Reason for posting: Raloxifene is used for the treatment and prevention of osteoporosis. It is a selective estrogen-receptor modulator with estrogen-agonist effects on bone and lipid metabolism but not the breasts and uterus. The drug's effect on a woman's risk of cardiovascular events and risk of invasive breast cancer was assessed in the RUTH (Raloxifene Use for The Heart) trial. The drug's manufacturer recently disclosed that women taking the drug in the trial had an increased risk of death from stroke.1
The drug: Raloxifene is a benzothiophene compound taken orally once a day. It undergoes significant first-pass metabolism to glucuronide conjugates. Ninety-five percent of the drug circulates protein-bound, and it is mostly excreted in the feces. As with estrogen, raloxifene's effects occur when the drug binds tightly to estrogen receptors, which alters gene transcription in susceptible cells. Raloxifene's bone effects appear to be mediated through osteoblasts, which results in the promotion of bone deposition in a manner similar to that of estrogen (rather than the osteoclast inhibition seen with other therapies such as bisphosphonates). Raloxifene is less effective than estrogen at promoting bone deposition but is more effective than placebo at increasing bone mineral density, and it is used to both treat and prevent osteoporosis in postmenopausal women.
Common adverse effects include vasodilation (hot flushes), affecting about 10%–25% of users, and leg cramps, affecting about 7%. Other significant adverse effects include an increased risk, particularly in the first 4 months of therapy, of venous thrombosis, including superficial phlebitis, deep vein thrombosis and pulmonary embolism. Women taking the drug do not appear to be at increased risk of endometrial or ovarian cancer and may be at decreased risk of breast cancer.
Raloxifene increases serum levels of high-density lipoprotein and apolipoprotein A-I and decreases levels of total cholesterol, low-density lipoprotein, fibrinogen, apolipoprotein B and lipoprotein (a). It does not appear to alter C-reactive protein levels.
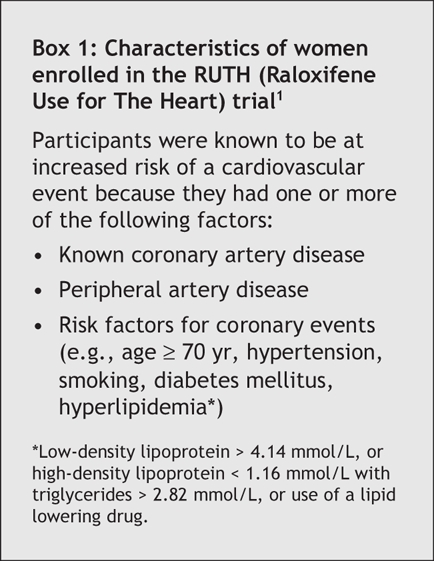
The RUTH trial remains unpublished. According to the drug's manufacturer,1 the trial enrolled more than 10 000 postmenopausal women (mean age 67 years), all of whom were known to have heart disease or to be at high risk of a coronary event (Box 1). The women were randomly assigned to receive either 60 mg/d of raloxifene at the standard dose or a placebo and were followed for up to 7 years. The incidence of fatal and nonfatal stroke, myocardial infarction (MI) and acute coronary syndromes as well as overall (all-cause) mortality was tracked. Clinical details (e.g., rates of smoking, cardiovascular risk factors and stroke risk factors such as atrial fibrillation) in both groups are sparse in the current advisory. Nevertheless, cardiovascular mortality, all-cause mortality and the incidence of nonfatal stroke, MI and hospital admission because of acute coronary syndromes is stated to be no different between those taking the drug and those taking the placebo.1
Box 1.
In contrast, however, the rate of fatal stroke is stated to have been higher in the raloxifene group than in the placebo group (2.2 per 1000 women using raloxifene per year v. 1.5 per 1000 women using placebo per year; p = 0.0499 [no confidence intervals were stated]).1 This means that about 1 in 455 women in the trial taking raloxifene would have had a stroke in a year, as compared with only 1 in 667 women in the trial taking placebo. In terms of the number needed to harm, 1428 postmenopausal women at risk of a cardiovascular event would have to be treated with the drug before 1 woman would have a treatment-related fatal stroke. The reasons for this effect, if it is real, are unclear.
What to do: Raloxifene should not be used to reduce a woman's risk of cardiovascular disease. Women prescribed the drug should be warned about the potential risk of stroke. Stroke risk calculators (e.g., Framingham calculators) allow women at high risk of stroke to be identified. In such women, as well as those with characteristics that would have allowed them entry into the trial (Box 1) and those with a prior history of cerebrovascular events (including transient ischemic attacks) or atrial fibrillation, the choice of alternate therapies for osteoporosis seems wise.
Eric Wooltorton CMAJ
REFERENCE
- 1.Association of Evista (raloxifene hydrochloride) with increased risk of mortality due to stroke in postmenopausal women at increased risk for cardiovascular disease: preliminary results from the RUTH trial [Dear Health Care Professional letter]. Toronto: Eli Lilly Canada Inc.; 2006 May 18. Available: www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/prof/2006/evista_hpc-cps_e.html (accessed 2006 Jun 20).


