Abstract
Burkholderia mallei is a highly infectious gram-negative pathogen and is the causative agent of human and animal glanders. By generating polar mutations (disruption of bsaQ and bsaZ) in the B. mallei ATCC 23344 animal pathogen-like type III secretion system (TTS), we demonstrate that this bacterial protein delivery system is required for intracellular growth of B. mallei in J774.2 cells, formation of macrophage membrane protrusions, actin polymerization, and phagosomal escape. These findings suggest that TTS plays a role in the intracellular trafficking of B. mallei and may facilitate cell-to-cell spread via actin-based motility.
Burkholderia mallei is the etiologic agent of glanders and is a gram-negative, oxidase-positive, nonmotile bacillus that is a facultative intracellular pathogen (3). The natural hosts for B. mallei are horses, donkeys, and mules (solipeds), but other animals, including mice, hamsters, guinea pigs, monkeys, lions, and dogs, are susceptible to this pathogen (3, 7). Cases of human acquired glanders in the United States are uncommon since the implementation of quarantine strategies for imported animals in the 21st century (3). Both human and animal glanders can occur in acute and chronic forms, depending on the route of exposure. For humans, acute glanders is acquired via the inhalational route (without treatment, death results within days) while chronic forms of the disease occur following cutaneous exposure to the pathogen (3).
Various gram-negative bacterial pathogens utilize type III secretion (TTS) for toxin delivery (i.e., effector proteins) into the cytoplasm of infected cells, which in turn subverts host immunological responses to the microbe (2, 6). Recent investigations have demonstrated that the B. mallei and Burkholderia pseudomallei animal pathogen-like TTSs, which are similar to the Salmonella Inv/Spa/Prg and Shigella Ipa/Mxi/Spa TTS networks, are important for in vitro and in vivo survival of these pathogenic Burkholderia species (9-12, 14, 15). These gram-negative bacterial TTSs function to translocate bacterial effector proteins directly into the host cell, which allows bacterial pathogens to evade or alter host defenses (2, 5, 6).
We have recently shown that the B. mallei ATCC 23344 animal pathogen-like TTS is essential for full virulence in BALB/c mice and Syrian hamsters (14). In this investigation, we demonstrate that the B. mallei animal pathogen-like TTS is required for intracellular survival in J774.2 macrophages. Disruption of this TTS drastically reduced intracellular replication within J774.2 cells, prevented phagosomal escape into the host cell cytoplasm, and inhibited membrane protrusion and actin tail formation.
B. mallei strains used in this study.
The bacterial strains used in this investigation, RD01 (bsaQ::pTSV3) and RD02 (bsaZ::pTSV3), have been described by Ulrich and DeShazer (14). These B. mallei strains contain polar mutations (disrupted homologues of the Salmonella enterica serovar Typhimurium invA and spaS genes) within the animal pathogen-like TTS and are avirulent in both hamsters and BALB/c mice (14). To analyze RD01 and RD02 in vitro, a broad-host-range expression plasmid (pBHR1) encoding the green fluorescent protein (GFP) was designed as previously described (8) and mobilized into RD01 and RD02 according to the methods of DeShazer et al. (4).
Macrophage intracellular replication assays.
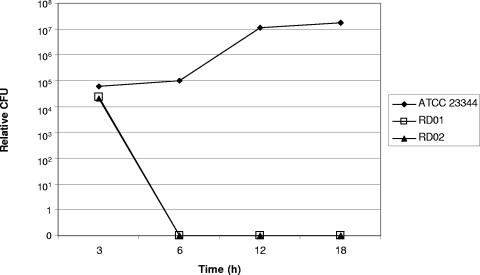
To determine if disrupting the B. mallei animal pathogen-like TTS affects intracellular survival and growth, J774.2 macrophages were infected with either wild-type B. mallei, RD01, or RD02 at a multiplicity of infection of 10 bacteria per macrophage in six-well plates. Cells were centrifuged for 5 min at 1,500 rpm and incubated for 1 h at 37°C with 5% CO2. Cells were washed three times with phosphate-buffered saline (PBS) and overlaid with medium containing 250 μg/ml kanamycin to prevent the growth of extracellular bacteria. At 3, 6, 12, and 18 h postinfection, macrophages were washed and lysed with 1 ml of cold sterile water containing 0.1% Triton X-100 (Sigma, St. Louis, Mo.). Cellular lysates were serially diluted 10-fold, and bacteria were enumerated on Luria-Bertani plates (Fisher Scientific, Pittsburgh, Pa.) supplemented with 4% glycerol containing 100 μg/ml trimethoprim (Sigma). All assays were performed in duplicate. As Fig. 1 depicts, the B. mallei animal pathogen-like TTS is important for the intracellular survival of B. mallei in J774.2 macrophages. At 6 h postexposure (p.e.), both RD01 and RD02 were cleared from macrophages while the number (9.8 × 104 CFU) of wild-type B. mallei organisms remained consistent (Fig. 1). At 18 h p.e., the number of wild-type B. mallei organisms reached 1.8 × 107 CFU while RD01 and RD02 remained undetected, suggesting that TTS is essential for the intracellular survival of B. mallei within J774.2 cells (Fig. 1). Interestingly, compared to B. pseudomallei macrophage intracellular growth (∼105 CFU at 12 h p.e.) (11), it appears that B. mallei proliferation is more pronounced in murine macrophage-like cells (1.8 × 107 CFU by 12 h p.e.) (data not shown). Since polar mutations were generated in RD01 and RD02 TTS gene complementation studies were not performed.
FIG. 1.
Disruption of the B. mallei ATCC 23344 animal pathogen-like TTS prevents intracellular replication of B. mallei within J774.2 murine macrophage-like cells. Infected macrophages were lysed at 3, 6, 12, and 18 h p.e., and bacterial loads were determined in duplicate experiments. RD01 contains a disrupted bsaQ gene (BMAA1542), RD02 harbors a mutation in the bsaZ allele (BMAA1533), and ATCC 23344 represents wild-type B. mallei.
Mutagenesis of the B. mallei bsaQ and bsaZ TTS genes disrupts host cell actin tail formation.
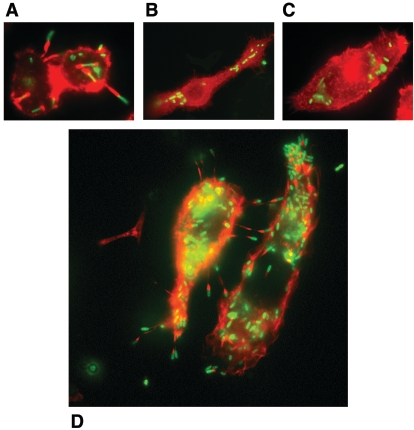
J774.2 murine macrophages were infected with wild-type B. mallei, RD01, or RD02 (each strain constitutively expresses GFP) as described above, with the exception that kanamycin was replaced with 30 μg/ml gentamicin (Sigma) to retard the growth of extracellular bacteria (pBHR1 encodes kanamycin resistance). After 6 h of incubation, cells were washed once with PBS and fixed with 4% paraformaldehyde in PBS overnight at 4°C. Cells were permeabilized with 1% Triton X-100, and filamentous actin was stained red by overnight incubation at 4°C with Alexa Fluor568-phalloidin diluted to 5 U/ml in PBS (Molecular Probes, Eugene, Oreg.). Microscopic visualization (Nikon Eclipse TE2000-S inverted microscope equipped with a Spot-RT digital camera; Image Systems, Columbia, Md.) of J774.2 cells infected with wild-type B. mallei or each TTS mutant clearly demonstrated that the B. mallei TTS is involved in the induction of host cell actin polymerization (Fig. 2). Consistent with a recent investigation (8), Fig. 2A and D show that wild-type B. mallei ATCC 23344 is capable of causing host cellular actin rearrangements whereas RD01 and RD02 fail to promote actin tail formation. These findings suggest that B. mallei employs the Bsa TTS for intracellular trafficking and cell-to-cell spread.
FIG. 2.
The B. mallei ATCC 23344 animal pathogen-like TTS is involved in the induction of actin-based host cell membrane protrusions. J774.2 cells were infected wild-type B. mallei (A and D), RD01 (B), and RD02 (C) expressing GFP at a multiplicity of infection of 10 bacteria to one macrophage. At 6 h p.e., cells were fixed and cellular actin was stained with Alexa Fluor568-phalloidin and viewed at a magnification of ×630.
Association of B. mallei with lysosome-associated membrane glycoprotein 1 (LAMP-1).
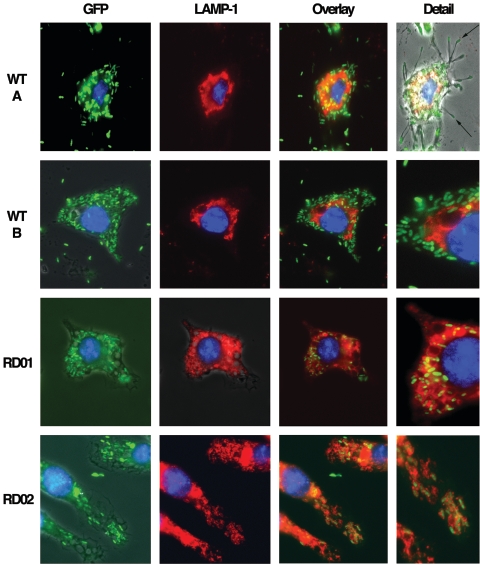
To determine if the B. mallei animal pathogen-like TTS is involved in confining B. mallei within host cell phagosomes, J774.2 macrophages were infected as described for actin polymerization analysis and the association of LAMP-1 with wild-type B. mallei, RD01, and RD02 was determined at 6 h postinfection in duplicate experiments. B. mallei strains constitutively expressing GFP were visualized by their green fluorescence, and LAMP-1 was detected with rat anti-LAMP-1 (1D4B; Department of Biological Sciences, The University of Iowa, Iowa City) and an anti-rat immunoglobulin-Alexa568 (red; Molecular Probes) antibody. Bacteria were considered LAMP-1 associated if any region of the bacterial cell was colocalized with LAMP-1. For quantitative analysis (percent association), bacteria localized with LAMP-1 were determined for 500 bacilli of wild-type B. mallei, RD01, and RD02 and scored as LAMP-1 positive if the green fluorescent bacterial cells were surrounded by red fluorescent membranes (data not shown) (1). As depicted in Fig. 3, wild-type B. mallei was infrequently (18% of the bacterial cells analyzed) colocalized with LAMP-1 staining. In contrast, RD01 (97% of the cells) and RD02 (94% of the bacteria) were heavily colocalized with LAMP-1-positive phagosomes. In the majority of the macrophages observed, the pattern of LAMP-1 distribution differed between cells infected with wild-type B. mallei and those infected with either RD01 or RD02 (Fig. 3). The LAMP-1 distribution in cells infected with wild-type B. mallei was perinuclear, whereas in the RD01 and RD02 infections, the LAMP-1 distribution was more uniformly distributed throughout the cell (Fig. 3). A possible explanation for these differences in LAMP-1 distribution is (i) that LAMP-1 has not yet been recruited to the membrane or (ii) that the phagocytosed organisms, in particular, wild-type B. mallei, are able to escape into the host cell cytosol (Fig. 3). The LAMP-1 staining pattern(s), in parallel with our actin polymerization assays, suggests that the B. mallei bsa TTS is involved in the access of this pathogen to the host cell cytosol, which, in turn, likely contributes to the differences in the LAMP-1 distribution patterns within macrophages infected with wild-type B. mallei and each TTS mutant (Fig. 2 and 3). These results suggest that wild-type B. mallei is able to escape from phagosomal compartments, whereas RD01 and RD02 remain within the maturing phagolysosomes.
FIG. 3.
The Bsa TTS is required for phagosomal escape of B. mallei from infected J774.2 cells. Macrophage-like cells were infected as described for intracellular replication and actin polymerization assays. Wild-type (WT) B. mallei, RD01, and RD02 constitutively express GFP (green). The phagosome-associated protein LAMP-1 was detected with rat anti-LAMP-1 and anti-rat immunoglobulin-Alexa568 antibodies (red) at 6 h following infection at a magnification of ×630. Host cell nuclei were visualized with 4′,6′-diamidino-2-phenylindole (DAPI) stain (blue). Images are from representative slides obtained from duplicate experiments. The Detail column demonstrates that disruption of the Bsa TTS enhances the colocalization of LAMP-1 with RD01 and RD02 at 6 h p.e., whereas the majority of wild-type B. mallei cells (WT B) did not colocalize with LAMP-1 staining. The LAMP-1 staining pattern observed in the wild-type experiments and the low levels of bacterial colocalization are suggestive of bacterial escape into the cytosol. Furthermore, the wild-type bacteria are able to polymerize actin, resulting in membrane protrusions (WT A Detail), which is possible only if the bacteria have gained access to the cytosol.
TTS and B. mallei phagosomal escape.
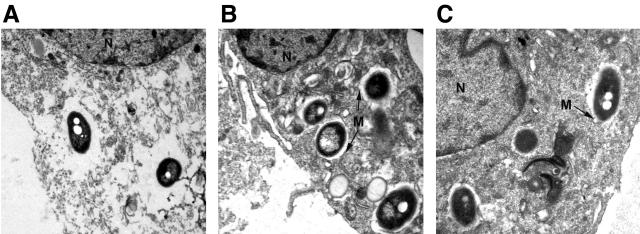
To further analyze the role of the B. mallei animal pathogen-like TTS, transmission electron microscopy (TEM) was employed to determine the intracellular location of wild-type B. mallei, RD01, and RD02 within J774.2 cells. For TEM, macrophages were infected with wild-type B. mallei, RD01, or RD02 (as described for intracellular replication assays) for 6 h and fixed at 25°C with 2.5% glutaraldehyde in a modified Millonig buffer for 16 h. Cells were stained en bloc with 0.5% uranyl acetate in ethanol. Samples were dehydrated in graded ethanol and propylene oxide and embedded in Poly/Bed 812 resin (Polysciences, Inc., Warrington, Pa.). Ultrathin sections were placed on 200-mesh nickel grids and stained with 5% uranyl acetate and 0.2% lead citrate. Figure 4 demonstrates that wild-type B. mallei is capable of endocytic escape, whereas RD01 and RD02 are confined within cellular phagosomes containing intact membranes. These findings imply that the B. mallei animal pathogen-like TTS is required for phagosomal membrane lysis and bacterial escape into the macrophage cytoplasm.
FIG. 4.
Representative TEM image depicting the intracellular location of wild-type B. mallei (A), RD01 (B), and RD02 (C) at 6 h postinfection. Panel A demonstrates that wild-type B. mallei disrupts the phagosomal membrane, whereas RD01 and RD02 remain within phagosomes containing intact membranes (membranes are labeled with the letter M). The host cell nucleus is labeled with the letter N. Magnification, ×25,000.
Several virulence determinants have recently been identified for B. mallei, with the most attenuated strains resulting from disruption of genes involved in B. mallei capsule biosynthesis (wcbB) (4) and the TTS (bsaQ and bsaZ) (14). In addition, we have shown that a B. mallei branched-chain amino acid auxotroph was significantly attenuated in an aerosol BALB/c and hamster model of acute glanders (13). This investigation further shows the importance of the B. mallei animal pathogen-like TTS and how this bacterial protein delivery system is required for the intracellular replication of B. mallei in J774.2 murine macrophage-like cells, induction of host cell actin-based membrane protrusions, and phagosomal escape. Additional work is needed to further characterize the B. mallei animal pathogen-like TTS and to identify the secreted effector molecule(s).
Acknowledgments
We thank Melanie Ulrich, David Heath, and Katheryn Kenyon for reviewing the manuscript and Kathy Kuehl for performing the electron microscopy.
The rat anti-LAMP-1 (1D4B) monoclonal antibody developed by J. T. August was obtained from the Developmental Studies Hybridoma Bank developed under the auspices of the NICHD and maintained by the Department of Biological Sciences, The University of Iowa, Iowa City. The research described herein was sponsored by NIAID interagency agreement Y1-AI-5004-01.
The opinions, interpretations, conclusions, and recommendations presented here are ours and are not necessarily endorsed by the U.S. Army.
Editor: V. J. DiRita
REFERENCES
- 1.Bellaire, B. H., R. M. Roop II, and J. A. Cardelli. 2005. Opsonized virulent Brucella abortus replicates within nonacidic, endoplasmic reticulum-negative, LAMP-1-positive phagosomes in human monocytes. Infect. Immun. 73:3702-3713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cornelis, G. R., and F. Van Gijsegem. 2000. Assembly and function of type III secretory systems. Annu. Rev. Microbiol. 54:735-774. [DOI] [PubMed] [Google Scholar]
- 3.DeShazer, D., and D. Waag. 2004. Glanders: new insights into an old disease, p. 209-237. In L. Lindler, F. Lebeda, and G. W. Korch (ed.), Biological weapons defense: infectious diseases and counterbioterrorism. The Humana Press, Inc., Totowa, N.J.
- 4.DeShazer, D., D. M. Waag, D. L. Fritz, and D. E. Woods. 2001. Identification of a Burkholderia mallei polysaccharide gene cluster by subtractive hybridization and demonstration that the encoded capsule is an essential virulence determinant. Microb. Pathog. 30:253-269. [DOI] [PubMed] [Google Scholar]
- 5.Galan, J. E. 2001. Salmonella interactions with host cells: type III secretion at work. Annu. Rev. Cell Dev. Biol. 17:53-86. [DOI] [PubMed] [Google Scholar]
- 6.Hueck, C. J. 1998. Type III protein secretion systems in bacterial pathogens of animals and plants. Microbiol. Mol. Biol. Rev. 62:379-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller, W. R., L. Pannell, L. Cravitz, W. A. Tanner, and T. Rosebury. 1947. Studies on certain biological characteristics of Malleomyces mallei and Malleomyces pseudomallei. J. Bacteriol. 55:115-126. [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens, J. M., R. L. Ulrich, L. A. Taylor, M. W. Wood, D. Deshazer, M. P. Stevens, and E. E. Galyov. 2005. Actin-binding proteins from Burkholderia mallei and Burkholderia thailandensis can functionally compensate for the actin-based motility defect of a Burkholderia pseudomallei bimA mutant. J. Bacteriol. 187:7857-7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stevens, M. P., A. Friebel, L. A. Taylor, M. W. Wood, P. J. Brown, W. D. Hardt, and E. E. Galyov. 2003. A Burkholderia pseudomallei type III secreted protein, BopE, facilitates bacterial invasion of epithelial cells and exhibits guanine nucleotide exchange factor activity. J. Bacteriol. 185:4992-4996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stevens, M. P., A. Haque, T. Atkins, J. Hill, M. W. Wood, A. Easton, M. Nelson, C. Underwood-Fowler, R. W. Titball, G. J. Bancroft, and E. E. Galyov. 2004. Attenuated virulence and protective efficacy of a Burkholderia pseudomallei bsa type III secretion mutant in murine models of melioidosis. Microbiology 150:2669-2676. [DOI] [PubMed] [Google Scholar]
- 11.Stevens, M. P., M. W. Wood, L. A. Taylor, P. Monaghan, P. Hawes, P. W. Jones, T. S. Wallis, and E. E. Galyov. 2002. An Inv/Mxi-Spa-like type III protein secretion system in Burkholderia pseudomallei modulates intracellular behaviour of the pathogen. Mol. Microbiol. 46:649-659. [DOI] [PubMed] [Google Scholar]
- 12.Suparak, S., W. Kespichayawattana, A. Haque, A. Easton, S. Damnin, G. Lertmemongkolchai, G. J. Bancroft, and S. Korbsrisate. 2005. Multinucleated giant cell formation and apoptosis in infected host cells is mediated by Burkholderia pseudomallei type III secretion protein BipB. J. Bacteriol. 187:6556-6560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ulrich, R. L., K. Amemiya, D. Waag, C. J. Roy, and D. DeShazer. 2005. Aerogenic vaccination with a Burkholderia mallei auxotroph protects against aerosol-initiated glanders in mice. Vaccine 23:1986-1992. [DOI] [PubMed] [Google Scholar]
- 14.Ulrich, R. L., and D. DeShazer. 2004. Type III secretion: a virulence factor delivery system essential for the pathogenicity of Burkholderia mallei. Infect. Immun. 72:1150-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warawa, J., and D. E. Woods. 2005. Type III secretion system cluster 3 is required for maximal virulence of Burkholderia pseudomallei in a hamster infection model. FEMS Microbiol. Lett. 242:101-108. [DOI] [PubMed] [Google Scholar]