The World Health Organization (WHO) compiles and disseminates data on mortality and morbidity reported by its Member States, according to one of its mandates. Since the WHO's inception in 1948, the number of Member States has grown continually and so has the WHO mortality data bank. From 11 countries reporting data on mortality in 1950, the number of countries involved increased to 74 in the year 1985. More than 100 Member States reported on mortality at some point in time.
Data from developed countries (mostly in the North of Europe and of America, and a few countries of the Western Pacific Region) are received on a mostly regular basis. Most developing countries (in Latin America, Asia and in the Eastern Mediterranean Region) report on an irregular basis; very few countries in Africa regularly report on mortality to WHO.
Deaths associated with suicide are an integral part of the WHO mortality data bank. Throughout consecutive editions of the International Classification of Diseases (ICD-6 to ICD-10), the category name and code of suicide have remained relatively stable. Suicide data are reported in absolute numbers along with the mid-year population of a country. The suicide rates are usually represented by country, year, sex, and age group. The most recent data available to the WHO can be accessed through its web site (www.who.int).
The official figures made available to WHO by its Member States are based on death certificates signed by legally authorized personnel, usually doctors and, to a lesser extent, police officers. Generally speaking, these professionals do not misrepresent the information. However, suicide may be hidden and underreported for several reasons, e.g. as a result of prevailing social or religious attitudes. In some places, it is believed that suicide is underreported by a percentage between 20% and 100%. This underlines the importance of bringing about corrections and improvement on a world wide basis.
In contrast to data on completed suicide, no country in the world reports to WHO official statistics on attempted suicide (and most probably countries do not collect them), which makes it impossible to relate national trends of suicide to national trends of attempted suicide. In the absence of national data, one is forced to rely on local studies, which vary considerably, for instance in terms of the operational definition of attempted suicide. The WHO/EURO Multicentre Study on Suicidal Behaviour (1) constitutes a major step forward in this area.
EPIDEMIOLOGICAL CONSIDERATIONS
According to calculations based on data reported to WHO by its Member States, in 1998 suicide represented 1.8% of the global burden of disease and it is expected to increase to 2.4% by the year 2020. Suicide is among the 10 leading causes of death for all ages in most of the countries for which information is available. In some countries, it is among the top three causes of death for people aged 15-34 years.
In the year 2020, approximately 1.53 million people will die from suicide based on current trends and according to WHO estimates. Ten to 20 times more people will attempt suicide worldwide (2). This represents on average one death every 20 seconds and one attempt every 1-2 seconds.
The highest suicide rates for both men and women are found in Europe, more particularly in Eastern Europe, in a group of countries that share similar historical and sociocultural characteristics, such as Estonia, Latvia, Lithuania and, to a lesser extent, Finland, Hungary and the Russian Federation. Nevertheless, some similarly high rates are found in countries that are quite distinct in relation to these characteristics, such as Sri Lanka and Cuba.
According to the WHO regional distribution, the lowest rates as a whole are found in the Eastern Mediterranean Region, which comprises mostly countries that follow Islamic traditions; this is also true of some Central Asian republics that had formerly been integrated into the Soviet Union. Curiously enough, when the data are separated by WHO region, the highest rates in each region, with the exception of Europe, are found in island countries, such as Cuba, Japan, Mauritius and Sri Lanka.
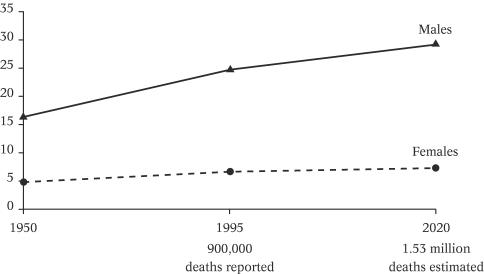
In Figure 1, global suicide rates (per 100,000 population) have been calculated starting from 1950. Deaths reported by countries in each year were averaged and projected in relation to the global population over 5 years of age at each respective year. An increase of approximately 49% for suicide rates in males and 33% for suicide rates in females can be observed between 1950 and 1995.
Figure 1.
Global suicide rates since 1950 and projected trends until 2020
The increase in these global suicide rates must be interpreted with caution. On the one hand, it might reflect the fact that since the end of the USSR (which had an overall rate below the average), some of its former republics (particularly those with the highest rates in the world) started to report individually, thus inflating the global rate. On the other hand, figures for 1950 were based on 11 countries only, and this gradually increased up to 1995, when the estimates were based on 62 countries that reported on suicide. These 62 countries as a whole probably have higher rates, are more concerned with them and have a higher tendency to report on suicide mortality than countries where suicide is not perceived as a major public health problem.
Although it is customary in the suicidology literature to present total rates of suicide for both men and women combined, it should be noted that the current general epidemiological practice is to present rates according to sex and age, particularly when important differences (in terms of figures or risk factors) across sex or age groups exist. This is precisely the situation in relation to suicide; suicide rates of men and women are consistently different in most places, as are rates in different age groups.
Figure 1 also highlights the relatively constant predominance of suicide rates in males over suicide rates in females: 3.2:1 in 1950, 3.6:1 in 1995 and 3.9:1 in 2020. There is only one exception (China), where suicide rates in females are consistently higher than suicide rates in males, particularly in rural areas (3).
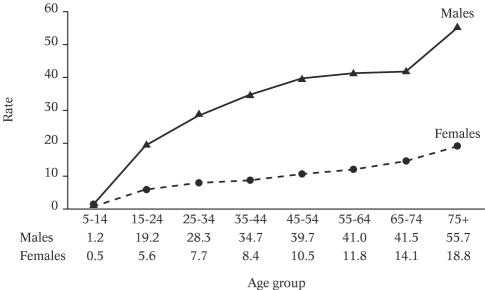
There is a clear tendency for suicide rates to increase with age (Figure 2). By comparison with a global suicide rate of 26.9 deaths per 100,000 for men in 1998, the rates for specific age groups start at 1.2 (in the age group 5-14 years) and gradually increase up to 55.7 (in the age group over 75 years). The same positive relationship between age and suicide rates is observed in females: for an overall rate of 8.2 in 1998, specific age group rates grow from 0.5 per 100,000 (in the age group 5-14 years) to 18.8 (in the age group over 75 years).
Figure 2.
Distribution of suicide rates (per 100,000) by gender and age, 1998
In spite of the wide and appropriate use of rates, the information conveyed by them alone can be misleading, particularly when comparing data across countries or regions with important differences in the demographic structure. As indicated earlier, the highest suicide rates are currently reported in Eastern Europe; however, the largest numbers of suicides are found in Asia. Given the size of their population, almost 30% of all cases of suicide worldwide are committed in China and India alone, although the suicide rate of China practically coincides with the global average and that of India is almost half of the global suicide rate. The number of suicides in China alone is 30% greater than the total number of suicides in the whole of Europe, and the number of suicides in India alone (the second highest) is equivalent to those in the four European countries with the highest number of suicides together (Russia, Germany, France and Ukraine).
Given the relatively narrow differences in the population of males and females in each age group, the large predominance of suicide rates among males is also found in relation to the actual number of suicides committed.
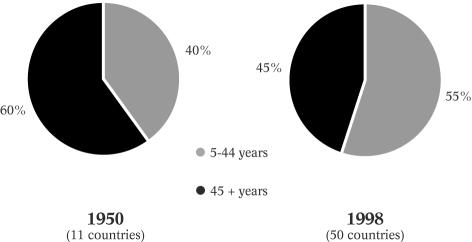
It is in relation to age, however, that the most striking changes are perceived when we move from rates to total numbers. Although suicide rates can be between six and eight times higher among the elderly, as compared with young people, currently more young people than elderly people are dying from suicide, globally speaking. Currently, more suicides (55%) are committed by people aged 5-44 years than by people aged 45 years and older (Figure 3). Accordingly, the age group in which most suicides are currently completed is 35-44 years for both men and women.
Figure 3.
Distribution of suicide rates (per 100,000) by gender and age, 1998
This shift in the predominance of numbers of suicide from the elderly to young people is a new phenomenon. It becomes dramatic when one considers that the proportion of the elderly in the total population is increasing at a greater rate than the one of younger people. Also, it is not the result of a divergent modification in suicide rates in these age groups: the suicide rate in young people is increasing at a greater pace than it is in the elderly.
SUICIDE AND MENTAL DISORDERS
The presence of a mental disorder is an important risk factor for suicide. It is generally acknowledged that over 90% of those who committed suicide had a psychiatric diagnosis at the time of death.
In order to discuss the implications of psychiatric diagnosis for suicide prevention, we have undertaken a systematic review of studies reporting diagnoses of mental disorders. Preliminary findings are to be found elsewhere (4,5).
The review included 31 papers, published between 1959 and 2001 world wide. In total, 15,629 cases of suicide in the general population (above the age of 10 years, both sexes) were identified. Papers focusing only on specific age groups, such as young people or the elderly, or only on specific disorders, such as depression or schizophrenia, were excluded; usually these studies included a rather small sample size. All studies retained refer to people with or without history of admission to mental hospitals (47.5% versus 52.5%, respectively). The diagnostic methods included both diagnoses established while the person was still alive and post-mortem diagnoses based on e.g. psychological autopsies (6). All diagnoses of mental disorders were made on the basis of ICD (8, 9 or 10) or DSM (III, IIIR or IV) and converted to general categories common to both systems.
It is noteworthy that the geographical and cultural representation of the cases was limited, since 82.1% of the cases originated from Europe and North America, whereas cases of Asian countries (including Australia and New Zealand) constituted the remaining part.
The overall results showed that 98% of those who committed suicide had a diagnosable mental disorder, and in this paper we will concentrate on the differences between the psychiatric diagnoses of general populations and of populations which had been admitted to mental hospitals. Out of the 15,629 cases reviewed, 7,424 cases (47.5%) had been admitted at least once to a psychiatric hospital or ward (heretofore designated as PIP), whereas there was no indication of this type of admission in 8,205 cases (52.5%), heretofore designated as GP.
Table 1 shows the distribution of the diagnoses found in all cases. It should be noted that in some studies on GP (but in none on PIP) multiple diagnoses were established, thus making the number of diagnoses greater than the number of cases.
Table 1.
Diagnoses of mental disorders in cases of suicide in psychiatric inpatient and general populations
| Psychiatric inpatient population | General population | |||
|---|---|---|---|---|
| One diagnosis | One and multiple diagnoses | |||
| (7424 cases) | (8205 cases) | |||
| Disorder | Diagnoses | % | Diagnoses | % |
| Mood disorders | 1545 | 20.8 | 4405 | 35.8 |
| Substance-related disorders | 725 | 9.8 | 2754 | 22.4 |
| Schizophrenia | 1481 | 19.9 | 1306 | 10.6 |
| Personality disorders | 1129 | 15.2 | 1432 | 11.6 |
| Organic mental disorders | 1115 | 15.0 | 128 | 1.0 |
| Other psychotic disorders | 769 | 10.4 | 43 | 0.3 |
| Anxiety/somatoform disorders | 187 | 2.5 | 755 | 6.1 |
| Adjustment disorder | 3 | 0.0 | 448 | 3.6 |
| Other DSM axis I diagnosis | 460 | 6.2 | 633 | 5.1 |
| No diagnosis | 130 | 0.1 | 388 | 3.2 |
| Total | 7424 | 100.0 | 12292 | 100.0 |
Unsurprisingly, a psychiatric diagnosis was made in the majority of people who committed suicide; in 3.2% of the cases of GP and in 0.1% of PIP a psychiatric diagnosis was not established, which leaves it open whether there were no good conditions or information for the establishment of a psychiatric diagnosis or whether the person did not actually have a diagnosable mental disorder.
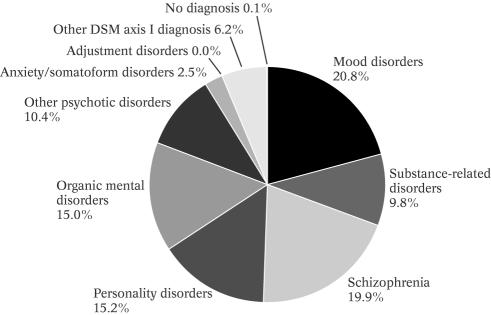
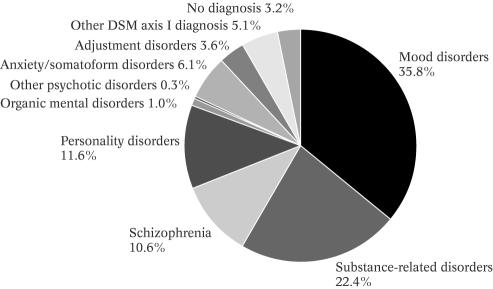
Apart from the predominance of mood disorders in both groups (however, with an important difference between them), there are major differences in the prevalence of psychiatric diagnoses across these two groups, as highlighted below (Figures 4 and 5):
Mood disorders (actually, depression, since a minority of cases of mania was identified in association with suicide) were the most frequently found mental disorders in both types of populations; however, it amounted to 20.8% of PIP and 35.8% of GP, a much smaller percentage than what is currently held.
Schizophrenia is the second most frequent diagnosis in the PIP (19.9%), but only the fourth in GP (10.6%).
Substance-related disorders (actually, alcohol-related disorders, in the vast majority of the cases) was the second most frequent diagnosis in GP (22.4%) but only the sixth in PIP (9.8%).
Personality disorders were third both in PIP (15.2%, a percentage quite similar to organic mental disorders) and in GP (11.6%).
Both organic mental disorders and other psychotic disorders each represented more than 10% of all diagnoses in PIP (15% and 10.4%, respectively), but were below 1% in GP (1% and 0.3%, respectively).
All other individual disorders represented less that 5% of all diagnoses, with the exception of anxiety/somatoform disorders in GP (6.1%, but only 2.5% in PIP).
The combination of the two major psychotic disorders (schizophrenia and other psychotic disorders) in PIP amounts to 30.3% of all cases, which is 50% higher than mood disorders, in this group. If we transfer the few cases of mania from mood disorders into psychotic disorders, this gap is further increased.
The comorbidity of mood disorders with substancerelated disorders (in practice, depression and alcoholism) was the most frequently found by those GP studies that recorded multiple diagnoses (all PIP studies gave only one main diagnosis).
Figure 4.
Suicide and mental disorders: distribution of diagnoses in studies with psychiatric inpatients
Figure 5.
Suicide and mental disorders: distribution of diagnoses in studies with general population
IMPLICATIONS FOR PREVENTION
The data presented above clearly point out the appropriateness of the treatment of mental disorders as a major component of suicide prevention programmes. However, on the one hand, suicide is found associated with a variety of mental disorders, each one of them with a different therapeutic approach, thus making a 'blanket approach' probably unsound. On the other hand, no single mental disorder is found in association with suicide with such a magnitude as to have any significant impact in national suicide rates, should its treatment be even at an impossible 100% of effectiveness.
Although the data presented here included all the studies found in the whole scientific literature in English, through the methodology described earlier on, more than 80% of the cases come from three countries only, namely Denmark, UK and USA. It is quite possible that a different diagnostic distribution be found in other countries or regions. Actually, there are indications that in the Baltic region alcohol-related disorders have a stronger association with suicide than in other regions (7) and that in Asia less suicides are associated with depression, in comparison with Western countries (8,9). According to these authors, in Asian countries there are more suicides of the impulsive type, committed within hours of the triggering factor, than what is usually seen in industrialized countries.
Therefore, a sound suicide prevention strategy should definitely include the treatment of the disorders most fre- quently associated with suicide, on a local basis. In the absence of the relevant information, it should include the treatment of at least schizophrenia, depression and alcohol- related disorders as a main component, but should not overlook other components more dependent on the social and physical environment, as proposed by the WHO human-ecological approach (10).
According to this approach, other actions to prevent suicide include:
Control of the availability of toxic substances and medicines;
Detoxification of domestic gas and car emissions;
Restricted access to guns;
Responsible media reporting about suicide;
Erection of barriers to deter jumping from high places.
At any rate, suicide remains a major public health problem, nevertheless preventable, and action for its prevention calls for a coordinated multisectoral approach. In view of the close association between suicide and mental disorders, psychiatrists are in a particularly strategic position to lead effective suicide prevention programmes.
References
- 1.Schmidtke A, Bille-Brahe U, De Leo D, et al., editors. Suicidal behaviour in Europe: results from the WHO/EURO multicentre study on suicidal behaviour. Bern: Hogrefe & Huber; 2001. [Google Scholar]
- 2.World Health Organization. Figures and facts about suicide. Geneva: World Health Organization; 1999. [Google Scholar]
- 3.Phillips MR. Li X. Zhang Y. Suicide rates in China, 1995–99. Lancet. 2002;359:835–840. doi: 10.1016/S0140-6736(02)07954-0. [DOI] [PubMed] [Google Scholar]
- 4.Bertolote JM. Fleischmann A. Suicide rates in China. Lancet. 2002;359:2274. doi: 10.1016/S0140-6736(02)09268-1. [DOI] [PubMed] [Google Scholar]
- 5.Bertolote JM. Fleischmann A. Suicide and mental disorders in the general population. Submitted for publication. [Google Scholar]
- 6.Beskow J. Runeson B. Asgard U. Psychological autopsies: methods and ethics. Suicide and Life-Threatening Behavior. 1990;20:307–323. [PubMed] [Google Scholar]
- 7.Wasserman D. Värnik A. Suicide-preventive effects of perestroika in the former USSR: the role of alcohol restriction. Acta Psychiatr Scand. 1998;98(Suppl. 394):1–4. doi: 10.1111/j.1600-0447.1998.tb10758.x. [DOI] [PubMed] [Google Scholar]
- 8.Phillips MR. Suicide rates in China. Lancet. 2002;359:2274. [Google Scholar]
- 9.Vijayakumar L. Rajkumar S. Are risk factors for suicide universal? A case-control study in India. Acta Psychiatr. Scand. 1999;99:407–411. doi: 10.1111/j.1600-0447.1999.tb00985.x. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Primary prevention of mental, neurological and psychosocial disorders. Geneva: World Health Organization; 1998. [Google Scholar]