Abstract
We isolated and characterized mutants of Bartonella bacilliformis that are resistant to the fluoroquinolone antibiotic ciprofloxacin, which targets the A subunit of DNA gyrase. Mutants had single point mutations in the gyrA gene that changed either Asp-90 to Gly or Asp-95 to Asn and had 3- or 16-fold higher resistance, respectively, to ciprofloxacin than did wild-type B. bacilliformis. Asp-95 is homologous to Asp-87 of Escherichia coli GyrA and is a common residue mutated in fluoroquinolone-resistant strains of other bacteria. This is the first report of a mutation at an Asp-90 homologue, which corresponds to Asp-82 in E. coli GyrA.
Bartonella bacilliformis is the bacterial agent of Carrión's disease in humans, an ailment endemic to the high-altitude regions of Ecuador, Colombia, and Peru (12). The pathogen is transmitted between humans through the bite of contaminated phlebotamine sand flies (22), and three outcomes of infection are possible. In the first syndrome, a patient develops chronic, asymptomatic bacteremia. Usually, these patients are indigenous to the area where the disease is endemic and may serve as reservoirs of infection (12). In the second syndrome, a patient develops chronic angiomatic lesions of the skin, referred to as verruga peruana, that are virtually indistinguishable from bacillary angiomatosis that can develop during infection by Bartonella quintana or Bartonella henselae (21). Although rarely fatal, verruga peruana lesions may scar the patient and can be accompanied by chronic bacteremia (22). The third syndrome, Oroya fever, produces a life-threatening course of acute hemolytic anemia characterized by disseminated erythrocyte infection and a severe reduction in hematocrit (16). Patients who present with Oroya fever are often not indigenous to areas where the disease is endemic (10, 17). Oroya fever is fatal in 40 to 88% of patients unless antibiotics are administered (10, 17, 22). Antimicrobial therapy varies with syndrome and includes the use of chloramphenicol for Oroya fever (4, 19) and of streptomycin or rifampin for verruga peruana (13). Reports of successful treatment of a limited number of infected patients with fluoroquinolones (ciprofloxacin) or macrolides (roxithromycin or erythromycin) hold promise for alternative therapeutic strategies (13).
The primary targets of fluoroquinolone antibiotics are the bacterial type II topoisomerases, DNA gyrase and topoisomerase IV (6, 9). Both enzymes catalyze the cleavage, passage, and reunion of double-stranded DNA in an ATP-dependent fashion (6, 15). However, DNA gyrase introduces negative supercoiling in order to relieve torsional stress imposed on DNA during transcription and replication, whereas topoisomerase IV decatenates interlinked daughter chromosomes following replication and is involved in relaxation (6, 15, 25). Both enzymes are A2B2 tetramers. The A subunit (GyrA or ParC) catalyzes DNA breakage and reunion, whereas the B subunit (GyrB or ParE) binds and hydrolyzes ATP to drive the process (15).
Fluoroquinolones effectively inhibit type II DNA topoisomerases by disrupting DNA breakage-reunion reactions (6, 15). The result is an accumulation of lethal, double-stranded breaks (11, 24). Resistance to these drugs is typically conferred by point mutations in the quinolone resistance-determining region (QRDR) located near the N terminus of the A subunits of both gyrase (GyrA) and topoisomerase IV (ParC) (6, 23). The specific target of fluoroquinolones, either DNA gyrase or topoisomerase IV, varies among different bacterial species as well as with different fluoroquinolones (1, 6-8, 14). Given the growing potential of ciprofloxacin for treatment of bartonellosis (13), this study was undertaken to genetically determine the specific target and frequency of mutations that confer resistance to this drug. We hypothesized that mutations in gyrA of B. bacilliformis would cause resistance to ciprofloxacin.
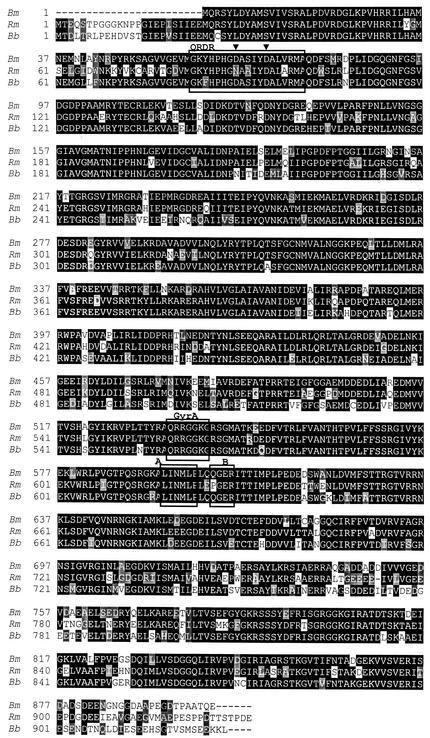
GyrA, a target of fluoroquinolone antibiotics, has not previously been described in any species of Bartonella. The entire gyrA gene of strain KC583 (ATCC 35685) was analyzed to obtain a wild-type sequence for comparison with fluoroquinolone-resistant mutants. The gyrA gene was cloned from a λ Zap Express (Stratagene) genomic library of B. bacilliformis and sequenced as previously described (3). The gene contains 2,784 bp and encodes a protein of approximately 103 kDa. The open reading frame is characterized by a GTG initiation codon and is preceded by a putative strong promoter region spanning nucleotides −16 to −65 (promoter neural network score = 0.93). The gyrA gene is flanked upstream by a 560-bp gene encoding a putative single-stranded DNA binding protein (ssb) and is followed immediately by a 492-bp gene encoding the phosphopantetheine adenylyltransferase enzyme (coaD) (Fig. 1). The encoded GyrA protein contains the GyrA-specific consensus sequences, including the A and B boxes plus the GyrA box (Fig. 2), all of which are elements that are absent in ParC (20). BLASTp searches suggest that GyrA homologues from other α-Proteobacteria, including Brucella melitensis and Agrobacterium tumefaciens (81 and 77% amino acid identities, respectively), are the closest relatives, while E. coli GyrA shares 55% identity with this protein (Fig. 2). Unlike GyrB of B. bacilliformis (2), GyrA does not have an unusually long N terminus compared with those of closely related homologues (Fig. 2).
FIG. 1.
Linkage map of the B. bacilliformis gyrA locus, including two putative flanking genes encoding a single-stranded DNA binding protein (ssb) and phosphopantetheine adenylyltransferase (coaD).
FIG. 2.
Multiple-sequence alignment of B. bacilliformis GyrA (Bb) with GyrA proteins from Rhizobium meliloti (Rm) and Brucella melitensis (Bm). Identical amino acid residues are shown in black, conserved residues are shown in gray, and introduced gaps are indicated with hyphens. The GenBank accession numbers for the Rm and Bm homologues are NP385666 and NP539801, respectively. The QRDR is boxed and the nested ciprofloxacin resistance mutations observed at Asp-90 and Asp-95 are indicated by arrowheads. The highly conserved GyrA, A, and B boxes of the GyrA subunit are also shown.
Wild-type B. bacilliformis strain KC583 was routinely grown for 4 days at 30°C and 100% relative humidity on heart infusion agar (Difco, Detroit, Mich.) supplemented with 4% sheep erythrocytes and 2% sheep serum (Quad Five, Ryegate, Mont.). Antibiotic-resistant mutants were obtained by plating cells on medium supplemented with 0.4 μg of ciprofloxacin (Pentex; Miles Inc., Kankakee, Ill.)/ml. Twenty of the resulting mutants were isolated. The putative QRDR sequence of B. bacilliformis gyrA (Fig. 2) was amplified by PCR using primers QRDR-F (CATGCGATGAATGAAATGGGACTTTTG) and QRDR-R (AAACGACATTCCGTGTAACGCATCGC) and sequenced on both strands as previously described (2).
The mutation rate was calculated to be 6 × 10−9 ciprofloxacin-resistant mutants per generation, a value that is about 10-fold higher than the estimated point mutation rate of E. coli (5) and that is the same as the rate we observed for coumermycin A1 resistance in B. bacilliformis gyrB (2). Twenty ciprofloxacin-resistant mutants were obtained in vitro, and their QRDR regions were characterized by sequence analysis. Of these, four contained transitions of GAT to AAT (G283 to A), encoding predicted substitutions of Asn for Asp-95. A single mutant contained a transition of GAT to GGT (A269 to G), encoding a predicted substitution of Gly for Asp-90. Asp-90 and Asp-95 are homologous to Asp-82 and Asp-87 of E. coli GyrA, respectively. The level of ciprofloxacin resistance of the mutant with the A269-to-G mutation was threefold higher (MIC of ciprofloxacin, 0.9 μg/ml) than that of the wild-type parental strain, for which the MIC was 0.3 μg/ml (a previous study [18] obtained a similar MIC [0.25 μg/ml] for the same wild-type strain), and the level for the mutant with the G283-to-A mutation was approximately 16-fold higher (MIC, 4.7 μg/ml) (these MICs were determined as described previously [2]). The remaining 15 ciprofloxacin-resistant mutants apparently possess mutations that map outside the gyrA QRDR, possibly being located in gyrB, parC, or other regions of gyrA (6). The replacement of Asp-95 by Asn that was observed in the majority of ciprofloxacin QRDR mutants of B. bacilliformis is similar to the mutation of Asp-87 to Asn commonly observed in E. coli and the homologous Asp-94 and Asp-95 substitutions reported for several other bacteria (6). Mutations at Asp-90 or its homologues, including Asp-82 of E. coli GyrA, that are associated with fluoroquinolone resistance have not, to our knowledge, been reported previously in the literature.
This study includes the first characterization of a gyrA gene for the Bartonella genus, a group responsible for several emerging infectious diseases of humans. The sequence data will be useful for future studies examining mechanisms of fluoroquinolone resistance in these pathogens. Our results also show that B. bacilliformis mutations occur in the gyrA QRDR of ciprofloxacin-resistant mutants, particularly at residue Asp-95 and infrequently at Asp-90. Our data also suggest that fluoroquinolone resistance in B. bacilliformis arises more frequently from mutations that map outside the gyrA QRDR. Although genetic tools are limited in B. bacilliformis, the association of these two mutations within the well-established QRDR of GyrA is strong evidence for their involvement in fluoroquinolone resistance. This is the first description of mutations in a Bartonella species that may cause resistance to a clinically useful antimicrobial agent. These data may have clinical relevance as ciprofloxacin and other fluoroquinolones gain popularity as treatment regimens for bartonellosis.
Nucleotide sequence accession number.
The nucleotide sequence reported in this paper is listed in GenBank under accession no. AF469609.
Acknowledgments
We thank Patty McIntire of the Murdock Molecular Biology Facility at The University of Montana for her assistance in nucleotide sequence analysis and Peter Heisig for helpful discussions.
Research support was provided by Public Health Service grant AI45534 and American Heart Association grant 9940002N (to M.F.M.) and National Science Foundation grant MCB-9722408 (to D.S.S.). Z.R.W. was a recipient of an NSF-EPSCoR undergraduate research assistantship.
REFERENCES
- 1.Bagel, S., V. Hullen, B. Wiedemann, and P. Heisig. 1999. Impact of gyrA and parC mutations on quinolone resistance, doubling time, and supercoiling degree of Escherichia coli. Antimicrob. Agents Chemother. 43:868-875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Battisti, J. M., L. S. Smitherman, D. S. Samuels, and M. F. Minnick. 1998. Mutations in Bartonella bacilliformis gyrB confer resistance to coumermycin A1. Antimicrob. Agents Chemother. 42:2906-2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carroll, J. A., S. A. Coleman, L. S. Smitherman, and M. F. Minnick. 2000. Hemin-binding surface protein from Bartonella quintana. Infect. Immun. 68:6750-6757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cuadra, M. S. 1956. Salmonellosis complication in human bartonellosis. Tex. Rep. Biol. Med. 14:97-113. [PubMed] [Google Scholar]
- 5.Drake, J. W. 1991. A constant rate of spontaneous mutation in DNA-based microbes. Proc. Natl. Acad. Sci. USA 88:7160-7164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drlica, K., and X. Zhao. 1997. DNA gyrase, topoisomerase IV, and the 4-quinolones. Microbiol. Mol. Biol. Rev. 61:377-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferrero, L., B. Cameron, B. Manse, D. Lagneaux, J. Crouzet, A. Famechon, and F. Blanche. 1994. Cloning and primary structure of Staphylococcus aureus DNA topoisomerase IV: a primary target of fluoroquinolones. Mol. Microbiol. 13:641-653. [DOI] [PubMed] [Google Scholar]
- 8.Fournier, B., and D. C. Hooper. 1998. Mutations in topoisomerase IV and DNA gyrase of Staphylococcus aureus: novel pleiotropic effects on quinolone and coumarin activity. Antimicrob. Agents Chemother. 42:121-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gellert, M., K. Mizuuchi, M. H. O'Dea, T. Itoh, and J. I. Tomizawa. 1977. Nalidixic acid resistance: a second genetic character involved in DNA gyrase activity. Proc. Natl. Acad. Sci. USA 74:4772-4776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gray, G. C., A. A. Johnson, S. A. Thornton, W. A. Smith, J. Knobloch, P. W. Kelley, L. Obregon Escudero, M. Arones Huayda, and F. S. Wignall. 1990. An epidemic of Oroya fever in the Peruvian Andes. Am. J. Trop. Med. Hyg. 42:215-221. [DOI] [PubMed] [Google Scholar]
- 11.Khodursky, A. B., and N. R. Cozzarelli. 1998. The mechanism of inhibition of topoisomerase IV by quinolone antibacterials. J. Biol. Chem. 273:27668-27677. [DOI] [PubMed] [Google Scholar]
- 12.Kreier, J. P., and M. Ristic. 1981. The biology of hemotrophic bacteria. Annu. Rev. Microbiol. 35:325-338. [DOI] [PubMed] [Google Scholar]
- 13.Maguina Vargas, C. 1988. Bartonellosis or enfermedad de Carrión. Nuevos aspectos de una vieja enfermedad. A.F.A. Editores Importadores S.A., Lima, Peru.
- 14.Pan, X. S., and L. M. Fisher. 1998. DNA gyrase and topoisomerase IV are dual targets of clinafloxacin action in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 42:2810-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reece, R. J., and A. Maxwell. 1991. DNA gyrase: structure and function. CRC Crit. Rev. Biochem. Mol. Biol. 26:335-375. [DOI] [PubMed] [Google Scholar]
- 16.Reynafarje, C., and J. Ramos. 1961. The hemolytic anemia of human bartonellosis. Blood 17:562-578. [PubMed] [Google Scholar]
- 17.Schultz, M. G. 1968. A history of bartonellosis (Carrion's disease). Am. J. Trop. Med. Hyg. 17:503-515. [DOI] [PubMed] [Google Scholar]
- 18.Sobraquès, M., M. Maurin, R. J. Birtles, and D. Raoult. 1999. In vitro susceptibilities of four Bartonella bacilliformis strains to 30 antibiotic compounds. Antimicrob. Agents Chemother. 43:2090-2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Urteaga, B. O., and E. H. Payne. 1955. Treatment of the acute febrile phase of Carrion's disease with chloramphenicol. Am. J. Trop. Med. 4:507-511. [DOI] [PubMed] [Google Scholar]
- 20.Ward, D., and A. Newton. 1997. Requirement of topoisomerase IV parC and parE genes for cell cycle progression and developmental regulation in Caulobacter crescentus. Mol. Microbiol. 26:897-910. [DOI] [PubMed] [Google Scholar]
- 21.Webster, G. F., C. J. Cockerell, and A. E. Friedman-Kien. 1992. The clinical spectrum of bacillary angiomatosis. Br. J. Dermatol. 126:535-541. [DOI] [PubMed] [Google Scholar]
- 22.Weinman, D. 1965. The bartonella group, p. 775-785. In R. J. Dubos and J. G. Hirsch (ed.), Bacterial and mycotic infections of man. Lippincott, Philadelphia, Pa.
- 23.Yoshida, H., M. Bogaki, M. Nakamura, and S. Nakamura. 1990. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob. Agents Chemother. 34:1271-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoshida, H., M. Nakamura, M. Bogaki, H. Ito, T. Kojima, H. Hattori, and S. Nakamura. 1993. Mechanism of action of quinolones against Escherichia coli DNA gyrase. Antimicrob. Agents Chemother. 37:839-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zechiedrich, E. L., A. B. Khodursky, S. Bachellier, R. Schneider, D. Chen, D. M. Lilley, and N. R. Cozzarelli. 2000. Roles of topoisomerases in maintaining steady-state DNA supercoiling in Escherichia coli. J. Biol. Chem. 275:8103-8113. [DOI] [PubMed] [Google Scholar]