Our understanding of brain function has developed considerably since the advent of cognitive neuroscience and functional neuroimaging. Apparently, there are two central principles that functional brain architectures conform to: functional specialisation and functional integration. The former posits that brain systems are specialised for various perceptual and cognitive functions, and the latter emphasises interactions among these specialised systems. This integration is mediated by the functional equivalent of anatomical connections, i.e. effective connectivity (defined as the influence one neuronal system exerts over another). The notion of effective connectivity engendered the disconnection hypothesis, which represented an attempt to understand schizophrenia in mechanistic terms. This paper reviews the disconnection hypothesis and its implications for how one might use the powerful tools that are emerging from functional neuroimaging and genomics, to pinpoint the mechanisms that might cause schizophrenia.
WHAT SORT OF DISCONNECTION SYNDROME?
The idea that dysfunctional integration underlies schizophrenia is as old as its name, coined by Bleuler (1) to denote the disintegration of psychic processes. The disconnection hypothesis considered here states that schizophrenia can be understood in cognitive terms, and in terms of pathophysiology, as a failure of functional integration within the brain. Functional integration refers to the interactions of functionally specialised systems (i.e., populations of neurons, cortical areas and sub-areas), that are required for adaptive sensorimotor integration, perceptual synthesis and cognition. Functional integration is mediated by the influence that the dynamics or activity of one neuronal system exerts over another and therefore rests on the connections among them. The pattern of connectivity is, in turn, a function of epigenetic activity and experience-dependent plasticity. The idea, developed below, is that the pathology of schizophrenia targets the modulation, facilitation or consolidation of changes in connection strength. This is distinct from an abnormality of plasticity per se and highlights aberrant regulation of where and when synaptic plasticity can occur. This dynamic regulation can be attributed, in part, to ascending modulatory neurotransmitter systems, like the dopaminergic system.
The notion that psychosis can be explained by a pathology of extrinsic connections (cortico- cortical and cortico-subcortical connections that constitute white matter tracts) can be attributed to Wernicke, who referred to disruptions of these 'organs of connection'. This implies an anatomical disconnection. This is not the sort of disconnection syndrome proposed for schizophrenia. In schizophrenia, the disconnection is thought of as explicitly functional, not anatomical (2). More precisely, the disconnection is in terms of effective connectivity (3) as opposed to anatomical connectivity. The abnormal interactions among neuronal populations will clearly have infrastructural correlates, but these are likely to be expressed at the level of synaptic specialisations, cellular morphology and cytoarchitectonics, not necessarily at the level of white matter fasciculi.
DYSFUNCTIONAL INTEGRATION OR SPECIALISATION?
It is worthwhile considering disconnection in relation to other formulations. The alternative is that schizophrenia could be explained by regionally specific pathophysiology in one or more neuronal systems. In other words, impaired functional specialisation as opposed to dysfunctional integration. There is an important distinction here between the pathological interaction of two cortical areas and the otherwise normal interaction of two pathological areas.
The distinction between a regionally specific insult to the brain and aberrant interactions is fundamental. A regionally specific pathology, such as stroke or a tumour, is a sufficient explanation for the cognitive or sensorimotor deficits of some patients. However, with the exception of psychomotor poverty syndromes, these lesion deficit models are not generally useful in schizophrenia. In terms of neuropsychology, many of the experiential symptoms and positive signs of schizophrenia can only be explained by considering one cognitive process in relation to another. For example, hallucinations can be construed as a misattribution of internally generated speech to an outside agency (4). This speaks to a failure to integrate the attribution of agency and inner speech. In other words, the symptoms and signs of schizophrenia do not generally represent a single deficit, but can be seen as resulting from the abnormal integration of two or more processes. In a similar vein, the disconnection hypothesis suggests that the neuronal dynamics underlying these symptoms are not due to a single regionally specific pathophysiology, but are expressed when two or more regions interact. This is not to say that the regions involved will not show region-specific abnormalities, but these abnormalities are secondary to a more pervasive problem.
THE DISCONNECTION HYPOTHESIS
Connections and plasticity
The key assumption here is that the pathophysiology of schizophrenia is expressed in terms of abnormal connections. Because synaptic connections are in a continual state of flux, this implies an abnormality of changes in connectivity, i.e. abnormal plasticity. The disconnection hypothesis is therefore, implicitly, a dysplastic hypothesis (5). The challenge is to identify the particular form of dysplasia that might underlie schizophrenia.
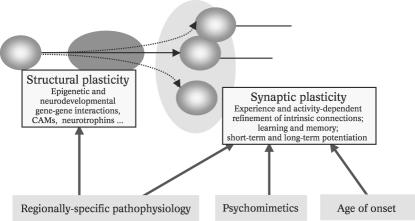
To understand functional disconnection, in its broadest sense, one has to appreciate the diversity of mechanisms that are responsible for establishing connections in the normal brain. These result from an interplay between genetic, epigenetic and activity or experience-dependent mechanisms. The emphasis in utero is clearly on epigenetic mechanisms, such as the interaction between the spatiotemporal topography of the developing cortical sheet, cell migration, gene expression and the mediating role of gene-gene interactions and gene products such as cell adhesion molecules (CAMs). Following birth, the broad schema of connections is progressively refined and remodelled with a greater emphasis on activity- and usedependent plasticity. These changes endure into adulthood, with ongoing reorganisation and experiencedependent plasticity that subserves behavioural adaptation and learning throughout life. In summary, there are two basic determinants of connectivity in the brain: a) structural plasticity, reflecting the interactions between the molecular biology of gene expression, cell migration and neurogenesis in the developing brain (these processes are expressions of plasticity at the cellular level and are usually neurodevelopmental in nature); b) synaptic plasticity, i.e., activity-dependent modelling of the pattern and strength of synaptic connections (this plasticity involves changes in the form, expression and function of synapses that endure throughout life; it subserves perceptual and procedural learning and memory).
Structural or synaptic plasticity?
Schizophrenia is a disorder that evidences a degree of specificity, in terms of functional, anatomical and neurotransmitter systems. This specificity could be explained by selective damage to cellular or molecular systems mediating either structural or synaptic plasticity. However, there are two simple facts that point to synaptic plasticity as the most likely target in schizophrenia (Figure 1). The first is that schizophrenic symptoms can be produced by psychomimetic drugs (6). This tells us immediately that the locus of abnormality is likely to be synaptic as opposed to cellular. This is because neurotransmitters act at synapses, not at the level of neurogenesis during development. Secondly, the fact that schizophrenia is expressed symptomatically in adulthood points to abnormal modulation of experience-dependent synaptic plasticity, as distinct from the induction and maintenance of connections though epigenetic mechanisms or indeed activity-dependent plasticity in utero. This does not preclude neurodevelopmental explanations for schizophrenia (7-9), but suggests that the mechanistic endpoint, of any putative aetiology, involves processes that are expressed post-developmentally.
Figure 1.
Processes determining connectivity
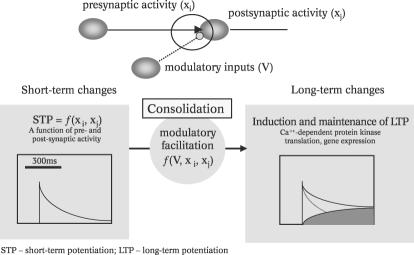
Short vs. long-term synaptic plasticity
Synaptic plasticity may be transient (e.g., short-term potentiation, STP or short-term depression, STD) or enduring (e.g., long-term potentiation, LTP, with early and late phases). In contrast to the short-term plasticity, longterm changes rely on protein synthesis, synaptic remodelling and infrastructural changes in cell processes (e.g., terminal arbours or dendritic spines [10]). These may be induced by local dynamics and may be influenced by other (modulatory) neurotransmitter systems (e.g., 11,12). It is useful to regard long-term changes as a consolidation of short-term changes (Figure 2).
Figure 2.
Synaptic plasticity: activity-dependent processes
From the perspective of the disconnection hypothesis, it is of no surprise that the neurotransmitter systems implicated in schizophrenia are exactly those that are responsible for modulating short-term changes in synaptic plasticity and their consolidation. The important role of Nmethyl- D-aspartate (NMDA) glutamate receptors in conferring voltage sensitivity on post-synaptic responses (short-term) and their necessary role in the induction of LTP (long-term) sit comfortably with glutaminergic theories of schizophrenic pathology (13,14). Voltage-sensitivity and implicit nonlinear effects have been elaborated, at a systems level, in terms of 'contextual co-ordination' (15). Late developmental changes in the expression of glutamate receptor subunits and concomitant changes in synaptic function provide a potentially exciting focus for molecular and cellular biology in schizophrenia research (16). The role of the ascending classical neuromodulatory transmitter systems such as dopamine (DA) and acetylcholine (ACh) in modulating short-term changes in efficacy at a synaptic and cell assembly level is well known (e.g., 17,18). There are several compelling accounts of how abnormal DA modulation might translate in cognitive terms (e.g., 19,20). However, these ascending systems also have a crucial role in modulating long-term associative plasticity, that may be even more important in elaborating and maintaining adaptive patterns of connections.
Synaptic consolidation and schizophrenia
There is considerable evidence to suggest that monoaminergic - DA, norepinephrine (NE) and serotonin (5HT) - and ACh neurotransmission facilitates either the induction or maintenance of long-term changes in synaptic strength. The three most compelling lines of evidence are modulation of a) experience-dependent changes in synaptic efficacy, b) behavioural plasticity and c) experimentally induced LTP. One neurodevelopmental example is the role of ACh in facilitating experience-dependent organisation of connections in striate cortex (11,21). Further evidence implicating ACh in the modulation of plasticity comes from the electrophysiological correlates of learning (22). These findings suggest that ACh is necessary for, and can modulate, associative plasticity in a learningrelated context. In short, the ascending neurotransmitter systems can exert a regulatory control over the translation of short- into long-term changes in connections that are associated with learning and memory.
From the perspective of theoretical neurobiology, in particular neuronal selection and reinforcement learning, this modulatory effect has profound implications for the way that adaptive connections can be established. Experimental evidence for reinforcement-specific responses in these systems is clear cut: for example, the experiments of Ljungberg et al (23) have demonstrated phasic discharges in the cells of origin of the dopaminergic system that are selective for reinforcing stimuli. Other models include intracranial self-stimulation and studies of emotional learning in animals (24-26).
Many of the disintegrative and autistic aspects of schizophrenic symptomatology can be viewed as a failure of emotional and social learning that is secondary to a fundamental failure of learning (27). However, it is more compelling to ask 'what would be the consequences of abnormal learning in adulthood?' Synaptic plasticity underlies both reinforcement learning in the context of emotional learning and representational learning involved in perceptual synthesis. The former learning difficulties could manifest as maladaptive responses to social contingencies, resembling those caused by inappropriate (disorganisation syndromes) or absent (psychomotor poverty) reinforcement. In terms of perceptual learning, the construction of high-order representations, that are used to explain sensory input, would be impoverished or inappropriate (reality distortion). The highest-order representations are probably the representations of the mental state of others, providing a nice connection with 'theory of mind' in schizophrenia (44). It is pleasing that a single mechanism can encompass the main aspects or sub-syndromes that constitute schizophrenia.
In conclusion, consolidation or reinforcement of synaptic plasticity underpins learning and must represent a clear candidate for pathophysiology in schizophrenia. This is important because recent advances in understanding the molecular biology of post-translational changes at the synapse that lead to long-term consolidation (e.g., 28,29) may afford much more detailed mechanistic hypotheses about schizophrenia.
IMPLICATIONS
Explanatory power and predictions
Tables 1 and 2 list some implications and predictions of the disconnection hypothesis that lend it explanatory power. Perhaps the most important is that it links anatomy, pathophysiology and neuropsychology in terms of specific systems. If the pathophysiology lies in synaptic plasticity, then its expression will be restricted to those anatomical systems with high plastic potential. These are exactly the limbic and paralimbic/associational systems in which abnormalities have been found in schizophrenia. Furthermore, the neurotransmitters targeted by psychomimetics or antipsychotics should be those implicated in synaptic plasticity, as they are. Finally, the neuropsychology of schizophrenia should be reducible to a failure of perceptual, social or emotional learning, which it can.
Table 1.
Explanatory power of the disconnection hypothesis of schizophrenia
| • | Explicit model for the necessary and conjoint influence of genetic and environmental factors |
| i.e. Abnormal molecular biology of experience-dependent plasticity associated with emotional learning | |
| • | Pathophysiology of processes that are expressed in the developed brain |
| - Psychomimetic drugs can induce psychotic symptoms | |
| - Schizophrenia is a disorder of adulthood | |
| • | Anatomical specificity - pathophysiology restricted to systems with a high plastic potential |
| (These include the medial temporal lobe [amygdala, hippocampus, parahippocampal gyrus] and the prefrontal cortex) | |
| - Systems with a role in learning and memory | |
| - Systems implicated in schizophrenia by imaging, cytoarchitectonic and histochemical studies | |
| • | Neurochemical specificity |
| - Posits a mechanistic role for the ascending neurotransmitter systems implicated in schizophrenia | |
| • | Disintegrative aspects of schizophrenic neuropsychology |
| - Impaired perceptual learning (Reality distortion) | |
| - Impaired social learning (Disorganisation) | |
| - Impaired precedural learning (Psychomotor poverty) | |
Table 2.
Predictions of the disconnection hypothesis of schizophrenia
| • | Abnormal functional integration, as measured by effective connectivity and coherence in neuroimaging |
| • | Impairment on tasks that emphasise temporal succession, reinforcement and new learning, perceptual or procedural |
| • | Demonstrable molecular abnormality in terms of how synaptic connections are consolidated during learning |
| • | Markers of functional disconnection seen only in systems that have high plastic potential |
| i.e. Systems that are involved in learning and memory | |
The practical importance of hypotheses like the disconnection hypothesis is that they focus research resources more efficiently. In my own field (functional neuroimaging), the implications of dysfunctional connectivity are clear. We must develop mathematical and empirical models of connectivity that can be applied in the context of schizophrenia research. In functional genomics, the issues are summarised nicely by Daniel Weinberger in the first issue of World Psychiatry: "Genes do not encode hallucinations, delusions or thought disorganisation per se. Genes determine the structure of simple molecules in cells, usually proteins, and these proteins affect how cells process and respond to stimuli. A variation in the sequence of a gene... could lead to changes in the interactions that cell has with other cells, in the connections and cell assemblies that develop, and in how such assemblies and networks operate as functional systems" (30). The scope of enquiry, developmental cell assemblies vs. dynamic cell assemblies, cellular vs. synaptic processes, short vs. long term plasticity, is clearly constrained by a number of key questions posed by the disconnection perspective.
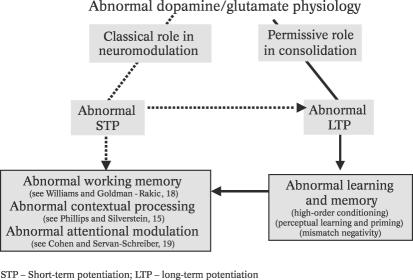
Outstanding questions
Two key questions are depicted schematically in Figures 3 and 4. The first pertains to whether schizophrenic pathophysiology involves short- or long-term synaptic plasticity. For example, it may be the case that abnormalities in DA or glutaminergic function, or indeed the interaction between them (31), cause abnormalities in STP or LTP. Knowing which mechanism is affected speaks to the behavioural paradigms one might employ. If STP were affected, then one would look for impaired working memory, attentional deficits and other abnormalities of highorder perceptual synthesis. These psychological deficits would be potentially important as surrogates for phenotyping subjects in genetic studies or as correlates of markers of DA or glutaminergic function. Conversely, if LTP were implicated, one might look to high-order conditioning paradigms and the psychophysics of perceptual learning (e.g., priming). The situation is, of course, complicated by the fact that abnormalities in LTP may be secondary to abnormal STP, and learning difficulties may be caused, not by a failure of consolidation, but by abnormalities in the short-term changes consolidated (dashed line in Figure 3). The bias presented in this paper is towards a consolidation problem in schizophrenia, where working memory and attentional deficits are seen as secondary to impaired learning. There are several lines of argument in favour of this, including the fact that the time course of antipsychotic action parallels the disappearance of experimentally induced LTP in animal models.
Figure 3.
Short vs. long-term (modulation vs. consolidation)
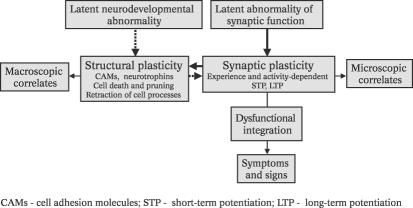
Figure 4.
Structural vs. synaptic (neurodevelopmental vs. functional)
An equally fundamental distinction is depicted in Figure 4. This is the distinction between neurodevelopmental accounts of schizophrenia, that invoke abnormal structural plasticity in development to explain disrupted synaptic connections, and those that posit molecular abnormalities in synaptic plasticity per se. The developmental perspective has been clearly articulated (see Robin Murray's article in a forthcoming issue of World Psychiatry). An explicit neurodevelopmental model for synaptic disconnection can be found in McGlashan and Hoffman (32). If schizophrenia is developmental, then focus on developmental markers of abnormal structural plasticity - e.g., magnetic resonance imaging (MRI) morphometry (33) - will be much more useful in genetic studies than those of synaptic plasticity. Furthermore, appropriate animal models of schizophrenia may be found in developmental anatomy. Conversely, if the mechanisms causing schizophrenic symptoms are expressed at the level of synaptic plasticity, markers of cellular plasticity will segregate less with the genotype than those of synaptic function. In this case, studying molecular mechanisms of synaptic consolidation in adults seems more sensible. Both etiological perspectives can explain the same outcomes (dashed and solid lines in Figure 4), but they differ profoundly in terms of suggesting what should be studied.
The developmental view is appealing, but framing schizophrenia as something like 'late-onset autism' does not explain how developmental abnormalities in anatomical connections, at the structural level, cause symptoms and dysfunctional integration mediated by synapses (or indeed how psychomimetics and antipsychotics work) (horizontal arrow in Figure 4). This explanation may not be easy for the neurodevelopmental hypothesis, because the developing brain is notoriously resistant to structural insults. However, having made a clear distinction between structural and synaptic plasticity, it should be noted that, although they are often viewed as unrelated, "they seem to be part of a common process that involves a CaMKIIdependent enhancement of synaptic strength" (29). In conclusion, although the bias of this paper is in favour of synaptic abnormalities (Figure 2), a resolution of the developmental issues is clearly important for directing future research.
CONCLUSION
This article has reviewed the disconnection hypothesis of schizophrenia and has presented a mechanistic account of how dysfunctional integration among neuronal systems might arise. The particular hypothesis put forward is that the pathophysiology of schizophrenia is expressed at the level of synaptic plasticity, specifically the consolidation of associative plasticity in those brain systems responsible for emotional learning and memory. This modulation is mediated by ascending neurotransmitter systems that a) have been implicated in schizophrenia and b) are known to be involved in consolidating synaptic plasticity. By reference to theoretical neurobiology, this pathophysiology can be understood as disrupting the reinforcement of adaptive behaviour in a way that is consistent with the disintegrative aspects of schizophrenic neuropsychology.
Acknowledgements
The author thanks his colleagues at the Wellcome Department of Imaging Neuroscience for invaluable discussion, particularly Chris Frith, and acknowledges support from the Wellcome Trust.
References
- 1.Bleuler E. Dementia Praecox or the group of schizophrenias. New York: International Universities Press; 1911. [Google Scholar]
- 2.Friston KJ. Frith CD. Schizophrenia: a disconnection syndrome? Clin Neurosci. 1995;3:89–97. [PubMed] [Google Scholar]
- 3.Gerstein GL. Perkel DH. Simultaneously recorded trains of action potentials: analysis and functional interpretation. Science. 1969;164:828–830. doi: 10.1126/science.164.3881.828. [DOI] [PubMed] [Google Scholar]
- 4.Frith CD. The cognitive neuropsychology of schizophrenia. Sussex: Lawrence Erlbaum; 1992. [Google Scholar]
- 5.Haracz JL. Neural plasticity in schizophrenia. Schizophr Bull. 1985;2:191–229. doi: 10.1093/schbul/11.2.191. [DOI] [PubMed] [Google Scholar]
- 6.Allen RW. Young SJ. Phencyclidine-induced psychosis. Am J Psychiatry. 1978;135:1081–1084. doi: 10.1176/ajp.135.9.1081. [DOI] [PubMed] [Google Scholar]
- 7.Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44:660–669. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- 8.Murray RM. Lewis SR. Is schizophrenia a developmental disorder? Br Med J. 1987;295:681–682. doi: 10.1136/bmj.295.6600.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bilder RM. Schizophrenia as a neurodevelopmental disorder. Curr Opin Psychiatry. 2001;14:9–15. [Google Scholar]
- 10.Rotshenker S. Multiple nodes and sites for the induction of axonal growth. Trends Neurosci. 1988;11:363–366. doi: 10.1016/0166-2236(88)90059-8. [DOI] [PubMed] [Google Scholar]
- 11.Bear MF. Singer W. Modulation of visual cortical plasticity by acetylcholine and noradrenaline. Nature. 1986;320:172–176. doi: 10.1038/320172a0. [DOI] [PubMed] [Google Scholar]
- 12.McGaugh JL. Neuromodulatory systems and the regulation of memory storage. In: Squire L, Butters N, editors. Neuropsychology of memory. New York: Guilford Press; 1992. pp. 386–401. [Google Scholar]
- 13.Deakin JFW. Slater P. Simpson MDC, et al. Frontal cortical and left temporal glutaminergic dysfunction in schizophrenia. J Neurochem. 1989;52:1781–1786. doi: 10.1111/j.1471-4159.1989.tb07257.x. [DOI] [PubMed] [Google Scholar]
- 14.Tamminga CA. Schizophrenia and glutaminergic transmission. Crit Rev Neurobiol. 1998;12:21–36. doi: 10.1615/critrevneurobiol.v12.i1-2.20. [DOI] [PubMed] [Google Scholar]
- 15.Phillips WA. Silverstein SM. Convergence of biological and psychological perspectives on cognitive co-ordination in schizophrenia. Submitted for publication. [DOI] [PubMed] [Google Scholar]
- 16.Singer W. Personal communication. 2002. [Google Scholar]
- 17.Mantz J. Milla C. Glowinski J, et al. Differential effects of ascending neurons containing dopamine and noradrenaline in the control of spontaneous activity and of evoked responses in the rat prefrontal cortex. Neuroscience. 1988;27:517–526. doi: 10.1016/0306-4522(88)90285-0. [DOI] [PubMed] [Google Scholar]
- 18.Williams GV. Goldman-Rakic PS. Modulation of memory fields by dopamine D1 receptors in prefrontal cortex. Nature. 1995;376:572–575. doi: 10.1038/376572a0. [DOI] [PubMed] [Google Scholar]
- 19.Cohen JD. Servan-Schreiber D. Context, cortex and dopamine: a connectionist approach to behavior and biology in schizophrenia. Psychol Rev. 1992;99:45–77. doi: 10.1037/0033-295x.99.1.45. [DOI] [PubMed] [Google Scholar]
- 20.Joel D. Weiner I. Striatal contention scheduling and the split circuit scheme of basal ganglia-thalamocortical circuitry: from anatomy to behaviour. In: Miller R, editor; Wickens JR, editor. Conceptual advances in brain research: brain dynamics and the striatal complex. London: Harwood Academic; 1999. pp. 209–236. [Google Scholar]
- 21.Brocher S. Artola A. Singer W. Agonists of cholinergic and noradrenergic receptors facilitate synergistically the induction of long-term potentiation in slices of rat visual cortex. Brain Res. 1992;573:27–36. doi: 10.1016/0006-8993(92)90110-u. [DOI] [PubMed] [Google Scholar]
- 22.Metherate R. Weinberger NM. Acetylcholine produces stimulus specific receptive field alterations in cat auditory system. Brain Res. 1989;480:372–377. doi: 10.1016/0006-8993(89)90210-2. [DOI] [PubMed] [Google Scholar]
- 23.Ljungberg T. Apicella P. Schultz W. Responses of monkey dopamine neurones during learning of behavioural reactions. J Neurophysiol. 1992;67:145–163. doi: 10.1152/jn.1992.67.1.145. [DOI] [PubMed] [Google Scholar]
- 24.Cador M. Robbins TW. Everitt BJ. Involvement of the amygdala in stimulus-reward associations: interaction with the ventral striatum. Neuroscience. 1989;30:77–86. doi: 10.1016/0306-4522(89)90354-0. [DOI] [PubMed] [Google Scholar]
- 25.McGaugh JL. Neuroscience - Memory - a century of consolidation. Science. 2000;287:248–251. doi: 10.1126/science.287.5451.248. [DOI] [PubMed] [Google Scholar]
- 26.White NM. Milner PM. The psychobiology of reinforcers. Ann Rev Psychol. 1992;43:443–471. doi: 10.1146/annurev.ps.43.020192.002303. [DOI] [PubMed] [Google Scholar]
- 27.Friston KJ. The disconnection hypothesis. Schizophr Res. 1998;30:115–125. doi: 10.1016/s0920-9964(97)00140-0. [DOI] [PubMed] [Google Scholar]
- 28.Frey U. Morris RGM. Synaptic tagging and long-term potentiation. Nature. 1997;385:533–536. doi: 10.1038/385533a0. [DOI] [PubMed] [Google Scholar]
- 29.Lisman J. Schulman H. Cline H. The molecular basis of CaMKII function in synaptic and behavioural memory. Nature Rev Neurosci. 2002;3:175–190. doi: 10.1038/nrn753. [DOI] [PubMed] [Google Scholar]
- 30.Weinberger DR. Biological phenotypes and genetic research on schizophrenia. World Psychiatry. 2002;1:2–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Levine MS. Li Z. Cepeda C, et al. Neuromodulatory actions of dopamine on synaptically-evoked neostriatal responses in slices. Synapse. 1996;24:65–78. doi: 10.1002/syn.890240102. [DOI] [PubMed] [Google Scholar]
- 32.McGlashan TH. Hoffman RE. Schizophrenia as a disorder of developmentally reduced synaptic connectivity. Arch Gen Psychiatry. 2000;57:637–648. doi: 10.1001/archpsyc.57.7.637. [DOI] [PubMed] [Google Scholar]
- 33.Woodruff PW. McManus IC. David AS. Meta-analysis of corpus callosum size in schizophrenia. J Neurol Neurosurg Psychiatry. 1995;58:457–461. doi: 10.1136/jnnp.58.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]