Abstract
CONTEXT
Previous studies have demonstrated a strong association between minority race, low socioeconomic status (SES), and lack of potential access to care (e.g., no insurance coverage and no regular source of care) and poor receipt of health care services. Most studies have examined the independent effects of these risk factors for poor access, but more practical models are needed to account for the clustering of multiple risks.
OBJECTIVE
To present a profile of risk factors for poor access based on income, insurance coverage, and having a regular source of care, and examine the association of the profiles with unmet health care needs due to cost. Relationships are examined by race/ethnicity.
DESIGN
Analysis of 32,374 adults from the 2000 National Health Interview Survey.
MAIN OUTCOME MEASURES
Reported unmet needs due to cost: missing/delaying needed medical care, and delaying obtaining prescriptions, mental health care, or dental care.
RESULTS
Controlling for personal demographic and community factors, individuals who were low income, uninsured, and had no regular source of care were more likely to miss or delay needed health care services due to cost. After controlling for these risk factors, whites were more likely than other racial/ethnic groups to report unmet needs. When presented as a risk profile, a clear gradient existed in the likelihood of having an unmet need according to the number of risk factors, regardless of racial/ethnic group.
CONCLUSION
Unmet health care needs due to cost increased with higher risk profiles for each racial and ethnic group. Without attention to these co-occurring risk factors for poor access, it is unlikely that substantial reductions in disparities will be made in assuring access to needed health care services among vulnerable populations.
Keywords: race/ethnicity, SES, vulnerability, access to care, disparities
The United States has adopted a national priority of reducing or eliminating disparities in health and health care by 2010.1 Minority race and ethnicity and having low socioeconomic status (SES) remain critical barriers to obtaining care.2–4 National strategies to reduce disparities in the health of vulnerable populations have focused on increasing potential access—resources such as health insurance and a regular source of care—that enables the use of health services.5,6 However, given that health care is not equally financially available to all individuals in the United States, the potential for delaying or missing needed care is intensified, particularly among vulnerable populations.7
Vulnerable populations are defined as those at greater risk for poor health status and health care access. Many efforts have been made to characterize vulnerable groups, including by diseases (e.g., HIV), age groups (e.g., the elderly), and demographics (e.g., homeless individuals).8 Regardless of how they are categorized, vulnerable populations generally include racial and ethnic minorities, low SES populations, and those without adequate potential access to care (e.g., the uninsured or those without a regular source of care). Yet, health care initiatives to reduce the barriers created by vulnerability rarely recognize the common overlap of risk factors, and few studies have examined the combined influences of multiple risks on obtaining needed health care services.
Previous studies have indelibly linked minority race/ethnicity,9–13 low SES,14–20 and not having potential access21–29 with poor receipt of health care services for adults. The findings have been so salient and persistent that now nearly every national health survey routinely collects and reports most aspects of health care utilization according to race/ethnicity, SES, and often by health insurance coverage. While research frequently aims to examine independent contributions of risk factors, in order to tease out pathways through which disparities persist, few studies have adopted more pragmatic models of vulnerability that account for common clustering of multiple risk factors for poor access.
This study operationalizes the concept of vulnerability using profiles that account for these multiple risks. The risk factors included in this study reflect both predisposing (i.e., race/ethnicity) and enabling factors (i.e., income, health insurance, and regular source of care) that are associated with access to care.5 Risk profiles are assembled from data on income, health insurance coverage, and having a regular source of care (reflecting those factors that are modifiable through policy) and examined by race/ethnicity (a nonmodifiable factor) so that differences in the influences of risk factors across racial/ethnic groups can be readily detected. These risk profiles are examined in relation to five reported unmet health care needs due to the costs of care, including missed or delayed medical care, prescriptions, mental health, and dental care. The analyses are adjusted for demographic and community factors that have been associated with access to care.
METHODS
Study Design
This study uses data on 32,374 adults ages 18 and over from the publicly released Sample Adult Core of the 2000 National Health Interview Survey (NHIS) that was conducted by the National Center for Health Statistics (NCHS) at the Centers for Disease Control (CDC). Discussion of the complex survey design of NHIS is available elsewhere.30 Several of the population groups were oversampled, including Hispanics and African Americans. Within each family participating in the NHIS, one sample adult is selected to complete the Sample Adult Core. Additional data on delays for these adults were also obtained by linking with the NHIS Person File. Children (under 18) were excluded from this study because the health needs and health care financing and delivery systems designed for children are quite different from those of adults.31
Conceptual Framework
The risk factors for poor access to care in this study are low income, not having health insurance, and lacking a regular source of care. The selection of these factors was based on the access to care models developed by Andersen and Aday,6 and reflect those enabling factors that are the most amenable to policy changes. Enabling factors are the means that individuals have to obtain health services. Race/ethnicity is a predisposing factor (i.e., a sociodemographic characteristic of a person that indicates the propensity to use medical services), but was used mostly for stratification rather than as part of the multiple risk profiles.
Of the enabling risk factors for poor access, both income and health insurance coverage reflect the resources to pay for needed health services, such as actual service costs and insurance copayments. Having a regular source of care means a person has established a link with an accessible source of health services and potentially someone from whom they can receive their needed care. A regular source of care may also create demand for services by reminding adults of the need for these services and initiating their delivery. Though a regular source of care is often used as a measure of access itself, it is generally thought to be an enabling factor when the end point is the receipt of needed services rather than simply entry into care.6
Measures
The study's independent variables were risk factors for poor access including race and ethnicity, income, insurance coverage, and having a regular source of care. Adults reported their race/ethnicity in two separate questions about patient race and whether they were of Hispanic or Latino ethnicity. Analytic categories include white (non-Hispanic), African American (non-Hispanic), Asian (Asian, Pacific Islander, non-Hispanic), and Hispanic (answering Hispanic or Latino ethnicity and of any race). Income was divided into high and low with 200% of the federal poverty line as the cutoff. Because of the large proportion of the sample (∼25%) that did not report income information, an analytic category for these missing values was included so as not to lose these individuals during multivariate regression analysis; but for simplicity this category was not presented in the regression results. Insurance coverage was coded as private coverage, public coverage (e.g., Medicaid or Medicare), other coverage, and uninsured. The presence of a regular source of care was measured by asking the adult, “Is there a place that you usually go to when you are sick or need advice about your health?” The responses were dichotomized (yes/no).
The study's dependent variables—unmet health care needs due to costs—are assessed through 5 questions about delayed or missed care due to affordability in the past 12 months. The first question asked adults, “Was there any time when you needed medical care, but did not get it because you couldn't afford it?” Second, adults were asked, “Has medical care been delayed for you because of worry about the cost?” Adults were also asked, “Was there any time when you needed any of the following but didn't get it because you couldn't afford it: 1) prescription medicines, 2) mental health care or counseling, and 3) dental care (including check-ups)?” Delayed or missed care for each of these topics was measured dichotomously, yes or no. Responses of “don't know” were excluded from the analyses. These measures are frequently used in studies of access to care.32–35
Study covariates included respondent age (18–64 years and 65+), gender, education (less than high school, high school, and bachelor's degree or higher), marital status, employment status, insurance coverage and type (private, public, and uninsured), and metropolitan statistical area (MSA vs non-MSA).
Analysis
Analyses were performed with SUDAAN (Research Triangle Park,NC,USA) to account for the multistage, stratified cluster sampling of the 2000 NHIS. All estimates presented in the text and tables were weighted to reflect national population totals. First, characteristics of the population are presented by race and ethnicity. Second, 5 logistic regression models were developed to predict each unmet health care need according to the risk factors for poor access (i.e., race/ethnicity, income, health insurance, and regular source of care) independently. Odds ratios and confidence intervals are presented.
Third, we present 5 graphs showing the bivariate relationships between the risk profiles and the frequency of each unmet need (Figs. 1–5). A sixth figure presents the relationship between the 7 unique possible combinations of the 3 risk factors and their bivariate relationship with 1 of the measures of unmet needs (did not get needed medical care) to show the relative contributions of different combinations of risks with unmet needs. We examined the relationship of the combinations with the other measures of unmet needs (data not shown) and found similar patterns of relationships, so the results are only presented for the 1 measure of unmet needs.
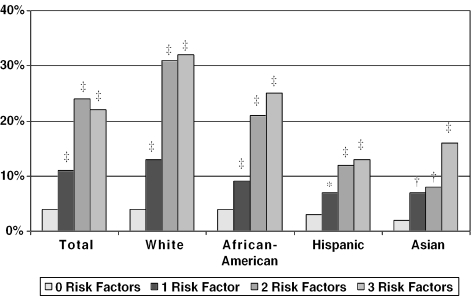
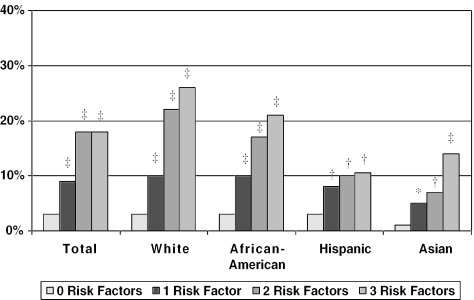
Figure 1.
Delayed needed medical care by number of risk factors. *P <.05, †P <.01, ‡P <.001 for the vulnerability profile compared to 0 risk factors within each racial/ethnic group.
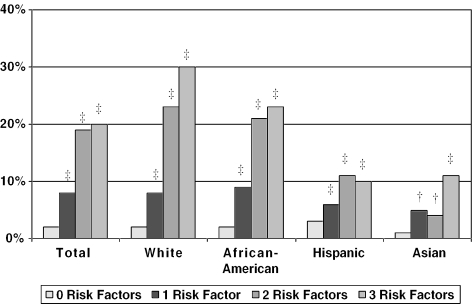
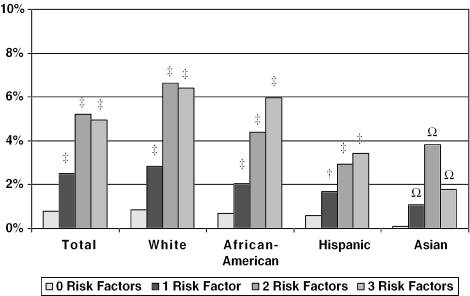
Figure 5.
Delayed dental care by number of risk factors. †P <.01, ‡P <.001 for the vulnerability profile compared to 0 risk factors within each racial/ethnic group. Columns with (Ω) may not be stable estimates due to a small number of respondents.
RESULTS
Table 1 presents the characteristics of the national sample of adults in our study. The majority of respondents were under age 65, and slightly more likely to be female. Hispanics and African Americans were significantly more likely than whites and Asians to have less than a high school education (45.8% and 24.2% vs 13.3% and 10.7%). Hispanics were most likely to be uninsured (37.3%) compared to 19.8% of African Americans, 16.5% of Asians, and 10.3% of whites. Hispanics were also much less likely than other racial and ethnic groups to have a regular source of care (70.9% vs 81.7% of Asians, 84.9% of African Americans, and 88.2% of whites). Summarizing these risk factors as a profile, Hispanics were more likely than other groups to have, for example, 2 or more risk factors (36.0%) compared to African Americans (19.7%), Asians (17.7%), and whites (9.66%).
Table 1.
Characteristics of the National Population by Race and Ethnicity (N =32,374)
| Study Variable | Asian N =861 % (SE) | African-American N =4,546 % (SE) | Hispanic N =5,377 % (SE) | White N =21,318 % (SE) |
|---|---|---|---|---|
| Vulnerability characteristics | ||||
| Income* | ||||
| Low income | 22.27 (1.87) | 33.62 (1.08) | 39.74 (1.00) | 17.38 (0.36) |
| High income | 55.35 (2.35) | 41.64 (1.02) | 38.12 (1.01) | 58.77 (0.47) |
| Missing | 22.37 (1.79) | 24.74 (0.95) | 22.14 (1.02) | 23.86 (0.46) |
| Health insurance* | ||||
| Private coverage | 73.68 (1.87) | 59.67 (1.09) | 47.70 (0.97) | 79.28 (0.35) |
| Public coverage | 9.85 (1.24) | 20.54 (0.87) | 15.02 (0.59) | 10.59 (0.25) |
| Uninsured | 16.48 (1.37) | 19.78 (0.75) | 37.28 (1.11) | 10.13 (0.29) |
| Have RSC or not* | ||||
| Have RSC | 81.71 (1.37) | 84.88 (0.66) | 70.87 (1.10) | 88.22 (0.30) |
| No RSC | 18.29 (1.37) | 15.12 (0.66) | 29.13 (1.10) | 11.78 (0.30) |
| Demographic factors | ||||
| Age group, y* | ||||
| 18–64 | 91.48 (1.25) | 88.25 (0.56) | 91.00 (0.63) | 81.64 (0.34) |
| 65+ | 8.52 (1.25) | 11.75 (0.56) | 9.00 (0.63) | 18.36 (0.34) |
| Female gender† | 49.69 (2.17) | 55.56 (1.02) | 50.71 (0.93) | 51.94 (0.39) |
| Marital status* | ||||
| Married | 64.93 (1.97) | 37.05 (0.90) | 58.37 (0.78) | 61.40 (0.46) |
| Not married | 35.07 (1.97) | 62.50 (0.90) | 41.63 (0.78) | 38.60 (0.46) |
| Education* | ||||
| Less than high school | 10.66 (1.42) | 24.18 (0.87) | 45.79 (1.04) | 13.29 (0.32) |
| High school graduate | 44.36 (2.15) | 61.68 (0.86) | 45.59 (0.97) | 61.19 (0.42) |
| Bachelor's+ | 44.98 (2.08) | 14.14 (0.71) | 8.63 (0.54) | 25.52 (0.42) |
| Employment status | ||||
| Employed | 67.97 (2.03) | 64.59 (0.94) | 66.37 (0.88) | 65.76 (0.41) |
| Unemployed | 32.03 (2.03) | 35.41 (0.94) | 33.63 (0.88) | 34.24 (0.41) |
| Health status* | ||||
| Poor health | 6.01 (0.86) | 16.71 (0.65) | 13.61 (0.65) | 10.66 (0.26) |
| Good health | 93.99 (0.86) | 83.29 (0.65) | 86.39 (0.65) | 89.34 (0.26) |
| Community factors | ||||
| In MSA or not* | ||||
| In MSA | 95.13 (1.48) | 86.13 (1.35) | 92.02 (0.87) | 75.44 (0.54) |
| Not in MSA | 4.87 (1.48) | 13.87 (1.35) | 7.98 (0.87) | 24.56 (0.54) |
| Region* | ||||
| Northeast | 22.27 (1.78) | 17.43 (0.80) | 15.88 (0.84) | 20.13 (0.41) |
| Midwest | 12.19 (1.48) | 19.50 (0.93) | 7.80 (0.75) | 29.24 (0.46) |
| South | 18.57 (1.74) | 55.80 (1.27) | 34.80 (1.31) | 33.97 (0.50) |
| West | 46.97 (2.51) | 7.27 (0.46) | 41.51 (1.34) | 16.66 (0.42) |
| Combined risk factors§ | ||||
| 0 risk factors | 53.86 (2.35)‡ | 41.41 (1.25)‡ | 30.79 (1.04)‡ | 62.65 (0.51) |
| 1 risk factor | 28.42 (1.99)‡ | 38.94 (1.14)‡ | 33.21 (0.94)‡ | 27.70 (0.45) |
| 2 risk factors | 13.43 (1.45)‡ | 14.34 (0.71)‡ | 22.53 (0.92)‡ | 7.59 (0.26) |
| 3 risk factors | 4.29 (0.81)‡ | 5.31 (0.40)‡ | 13.47 (0.80)‡ | 2.07 (0.13) |
P <.001.
P <.01 for the χ2 across racial/ethnic groups.
P <.001 for the χ2 of the number of risk factors for a given racial/ethnic group compared to white.
The number of vulnerabilities a person has (having low income, no insurance coverage, and lacking a regular source of care).
SE, standard error; RSC, regular source of care; MSA, metropolitan statistical area.
Table 2 presents the independent effects of risk factors on the likelihood of having delayed or missed health care. Controlling for race and ethnicity and other study covariates, each risk factor was independently associated with greater odds of having unmet needs. Adults with low income were more likely than those with high income to delay needed medical care, not receive needed medical care, not get a prescription, not get mental health care, and not get dental care (odds ratios ranging from 1.50 to 2.12, all statistically significant with all 95% lower confidence intervals ranging no lower than 1.31). Lacking health insurance was more strongly associated with each delayed and missed care variable (odds ratios from 3.94 to 6.92, all statistically significant with all 95% lower confidence intervals ranging no lower than 3.72). Lacking a regular source of care was also associated with greater likelihood of delayed or missed medical and dental care and delays filling a prescription, but was not significantly associated with receipt of mental health care. Interestingly, after adjustment for the study covariates, whites were much more likely than other racial/ethnic groups to report each unmet need.
Table 2.
Logistic Regression Predicting Delayed or Missed Care Due to Costs (N =32,374)
| Delayed Needed Medical Care OR (95% CI) | Did Not Get Needed Medical Care OR (95% CI) | Delayed Filling a Prescription OR (95% CI) | Delayed Mental Health Care OR (95% CI) | Delayed Dental Health Care OR (95% CI) | |
|---|---|---|---|---|---|
| Race/ethnicity (ref: white) | |||||
| African-American | 0.56 (0.49 to 0.65) | 0.76 (0.65 to 0.88) | 0.73 (0.63 to 0.85) | 0.57 (0.42 to 0.78) | 0.66 (0.57 to 0.76) |
| Hispanic | 0.39 (0.32 to 0.46) | 0.45 (0.37 to 0.55) | 0.47 (0.40 to 0.57) | 0.41 (0.30 to 0.54) | 0.46 (0.40 to 0.54) |
| Asian | 0.40 (0.26 to 0.62) | 0.36 (0.22 to 0.60) | 0.42 (0.26 to 0.68) | 0.30 (0.11 to 0.79) | 0.41 (0.28 to 0.60) |
| Vulnerability factors | |||||
| Low income (ref: high) | 1.50 (1.31 to 1.71) | 1.58 (1.36 to 1.84) | 2.12 (1.79 to 2.51) | 1.77 (1.34 to 2.34) | 1.65 (1.44 to 1.89) |
| Health insurance (ref: private) | |||||
| Public coverage | 1.67 (1.41 to 1.98) | 1.93 (1.58 to 2.35) | 1.65 (1.37 to 1.99) | 1.35 (0.96 to 1.90) | 1.89 (1.61 to 2.22) |
| Uninsured | 6.13 (5.30 to 7.09) | 7.33 (6.24 to 8.62) | 4.55 (3.81 to 5.45) | 4.94 (3.72 to 6.56) | 4.69 (4.13 to 5.32) |
| No RSC (ref: having an RSC) | 1.31 (1.14 to 1.51) | 1.37 (1.17 to 1.60) | 1.20 (1.03 to 1.40) | 1.14 (0.87 to 1.49) | 1.44 (1.27 to 1.63) |
Models are adjusted for age, gender, marital status, education, employment, health status, MSA, and geographic region.
The “missing” category for income was included in the regression but is not presented in this table for simplicity.
OR, odds ratio; CI, confidence interval; RSC, regular source of care; MSA, metropolitan statistical area.
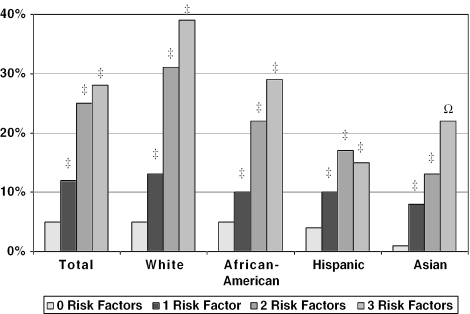
Figures 1–5 show the relationship between the risk profiles and the likelihood of 1) delaying needed medical care, 2) not getting needed medical care, 3) delaying filling a prescription, 4) delaying mental health care, and 5) delaying dental care. The figures, which present the relationships for the total sample and for each racial/ethnic group separately, show a stepwise increase in the likelihood of delaying or missing care regardless of race or ethnicity. The largest jump in the frequency of unmet needs is during the transition from 1 to 2 risk factors. While a single risk factor frequently doubles the likelihood of having an unmet need compared to zero risk factors, adding a second risk factor often more than triples the likelihood of having an unmet need compared to zero risk factors. The addition of a third risk factor appears to contribute less to the likelihood of having an unmet need.
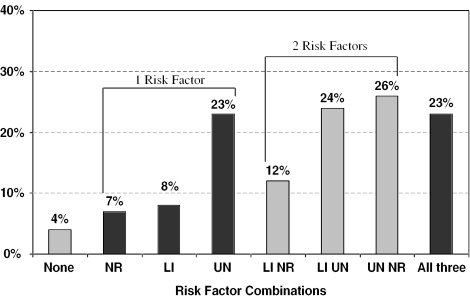
Figure 6 shows the relationship between all possible combinations of risk factors and delaying needed medical care. The results show that, in general, individuals with any 1 risk factor are more likely to have delayed medical care than individuals with no risk factors. However, within the 1–risk factor category, individuals who are uninsured are much more likely to delay medical care than individuals who are low income or do not have a regular source of care. This same pattern is found within the 2–risk factor category such that individuals with combinations of uninsured with either low income or no regular source of care are more likely to delay medical care than the third combination that does not include being uninsured. Being uninsured alone and or any other combination of risk factors with lack of health insurance appears to be a major driving force for delaying needed medical care. The results are similar for the other measures of unmet needs.
Figure 6.
Delayed medical care by all combinations of risk factors. NR, no regular source of care; LI, income less than 200% of federal poverty line; UN, uninsured.
DISCUSSION
This study demonstrates that vulnerability can be operationalized as a profile of multiple enabling risk factors to present a more comprehensive view of unmet health care needs due to cost. Regardless of race/ethnicity, having low income, lacking insurance coverage, and not having a regular source of care combine to create substantial barriers to accessing needed health services. This study further demonstrates that a substantial proportion of U.S. adults (about 1 in 5) has multiple risk factors for unmet health care needs, and that these risk factors create up to 5-fold differences in rates of unmet needs (e.g., delayed medical care) between the highest and lowest profiles, regardless of race/ethnicity. This view of vulnerability in the United States is even more striking when we consider that individuals with poor health status are among the most likely to report delayed or missed care.
Interestingly, our study shows that both before and after adjusting for the study covariates, whites were actually more likely than other racial and ethnic groups studied to report delayed or missed care due to cost for each type of health service. After controlling for each other vulnerability factor, minorities had 0.40 to 0.80 lower odds of reporting delayed or missed care than whites. Because minorities have lower income, are more likely to be uninsured, are less likely to have a regular source of care, and have poorer health status than whites, it is difficult to believe that whites are more likely to have delayed or missed needed care.
One possible explanation for this finding is that whites may have different ideas or perceptions of health needs, or a greater belief in their ability to access care than other racial and ethnic groups. This may contribute to greater reporting of delayed or missed care because whites may feel more empowered to obtain care and speak up when their health care needs are not being met. It is also possible that minorities may have lower expectations than whites for health care (owing to a long history of difficult interactions with the health care system) and consequently are less likely to report an unmet need when a health need is not addressed.36 Lower health literacy (including where to go to obtain needed health services) among some racial/ethnic minority groups may also contribute to lower reported rates of unmet needs.37,38
Lacking a sense of empowerment to address health care needs may stem from several sources. Minorities are less likely to have health insurance, and more likely to have public coverage (for which there is little cost sharing), both of which may discourage a sense of an entitlement to care. Similarly, racial/ethnic minorities may be more likely to believe that the health system is unable to meet their health needs (resulting in lower expectations for care) due to discrimination, distrust, negative prior interpersonal experiences in care, or poorer quality of care.39–45
Adding to the interpretation of the data, several sociodemographic factors were also strongly associated with unmet needs due to cost (data not shown). In particular, poor health status was associated with a higher likelihood of an unmet need (odds ratios ranging from 2.43 to 4.06; all P <.001), suggesting that those with the greatest health care needs are not having them adequately met. Younger age, female gender, not being married, and having lower education were all independently associated with a higher odds of having an unmet need for most types of care. These relationships may suggest that differing perceptions of health needs may contribute to differences in reports of unmet needs across groups.
Low income, no health insurance coverage, and lacking a regular source of care are closely related risk factors that build upon each other to influence the likelihood of having an unmet health need due to cost. From both the logistic regression and the comparison of all the different combinations of risk factors, lacking health insurance appears to have the strongest association with unmet health needs, followed by family income and having a regular source of care. There may be several different mechanisms underlying the effects of these factors on obtaining needed care. For example, health insurance and income influence the ability to purchase health care services and are essential factors in assuring access to a range of primary and specialty care services. Having a regular source of care means that, above and beyond the financial ability to obtain care, a person identifies with a health care provider or place of care from which they have been able to readily obtain health services.
Overall, our study suggests that the potential determinants of delayed or missed care are multifactorial. Reducing disparities in obtaining needed health care services for vulnerable populations will, therefore, likely require multiple clinical or policy strategies. To ensure that racial/ethnic minorities obtain needed health care services, health systems may need to address language difficulties, cultural beliefs, and practices, and ensure that all adults feel empowered to obtain care. Reducing disparities associated with SES will require attention to assuring health insurance coverage, but may also require attention to factors not assessed in this study such as the level of education (which is related to income, health behaviors, and health care seeking) and occupation (which may limit the flexibility in where and when health care services are sought).
Furthermore, providing insurance coverage to the uninsured continues to be an important enabling factor in obtaining care, but is an incomplete solution to assuring that needed health care services are obtained.21,28 Efforts to propagate the concept of primary care and encourage the linkage of adults with a regular source of care or “medical home” build upon health insurance to improve potential access to care,46 though there remains debate about what type of regular source of care is the most effective (e.g., the setting of care, and linkage with a specific provider vs team care).23,29,47
There are several limitations to this study. First, the risk factors included in the vulnerability profiles were meant to be illustrative and not exhaustive. The risk factors reflect primarily (though not entirely) financial risks for not obtaining needed care. Other risk factors that could be taken into account including demographics such as language, educational level, and marital status; provider factors such as availability, accessibility, and continuity; and health plan factors such as cost sharing and reimbursement for delivery of primary care services. We selected 4 key risk factors based on demonstrated associations with access to care in the literature. Other studies might consider combining additional or different risk factors to examine the robustness of these findings.
Second, the measures of unmet needs assess delayed or missed care due to costs but do not assess delayed or missed care for other potential reasons such as a lack of transportation, availability of providers, or discrimination. The data are also reported by respondents and may not accurately represent the presence of unmet health care needs. Because the unmet need questions in the NHIS did not provide guidance on what constitutes a health need, the unmet need measures may be less likely to capture conditions that are less easily recognized by patients as requiring medical care (e.g., obesity, hypertension). Perceived health needs may be susceptible to different personal conceptualizations of health needs and beliefs regarding what services should be received. On the other hand, health care should always meet the needs of individuals, and because individual perceptions of health needs are the strongest drivers of care seeking, it is important to assess how these patient-perceived needs are being met.
Third, due to the limitations of secondary data analysis, the study was not able to account for managed care insurance type. Managed care plans are constantly studied for their influence on access to care, particularly for vulnerable populations.48–52 Because most Medicaid plans have switched to managed care, racial/ethnic minorities and lower-income adults are more frequently enrolled in managed care plans, and thus may be most strongly affected by managed care in analyses of unmet needs. Fourth, we did not account for more complex subgroupings of race/ethnicity or SES (i.e., through education and employment) that may reveal more complex findings than are presented here.53–56
In conclusion, this study demonstrates that vulnerability may be operationalized to account for multiple risk factors through the use of profiles. These profiles revealed a distinct dose-response relationship between the number of enabling risks and unmet health care needs due to cost. Because of these interactive risks, strategies to reduce disparities for vulnerable populations should simultaneously address these co-occurring risks, rather than continue fragmented approaches of targeting single risk factors. More integrative approaches will likely require greater partnerships between medical and social sectors in designing interventions for vulnerable populations. Barring these integrated approaches, it is unlikely that substantial gains will be made in improving access to needed health and dental services among vulnerable populations.
Figure 2.
Did not get needed medical care by number of risk factors. †P <.01, ‡P <.001 for the vulnerability profile compared to 0 risk factors within each racial/ethnic group.
Figure 3.
Delayed filling a prescription by number of risk factors. *P <.05, †P <.01, ‡P <.001 for the vulnerability profile compared to 0 risk factors within each racial/ethnic group.
Figure 4.
Delayed mental health care by number of risk factors. †P <.01, ‡P <.001 for the vulnerability profile compared to 0 risk factors within each racial/ethnic group. Columns with (Ω) may not be stable estimates due to a small number of respondents.
REFERENCES
- 1.Healthy People 2010. Washington, DC: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- 2.Smedley B, Stith A, Nelson A, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 3.Satcher D. Eliminating racial and ethnic disparities in health:the role of the ten leading health indicators. J Natl Med Assoc. 2000;92:315–8. [PMC free article] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Health, United States 1998, with Socioeconomic Status and Health Chartbook. Hyattsville, MD: Centers for Disease Control; 1998. [Google Scholar]
- 5.Andersen R. Revisiting the behavioral model and access to medical care:does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 6.Andersen R, Aday LA. Access to medical care in the U.S.:realized and potential. Med Care. 1978;16:533–46. doi: 10.1097/00005650-197807000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Shi L, Stevens GD, editors. Vulnerable Populations in the United States. San Francisco, CA: Jossey-Boss; 2005. [Google Scholar]
- 8.Aday L. At Risk in America: The Health and Health Care Needs of Vulnerable Populations in the United States. 2nd ed. San Francisco, CA: Jossey-Bass; 2001. [Google Scholar]
- 9.Fiscella K, Franks P, Doescher M, Saver B. Disparities in health care by race, ethnicity, and language among the insured. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Hargraves JL, Cunningham PJ, Hughes RG. Racial and ethnic differences in access to medical care in managed care plans. Health Serv Res. 2001;36:853–68. [PMC free article] [PubMed] [Google Scholar]
- 11.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57(suppl 1):108–45. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 12.Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev. 2000;57(suppl 1):36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- 13.Shi L. Experience of primary care by racial and ethnic groups in the United States. Med Care. 1999;37:1068–77. doi: 10.1097/00005650-199910000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Franks P, Fiscella K. Effect of patient socioeconomic status on physician profiles for prevention, disease management, and diagnostic testing costs. Med Care. 2002;40:717–24. doi: 10.1097/00005650-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Alegria M, Canino G, Rios R, et al. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr Serv. 2002;53:1547–55. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- 16.Fiscella K, Goodwin MA, Stange KC. Does patient educational level affect office visits to family physicians? J Natl Med Assoc. 2002;94:157–65. [PMC free article] [PubMed] [Google Scholar]
- 17.Solberg LI, Brekke ML, Kottke TE. Are physicians less likely to recommend preventive services to low-SES patients? Prev Med. 1997;26:350–7. doi: 10.1006/pmed.1997.0150. [DOI] [PubMed] [Google Scholar]
- 18.Schur CL, Albers LA. Language, sociodemographics, and health care use of Hispanic adults. J Health Care Poor Underserved. 1996;7:140–58. doi: 10.1353/hpu.2010.0024. [DOI] [PubMed] [Google Scholar]
- 19.Schur CL, Albers LA, Berk ML. Health care use by Hispanic adults: financial vs. non-financial determinants. Health Care Financ Rev. 1995;17:71–88. [PMC free article] [PubMed] [Google Scholar]
- 20.Aday L, Fleming G, Andersen R. Access to Medical Care in the US: Who Has It, Who Doesn't? Chicago, IL: Pluribus Press; 1984. [Google Scholar]
- 21.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults:insurance status and usual source of care. Am J Public Health. 2003;93:786–91. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corbie-Smith G, Flagg EW, Doyle JP, O'Brien MA. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002;17:458–64. doi: 10.1046/j.1525-1497.2002.10733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu KT. Usual source of care in preventive service use:a regular doctor versus a regular site. Health Serv Res. 2002;37:1509–29. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker DW, Shapiro MF, Schur CL. Health insurance and access to care for symptomatic conditions. Arch Intern Med. 2000;160:1269–74. doi: 10.1001/archinte.160.9.1269. [DOI] [PubMed] [Google Scholar]
- 25.Ayanian J, Weissman J, Schneider E, Ginsburg J, Zaslavsky A. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 26.Reschovsky J, Kemper P, Tu H. Does type of health insurance affect health care use and assessments of care among the privately insured? Health Serv Res. 2000;35(pt 2):219–37. [PMC free article] [PubMed] [Google Scholar]
- 27.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]
- 28.Sox CM, Swartz K, Burstin HR, Brennan TA. Insurance or a regular physician:which is the most powerful predictor of health care? Am J Public Health. 1998;88:364–70. doi: 10.2105/ajph.88.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lambrew JM, DeFriese GH, Carey TS, Ricketts TC, Biddle AK. The effects of having a regular doctor on access to primary care. Med Care. 1996;34:138–51. doi: 10.1097/00005650-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 30.National Center for Health Statistics. 2000. National Health Interview Survey (NHIS) Survey Description. Hyattsville, MD: Division of Health Interview Statistics; March 2002. [Google Scholar]
- 31.Forrest C, Simpson L, Clancy C. Child health services research. Challenges and opportunities. JAMA. 1997;277:1787–93. [PubMed] [Google Scholar]
- 32.Indicators and predictors of health services utilization. In: Aday L, editor; Williams S, Torrens P, editors. Introduction to Health Services. 4th ed. Albany, NY: Delmar; 1993. [Google Scholar]
- 33.Andersen R, Aday LA, Lyttle C, Cornelius L. Ambulatory Care and Insurance Coverage in an Era of Constraint. Chicago, IL: Pluribus Press; 1987. [Google Scholar]
- 34.Fleming G, Andersen R. The Municipal Health Services Program: Improving Access While Controlling Costs. Chicago, IL: Pluribus Press; 1986. [PubMed] [Google Scholar]
- 35.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res. 1983;18:49–74. [PMC free article] [PubMed] [Google Scholar]
- 36.Lurie N, Zhan C, Sangl J, Bierman AS, Sekscenski ES. Variation in racial and ethnic differences in consumer assessments of health care. Am J Manag Care. 2003;9:502–9. [PubMed] [Google Scholar]
- 37.Weathers A, Minkovitz C, O'Campo P, Diener-West M. Access to care for children of migratory agricultural workers:factors associated with unmet need for medical care. Pediatrics. 2004;113:e276–e282. doi: 10.1542/peds.113.4.e276. [DOI] [PubMed] [Google Scholar]
- 38.Byrd TL, Peterson SK, Chavez R, Heckert A. Cervical cancer screening beliefs among young Hispanic women. Prev Med. 2004;38:192–7. doi: 10.1016/j.ypmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 39.van Ryn M, Fu S. Paved with good intentions:do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93:248–55. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000;50:813–28. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 41.Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financ Rev. 2000;21:75–90. [PMC free article] [PubMed] [Google Scholar]
- 42.Doescher M, Saver B, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–63. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- 43.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(suppl 1):146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 44.Saha S, Taggart S, Komaromy M, Bindman A. Do patients choose physicians of their own race? Health Aff. 2000;19:76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- 45.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann NY Acad Sci. 1999;896:173–88. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 46.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 47.Starfield B, Powe N, Weiner J, et al. Costs vs quality in different types of primary care settings. JAMA. 1994;272:1903–8. [PubMed] [Google Scholar]
- 48.Schneider EC, Cleary PD, Zaslavsky AM, Epstein AM. Racial disparity in influenza vaccination:does managed care narrow the gap between African Americans and whites? JAMA. 2001;286:1455–60. doi: 10.1001/jama.286.12.1455. [DOI] [PubMed] [Google Scholar]
- 49.Miller R, Luft H. Managed care plan performance since 1980:a literature analysis. JAMA. 1994;271:1512–9. [PubMed] [Google Scholar]
- 50.Miller R, Luft H. Does managed care lead to better or worse quality of care? Health Aff. 1997;16:7–25. doi: 10.1377/hlthaff.16.5.7. [DOI] [PubMed] [Google Scholar]
- 51.Safran DG, Tarlov AR, Rogers WH. Primary care performance in fee-for-service and prepaid health care systems. JAMA. 1994;271:1570–86. [PubMed] [Google Scholar]
- 52.Safran D, Rogers W, Tarlov A, et al. Organizational and financial characteristics of health plans: are they related to primary care performance? Arch Intern Med. 2000;160:69–76. doi: 10.1001/archinte.160.1.69. [DOI] [PubMed] [Google Scholar]
- 53.Kaplan J, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289:2709–16. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- 54.Williams DR. Race/ethnicity and socioeconomic status:measurement and methodological issues. Int J Health Serv. 1996;26:483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14. [DOI] [PubMed] [Google Scholar]
- 55.Schulman K, Rubenstein L, Chesley F, Eisenberg J. The roles of race and socioeconomic factors in health services research. Health Serv Res. 1995;30(pt 2):179–95. [PMC free article] [PubMed] [Google Scholar]
- 56.LaVeist T. Beyond dummy variables and sample selection:what health services researchers ought to know about race as a variable. Health Serv Res. 1994;29:1–16. [PMC free article] [PubMed] [Google Scholar]