Abstract
Bronchoalveolar lavage (BAL) is widely used for evaluation of patients with suspected invasive pulmonary aspergillosis (IPA). However, the diagnostic yield of BAL for detection of IPA by culture and direct examination is limited. Earlier diagnosis may be facilitated by assays that can detect Aspergillus galactomannan antigen or DNA in BAL fluid. We therefore characterized and compared the diagnostic yields of a galactomannan enzyme immunoassay (GM EIA), quantitative real-time PCR (qPCR), and quantitative cultures in experiments using BAL fluid from neutropenic rabbits with experimentally induced IPA defined as microbiologically and histologically evident invasion. The qPCR assay targeted the rRNA gene complex of Aspergillus fumigatus. The GM EIA and qPCR assay were characterized by receiver operator curve analysis. With an optimal cutoff of 0.75, the GM EIA had a sensitivity and specificity of 100% in untreated controls. A decline in sensitivity (92%) was observed when antifungal therapy (AFT) was administered. The optimal cutoff for qPCR was a crossover of 36 cycles, with sensitivity and specificity of 80% and 100%, respectively. The sensitivity of qPCR also decreased with AFT to 50%. Quantitative culture of BAL had a sensitivity of 46% and a specificity of 100%. The sensitivity of quantitative culture decreased with AFT to 16%. The GM EIA and qPCR assay had greater sensitivity than culture in detection of A. fumigatus in BAL fluid in experimentally induced IPA (P ± 0.04). Use of the GM EIA and qPCR assay in conjunction with culture-based diagnostic methods applied to BAL fluid could facilitate accurate diagnosis and more-timely initiation of specific therapy.
Invasive pulmonary aspergillosis (IPA) is a major cause of morbidity and mortality in immunocompromised patients (7-9, 13, 14, 18, 27). Mortality rates of this severe infection range from 30% to 90% in neutropenic patients (9, 10, 15, 20). Accurate diagnosis of IPA routinely relies upon bronchoalveolar lavage (BAL) as a standard of care in assessing immunocompromised patients (1, 12). However, current culture-based methods for evaluation of BAL fluid may have low sensitivity (3, 19, 32, 33). Other methods, such as tissue biopsy, are often not optimal due to the fragile condition of the patient with respect to sustaining an invasive procedure. Early diagnosis of IPA remains difficult. Improved prognosis for IPA requires early diagnosis (40). The development of nonculture and noninvasive methods may facilitate an early diagnosis of IPA (5, 22, 25).
The sandwich enzyme immunoassay (EIA) based on the detection of the Aspergillus antigen galactomannan (GM) (3, 4, 21, 38) and real-time PCR methods (25, 34) for the detection of Aspergillus-specific DNA are encouraging alternatives to biopsy and culture. However, the sensitivity and optimal interpretive cutoff values of the GM EIA in studies using BAL fluid are not well defined (4, 34, 38). Although quantitative real-time PCR (qPCR) assays have been developed for the detection of IPA (16, 26, 34, 35), their diagnostic sensitivity and specificity for IPA in BAL fluid are not well understood. There is also a need for methods that will complement each other for the early detection of aspergillosis. We therefore hypothesized that the GM EIA and qPCR assay would be more sensitive than culture methods in detection of A. fumigatus in BAL fluid. In order to test this hypothesis, we studied the application of a qPCR assay for the detection of Aspergillus DNA in conjunction with the GM EIA for the detection of GM antigen in BAL fluid from experimentally induced IPA in persistently neutropenic rabbits. Receiver operator curves (ROC) were constructed for both GM EIA and qPCR. These curves were then used to define cutoff, sensitivity, and specificity values that optimized the test performance of each assay. Both methods were studied using a well-established persistently neutropenic rabbit model of IPA (11, 28, 42). We further investigated the impact of different antifungal modalities, including ravuconazole, micafungin, and deoxycholate amphotericin B, on the sensitivity and specificity of each assay.
MATERIALS AND METHODS
Animal model of IPA. (i) Animals.
Healthy female New Zealand White rabbits (Hazleton Research Products, Inc., Denver, PA) weighing 2.6 to 3.5 kg at the time of inoculation were used in all experiments. Rabbits were monitored under conditions of humane care and use in facilities accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International and according to National Institutes of Health guidelines for animal care and guidelines of the National Research Council (6). Vascular access was established in each rabbit by the surgical placement of a silastic tunneled central venous catheter as described in a previous publication (41).
(ii) Organism and inoculation.
Invasive pulmonary aspergillosis was established as described elsewhere (11). Briefly, Aspergillus fumigatus (A. fumigatus isolate NIH 4215, ATCC MYA-1163) obtained from a fatal case of IPA was used in all experiments. The concentration was adjusted to give each rabbit a predetermined endotracheal inoculum of 1 × 108 to 1.25 × 108 conidia of A. fumigatus in a volume of 250 to 350 μl. The concentration of the inoculum was confirmed by plating serial dilutions on 5% Sabouraud glucose agar plates (Bioworks, Inc., Baltimore, MD). Inoculation was performed on day 2 of the experiments under conditions of general anesthesia. The A. fumigatus inoculum was administered endotracheally under direct visualization with a tuberculin syringe attached to a 16 gauge, 5 in. Teflon catheter (Becton Dickinson Infusion Therapy Systems Inc., Sandy, UT).
(iii) Immunosuppression and maintenance of neutropenia.
Immunosuppression and neutropenia were established as previously described (28).
(iv) Antifungal compounds and treatment groups.
In order to study the effect of antifungal therapy on the possible diminution of sensitivity of GM EIA, qPCR, and culture, we studied compounds from each major class: triazoles, echinocandins, and polyenes. Antifungal therapy with ravuconazole (BMS-379224; Bristol-Myers Squibb Pharmaceutical Research Institute, Princeton, NJ) was administered at dosages of 5 to 10 mg/kg of body weight. Micafungin (Fujisawa Pharmaceutical Co., Ltd., Osaka, Japan) was administered at dosages of 0.5 to 2 mg/kg. Deoxycholate amphotericin B (Fungizone; Bristol-Myers Squibb Company, Princeton, NJ) was administered at 1 mg/kg. Antifungal therapy was administered for 12 days starting 24 h after endotracheal inoculation of A. fumigatus conidia.
Rabbits were euthanized according to Animal Care and Use Committee-approved prespecified humane end points by intravenous administration of pentobarbital (65 mg of pentobarbital sodium/kg; pentobarbital sodium was in the form of 0.5 ml of euthanasia solution) (Beuthanasia-D special; Schering-Plough Animal Health Corp., Union, NJ) at the end of each experiment. BAL was then performed at the time of postmortem examination.
(v) Tissue quantification of pulmonary aspergillosis.
Rabbits were considered to have invasive pulmonary aspergillosis when pulmonary lesions, histology, and quantitative culture of lung tissue were detected as described previously (28).
Diagnostic assays. (i) Bronchoalveolar lavage and BAL fluid fungal cultures.
A BAL was performed on each postmortem resected lung preparation by the instillation and subsequent withdrawal of 10 ml of sterile normal saline solution into the clamped trachea with a sterile 12 ml syringe. This process was repeated for a total infusion of 20 ml of normal saline. The lavage material was then centrifuged for 10 min at 200 × g. The supernatant was discarded, leaving 2 ml of BAL fluid in which the pellet was then resuspended. A 100 μl volume of this fluid and 100 μl of a dilution (10−1) were cultured on Sabouraud glucose agar plates and incubated at 37°C for the first 24 h and then at room temperature for another 24 h. CFU per ml were counted, and log CFU/ml was calculated. These samples were obtained from animals used for other primary studies (29, 30). BAL samples were stored at −70°C and later studied for expression of GM antigen and detection of nucleic acid.
(ii) EIA for detection of galactomannan in BAL fluid and serum.
GM antigen levels were determined by the Platelia Aspergillus EIA one-stage immunoenzymatic sandwich microplate assay method (Bio-Rad Laboratories, Redmond, WA). The assay was performed according to the manufacturer's directions. The assay uses the rat monoclonal antibody EBA-2, which is directed against the Aspergillus GM molecule (36). The optical absorbance of specimens and controls was determined by use of a microplate spectrophotometer equipped with 450 nm and 620 nm filters (Multiscan MMC/340; Titertek, Huntsville, AL).
Quantitative real-time PCR assay. (i) DNA isolation from BAL fluid.
To avoid potential contamination, DNA samples were extracted in an AirClean PCR workstation (AirClean Systems, Raleigh, NC). Frozen BAL fluid samples were brought to room temperature prior to DNA extraction. Samples were vortexed for 1 min, and 500 μl was centrifuged for 10 min at 16,000 × g; supernatants were then discarded. The pellets were gently resuspended in 100 μl spheroplast buffer (1.0 M sorbitol [Sigma S-1876], 50.0 mM sodium phosphate monobasic [Sigma S-0751], 0.1% 2-mercaptoethanol [Sigma M-3148], 10 mg/ml lyticase [Sigma L-2524]) and 10 μl of lysing enzymes (Novozyme [Sigma L-1412]) (20 mg/ml) and incubated at 37°C on a rocking platform for 1 h. After centrifugation for 20 min at 400 × g, the spheroplast-BAL fluid pellets were resuspended in 400 μl AP1 buffer (DNeasy Plant Mini kit; QIAGEN). The samples were added to Lysing Matrix D tubes (BioPulverizer system I; Qbiogene/MP Biomedical, Morgan Irvine, CA) and processed using a FastPrep instrument (Qbiogene/MP Biomedical, Morgan Irvine, CA) (24). Samples were processed at speed 5 for 30 s and placed on ice for 5 min; this process was performed a total of three times. Samples were centrifuged at 16,000 × g for 60 s and then gently vortexed. The specimens (approximately 300 μl) were transferred to new tubes. The beads in the Lysing Matrix D tubes were washed with 100 μl AP1 buffer, and this wash was added to the samples (resulting in a 400 μl final volume). Four microliters of RNase A (100 mg/ml) was added, and the mixture was vortexed vigorously and incubated for 10 min at 65°C in an Eppendorf thermomixer (Eppendorf, Westbury, NY) at 1,200 rpm. The pellets were processed according to the protocol for the DNeasy Plant Mini kit (QIAGEN, Valencia, CA) as described in a previous publication (26).
(ii) Threshold for detection of extrinsic contamination with Aspergillus conidia.
A 500 μl aliquot of normal BAL fluid was spiked with 103, 102, or 101 conidia or was left unspiked, and DNA was extracted as described above. In addition, water was processed through the extraction protocol as a kit blank control. All samples were processed in triplicate. The A. fumigatus-specific qPCR assay used in these studies was able to detect ≥100 CFU of conidia in 500 μl of a normal BAL sample. Thus, the kit blank control would be able to detect any extrinsic contamination from environmental conidia at a threshold of ≥100 CFU.
(iii) Primer and probe design.
The design of the primers and probes was described in a previous publication (26). Briefly, a quantitative real-time PCR assay targeting the internal transcribed spacer 1, 5.8S, and internal transcribed spacer 2 regions of the rRNA gene complex and fluorescence resonance energy transfer technology were used. The NCBI BLAST database search program documented the specificity of the primers and probes for A. fumigatus (12).
(iv) qPCR conditions.
The PCR master mix consisted of a 0.5 μM concentration of each of the primers Cap (+) sense (5′ CGAAGACCCCAACATG 3′) and Cap (−) sense 5′ TGAGGGCAGCAATGAC 3′), 5 mM MgCl2, 0.025% bovine serum albumin (Sigma-Aldrich Corp., St. Louis, MO), 0.025 U/ml Platinum Taq DNA polymerase (Invitrogen Corp., Carlsbad, CA), PCR 10× buffer (Invitrogen Corp., Carlsbad, CA), 0.2 mM PCR Nucleotide Mix PLUS (Roche Molecular Biochemicals, Indianapolis, IN) (1 dATP, dCTP, dGTP, and 3 dUTP in proportionate ratios), and 0.1 μM each of the fluorescein (5′ AGTATGCAGTCTGAGTTGATTATCG 3′) and LC Red-640 5′ ATCAGTTAAAACTTTCAACAACGGA 3′) probes. To prevent potential amplicon carryover, each reaction also contained HK-UNG thermostable uracil N-glycosylase (Epicenter, Madison, WI) as recommended by the manufacturer. Each reaction contained a 5 μl aliquot of extracted specimen together with 15 μl of the master mix. A LightCycler 2.0 instrument (Roche Applied Science, Indianapolis, IN) was used with the following cycling conditions: uracil activation, 37°C for 180 s; uracil heat inactivation, 95°C for 60 s for 1 cycle. Amplification cycles were as follows: denaturation at 95°C for 0 s (slope, 20°C/s), annealing at 58°C for 3 s (slope, 10°C/s), extension at 72°C for 15 s (slope, 3°C/s), and cool down at 40°C for 120 s. The total number of cycles was 45. Quantitation standards (serial dilutions of A. fumigatus genomic DNA ranging from 5 × 105 fg to 5 × 100 fg) were run in conjunction with each set of samples. The following controls were also included: DNA extracted from normal BAL fluid, kit blank control (water processed through extraction protocol), and negative master mix control (water). All samples were run in triplicate, and the median cycle number data were used for analysis. The master mix was prepared in a biosafety cabinet in a different room from that in which DNA extractions were performed. LightCycler carousel loading was performed in a separate room from that in which the PCR master mix was prepared.
(v) Analytical sensitivity and quantitation of the qPCR assay.
Quantitation, accuracy, and precision of the qPCR assay were determined through serial dilutions of A. fumigatus genomic DNA ranging from 5 × 105 fg to 5 × 100 fg. The calculated PCR efficiency was 1.98. A quantitative PCR signal of ≤36 cycles was considered a positive result. Fluorescent curves were analyzed with LightCycler software, version 3.5. The analysis of quantification data was done by the second derivative maximum method. This highly reproducible method performs automatic data calculations and determines crossing points with no user influence.
(vi) Specificity.
The specificity of the assay was determined by cross-reactivity studies using 100 fg of genomic DNA from the following organisms: Aspergillus flavus, Aspergillus niger, Aspergillus terreus, Penicillium marneffei, Penicillium notatum, Penicillium citrinum, Penicillium purpurogenum, Pseudallescheria boydii, Penicillium chrysogenum, Rhizopus oryzae, Fusarium solani, Saccharomyces cerevisiae, Trichosporon asahii, Trichosporon inkin, Cryptococcus neoformans, Candida albicans, Candida tropicalis, Candida parapsilosis, Candida krusei, and Candida glabrata as well as rabbit and human DNA. No cross-reactivity was observed.
(vii) Inhibition studies.
Separate PCR-fluorescence resonance energy transfer reactions were performed on all samples to test for any inhibitors of PCR. A master mix with Candida albicans primers-probes was used as previously described (17). Additionally, 5 μl of water was added to 15 μl of the master mix as a reference for results showing no inhibition. Crossover values of the experimental samples were compared to the crossover values of the water samples. The presence of inhibition would result in a higher crossover value compared to those of water samples. No inhibition was observed in any of the samples.
Statistical analysis.
The sensitivity, specificity, and cutoff for the GM EIA assay and qPCR assay were determined by ROC analysis. ROC analysis was also performed for BAL fluid samples from animals that received antifungal therapy (all treatment group data combined). The area under the ROC was determined using Prism 3 software (GraphPad Software Inc., San Diego, CA). The effect of ravuconazole, micafungin, and deoxycholate amphotericin B antifungal treatment was determined by a Mann-Whitney U test using untreated controls. Data from continuous variables are presented as means ± standard errors of the mean. A two-tailed P value of ≤0.05 was considered to be statistically significant. In order to measure the possible relationship between survival and diagnostic BAL parameters, survival was analyzed by linear regression as a function of GM EIA, qPCR, or quantitative culture results. The possible relationship between survival and diagnostic BAL parameters was further analyzed by determination of the presence or absence of a positive GM EIA, qPCR, or quantitative culture result for BAL fluid from treated versus untreated animals by Fisher's exact test and expressed in two-by-two contingency tables.
RESULTS
Sensitivity and specificity of GM EIA, qPCR, and culture in BAL fluid.
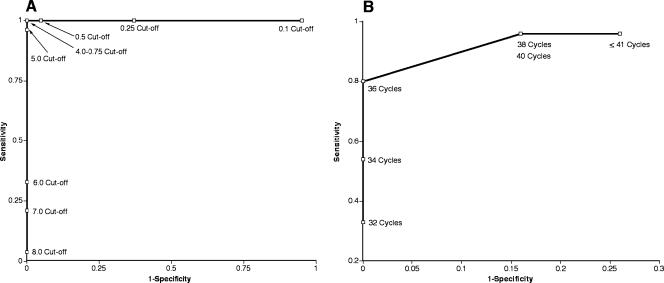
For the GM assay the ROC showed 100% sensitivity and 100% specificity at GM index (GMI) cutoffs ranging from 0.75 to 4.0. A cutoff optical density ratio of 0.75 was chosen to define GM positivity for this study. Choosing a lower cutoff value would result in lower specificity while retaining sensitivity (100%). A higher cutoff value (above 4.0) results in decreased specificity while retaining sensitivity (Fig. 1A). The GM EIA of corresponding serum samples showed 100% sensitivity with an optical density cutoff ratio of 0.5.
FIG. 1.
(A) ROC demonstrating sensitivity and 1-specificity for the GM EIA at different GMI cutoff values for BAL fluid from 24 untreated control rabbits with IPA and 19 healthy rabbits. There was 100% sensitivity and specificity within the range of 0.75 to 4.0. (B) ROC demonstrating sensitivity and 1-specificity for qPCR at different cycle number cutoff values for BAL fluid from 24 untreated control rabbits and 19 healthy rabbits. There was 80% sensitivity and 100% specificity at 36 cycles. Any crossover value ≤ 36 cycles was considered positive.
The ROC for the qPCR assay indicated that a crossover value of 36 cycles would be the optimal point for positivity, resulting in a sensitivity of 80% and a specificity of 100%. Therefore, a cycle number ≤ 36 cycles was considered positive. A crossover value > 36 cycles resulted in increased sensitivity but decreased specificity and was therefore considered negative (Fig. 1B).
The sensitivity of BAL fluid culture as measured by log (CFU/milliliter) was 42% with a specificity of 100%. GM EIA was positive for 100% and qPCR was positive for 70% of the infected animals that BAL fluid culture failed to detect as infected (Table 1).
TABLE 1.
Diagnostic yield of GM antigen and qPCR and residual fungal burden in animals with experimentally induced IPAa
| Treatment group | % Sensitivity (no. of animals)
|
|||||
|---|---|---|---|---|---|---|
| BAL fluid culture | BAL GM EIA | Serum GM EIA | BAL qPCR | GM EIA in culture-negative BAL fluid | qPCR in culture-negative BAL fluid | |
| Untreated (controls) | 42 (24)b,c | 100 (24)b | 100 (17)b | 80 (24)c | 100 (13) | 70 (13) |
| Treated | 16 (61)b,d | 92 (61)b | 90 (60)b | 50 (61)d | 90 (51) | 47 (51) |
Data are presented as percentages of sensitivity of assays for animals with microbiologically and histologically documented aspergillosis.
P < 0.0001; all P values represent comparisons of EIA and qPCR methods to BAL fluid culture.
P = 0.02.
P = 0.0002.
Effect of antifungal therapy on sensitivity and specificity of GM EIA, qPCR, and culture of BAL fluid.
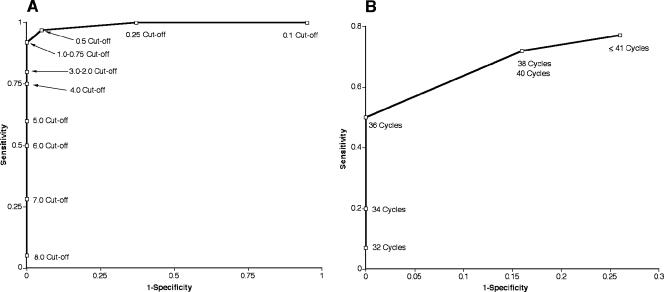
In analyses of the effect of antifungal treatment, different ROC results were observed for the GM EIA and qPCR assay. The GM EIA at our previously determined GMI cutoff of 0.75 had demonstrated a decrease in sensitivity to 92%, with the specificity remaining the same at 100% (Fig. 2A). This change corresponded to a 1% decline in the area under the ROC when antifungal therapy was administered. The sensitivity of the corresponding serum samples also declined with antifungal therapy to 90% (Table 1).
FIG. 2.
(A) ROC demonstrating sensitivity and 1-specificity for the GM EIA at different GMI cutoff values for BAL fluid from 61 rabbits receiving antifungal therapy for IPA and 19 healthy rabbits. There was a decline in sensitivity to 92% with 100% specificity. (B) ROC demonstrating sensitivity and 1-specificity for qPCR at different cycle number cutoff values for BAL fluid from 61 rabbits receiving antifungal therapy for IPA and 19 healthy rabbits. There was a decline in sensitivity to 50%, with 100% specificity.
When antifungal therapy was administered, the sensitivity of the qPCR assay decreased to 50%; however, the specificity of the assay remained the same at 100% (Fig. 2B) while the ≤36 cycle criterion for positivity was retained. This decline in assay sensitivity corresponded to a 30% decline in the area under the ROC. However, in animals treated with antifungal therapy, the sensitivity of BAL fluid culture decreased even more to 16% (Table 1).
The GM EIA and qPCR assay of BAL fluid both showed a significant decline in signal for detection in experiments using rabbits treated with ravuconazole (P ≤ 0.02). In contrast, BAL fluid cultures did not show a significant decline in fungal burden with ravuconazole treatment (P = 0.23) (Table 2).
TABLE 2.
Effect of antifungal therapy on detection of GM antigen, genomic DNA, and residual fungal burden in BAL fluid of animals with experimentally induced IPAa
| Treatment group (no. of animals) | Diagnostic yield ofb:
|
||
|---|---|---|---|
| EIA (GMI) | PCR (log DNA/ml) | Culture (log CFU/ml) | |
| Untreated controls (24) | 6.0 ± 0.18d,e | 3.3 ± 0.46e,f | 0.70 ± 0.2e |
| Animals treated with: | |||
| Ravuconazole (17) | 3.2 ± 0.50d | 1.6 ± 0.47e | 0.42 ± 0.24 |
| Micafungin (26) | 6.8 ± 0.30 | 2.1 ± 0.37e | 0.21 ± 0.10e |
| Deoxycholate amphotericin B (18) | 4.7 ± 0.50e | 1.2 ± 0.40f | 0.16 ± 0.15e |
All P values (see below) represent comparisons of treatment groups to untreated controls.
Data are means±SEM.
DNA data are expressed in femtograms.
P < 0.0001.
P < 0.05.
P = 0.003.
GM levels in BAL fluid remained elevated in rabbits treated with micafungin (Table 2), whereas BAL fluid from animals treated with micafungin showed a significant decline in signal when analyzed by qPCR (P = 0.04) (Table 2).
GM EIA, qPCR, and culture of BAL fluid demonstrated a treatment effect when deoxycholate amphotericin B was administered. All values were significantly lower than those of untreated controls (P ≤ 0.05) (Table 2).
Ability of BAL fluid to convey diagnostic or prognostic information.
In order to evaluate the relationship between qPCR analysis of BAL fluid and survival, we performed time sequence analysis and produced two-by-two contingency tables of diagnostic BAL parameters to address this question. Linear regression analysis of untreated controls demonstrated a trend towards an inverse relationship between survival (y) and qPCR result (x) [where y = −0.26x + (7.3 ± 0.54); P = 0.067]. Moreover, data with respect to the presence or absence of a positive qPCR result for BAL fluid demonstrated a significant difference (P = 0.03) between untreated controls (19/24; mean survival rate, 6.4 ± 0.3 days) and amphotericin B-treated animals (8/18; mean survival rate, 11.2 ± 0.3 days). Quantitative culture also revealed a significant difference (P = 0.02) between the results for untreated controls (11/24; mean survival rate, 6.4 ± 0.3 days) and amphotericin B-treated animals (2/18; mean survival rate, 11.2 ± 0.3) days.
DISCUSSION
The definitive diagnosis of IPA often requires invasive techniques such as biopsy of tissue for histology and culture (1). However, the diagnostic yield of conventional culture-based methods of BAL fluid may have a relatively low sensitivity for detection of A. fumigatus in patients with IPA (3, 19, 32). Incorporating diagnostic assays that are more sensitive and specific, such as GM EIA and qPCR, would permit earlier diagnosis of IPA, would improve clinical outcomes through timely initiation of antifungal therapy, and would allow withholding antifungal treatment when test results are negative. Additionally, both the GM EIA and qPCR assay may enable more rapid results than traditional culture-based methods (hours versus days).
In this well-established model of IPA, the ROC characterization of the GM EIA for BAL fluid had 100% sensitivity and specificity at an optimal GMI cutoff of 0.75. These findings are consistent with those of Musher et al. (25), who found a similar ROC as well as optimal sensitivities and specificities between cutoff values 0.5 and 1.0. In other clinical studies (4, 34, 38), the GM assay higher cutoff values (1.5 or 1.0), was applied to BAL fluid to yield sensitivity ranging from 85 to 100%. However, ROC analysis was not performed in these studies.
Due to documented cross-reactivity between GM antigen and antibiotics such as piperacillin-tazobactam, amoxicillin, and amoxicillin-clavulanic acid (2, 37, 39, 43), the specificity of the GM assay may be diminished in certain patient populations receiving these antibiotics. In these circumstances, the application of a second, more specific diagnostic test, such as qPCR, may provide important adjunctive information to improve diagnostic accuracy. The ROC characterization of the qPCR assay had a sensitivity of 80% and a specificity of 100% for BAL fluid. The threshold for detection of any extrinsic environmental contamination with conidia was ≥100 CFU.
Little is known about the effect of antifungal therapy on the release of GM and the detection of A. fumigatus DNA in BAL fluid. We therefore investigated the effects of antifungal treatment on the detection of GM antigen and A. fumigatus DNA in BAL fluid from neutropenic rabbits with experimentally induced IPA. ROC analysis performed with rabbits treated using antifungal therapy found lower sensitivities for GM EIA and qPCR, with specificities unchanged. The sensitivity of the GM EIA decreased to 92% with antifungal treatment, and the sensitivity of the qPCR assay decreased to 50%. In addition, antifungal therapy decreased the sensitivity of BAL fluid culture to 16%. These findings are consistent with the observation that antifungal therapy may lower the residual fungal burden in lung tissue and therefore diminish the sensitivity of these assays (3, 4, 22, 23, 31).
This study also found that antifungal therapy had a more profound effect on reducing the diagnostic yield of cultures than on that of GM EIA and qPCR. Antifungal therapy is widely used for prophylaxis or empirical therapy in high-risk patients. Consequently, culture-based assays of BAL from patients already receiving antifungal therapy may have diminished sensitivity. These findings are compatible with findings from a recent study of a cohort of patients with invasive aspergillosis; in that study, the sensitivity of GM EIA was diminished by previous antifungal therapy (23). Our findings indicate that the use of GM EIA and qPCR may complement culture-based methods and improve the analysis of BAL fluid for detection of A. fumigatus.
Triazole and echinocandin differed markedly in their effects on detection of GM antigen and genomic DNA of A. fumigatus in BAL fluid. Analysis of BAL fluid from rabbits treated with ravuconazole demonstrated a significant decline in GM antigen as well as a decline in detectable signal of A. fumigatus DNA by qPCR. In contrast to the effects observed with ravuconazole-treated rabbits, we found persistently elevated levels of GM with micafungin treatment. This paradoxical persistence in BAL GM levels in animals treated with micafungin may be due to the effect of the echinocandin in disrupting the cell wall and the inability of the drug to clear histologically detectable organism from lung tissue (30), thus causing the release of GM into the surrounding epithelial lining fluid of the alveoli.
To our knowledge this is the first study to fully characterize and compare GM EIA, qPCR, and quantitative culture for the detection of A. fumigatus in BAL fluid from a well-established animal model system of IPA. These data provide a scientific foundation for interpretation of data derived from clinical BAL fluid specimens from immunocompromised patients, for whom the diagnostic criteria may be less certain (1). The GM EIA and qPCR assay have greater sensitivity than culture in detection of A. fumigatus in BAL fluid. The performances of the GM EIA and qPCR assay may differ according to the specific type of antifungal therapy. These findings suggest that GM EIA and qPCR are useful tools in the analysis of BAL fluid for detection of A. fumigatus. Utilizing these assays in conjunction with culture-based diagnostic methods could facilitate an accurate diagnosis and more-timely initiation of targeted therapy and could result in fewer invasive procedures.
Acknowledgments
We thank Heidi A. Murray and Christine Mya-San for their assistance in conducting laboratory animal studies.
This research was supported by the Intramural Research Program of the National Institutes of Health and National Cancer Institute.
REFERENCES
- 1.Ascioglu, S., J. H. Rex, B. de Pauw, J. E. Bennett, J. Bille, F. Crokaert, D. W. Denning, J. P. Donnelly, J. E. Edwards, Z. Erjavec, D. Fiere, O. Lortholary, J. Maertens, J. F. Meis, T. F. Patterson, J. Ritter, D. Selleslag, P. M. Shah, D. A. Stevens, and T. J. Walsh. 2002. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin. Infect. Dis. 34:7-14. [DOI] [PubMed] [Google Scholar]
- 2.Aubry, A., R. Porcher, J. Bottero, S. Touratier, T. Leblanc, B. Brethon, P. Rousselot, E. Raffoux, J. Menotti, F. Derouin, P. Ribaud, and A. Sulahian. 2006. Occurrence and kinetics of false-positive Aspergillus galactomannan test results following treatment with beta-lactam antibiotics in patients with hematological disorders. J. Clin. Microbiol. 44:389-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Becker, M. J., S. de Marie, D. Willemse, H. A. Verbrugh, and I. A. Bakker-Woudenberg. 2000. Quantitative galactomannan detection is superior to PCR in diagnosing and monitoring invasive pulmonary aspergillosis in an experimental rat model. J. Clin. Microbiol. 38:1434-1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Becker, M. J., E. J. Lugtenburg, J. J. Cornelissen, C. Van Der Schee, H. C. Hoogsteden, and S. De Marie. 2003. Galactomannan detection in computerized tomography-based broncho-alveolar lavage fluid and serum in haematological patients at risk for invasive pulmonary aspergillosis. Br. J. Haematol. 121:448-457. [DOI] [PubMed] [Google Scholar]
- 5.Caillot, D., L. Mannone, B. Cuisenier, and J. F. Couaillier. 2001. Role of early diagnosis and aggressive surgery in the management of invasive pulmonary aspergillosis in neutropenic patients. Clin. Microbiol. Infect. 7(Suppl. 2):54-61. [DOI] [PubMed] [Google Scholar]
- 6.Council, N. R. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, D.C.
- 7.De Bock, R., and the EORTC Invasive Fungal Infections Cooperative Group. 1994. Epidemiology of invasive fungal infections in bone marrow transplantation. Bone Marrow Transplant. 14(Suppl. 5):S1-S2. [PubMed] [Google Scholar]
- 8.Denning, D. W. 1998. Invasive aspergillosis. Clin. Infect. Dis. 26:781-803, 804-5. [DOI] [PubMed] [Google Scholar]
- 9.Denning, D. W. 1996. Therapeutic outcome in invasive aspergillosis. Clin. Infect. Dis. 23:608-615. [DOI] [PubMed] [Google Scholar]
- 10.Denning, D. W., and D. A. Stevens. 1990. Antifungal and surgical treatment of invasive aspergillosis: review of 2,121 published cases. Rev. Infect. Dis. 12:1147-1201. [DOI] [PubMed] [Google Scholar]
- 11.Francis, P., J. W. Lee, A. Hoffman, J. Peter, A. Francesconi, J. Bacher, J. Shelhamer, P. A. Pizzo, and T. J. Walsh. 1994. Efficacy of unilamellar liposomal amphotericin B in treatment of pulmonary aspergillosis in persistently granulocytopenic rabbits: the potential role of bronchoalveolar d-mannitol and serum galactomannan as markers of infection. J. Infect. Dis. 169:356-368. [DOI] [PubMed] [Google Scholar]
- 12.Hope, W. W., T. J. Walsh, and D. W. Denning. 2005. Laboratory diagnosis of invasive aspergillosis. Lancet Infect. Dis. 5:609-622. [DOI] [PubMed] [Google Scholar]
- 13.Jantunen, E., V. J. Anttila, and T. Ruutu. 2002. Aspergillus infections in allogeneic stem cell transplant recipients: have we made any progress? Bone Marrow Transplant. 30:925-929. [DOI] [PubMed] [Google Scholar]
- 14.Jantunen, E., P. Ruutu, L. Niskanen, L. Volin, T. Parkkali, P. Koukila-Kahkola, and T. Ruutu. 1997. Incidence and risk factors for invasive fungal infections in allogeneic BMT recipients. Bone Marrow Transplant. 19:801-808. [DOI] [PubMed] [Google Scholar]
- 15.Jantunen, E., P. Ruutu, A. Piilonen, L. Volin, T. Parkkali, and T. Ruutu. 2000. Treatment and outcome of invasive Aspergillus infections in allogeneic BMT recipients. Bone Marrow Transplant. 26:759-762. [DOI] [PubMed] [Google Scholar]
- 16.Kami, M., T. Fukui, S. Ogawa, Y. Kazuyama, U. Machida, Y. Tanaka, Y. Kanda, T. Kashima, Y. Yamazaki, T. Hamaki, S. Mori, H. Akiyama, Y. Mutou, H. Sakamaki, K. Osumi, S. Kimura, and H. Hirai. 2001. Use of real-time PCR on blood samples for diagnosis of invasive aspergillosis. Clin. Infect. Dis. 33:1504-1512. [DOI] [PubMed] [Google Scholar]
- 17.Kasai, M., A. Francesconi, R. Petraitiene, V. Petraitis, A. M. Kelaher, H. S. Kim, J. Meletiadis, T. Sein, J. Bacher, and T. J. Walsh. 2006. Use of quantitative real-time PCR to study the kinetics of extracellular DNA released from Candida albicans, with implications for diagnosis of invasive candidiasis. J. Clin. Microbiol. 44:143-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latge, J. P. 1999. Aspergillus fumigatus and aspergillosis. Clin. Microbiol. Rev. 12:310-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levy, H., D. A. Horak, B. R. Tegtmeier, S. B. Yokota, and S. J. Forman. 1992. The value of bronchoalveolar lavage and bronchial washings in the diagnosis of invasive pulmonary aspergillosis. Respir. Med. 86:243-248. [DOI] [PubMed] [Google Scholar]
- 20.Lin, S. J., J. Schranz, and S. M. Teutsch. 2001. Aspergillosis case-fatality rate: systematic review of the literature. Clin. Infect. Dis. 32:358-366. [DOI] [PubMed] [Google Scholar]
- 21.Maertens, J., J. Verhaegen, K. Lagrou, J. Van Eldere, and M. Boogaerts. 2001. Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood 97:1604-1610. [DOI] [PubMed] [Google Scholar]
- 22.Marr, K. A., S. A. Balajee, L. McLaughlin, M. Tabouret, C. Bentsen, and T. J. Walsh. 2004. Detection of galactomannan antigenemia by enzyme immunoassay for the diagnosis of invasive aspergillosis: variables that affect performance. J. Infect. Dis. 190:641-649. [DOI] [PubMed] [Google Scholar]
- 23.Marr, K. A., M. Laverdiere, A. Gugel, and W. Leisenring. 2005. Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin. Infect. Dis. 40:1762-1769. [DOI] [PubMed] [Google Scholar]
- 24.Muller, F. M., K. E. Werner, M. Kasai, A. Francesconi, S. J. Chanock, and T. J. Walsh. 1998. Rapid extraction of genomic DNA from medically important yeasts and filamentous fungi by high-speed cell disruption. J. Clin. Microbiol. 36:1625-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Musher, B., D. Fredricks, W. Leisenring, S. A. Balajee, C. Smith, and K. A. Marr. 2004. Aspergillus galactomannan enzyme immunoassay and quantitative PCR for diagnosis of invasive aspergillosis with bronchoalveolar lavage fluid. J. Clin. Microbiol. 42:5517-5522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Sullivan, C. E., M. Kasai, A. Francesconi, V. Petraitis, R. Petraitiene, A. M. Kelaher, A. A. Sarafandi, and T. J. Walsh. 2003. Development and validation of a quantitative real-time PCR assay using fluorescence resonance energy transfer technology for detection of Aspergillus fumigatus in experimental invasive pulmonary aspergillosis. J. Clin. Microbiol. 41:5676-5682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perea, S., and T. F. Patterson. 2002. Invasive Aspergillus infections in hematologic malignancy patients. Semin. Respir. Infect. 17:99-105. [DOI] [PubMed] [Google Scholar]
- 28.Petraitiene, R., V. Petraitis, A. H. Groll, T. Sein, R. L. Schaufele, A. Francesconi, J. Bacher, N. A. Avila, and T. J. Walsh. 2002. Antifungal efficacy of caspofungin (MK-0991) in experimental pulmonary aspergillosis in persistently neutropenic rabbits: pharmacokinetics, drug disposition, and relationship to galactomannan antigenemia. Antimicrob. Agents Chemother. 46:12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petraitiene, R., V. Petraitis, C. A. Lyman, A. H. Groll, D. Mickiene, J. Peter, J. Bacher, K. Roussillon, M. Hemmings, D. Armstrong, N. A. Avila, and T. J. Walsh. 2004. Efficacy, safety, and plasma pharmacokinetics of escalating dosages of intravenously administered ravuconazole lysine phosphoester for treatment of experimental pulmonary aspergillosis in persistently neutropenic rabbits. Antimicrob. Agents Chemother. 48:1188-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petraitis, V., R. Petraitiene, A. H. Groll, K. Roussillon, M. Hemmings, C. A. Lyman, T. Sein, J. Bacher, I. Bekersky, and T. J. Walsh. 2002. Comparative antifungal activities and plasma pharmacokinetics of micafungin (FK463) against disseminated candidiasis and invasive pulmonary aspergillosis in persistently neutropenic rabbits. Antimicrob. Agents Chemother. 46:1857-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petraitis, V., R. Petraitiene, A. A. Sarafandi, A. M. Kelaher, C. A. Lyman, H. E. Casler, T. Sein, A. H. Groll, J. Bacher, N. A. Avila, and T. J. Walsh. 2003. Combination therapy in treatment of experimental pulmonary aspergillosis: synergistic interaction between an antifungal triazole and an echinocandin. J. Infect. Dis. 187:1834-1843. [DOI] [PubMed] [Google Scholar]
- 32.Reichenberger, F., J. Habicht, P. Matt, R. Frei, M. Soler, C. T. Bolliger, P. Dalquen, A. Gratwohl, and M. Tamm. 1999. Diagnostic yield of bronchoscopy in histologically proven invasive pulmonary aspergillosis. Bone Marrow Transplant. 24:1195-1199. [DOI] [PubMed] [Google Scholar]
- 33.Saito, H., E. J. Anaissie, R. C. Morice, R. Dekmezian, and G. P. Bodey. 1988. Bronchoalveolar lavage in the diagnosis of pulmonary infiltrates in patients with acute leukemia. Chest 94:745-749. [DOI] [PubMed] [Google Scholar]
- 34.Sanguinetti, M., B. Posteraro, L. Pagano, G. Pagliari, L. Fianchi, L. Mele, M. La Sorda, A. Franco, and G. Fadda. 2003. Comparison of real-time PCR, conventional PCR, and galactomannan antigen detection by enzyme-linked immunosorbent assay using bronchoalveolar lavage fluid samples from hematology patients for diagnosis of invasive pulmonary aspergillosis. J. Clin. Microbiol. 41:3922-3925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spiess, B., D. Buchheidt, C. Baust, H. Skladny, W. Seifarth, U. Zeilfelder, C. Leib-Mosch, H. Morz, and R. Hehlmann. 2003. Development of a LightCycler PCR assay for detection and quantification of Aspergillus fumigatus DNA in clinical samples from neutropenic patients. J. Clin. Microbiol. 41:1811-1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stynen, D., J. Sarfati, A. Goris, M. C. Prevost, M. Lesourd, H. Kamphuis, V. Darras, and J. P. Latge. 1992. Rat monoclonal antibodies against Aspergillus galactomannan. Infect. Immun. 60:2237-2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sulahian, A., S. Touratier, and P. Ribaud. 2003. False positive test for Aspergillus antigenemia related to concomitant administration of piperacillin and tazobactam. N. Engl. J. Med. 349:2366-2367. [DOI] [PubMed] [Google Scholar]
- 38.Verweij, P. E., J. P. Latge, A. J. Rijs, W. J. Melchers, B. E. De Pauw, J. A. Hoogkamp-Korstanje, and J. F. Meis. 1995. Comparison of antigen detection and PCR assay using bronchoalveolar lavage fluid for diagnosing invasive pulmonary aspergillosis in patients receiving treatment for hematological malignancies. J. Clin. Microbiol. 33:3150-3153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Viscoli, C., M. Machetti, P. Cappellano, B. Bucci, P. Bruzzi, M. T. Van Lint, and A. Bacigalupo. 2004. False-positive galactomannan platelia Aspergillus test results for patients receiving piperacillin-tazobactam. Clin. Infect. Dis. 38:913-916. [DOI] [PubMed] [Google Scholar]
- 40.von Eiff, M., N. Roos, R. Schulten, M. Hesse, M. Zuhlsdorf, and J. van de Loo. 1995. Pulmonary aspergillosis: early diagnosis improves survival. Respiration 62:341-347. [DOI] [PubMed] [Google Scholar]
- 41.Walsh, T. J., J. Bacher, and P. A. Pizzo. 1988. Chronic silastic central venous catheterization for induction, maintenance and support of persistent granulocytopenia in rabbits. Lab. Anim. Sci. 38:467-471. [PubMed] [Google Scholar]
- 42.Walsh, T. J., K. Garrett, E. Feurerstein, M. Girton, M. Allende, J. Bacher, A. Francesconi, R. Schaufele, and P. A. Pizzo. 1995. Therapeutic monitoring of experimental invasive pulmonary aspergillosis by ultrafast computerized tomography, a novel, noninvasive method for measuring responses to antifungal therapy. Antimicrob. Agents Chemother. 39:1065-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walsh, T. J., S. Shoham, R. Petraitiene, T. Sein, R. Schaufele, A. Kelaher, H. Murray, C. Mya-San, J. Bacher, and V. Petraitis. 2004. Detection of galactomannan antigenemia in patients receiving piperacillin-tazobactam and correlations between in vitro, in vivo, and clinical properties of the drug-antigen interaction. J. Clin. Microbiol. 42:4744-4748. [DOI] [PMC free article] [PubMed] [Google Scholar]