. High prevalence of KatG Ser315Thr substitution among isoniazid-resistant Mycobacterium tuberculosis clinical isolates from Northwestern Russia, 1996 to 2001. Antimicrob. Agents Chemother. 46:1417-1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morgan, M., S. Kalantri, L. Flores, and M. Pai. 2005. A commercial line probe assay for the rapid detection of rifampicin resistance in Mycobacterium tuberculosis: a systematic review and meta-analysis. BMC Infect. Dis. 5:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Committee for Clinical Laboratory Standards. 2000. Susceptibility testing of mycobacteria, nocardia, and other aerobic actinomycetes; tentative standard M24-T2. National Committee for Clinical Laboratory Standards, Wayne, Pa. [PubMed]
- 18.Nikolayevsky, V., T. Brown, Y. Balabanova, M. Ruddy, I. Fedorin, and F. Drobniewski. 2004. Detection of mutations associated with isoniazid and rifampin resistance in Mycobacterium tuberculosis isolates from Samara Region, Russian Federation. J. Clin. Microbiol. 42:4498-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramaswamy, S., and J. M. Musser. 1998. Molecular genetic basis of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update. Tuberc. Lung Dis. 79:3-29. [DOI] [PubMed] [Google Scholar]
- 20.Ramaswamy, S. V., R. Reich, S. J. Dou, L. Jasperse, X. Pan, A. Wanger, T. Quitugua, and E. A. Graviss. 2003. Single nucleotide polymorphisms in genes associated with isoniazid resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 47:1241-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richter, E., M. Weizenegger, A. M. Fahr, and S. Rüsch-Gerdes. 2004. Usefulness of the Genotype MTBC assay for differentiating species of the Mycobacterium tuberculosis complex in cultures obtained from clinical specimens. J. Clin. Microbiol. 42:4303-4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Richter, E., M. Weizenegger, S. Rüsch-Gerdes, and S. Niemann. 2003. Evaluation of Genotype MTBC assay for differentiation of clinical Mycobacterium tuberculosis complex isolates. J. Clin. Microbiol. 41:2672-2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossau, R., H. Traore, H. De Beenhouwer, W. Mijs, G. Jannes, P. De Rijk, and F. Portaels. 1997. Evaluation of the INNO-LiPA Rif. TB assay, a reverse hybridization assay for the simultaneous detection of Mycobacterium tuberculosis complex and its resistance to rifampin. Antimicrob. Agents Chemother. 41:2093-2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Telenti, A., N. Honoré, C. Bernasconi, J. March, A. Ortega, H. E. Takiff, and S. T. Cole. 1997. Genotyping assessment of isoniazid and rifampin resistance in Mycobacterium tuberculosis: a blind study at reference laboratory level. J. Clin. Microbiol. 35:719-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Telenti, A., P. Imboden, F. Marchesi, D. Lowrie, S. Cole, M. J. Colston, L. Matter, K. Schopfer, and T. Bodmer. 1993. Detection of rifampicin-resistance mutations in Mycobacterium tuberculosis. Lancet 341:647-650. [DOI] [PubMed] [Google Scholar]
- 26.Tuberculosis Service. 2003. A guide for tuberculosis control in Turkey. Ministry of Health, Ankara, Turkey.
- 27.Zhang, M., J. Yue, Y. P. Yang, H. M. Zhang, J. Q. Lei, R. L. Jin, X. L. Zhang, and H. H. Wang. 2005. Detection of mutations associated with isoniazid resistance in Mycobacterium tuberculosis isolates from China. J. Clin. Microbiol. 43:5477-5482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang, Y., and A. Telenti. 2000. Genetics of drug resistance in Mycobacterium tuberculosis, p. 235-251. In G. F. Hatfull and W. R. Jacobs, Jr. (ed.), Molecular genetics of mycobacteria. ASM Press, Washington, D.C.