Abstract
OBJECTIVE
To quantify the magnitude of general medical and/or pharmacy claims expenditures for individuals who use behavioral health services and to assess future claims when behavioral service use persists.
DESIGN
Retrospective cost trends and 24-month cohort analyses.
SETTING
A Midwest health plan.
PARTICIPANTS
Over 250,000 health plan enrollees during 2000 and 2001.
MEASUREMENTS
Claims expenditures for behavioral health services, general medical services, and prescription medications.
MAIN RESULTS
Just over one tenth of enrollees (10.7%) in 2001 had at least 1 behavioral health claim and accounted for 21.4% of total general medical, behavioral health, and pharmacy claims expenditures. Costs for enrollees who used behavioral health services were double that for enrollees who did not use such services. Almost 80% of health care costs were for general medical services and medications, two thirds of which were not psychotropics. Total claims expenditures in enrollees with claims for both substance use and mental disorders in 2000 were 4 times that of those with general medical and/or pharmacy claims only. These expenditures returned to within 15% of nonbehavioral health service user levels in 2001 when clinical need for behavioral health services was no longer required but increased by another 37% between 2000 and 2001 when both chemical dependence and mental health service needs persisted.
CONCLUSIONS
The majority of total claims expenditures in patients who utilize behavioral health services are for medical, not behavioral, health benefits. Continued service use is associated with persistently elevated total general medical and pharmacy care costs. These findings call for studies that better delineate: 1) the interaction of general medical, pharmacy, and behavioral health service use and 2) clinical and/or administrative approaches that reverse the high use of general medical resources in behavioral health patients.
Keywords: integrated care, cost outcomes, managed care expenditures, managed behavioral health, mental health
The evaluation and treatment of mental disorders causing emotional or behavioral difficulties and/or chemical dependence, collectively known as behavioral health disorders, have been effectively separated from the evaluation and treatment of general medical disorders. Most of those with health care coverage for behavioral health needs are served by managed behavioral health organizations.1,2 These management companies operate autonomously either from the managed medical care organization administering general medical benefits to the same patients (a behavioral health carve-out) or from the parent managed care organization which owns the behavioral health business (a behavioral health carve-in) but still manages behavioral health work processes (networks, care management, claims, etc.) separately. In practice, there is little difference between the two in the way that they service behavioral health needs. As a result of the widespread administrative separation of these two areas of health care, few studies have focused on the interaction of general medical, pharmacy, and behavioral health service use in those receiving behavioral health treatment.
This article expands on our current understanding of the magnitude, persistence, and interaction of behavioral health, general medical, and pharmacy spending by comparing total claims expenditures for those with and without behavioral health service use in over 250,000 enrollees of several managed health plan accounts. Few studies have evaluated general medical and behavioral health expenditure analyses in a similar way and none in as large and diverse a population. Based on reports of increased general medical service use and cost for those with behavioral health disorders3–11 and those with acute or chronic medical conditions with behavioral health comorbidity,12–14 the authors hypothesized that patients with behavioral health service use would have higher medical and pharmacy claims expenditures than those without. The reason for the predicted increased medical costs in these patients remains unclear. While this study does not specifically address this issue, they could be associated with the predisposition of those with psychiatric difficulties to present and be treated for unexplained somatic symptoms; the treatment of emotionally distraught patients with complex medical illness; or, more likely, both. Why the percentage of total health care costs used for nonbehavioral health services was so high and persistent behavioral health service use predicted increased future claims expenditures, however, is less certain.
METHODS
This study is a retrospective population comparison of enrollees from 4 groups managed by Blue Cross Blue Shield of Minnesota, a not-for-profit health plan. Results are presented for 2000 and 2001, a period when the behavioral health needs of members were handled through a carved-in behavioral health subsidiary owned by Blue Cross but operated independently from general medical health management with its own administrative staff and a separate budget. Benefit descriptions, contract terminology, and management practices were very similar to an independent (carved-out) managed behavioral health organization.
Submitted claims with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes from 291.00 to 316.99 were classified as behavioral health.15 All other claims diagnoses were classified as general medical.
Claims are divided into institutional claims, submitted by hospitals, and professional claims, submitted by clinical practitioners. Institutional claims are coded based only on the principle diagnosis for the claim; for example, hospitalization for ischemic heart disease, even though depression may have also been present and treated during the hospitalization, would not be considered a behavioral health service. Professional claims, on the other hand, are coded for all diagnoses for which a service is provided. For instance, during a hospitalization or clinic visit for ischemic heart disease in which a diagnosis of depression was also documented and a service was given, such as a referral, medication started, and so on, the professional claim database would code for both ischemic heart disease and depression. The portion of the claim for depression would be considered a behavioral health service regardless of whether the primary physician or a consultant provided the service. The portion of the claim related to ischemic heart disease would be considered nonbehavioral. It should be noted that a treatment without a documented diagnosis, such as a prescription for an antidepressant, does not generate claims coding for a “likely” diagnosis, such as depression.
Study Population
Claims were extracted for 4 populations with managed medical and behavioral health contracts during 2000 and 2001. Two commercial and 2 public program (Medicaid) populations were analyzed. To avoid the complications associated with claims assessments in members also covered by Medicare, those 65 years and older were excluded from analysis. Because continuous enrollment was not required, claims expenditures for “enrollees” covered during only a portion of the year were calculated for the months covered and adjusted to an annual total as if they had been enrolled for the entire year.
The populations were grouped based on service use and diagnosis: Groups 1, those with behavioral health services defined by at least 1 behavioral health claim whether or not general medical and/or pharmacy claims expenditures were present; Group 2, those with no behavioral health services but with general medical and/or pharmacy claims expenditures; and Group 3, those with no behavioral health, general medical, or pharmacy claims. Those with behavioral health services were further subdivided into those with mental health claims expenditures only, such as for depression, eating disorders, and so on (ICD-9-CM codes 293–302; 306–316; Group 1a), those with chemical dependence claims expenditures only, such as for alcoholism, narcotic abuse, and so on (ICD-9-CM codes 291–292; 303–305; Group 1b), and those with both mental health and chemical dependence claims expenditures (Group 1c).15
Claims expenditures reflect all services used for both general medical and behavioral health, including prescription drugs and ancillary services. They exclude denied services and services for which no claim was submitted, such as volunteer medical clinic and medication samples. Out-of-pocket costs for the member (copays and deductibles) are included. A common claims processing system was used for the members of all groups represented in this study.
Pharmacy Services
Though the terms pharmacy, pharmacy costs, pharmacy claims, and pharmacy services are used in this study based on sentence context, they all refer to the same distinct group of claims from general medical or behavioral health claims, regardless of the medication class prescribed. Because medication prescriptions do not link ICD-9-CM diagnostic codes to the medication prescribed, we identified GC3 drug classes used in association with behavioral health disturbances, such as antidepressants, antianxiety agents, antipsychotics, and so on (drug codes: C0D, H2F, H2G, H2I, H2 M, H2S, H2U, H2W, H2Z, H3 T, H7B, H7C, H7D, H7E, H7J, H7O, H7P, H7R, H7S, H7 T, and H7U). For each of these, we assigned 100% of those pharmacy claims to behavioral health expenditures. This approach leads to overinclusion of medications as “behavioral health” because they can also be used for nonbehavioral health purposes; however, it also provides an estimate of behavioral health and nonbehavioral health prescribing patterns for those with and without behavioral health service use. Some medications, for which a small percentage of prescriptions would be for behavioral health, such as anticonvulsants (sodium valproate and carbamazepine), were not included among the behavioral health medications.
Health Care Costs
Costs are based on adjudicated claims expenditures for services rendered to members during the study period. All claims expenditures are adjusted for inflation to 2001 levels using the Consumer Price Index.16 To protect the proprietary interests of Blue Cross Blue Shield of Minnesota, actual spending on the groups has been transformed into reported per capita spending17 and adjusted for inflation to 2001 levels to reflect the average per capita costs for health care in the United States in 2001 ($4,762/person). This was done by dividing $4,762 by the 2001 mean health care spending/enrollee of the total population to determine a ratio which was then used to calculate adjusted spending amounts for each subpopulation examined. Transformed cost figures are derived from the absolute dollar amounts allowed by the health plan for member services based on negotiated contract rates, not on providers' customary charges.
Analyses
In the analyses presented, claims from the 2 commercial contracts and the 2 public programs were aggregated. χ2tests and odds ratios were used to compare differences on categorical variables, while t tests and analysis of variance with Tukey posthoc testing (P <.05) were used to compare differences between groups on continuous variables.18 Fourteen percent of the population submitted no health care claims during the study period (12% in commercial contracts and 16% in public programs). Because no cost was associated with their coverage during the study period, they were excluded from analysis of claims expenditures.
The majority of, but not all members included in the study were enrolled in both 2000 and 2001. The analysis is cross-sectional for each year and, therefore, continuous enrollment was not required. A 24-month cohort analysis was performed for a subset of discrete individuals who had both chemical dependence and mental health service usage in 2000 and were also covered in 2001.
RESULTS
Population Characteristics
The characteristics of enrollees for 2001 are described in Table 1. The commercial and public program plans differed significantly in the proportion of enrollees using behavioral health services (10.3% vs 11.1%, respectively) or having no service use (12.1% vs 16.2%, respectively) (P <.001). Enrollees in public programs were younger than those in commercial plans (21.3 [95% confidence interval (CI), 21.2 to 21.4] years vs 32.1 [95% CI, 32.0 to 32.2] years; P <.0001). Those with behavioral health service use who were less than 18 years of age were more likely to be male (odds ratio [OR], 2.0) while those over 18 were more likely to be female (OR, 1.4; P <.001).
Table 1.
Characteristics of Commercial Plans, Public Programs, and Total Population in 2001
| Total | BH Service Use | No BH Service Use | No Service Use | |||||
|---|---|---|---|---|---|---|---|---|
| N (%) | % Male | N (%) | % Male | N (%) | % Male | N (%) | % Male | |
| Commercial | 117,945 (46.2) | 48.6 | 12,118 (10.3) | 41.5 | 91,580 (77.6) | 47.1 | 14,247 (12.1) | 64.0 |
| MH use only | 11,014 (90.9) | |||||||
| CD use only | 677 (5.5) | |||||||
| MH & CD use | 427 (3.5) | |||||||
| Mean age, y | 32.1 | 33.7 | 32.2 | 29.5 | ||||
| <18 | 33,768 (28.6) | 51.8 | 2,993 (24.7) | 57.4 | 27,307 (29.8) | 50.9 | 3,468 (24.3) | 54.2 |
| 18–44 | 47,359 (40.2) | 46.0 | 5,350 (44.1) | 34.3 | 34,184 (37.3) | 42.8 | 7,825 (54.9) | 68.2 |
| 45–64 | 36,818 (31.2) | 48.9 | 3,775 (31.1) | 39.2 | 30,089 (32.9) | 48.6 | 2,954 (20.7) | 64.6 |
| Public programs | 137,272 (53.8) | 44.3 | 15,217 (11.1) | 41.1 | 99,749 (72.7) | 42.2 | 22,306 (16.2) | 56.2 |
| MH use only | 13,091 (86.0) | |||||||
| CD use only | 1,290 (8.5) | |||||||
| MH & CD use | 836 (5.5) | |||||||
| Mean age, y | 21.3 | 25.9 | 20.9 | 20.1 | ||||
| <18 | 68,339 (49.8) | 50.8 | 5,578 (36.7) | 59.9 | 51,040 (51.2) | 49.2 | 11,721 (52.5) | 53.5 |
| 18–44 | 52,756 (38.4) | 36.0 | 7,655 (50.3) | 28.9 | 36,358 (36.4) | 32.1 | 8,743 (39.2) | 58.5 |
| 45–64 | 16,177 (11.8) | 43.9 | 1,984 (13.0) | 35.3 | 12,351 (12.4) | 42.6 | 1,842 (8.2) | 61.7 |
| Total | 255,217 (100) | 46.3 | 27,335 (10.7) | 41.3 | 191,329 (75.0) | 44.5 | 36,553 (14.3) | 59.2 |
| MH use only | 24,105 (88.2) | |||||||
| CD use only | 1,967 (7.2) | |||||||
| MH & CD use | 1,263 (4.6) | |||||||
| Mean age, y | 26.3 | 29.4 | 26.3 | 23.7 | ||||
| <18 | 102,107 (40.0) | 51.2 | 8,571 (31.4) | 59.0 | 78,347 (40.9) | 49.8 | 15,189 (41.6) | 53.7 |
| 18–44 | 100,115 (39.2) | 40.7 | 13,005 (47.6) | 31.1 | 70,542 (36.9) | 37.3 | 16.568 (45.3) | 63.1 |
| 45–64 | 52,995 (20.8) | 47.4 | 5,759 (21.1) | 37.8 | 42,440 (22.2) | 46.9 | 4,796 (13.1) | 63.4 |
BH, behavioral health; MH, mental health; CD, chemical dependence.
Annual Claims Expenditures
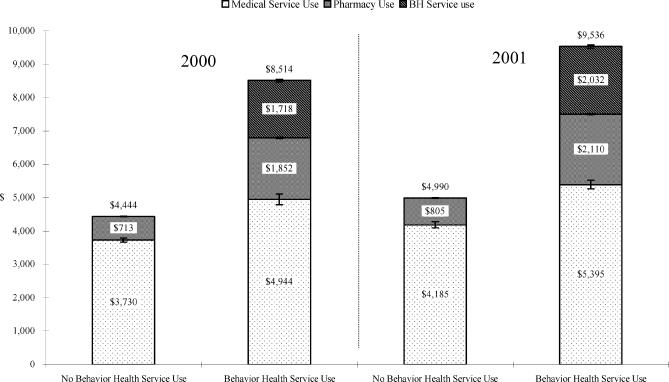
Figure 1 shows that annual costs in 2000 and 2001 for enrollees with behavioral health claims were 1.91 times higher in both years than for enrollees who used only general medical and/or pharmacy services. Claims expenditures for those with behavioral health service use in commercial plans and in public programs were 2.06 and 1.79 times the costs for those with only general medical and/or pharmacy service use, respectively.
Figure 1.
Annual mean claims expenditures for medical, pharmacy, and behavioral health services per enrollee in 2000 and 2001 for those with (Group 1) and without (Group 2) behavioral health claims expenditures in two commercial plans and two public programs. I-bars represent standard error.*There were 245,744 enrollees in 2000 and 255,217 enrollees in 2001 in these plans; 74.9% and 75.0%, respectively, used medical or pharmacy services only; 9.4% and 10.7%, respectively, used at least 1 behavioral health service, and 15.8% and 14.3%, respectively, did not use any medical, pharmacy, or behavioral health services. Those with no service use (Group 3) were excluded from this comparison. Total, general medical, and pharmacy claims expenditures between those who used medical and pharmacy services only (Group 2) and those who used at least 1 behavioral health service (Group 1) were all significantly different (P <.0001) in both 2000 and 2001.
Almost 80% (79.9% in 2000 and 78.7% in 2001) of the total health care costs associated with enrollees who had behavioral health claims expenditures was for pharmacy and/or general medical services. Two thirds of the additional cost in those who used behavioral health services compared to those who used only general medical and pharmacy services was for general medical and pharmacy claims.
When adjusted for age and gender, total (P <.0001), general medical (P <.0001), and pharmacy (P <.0001) claims expenditures for those with behavioral health service use remained significantly higher than those without.
Costs by Type of Behavioral Health Service
During the period of study, 4.0% of total claims expenditures were used for behavioral health benefits. Though only 9.4% and 10.7% of enrollees used behavioral health services in 2000 and 2001, respectively, they accounted for 19.4% and 21.4% of total claims expenditures when behavioral health, general medical, and pharmacy costs were included.
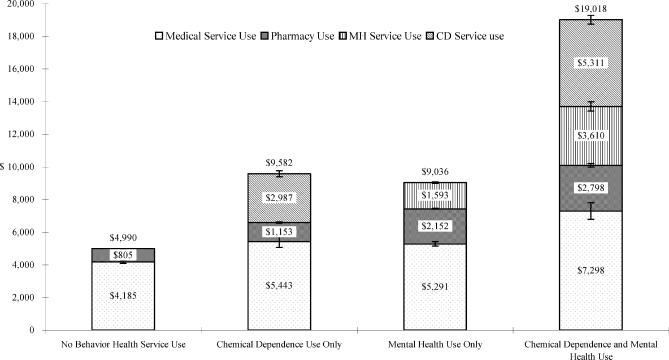
As shown in Figure 2, individuals who used both mental health and chemical dependence services (Group 1c—2001) had 3.8 times the total claims expenditure as those who used only general medical and pharmacy services (Group 2—2001) ($19,018 vs $4,990). Enrollees with mental health service use only (Group 1a—2001; N =24,105) had annual general medical claims expenditures that were 26% ($1,106/enrollee; $26.7 million cumulative) and pharmacy claims expenditures that were 167% ($1,347/enrollee; $32.5 million cumulative) higher than those with no behavioral health claims in 2001 (Group 2—2001).
Figure 2.
Annual mean claims expenditures in 2001 for medical, pharmacy, mental health, and chemical dependence services per enrollee for those with no behavioral health service use (Group 2—2001), those with at least 1 chemical dependence service use (Group 1b—2001), those with at least 1 mental health service use (Group 1a—2001), and those with both chemical dependence and mental health service use (Group 1c—2001). I-bars represent standard error.*Among the members in the groups, 75.0% used medical or pharmacy services only; 0.8% used at least 1 chemical dependence service only; 9.4% used at least 1 mental health service only; and 0.5% used both mental health and chemical dependence services. The 14.3% who did not use any services were excluded from comparison. Total claims expenditures for each group were significantly different from the others (P <.0001) with the exception of those with chemical dependence use only versus those with mental health use only. Medical claims expenditures were significantly lower for those with no behavioral health service use (Group 2—2001) compared to those with mental health service use only (Group 1a—2001) and those with both (Group 1c—2001) (P <.0001). Pharmacy claims expenditures were different among all groups (P <.0001).
Seven hundred sixty-eight of the 934 discrete individuals (82.2%) who had both mental health and chemical dependence service use in 2000 (Group 1c—24-month cohort 2000) continued enrollment with Blue Cross in 2001. When these individuals were assessed for claims expenditures in 2001 (Groups 1a, 1b, 1c, and 2—24-month cohort 2001), broken down by which types of services they used (Table 2), as a group, they had 3.18 times higher total health care spending in 2001 compared to those with general medical and pharmacy claims only (Group 2—2001). However, total claims expenditures for enrollees in the group who used no behavioral health services (Group 2—24-month cohort 2001) fell to within 15% of the 191,329 enrollees who used only general medical and/or pharmacy services in 2001 (Group 2—2001). Conversely, those with continued chemical dependence and mental health service needs (Group 1c—24-month cohort 2001) showed a 37% increase in total claims costs compared to 2000 (Group 1c—24-month cohort 2000) and 456% higher expenditures than those using only general medical and pharmacy services (Group 2—2001).
Table 2.
Mean Claims Expenditures in 2001 for Patients with Mental Health and Chemical Dependence Claims Expenditures in 2000*
| N | % | Annual Spending per Member, $ | |
|---|---|---|---|
| Total claims expenditures in 2000 | 768 | 100.0 | 16,634 |
| (Group 1c—24-month cohort 2000) | |||
| Total claims expenditures in 2001 | 768 | 100.0 | 12,506 |
| (Groups 1a, 1b, 1c, & 2—24-month cohort 2001) | |||
| Mental health use only | 281 | 36.6 | 12,736 |
| (Group 1a—24-month cohort 2001) | |||
| Chemical dependence use only | 65 | 8.4 | 10,471 |
| (Group 1b—24-month cohort 2001) | |||
| Mental health & chemical dependence use | 172 | 22.4 | 22,752 |
| (Group 1c—24-month cohort 2001) | |||
| No mental health or chemical dependence use | 250 | 32.6 | 5,729 |
| (Group 2—24-month cohort 2001) |
In 2001, 768 of the 934 members (82.2%) who used both mental health and chemical dependence services in 2000 (Group 1c—24-month cohort 2000) remained enrolled in 2001 (Groups 1a, 1b, 1c, and 2—24-month cohort 2001).
Costs by Type of Medication
Forty percent of total prescription claims expenditures (42% in 2000 and 39% in 2001) could be attributed to behavioral health treatment in those with behavioral health service use (Group 1) compared to 8% (in both 2000 and 2001) in those without behavioral health service use (Group 2). However, the claims expenditures for prescriptions of nonbehavioral medications were 71% higher in those with behavioral health service use (Group 1) compared to those without (Group 2).
DISCUSSION
This study extends our understanding of the documented higher service use and cost for those with behavioral health disorders seen in clinical settings3,5–9,12–14,19–23 in several important ways. It finds that 1) in a large and diverse population during 2 consecutive years, the 10% who used behavioral health services had total claims expenditures accounting for up to a fifth of a health plan's total claims expense; 2) 80% of the doubled health care resource utilization in these patients was for nonbehavioral health care; 3) while on a percentage basis there was a much greater increase in pharmacy expenditures for those with behavioral health service use (167%), nearly two thirds of that use was for nonpsychiatric medications; and 4) clinical improvement, such as that presumed in the 32% of individuals who used both mental health and chemical dependence services in 2000 (Group 1c—24-month cohort 2000) but none in 2001 (Group 2—24-month cohort 2001), was associated with substantial reductions in the total annual cost of care while continued behavioral health service need/use was associated with continued high service use and escalating costs (Groups 1a, 1b, and 1c—24-month cohort 2001 vs Group 2—2001).
While our findings fail to corroborate findings in one study,24 they substantiate four others in selected subpopulations of behavioral health service users4,8,25,26 that utilized claims data in employment groups and/or health plan enrollees to document higher total spending for general medical services in patients with behavioral health service use. We were unable to find other studies which document the percent contribution to total cost of care for behavioral health service users in a large managed population. Buck et al.27,28 addressed this question by assessing the contribution of behavioral health service users to total cost among high-cost Medicaid enrollees in a 1995 sample. They reported that 28% of claims expenditures, over 60% of which were for nonbehavioral health services, could be attributed to the 11% of patients who used behavioral health services. Twenty-eight percent is slightly higher than the 20% reported in our study, which includes patients falling at all points on the cost continuum.
To our knowledge, this is the first report to document consecutive annual total claims expenditures in a sample of individuals with high health care costs related to behavioral health needs in the first year, that is, both mental health and chemical dependence service use (Group 1c—24-month cohort 2000), and then to correlate second-year spending with second-year claims-based behavioral health service use (Groups 1a, 1b, 1c, and 2—24-month cohort 2001). While our data do not allow us to assign causality nor even to document behavioral health recovery during the second year, they do suggest an association between behavioral improvement as suggested by decreased behavioral health claims and the amount spent on health care in year 2.
As one might predict, in patients with both mental health and chemical dependence service use in 2000 (Group 1c—24-month cohort 2000) who used no behavioral health services in 2001 (despite continued insurance coverage; Group 2—24-month cohort 2001), total claims expenditures in this subgroup dropped and was close to the level of patients with general medical and pharmacy service use only (Group 2—2001). Among enrollees with either persistent mental health or chemical dependence service needs (Groups 1a or 1b—24-month cohort 2001), claims expenditures were more than double the nonbehavioral health service user group (Group 2—2001) but much lower than for those with continued use of both mental health and chemical dependency services where claims costs actually increased 37% above mean 2000 service use levels (Group 1c—24-month cohort 2001).
This study has several limitations. First, the groups included were all in a primary care clinic managed care model. Although they represent a broad cross-section of individuals less than age 65 covered in commercially insured and public programs, it is possible that those covered in totally open-access accounts would demonstrate different service use patterns. Second, those in the 4 groups are mainly residents of Minnesota. It is possible that state laws and regulations mandating coverage limits comparison to other states. Third, our findings identify an association, not an etiologic relationship, between behavioral health service use and increased general medical and pharmacy spending.
Finally, the study is based on diagnostic codes used for claims adjudication, which are known to be incomplete and/or inaccurate to varying degrees. For example, it is likely that patients with services provided for behavioral health reasons were not consistently coded with a behavioral health diagnosis, particularly in the nonbehavioral health setting.29 Costs associated with those services would thus be attributed to general medical care in our analyses. While this is an important issue, particularly as future studies unravel the reasons for high general medical service utilization in behavioral health service users, the accuracy of the psychiatric diagnosis in this study is less important than the impact that diagnosing and providing a clinical service for a behavioral health disorder in typical clinical practice, whether the main problem or a comorbid condition, has on predictable increases in general medical and pharmacy service use.
This is the first article we are aware of which emphasizes the magnitude, persistence, and pervasiveness of the interaction between general medical and behavioral health service use. It could be that its findings merely represent obvious outcomes in a system of care doing its best to treat behavioral health complaints found in patients with costly medical illness. The literature documents that patients with chronic medical illnesses and concurrent psychiatric symptoms demonstrate a worse physical health prognosis.12–14 Successful treatment of concurrent medical illness, therefore, may have reversed the need for psychiatric services and thus explain the substantial reduction in expenditures for patients in our 24-month cohort who no longer used mental health and chemical dependence services in 2001. This interpretation of the results suggests that patients with both mental health and chemical dependence service use should be closely assessed for comorbid medical illness. Aggressive treatment could change an otherwise dismal medical prognosis and reverse unnecessary secondary psychiatric expenses.
Alternatively, our results could be a reflection of the degree to which concurrent and unexplained physical symptoms are found in patients with psychiatric illness. Again, the literature clearly demonstrates a high frequency of unexplained complaints in patients suffering from depression,30–34 anxiety,33–35 and many other emotional and behavioral disorders.36–38 If this is used as the reason for high medical and pharmacy service use in behavioral health patients, then interpretation of the longitudinal outcome improvement would more accurately be attributed to successful intervention for or spontaneous resolution of both the patient's chemical dependence and mental health disorders with a secondary reduction in physical health symptoms requiring medical attention and high use of nonpsychiatric medication. This second scenario represents a less desirable (though more likely) explanation for our findings because it suggests that such patients are exposed to unnecessary, high-cost, and potentially dangerous medical assessments and treatments in a medical world in which iatrogenic illness and medical errors lead to increased morbidity and mortality.39–41
Yet another explanation for the results found in this retrospective cost trend analysis is that the magnitude and persistence of the interaction have nothing at all to do with the medical and psychiatric illnesses. Rather, the interaction may be the product of a medical system in which disincentives to use behavioral health care introduced by managed behavioral health business practices,42–44 difficulty in accessing behavioral health services,45 loss of behavioral health coverage,46 and/or exhausting annual or lifetime behavioral health benefits drives patients from the behavioral health sector to the medical sector for assistance as they attempt to alleviate psychiatric suffering which has not been successfully treated. Evidence for “cost shifting,” as described here, can be found in a study by Rosenheck et al.25 who demonstrated that, while the introduction of managed behavioral health practices reduced behavioral health service costs by 37.7% in 21,000 employees of a large manufacturing corporation over 3 years, there was an associated 36.6% increase in nonbehavioral health expenses with a net annual increase in total health care costs of $130/enrollee.
Unfortunately, our study raises more questions than it answers. While any of these interpretations, or perhaps more likely, a combination could be used as the reason for the findings reported in this study, our results point to a new and important area of needed investigation. We practice in a world in which there is an unspoken assumption that general medical and behavioral health difficulties are sufficiently different that they should be handled separately. Our results suggest that by doing so an important interaction between the two is missed, at great expense to both our patients and the health care system.
Acknowledgments
The authors wish to thank Rachel Starbuck for her administrative support, Nancy Garrett for suggestions regarding manuscript preparation, and Mary Boerjan for the leadership needed to reorganize and analyze claims data so that combined service use could be examined.
This manuscript is derived from routine claims analyses by the Cost Trends Committee at Blue Cross Blue Shield of Minnesota.
REFERENCES
- 1.Garnick DW, Horgan CM, Hodgkin D, et al. Risk transfer and accountability in managed care organizations' carve-out contracts. Psychiatr Serv. 2001;52:1502–9. doi: 10.1176/appi.ps.52.11.1502. [DOI] [PubMed] [Google Scholar]
- 2.Grazier KL, Eselius LL. Mental health carve-outs: effects and implications. Med Care Res Rev. 1999;56(suppl 2):37–59. [PubMed] [Google Scholar]
- 3.Escobar JI, Golding JM, Hough RL, Karno M, Burnam MA, Wells KB. Somatization in the community: relationship to disability and use of services. Am J Public Health. 1987;77:837–40. doi: 10.2105/ajph.77.7.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harlow K, Johnson R, Callen P. Comparison of physical health benefits utilization. Mental and physical health claimants, 1989 and 1990. J Occup Med. 1993;35:275–81. [PubMed] [Google Scholar]
- 5.Hansson L, Persson KB, Borgquist L. Patients with mental illness in primary health care. A long-term follow-up of health care utilization and contact patterns with psychiatric care. Scand J Prim Health Care. 1997;15:129–33. doi: 10.3109/02813439709018502. [DOI] [PubMed] [Google Scholar]
- 6.Rost K, Zhang M, Fortney J, Smith J, Smith GR., Jr Expenditures for the treatment of major depression. Am J Psychiatry. 1998;155:883–8. doi: 10.1176/ajp.155.7.883. [DOI] [PubMed] [Google Scholar]
- 7.Meerding WJ, Bonneux L, Polder JJ, Koopmanschap MA, van der Maas PJ. Demographic and epidemiological determinants of healthcare costs in Netherlands:cost of illness study. BMJ. 1998;317:111–5. doi: 10.1136/bmj.317.7151.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simon GE, Unutzer J. Health care utilization and costs among patients treated for bipolar disorder in an insured population. Psychiatr Serv. 1999;50:1303–8. doi: 10.1176/ps.50.10.1303. [DOI] [PubMed] [Google Scholar]
- 9.Druss BG, Rosenheck RA. Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiatr Serv. 1999;50:214–8. doi: 10.1176/ps.50.2.214. [DOI] [PubMed] [Google Scholar]
- 10.Katon WJ, Lin E, Russo J, Unutzer J. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 11.Hunkeler EM, Spector WD, Fireman B, Rice DP, Weisner C. Psychiatric symptoms, impaired function, and medical care costs in an HMO setting. Gen Hosp Psychiatry. 2003;25:178–84. doi: 10.1016/s0163-8343(03)00018-5. [DOI] [PubMed] [Google Scholar]
- 12.Goetzel RZ, Anderson DR, Whitmer RW, Ozminkowski RJ, Dunn RL, Wasserman J. The relationship between modifiable health risks and health care expenditures. An analysis of the multi-employer HERO health risk and cost database. The Health Enhancement Research Organization (HERO) Research Committee. J Occup Environ Med. 1998;40:843–54. doi: 10.1097/00043764-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Druss BG, Rohrbaugh RM, Rosenheck RA. Depressive symptoms and health costs in older medical patients. Am J Psychiatry. 1999;156:477–9. doi: 10.1176/ajp.156.3.477. [DOI] [PubMed] [Google Scholar]
- 14.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 15.International Classification of Diseases. Ninth Revision, Clinical Modification. Washington, DC: Public Health Service, U.S. Department of Health and Human Services; 1988. [Google Scholar]
- 16.U.S. Department of Labor: Bureau of Labor Statistics. Consumer Price Index. Available at: http://www.bls.gov/bls/inflation.htm. Accessed December 20, 2002.
- 17.Canaud M-C, Huber M, Lafortune G, Cerf KL, Morgan D, Thompson A. 4th ed. Paris: Organisation for Economic Cooperation and Development; 2002. OECD Health Data 2002: A Comparative Analysis of 30 Countries. [Google Scholar]
- 18.Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Ann Rev Public Health. 2002;23:151–69. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 19.Hansen MS, Fink P, Frydenberg M, Oxhoj ML. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64:668–75. doi: 10.1097/01.psy.0000024104.87632.94. [DOI] [PubMed] [Google Scholar]
- 20.Fischer LR, Wei F, Rolnick SJ, et al. Geriatric depression, antidepressant treatment, and healthcare utilization in a health maintenance organization. J Am Geriatr Soc. 2002;50:307–12. doi: 10.1046/j.1532-5415.2002.50063.x. [DOI] [PubMed] [Google Scholar]
- 21.Koenig HG, Kuchibhatla M. Use of health services by hospitalized medically ill depressed elderly patients. Am J Psychiatry. 1998;155:871–7. doi: 10.1176/ajp.155.7.871. [DOI] [PubMed] [Google Scholar]
- 22.Druss BG, Rosenheck RA, Sledge WH. Health and disability costs of depressive illness in a major U.S. corporation. Am J Psychiatry. 2000;157:1274–8. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- 23.Savoca E. Psychiatric co-morbidity and hospital utilization in the general medical sector. Psychol Med. 1999;29:457–64. doi: 10.1017/s0033291798008071. [DOI] [PubMed] [Google Scholar]
- 24.Cuffel BJ, Goldman W, Schlesinger H. Does managing behavioral health care services increase the cost of providing medical care? J Behav Health Serv Res. 1999;26:372–80. doi: 10.1007/BF02287298. [DOI] [PubMed] [Google Scholar]
- 25.Rosenheck RA, Druss B, Stolar M, Leslie D, Sledge W. Effect of declining mental health service use on employees of a large corporation. Health Aff (Millwood) 1999;18:193–203. doi: 10.1377/hlthaff.18.5.193. [DOI] [PubMed] [Google Scholar]
- 26.Trudeau JV, Deitz DK, Cook RF. Utilization and cost of behavioral health services:employee characteristics and workplace health promotion. J Behav Health Serv Res. 2002;29:61–74. doi: 10.1007/BF02287832. [DOI] [PubMed] [Google Scholar]
- 27.Buck JA, Teich JL, Bae J, Dilonardo J. Mental health and substance abuse services in ten state Medicaid programs. Adm Policy Ment Health. 2001;28:181–92. doi: 10.1023/a:1007855901228. [DOI] [PubMed] [Google Scholar]
- 28.Buck JA, Teich JL, Miller K. Use of mental health and substance abuse services among high-cost Medicaid enrollees. Adm Policy Ment Health. 2003;31:3–14. doi: 10.1023/a:1026089422101. [DOI] [PubMed] [Google Scholar]
- 29.Rost K, Smith R, Matthews DB, Guise B. The deliberate misdiagnosis of major depression in primary care. Arch Fam Med. 1994;3:333–7. doi: 10.1001/archfami.3.4.333. [DOI] [PubMed] [Google Scholar]
- 30.Waxman HM, McCreary G, Weinrit RM, Carner EA. A comparison of somatic complaints among depressed and non-depressed older persons. Gerontologist. 1985;25:501–7. doi: 10.1093/geront/25.5.501. [DOI] [PubMed] [Google Scholar]
- 31.Passamonti M, Pigni M, Fraticelli C, Calori G, Piccinelli M. Somatic symptoms and depression in general practice in Italy. Eur J Gen Pract. 2003;9:66–7. doi: 10.3109/13814780309160405. [DOI] [PubMed] [Google Scholar]
- 32.Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–35. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K. Patients presenting with somatic complaints: epidemiology, psychiatric comorbidity and management. Int J Methods Psychiatr Res. 2003;12:34–43. doi: 10.1002/mpr.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–41. doi: 10.1176/ajp.150.5.734. [DOI] [PubMed] [Google Scholar]
- 35.Katon W. Panic disorder: relationship to high medical utilization, unexplained physical symptoms, and medical costs. J Clin Psychiatry. 1996;57(suppl 10):11–8. discussion 19–22. [PubMed] [Google Scholar]
- 36.Khan AA, Khan A, Harezlak J, Tu W, Kroenke K. Somatic symptoms in primary care: etiology and outcome. Psychosomatics. 2003;44:471–8. doi: 10.1176/appi.psy.44.6.471. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153:2474–80. [PubMed] [Google Scholar]
- 38.Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology:relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med. 2001;134(pt 2):917–25. doi: 10.7326/0003-4819-134-9_part_2-200105011-00017. [DOI] [PubMed] [Google Scholar]
- 39.Morris JA, Jr, Carrillo Y, Jenkins JM, et al. Surgical adverse events, risk management, and malpractice outcome:morbidity and mortality review is not enough. Ann Surg. 2003;237:844–51. doi: 10.1097/01.SLA.0000072267.19263.26. discussion 851–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38:261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Brennan TA. The Institute of Medicine report on medical errors—could it do harm? N Engl J Med. 2000;342:1123–5. doi: 10.1056/NEJM200004133421510. [DOI] [PubMed] [Google Scholar]
- 42.Merrick EL, Garnick DW, Horgan CM, Goldin D, Hodgkin D, Sciegaj M. Benefits in behavioral health carve-out plans of Fortune 500 firms. Psychiatr Serv. 2001;52:943–8. doi: 10.1176/appi.ps.52.7.943. [DOI] [PubMed] [Google Scholar]
- 43.Goldman W, McCulloch J, Sturm R. Costs and use of mental health services before and after managed care. Health Aff (Millwood) 1998;17:40–52. doi: 10.1377/hlthaff.17.2.40. [DOI] [PubMed] [Google Scholar]
- 44.Scheffler RM. Managed behavioral health care and supply-side economics. 1998 Carl Taube Lecture. J Ment Health Policy Econ. 1999;2:21–8. doi: 10.1002/(sici)1099-176x(199903)2:1<21::aid-mhp33>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 45.Matevia ML, Poon D, Goldman W, Cuffel B, McCulloch J. Access to network clinicians in a managed behavioral health organization. Psychiatr Serv. 2001;52:1428. doi: 10.1176/appi.ps.52.11.1428. [DOI] [PubMed] [Google Scholar]
- 46. U.S. General Accounting Office. Private Health Insurance. Access to Individual Market Coverage May Be Restricted for Applicants with Mental Disorders. Report No. GAO-02–339. Washington, DC: U.S. General Accounting Office; 2002.