The severely mentally ill are at significant risk of neglect in large cities, where the prevalence of psychosis is high and services can be fragmented. Case management has been proposed as the service model of choice for this group of patients for some time. Case management arose, and has been chiefly researched, in the USA in response to deinstitutionalisation (1) and its procedures have been well described. An initially co-ordinating (brokerage) approach has been replaced with a practice combining direct patient care plus co-ordination (clinical case management) which requires clinically trained staff (2).
Assertive Community Treatment (ACT) is a particular form of case management which emphasises small case loads, comprehensive care and active outreach to the patient's home and neighbourhood. The relationship of Intensive Case Management (ICM), the term favoured in European studies, to ACT is close but somewhat ambiguous. Stein and Test's landmark study (3), convincingly replicated in Australia (4), demonstrated major advantages, both in clinical and social outcome for patients and in terms of reducing hospitalisation and costs. As a consequence the approach has spread rapidly and generated an extensive research literature into the varied forms of case management (5-7).
These research findings are, however, mixed. Overall, case management improves engagement with patients, but evidence for the reduction of hospitalisation rates appears restricted to ACT. Even here the evidence of superiority fades with time and is strikingly absent in European studies (2). Criticisms of this research highlight the lack of scientific rigour in many studies, in particular 'black-box' studies where the effective components are unclear and studies where bias from local enthusiasm and atypical service conditions are not minimised (8).
Four main themes emerge from the literature (9): a) the commonest outcome measure is reduced hospitalisation; b) patients with severe psychotic illness are the target group; c) a restricted case load of <15 patients per case manager is recommended; d) follow-up of over a year is needed to observe impact.
METHODS
We conducted a trial where only one key variable (caseload size) distinguished the experimental and control conditions. This is routine practice in most medical research, but uncommon in mental health services research. We chose caseload size because this could be precisely determined and is believed to be central to outcome. A multi-centre trial meant that we would have adequate power to test our hypotheses, analyse subgroups and evaluate predictors of outcome. It also helped avoid biases common in these studies (8). We took hospitalisation over two years as the primary outcome, because of its place in the literature and significance for service planning. Randomisation, equally to ICM (caseload 1:12-15) or Standard Case Management (SCM, caseload 1:30-35) was conducted blindly and independently and was stratified for point of recruitment (inpatient or outpatient) and for ethnicity (black Afro-Caribbean or other). The data analytical strategy was determined a priori and strictly adhered to.
We tested the hypotheses that ICM would: a) reduce hospitalisation and overall costs compared to SCM; b) produce better outcomes and lower costs in severely, but not moderately, disabled patients; c) produce greater outcome differences in Afro-Caribbean patients than other ethnic groups.
Inclusion criteria for patients were: a) aged 16-65; b) psychosis defined by Research Diagnostic Criteria; c) hospitalised at least twice, most recent in preceding 2 years; d) one third of the sample Afro-Caribbean; e) not suffering from primary substance abuse or organic brain damage; f) not already involved in specific or specialised case management programme.
Staff in both arms of the trial were equally well trained and of equal seniority, and all received an introduction to the study (10). The ICM staff also received a further day's training in ICM from a leading US practitioner. Patients were required to remain with the treatment arm to which they were randomised unless there were serious, overwhelming clinical reasons. Detailed recording of treatment was carried out throughout the study (11).
RESULTS
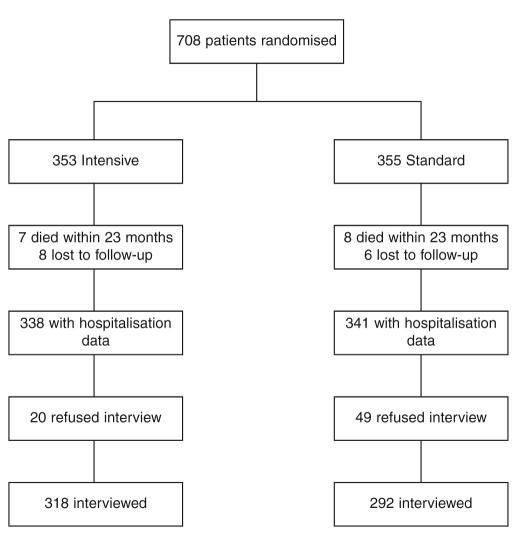
708 subjects were recruited (57% male; mean age 38 yrs). 87% had a diagnosis of schizophrenia or schizoaffective disorder. Only 35% were living with families. There were no significant baseline differences between the experimental and control groups, although there was some overall variation between the four sites (12). 610 patients (86%) were interviewed at 2 years and hospitalisation data were available for 679 (Figure 1).
Figure 1.
UK700 trial profile
Table 1 shows that there were no differences in hospitalisation rates between the two conditions, each group spending a mean of just over 73 days in hospital over these two years. There were no significant interactions based on site, ethnicity or level of baseline disability (10). Afro- Caribbean patients spent exactly the same proportion of time as inpatients as did the mainly white group (a mean of just over 72 days). More severely socially disabled patients did appear to spend more time in hospital and there is just a suggestion that ICM may have more impact, but the differences are small and statistically insignificant with wide confidence intervals. A very detailed economic analysis (13) found no significant cost differences between the two treatment arms. Overall costs were driven substantially by inpatient care and, although there were extra costs incurred for the smaller caseloads for ICM, these were partially balanced by increased costs in social care. The variation in costs for individual patients was very great, reducing the possibility of identifying statistically significant differences.
Table 1.
Days in hospital over 2 years in patients receiving Intensive vs. Standard Case Management
| Intensive | Standard | Difference (Intensive-Standard) | ||||
|---|---|---|---|---|---|---|
| (n=353) | (n=355) | Estimate | 95% CI | p value | ||
| Missing data* | 15 (4.3%) | 14 (3.9%) | ||||
| Mean days in hospital | 73.5 | 73.1 | 0.4 | -17.4 | 18.1 | 0.97 |
| (SD) | (124.2) | (111.2) | ||||
| Centre1 | ||||||
| St. George’s (n=189) | 73.9 | 63.4 | 10.5 | -22.3 | -43.3 | |
| Manchester (n=151) | 78.9 | 59.4 | 19.5 | -19.6 | 58.7 | |
| St. Mary’s (n=189) | 65.7 | 90.9 | -25.3 | -59.5 | 9.0 | |
| King’s (n=150) | 76.7 | 75.8 | 0.9 | -36.9 | 38.7 | |
| Ethnicity2 | ||||||
| Afro-Caribbean (n=194) | 72.3 | 72.3 | -0.1 | -30.6 | 30.5 | |
| Other (n=485) | 74.0 | 73.4 | 0.6 | -21.2 | 22.3 | |
| Severity (DAS total)3 | ||||||
| <1 (moderate) (n=306) | 67.9 | 66.9 | 1.0 | -25.9 | 27.9 | |
| ≥1 (severe) (n=363) | 75.1 | 81.0 | -5.9 | -30.1 | 18.3 | |
| Median days in hospital | 17.5 | 28.0 | 10.5 | -22.0 | 2.0 | 0.16 |
| Any time in hospital | 210 (62.1%) | 228 (66.9%) | -4.7% | -11.9% | 2.5% | 0.20 |
Missing data: 15 deaths before 23 months and 14 lost to follow-up (see Figure 1)
DAS: Disability Assessment Schedule
Test of common difference for all centres: P=0.31;
Test of common difference for both ethnic groups: P=0.98;
Test of common difference for both levels of severity: P=0.69
Despite a comprehensive assessment of a wide range of clinical status, social functioning, needs for care and quality of life data, no differences were found between the two groups (10). Deaths (9 suicides, one homicide and 6 natural causes) were equally distributed. Surprisingly, more patients were lost to care in ICM (46 vs. 27, p=0.02). The study was an opportunity to characterise treatment patterns in detail and this confirmed that the rate of contact in ICM was double that in SCM: 3.35 vs. 1.46 face to face contacts per 30 days, a difference of 1.9 (p<0.001, 95% CI 1.5, 2.29) (11).
DISCUSSION
Criticisms of the trial
The failure of caseload size to impact at all on hospitalisation or on clinical and social functioning was initially very unexpected, given both the literature in this area and current political and professional assumptions (14). Not surprisingly it has caused considerable controversy (15-19). There were two main criticisms. The first was that there were no differences at all in process of care between the two arms - staff in ICM had simply carried on as before. The second was that we had tested an ineffectual model of care. This second criticism reflects the belief that ACT and ICM are qualitatively different and only ACT would make a difference (20). ACT, so this criticism goes, is an 'all or nothing' approach and individual components are not exportable. Both these criticisms are important ones and need to be taken seriously.
Detailed prospective recording convincingly dispels the first criticism (11). ICM patients did have higher levels of care and this did encompass a broad range of social as well as medical interventions (although the proportion of the former was low). That something different was happening (even if it failed to produce significant differences in our initial hypotheses) is confirmed by a post-hoc analysis demonstrating that trial subjects with psychosis and borderline intelligence did have reduced hospitalisation in ICM (21).
The second criticism, that only ACT in pure form makes a difference, is pervasive and requires detailed attention. From a scientific perspective, we would argue that such a position is a belief and not knowledge. The history of medicine is littered with such beliefs that have subsequently proved to be unfounded when the effective ingredients of treatments have been isolated. Our approach in the UK700 trial, however, is not the most powerful way to examine this criticism. That would be to find two functioning ACT teams (preferably groups of teams) and alter one component within one of them and observe the outcome. Such studies are highly improbable, so we would argue that testing the individual parameters which are thought to be responsible for efficacy in the ACT approach has still to be pursued. After all, the configuration of ACT teams did not evolve from painstaking scientific enquiry but is simply based on Stein and Test's study. Even if synergy were of such importance, this would predict a reduced impact, not an absent one. Such a proposed synergistic configuration should be based on theory, with implications that could then be described and then tested. This is currently not the case.
Alternative explanations for the similar outcomes in the two arms
Closer attention to the literature suggests that the large differences in hospitalisation demonstrated by earlier US and Australian studies are no longer being achieved (5,22,23). Increasingly the 'defining characteristics' of ACT in earlier studies are to be found in the control services against which they are compared. What were once the experimental services (e.g. case management, community support teams) in such studies are now often the controls (24). In a systematic review by Catty et al (24), it becomes clear that studies that have community mental health services as their controls achieve much less reduction in hospitalisation rates than (often earlier) studies where the control was based on hospital care. With community-based control services, the mean reduction was only 0.5 days hospitalisation a month versus 6 days when the control was hospital based - a twelve-fold difference. Improvements in standard community services and gradually reducing lengths of stay have profoundly altered the possibilities for significantly reducing hospitalisation in the severely mentally ill.
A possible alternative approach to resolving this ongoing uncertainty is to ignore the designation of the service and to examine the impact of individual components. In the review by Catty et al (24), individual components of experimental and control services (obtained from the authors) were tested for associations with reduction in hospitalisation. Significant associations were found only for 'joint health and social care' and 'regularly visiting at home'. Caseload size and a number of other 'key variables' failed to correlate with a reduction. These variables may be more suitable candidates for further consideration and perhaps rigorous randomized controlled trials than some of the structural features usually proposed in this area.
CONCLUSIONS
The UK700 trial has been an ambitious attempt to introduce the scientific rigour associated with most other medical research (e.g., adequately powered, single variable tested, strict attention to controlling for bias and a clearly articulated analytical plan) to mental health services research. It proposed three main hypotheses about the benefits for psychotic patients of reducing caseload size, and none was supported by the results. It highlights for researchers the problems inherent in smaller or less rigorous trials, and points the way to either further large-scale trials or second generation case management trials with more carefully argued questions and outcome measures.
Collaboration across four sites led to increased clarity about measures and questions, and proved an essential check on dogma and over-enthusiasm. It also resulted in a rich database about these patients and their treatment that has permitted the subsequent examination of several questions. Less rigorously designed trials in this area (particularly small head-to-head studies) are unlikely to move our understanding on. Our conclusion is that currently, in wellcoordinated mental health services, simply reducing the caseload does not improve outcome for these patients. Mental health planners may need to pay more attention to the content of treatment rather than changes in service configurations.
Appendix
The UK700 Group is a collaborative study team involving four clinical centres: Manchester Royal Infirmary (Tom Butler, Francis Creed, Janelle Fraser, Peter Huxley, Nick Tarrier, Theresa Tattan); King's College and Maudsley Hospitals, London (Tom Fahy, Catherine Gilvarry, Kwame McKenzie, Robin Murray, Jim van Os, Elizabeth Walsh); St. Mary's and St. Charles' Hospitals, London (John Green, Anna Higgitt, Elizabeth van Horn, Donal Leddy, Patricia Thornton, Peter Tyrer); St. George's Hospital, London (Rob Bale, Tom Burns, Matthew Fiander, Kate Harvey, Andy Kent, Chiara Samele); Health Economics Centre, York (Sarah Byford, David Torgerson, Ken Wright); Statistical Centre, London (Simon Thompson, Ian White).
Acknowledgements
The UK700 trial was funded by grants from the UK Department of Health and NHS Research and Development programme.
References
- 1.Intagliata J. Improving the quality of community care for the chronically mentally disabled: the role of case management. Schizophr Bull. 1982;8:655–674. doi: 10.1093/schbul/8.4.655. [DOI] [PubMed] [Google Scholar]
- 2.Holloway F. Case management for the mentally ill: looking at the evidence. Int J Soc Psychiatry. 1991;37:2–13. doi: 10.1177/002076409103700102. [DOI] [PubMed] [Google Scholar]
- 3.Stein LI. Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry. 1980;37:392–327. doi: 10.1001/archpsyc.1980.01780170034003. [DOI] [PubMed] [Google Scholar]
- 4.Hoult J. Rosen A. Reynolds I. Community orientated treatment compared to psychiatric hospital orientated treatment. Soc Sci Med. 1984;18:1005–1010. doi: 10.1016/0277-9536(84)90272-7. [DOI] [PubMed] [Google Scholar]
- 5.Mueser KT. Bond GR. Drake RE, et al. Models of community care for severe mental illness: a review of research on case management. Schizophr Bull. 1998;24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314. [DOI] [PubMed] [Google Scholar]
- 6.Marshall M. Lockwood A. Assertive Community Treatment for people with severe mental disorders (Cochrane Review) The Cochrane Library. 1998 doi: 10.1002/14651858.CD001089. [DOI] [PubMed] [Google Scholar]
- 7.Marshall M. Gray A. Lockwood A, et al. Case management for severe mental disorders. The Cochrane Collaboration. 1997 [Google Scholar]
- 8.Coid J. Failure in community care: psychiatry's dilemma. Br Med J. 1994;308:805–806. doi: 10.1136/bmj.308.6932.805a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Creed F. Burns T. Butler T, et al. Comparison of intensive and standard case management for patients with psychosis. Rationale of the trial. 1999;174:74–78. doi: 10.1192/bjp.174.1.74. [DOI] [PubMed] [Google Scholar]
- 10.Burns T. Creed F. Fahy T, et al. for the UK700 Group Intensive versus standard case management for severe psychotic illness: a randomised trial. Lancet. 1999;353:2185–2189. doi: 10.1016/s0140-6736(98)12191-8. [DOI] [PubMed] [Google Scholar]
- 11.Burns T. Fiander M. Kent A, et al. Effects of case load size on the process of care of patients with severe psychotic illness. Br J Psychiatry. 2000;177:433. doi: 10.1017/s0007125000227359. [DOI] [PubMed] [Google Scholar]
- 12.Fahy T. Kent A. Tattan T, et al. for the UK700 Group Predictors of quality of life in people with severe mental illness: study methodology with baseline analysis in the UK700 trial. Br J Psychiatry. 1999;175:426–432. doi: 10.1192/bjp.175.5.426. [DOI] [PubMed] [Google Scholar]
- 13.Byford S. Fiander M. Torgerson D, et al. for the UK700 Group Cost-effectiveness of intensive versus standard case management for severe psychotic illness. Br J Psychiatry. 2000;176:537–543. doi: 10.1192/bjp.176.6.537. [DOI] [PubMed] [Google Scholar]
- 14.Department of Health. The NHS Plan - A plan for investment, a plan for reform. London: Department of Health; 2000. [Google Scholar]
- 15.Gournay K. Thornicroft G. Comments on the UK700 case management trial. Br J Psychiatry. 2000;370:370–372. doi: 10.1192/bjp.177.4.371. [DOI] [PubMed] [Google Scholar]
- 16.McGovern D. Owen A. Intensive case management for severe psychotic illness. Lancet. 1999;354:1384–1386. doi: 10.1016/S0140-6736(05)76235-8. [DOI] [PubMed] [Google Scholar]
- 17.Pelosi AJ. Duncan GL. McNulty SV. Intensive case management for severe psychotic illness. Lancet. 1999;354:1384–1386. doi: 10.1016/s0140-6736(05)76236-x. [DOI] [PubMed] [Google Scholar]
- 18.McGee MA. Intensive case management for severe psychotic illness. Lancet. 2000;354:1385–1386. doi: 10.1016/S0140-6736(05)76237-1. [DOI] [PubMed] [Google Scholar]
- 19.Burns T. Fahy T. Thompson S, et al. Intensive case management for severe psychotic illness (Authors' reply) Lancet. 1999;354:1384–1386. doi: 10.1016/s0140-6736(05)76236-x. [DOI] [PubMed] [Google Scholar]
- 20.Marshall M. London's mental health services in crisis. Br Med J. 1997;314:246. doi: 10.1136/bmj.314.7076.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tyrer P. Hassiotis A. Ukoumunne O, et al. for the UK700 Group Intensive case management for psychotic patients with borderline intelligence. UK 700 Group. Lancet. 1999;354:999–1000. doi: 10.1016/s0140-6736(99)02080-2. [DOI] [PubMed] [Google Scholar]
- 22.Holloway F. Oliver N. Collins E, et al. Case management: a critical review of the outcome literature. Eur Psychiatry. 1995;10:113–128. doi: 10.1016/0767-399X(96)80101-5. [DOI] [PubMed] [Google Scholar]
- 23.McHugo GJ. Drake RE. Teague GB, et al. Fidelity to assertive community treatment and client outcomes in the New Hampshire dual disorders study. Psychiatr Serv. 1999;50:818–824. doi: 10.1176/ps.50.6.818. [DOI] [PubMed] [Google Scholar]
- 24.Catty J. Burns T. Knapp M, et al. Home treatment for mental health problems: a systematic review. Psychol Med. 2002;32:383–401. doi: 10.1017/s0033291702005299. [DOI] [PubMed] [Google Scholar]