Abstract
BACKGROUND/OBJECTIVE
In-home automated external defibrillators (AEDs) are increasingly recommended as a means for improving survival of cardiac arrests that occur at home. The current study was conducted to explore the relationship between individuals' risk of cardiac arrest and cost-effectiveness of in-home AED deployment.
DESIGN
Markov decision model employing a societal perspective.
PATIENTS
Four hypothetical cohorts of American adults 60 years of age at progressively greater risk for sudden cardiac death (SCD): 1) all adults (annual probability of SCD 0.4%); 2) adults with multiple SCD risk factors (probability 2%); 3) adults with previous myocardial infarction (probability 4%); and 4) adults with ischemic cardiomyopathy unable to receive an implantable defibrillator (probability 6%).
INTERVENTION
Strategy 1: individuals suffering an in-home cardiac arrest were treated with emergency medical services equipped with AEDs (EMS-D). Strategy 2: individuals suffering an in-home cardiac arrest received initial treatment with an in-home AED, followed by EMS.
RESULTS
Assuming cardiac arrest survival rates of 15% with EMS-D and 30% with AEDs, the cost per quality-adjusted life-year gained (QALY) of providing in-home AEDs to all adults 60 years of age is $216,000. Costs of providing in-home AEDs to adults with multiple risk factors (2% probability of SCD), previous myocardial infarction (4% probability), and ischemic cardiomyopathy (6% probability) are $132,000, $104,000, and $88,000, respectively.
CONCLUSIONS
The cost-effectiveness of in-home AEDs is intimately linked to individuals' risk of SCD. However, providing in-home AEDs to all adults over age 60 appears relatively expensive.
Keywords: emergency medical services, heart arrest, defibrillators
Approximately 250,000 Americans suffer out-of-hospital cardiac arrests each year.1,2 Available evidence supports the use of implantable cardioverter defibrillators (ICDs) in individuals at highest risk for cardiac arrest (e.g., those with an ejection fraction of ≤30%) because their risk of cardiac arrest is 5% to 10% per year.3–6 However, approximately 70% of out-of-hospital cardiac arrests occur among individuals at increased risk for sudden cardiac death (SCD) but who lack sufficient risk to warrant a prophylactic ICD.1,7–10
In the absence of an ICD, survival of out-of-hospital cardiac arrest depends upon a rapid response by emergency medical services (EMS) to deliver defibrillation. While cardiac arrest survival rates of 25% have been reported, prolonged EMS response times and survival rates of 3% to 5% are common.11–14 In an effort to reduce the time-to-defibrillation interval and improve cardiac arrest survival, the public health system has increasingly turned to a strategy of public access defibrillation (PAD) to augment EMS.15 The strategy of PAD is predicated upon the idea that automated external defibrillators (AEDs) should be placed in densely populated public locations where cardiac arrests are likely to occur.16 A recently published study demonstrated that PAD can increase cardiac arrest survival,17 but PAD is hampered by at least 2 important constraints18,19. First, there are an infinite number of public locations where cardiac arrests may occur and AEDs can be deployed; second, PAD is ineffective for the 50% to 70% of out-of-hospital cardiac arrests that occur in private homes.7,15,20–22 One potential solution to the problem of in-home cardiac arrests is to provide individuals at increased risk of SCD with personal AEDs for in-home use. While the idea of home defibrillators has been contemplated for many years, only recently have improvements in technology made in-home AEDs a viable option.15,23,24 The Federal Drug Administration (FDA) responded to these improvements by approving AEDs for in-home use with a prescription in 2002 and is currently considering over-the-counter availability.25,26
However, the relationship between an individual's risk of SCD and the cost-effectiveness of in-home AED deployment relative to EMS is unknown. Accordingly, we developed a decision analytic model to evaluate the clinical and economic consequences of in-home AED deployment for individuals at increased risk of SCD in an effort to clarify the relationship between an individual's risk of SCD and the cost-effectiveness of an in-home AED.
METHODS
Literature Review
MEDLINE was used to search the 1966–2003 medical literature using the terms heart arrest, emergency medical services, and public access defibrillation, as were abstracts of major scientific meetings from 2000 to 2003. Bibliographies of selected review articles were scanned to identify additional articles.
Relevant articles were abstracted by one of the authors (P.C.) to obtain the values for the model. In cases where multiple publications estimating a particular input were available, we assessed the methodology of each study and used the estimate from the study deemed to be the most methodologically sound. If no single study was superior, we took the mean of the estimates provided by the available studies and used broad confidence intervals to incorporate the range of available estimates into sensitivity analysis.
Decision Analytic Model
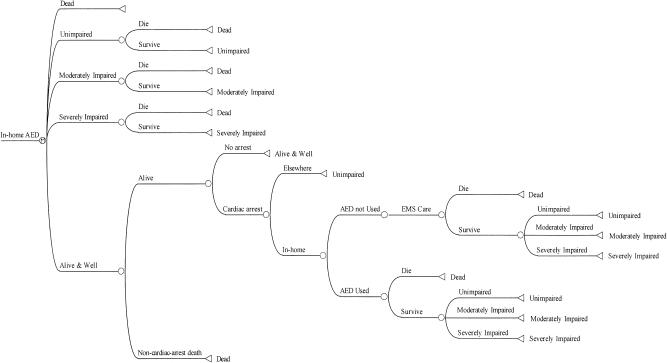
We constructed a Markov decision model using the societal perspective to evaluate the lifetime clinical and economic impact of 2 alternative strategies in a cohort of adults 60 years of age (Fig. 1): strategy 1: individuals suffering an in-home cardiac arrest initially received cardiopulmonary resuscitation (CPR) followed by care administered by EMS equipped with AEDs (EMS-D); strategy 2: individuals suffering an in-home cardiac arrest were initially treated with a home AED followed by care administered by EMS-D (AED). The two strategies differed only in the initial availability of an AED and its impact on cardiac arrest survival and costs. All probabilities for model inputs are shown in Table 1. DATA 4.0 (TreeAge Software Inc., Williamstown, MA) and Excel 2000 (Microsoft Inc., Redmond, WA) were used for all analyses.
FIGURE 1.
Decision analytic model for strategy 2
Table 1.
Model Inputs
| Variable | Base-case | Range | Reference |
|---|---|---|---|
| Probabilities | |||
| Probability arrest will occur at home | .50 | .40–.70 | (15, 20–22) |
| Probability AED will be used on in-home arrest victim | .40 | .25–.75 | (20) |
| Probability of initial resuscitation with emergency medical services (EMS) | .30 | .15–.60 | (11–13) |
| Probability of initial resuscitation with AED | .50 | .40–.80 | (18, 19, 75, 76) |
| Probability of surviving to hospital discharge with EMS | .15 | .03–.30 | (11–14, 55, 56) |
| Probability of surviving to hospital discharge with AED | .30 | .20–.50 | (18, 19, 75, 76) |
| Annual probability of dying—cardiac arrest survivors | .15 | .10–.30 | (3, 60–62) |
| Probability of surviving cardiac arrest unimpaired | .75 | .50–.85 | (60, 63, 64) |
| Probability of surviving arrest moderately impaired | .15 | .05–.30 | (60, 63, 64) |
| Probability of surviving arrest severely impaired | .10 | .00–.20 | (60, 63, 64) |
| Costs, $ | |||
| Annual medical costs | |||
| Unselected population | 4,000 | 3,000–8,000 | (40, 41) |
| Multiple risk factors | 5,000 | 4,000–12,000 | (42) |
| Previous myocardial infarction | 5,500 | 4,500–14,000 | (43) |
| Congestive heart failure | 10,000 | 8,000–20,000 | (44) |
| AED purchase | 2,000 | 250–2,500 | (45) |
| AED maintenance | 40 | 20–80 | (45) |
| Annual cost of AED training | 50 | 25–100 | Personal written communication, Johnson County Red Cross |
| Time for training at $17/hour for 4 hours | 70 | 35–140 | (47) |
| AED supplies per use | 150 | 100–200 | (45) |
| Postarrest hospitalization | |||
| Survive to discharge | 54,000 | 40,000–100,000 | (48–50) |
| Death in hospital | 15,000 | 3,000–30,000 | (46, 50, 51) |
| Annual medical costs for arrest survivors | 13,000 | 9,000–20,000 | (46, 48, 49) |
| Other parameters | |||
| Quality of life | |||
| Unimpaired | .85 | .7–1 | (65, 67) |
| Moderately impaired | .20 | 0–.40 | (68) |
| Severely impaired | .1 | 0–.2 | (68) |
EMS, emergency medical services; AED, automated external defibrillator.
Patient Population, Probability of Cardiac Arrest, and AED Use
While the risk of SCD among an unselected population of American adults is 0.4% per year, the probability of cardiac arrest among adults with multiple SCD risk factors ranges from 2% to 6% per year depending upon the precise population.1,3,5,8,9,27–37 We evaluated the cost-effectiveness of in-home AEDs among 4 cohorts of adults at progressively increasing risk of SCD: 1) all adults (initial probability of SCD at age 60 of 0.4%); 2) adults with multiple SCD risk factors such as hypertension or left ventricular hypertrophy (initial probability 2%); 3) adults with previous myocardial infarction (initial probability 4%); and 4) adults with ischemic cardiomyopathy and an ejection fraction ≤30%, but unable/unwilling to receive an ICD (initial probability 6%).
Individuals in each cohort were considered to be at risk for both SCD and death from other causes on an annual basis. The initial risk of both SCD and overall mortality in each cohort were derived from the medical literature and assumed to increase in subsequent years based upon life-table estimates.27,38
Available evidence suggests that 50% to 70% of all out-of-hospital arrests occur at home and that at least 50% are witnessed.15,20–22,39 However, even if a cardiac arrest occurs at home, is witnessed, and an AED is available, it is likely that the device will not always be used. In the base-case, it was assumed that 50% of all arrests occurred at home and that 40% of these arrests were witnessed and treated with the available in-home AED. These assumptions were evaluated in sensitivity analyses. It was assumed that an in-home AED was used exclusively for arrests that occurred in the home of the individual for whom the device was prescribed and that the only person at risk of suffering an in-home cardiac arrest was the individual for whom the AED was prescribed. It was also assumed that all individuals purchasing an in-home AED lived with at least one other person capable of using the device.
Costs
Costs included in the model are shown in Table 1. Individuals in each of the 4 cohorts accrued annual medical costs based upon values in the published literature.40–44 The cost of an in-home AED was $2,000;45 AED maintenance costs were also included in the model.45,46 We assumed that for each AED purchased, two individuals would undergo CPR and AED training on a biennial basis (the individual “at-risk” and one cohabitant). Additional costs were included to account for the time required for training.47
Previous studies have demonstrated that the cost of hospitalization for cardiac arrest victims varies, depending upon whether an individual dies in the hospital or survives to discharge.46,48–51 Hospitalization costs among cardiac arrest survivors accounted for the expectation that most would receive an ICD. Future medical costs incurred by cardiac arrest survivors were included in the model and accounted for the likelihood that a proportion of survivors would require long-term care.46,48,49 Historical costs were adjusted to 2004 dollars using an inflation rate of 2.5% to reflect inflation in the consumer price index between 1999 and 2002.52 Future costs and benefits were discounted at 3% in accordance with accepted guidelines.53
Effectiveness of Strategy 1
In the absence of an in-home AED, individuals suffering an arrest at home would be treated by EMS equipped with AEDs (EMS-D). While survival rates of 25% have been reported with optimized EMS-D, survival rates of 3% to 5% are common in congested urban and remote rural areas.11–14,54–56; this variation in survival reflects the fact that cardiac arrest survival falls by approximately 10% per-minute delay in defibrillation.57 In the base-case, 15% of in-home cardiac arrest victims were assumed to survive to hospital discharge based upon survival rates with an optimized EMS-D system and a time-to-defibrillation interval of 10 minutes.58,59 This assumption was deliberately optimistic for EMS-D and it is likely that many cardiac arrest victims experience a time-to-defibrillation interval of 15 minutes or more, thus resulting in cardiac arrest survival rates of 10% or less. Sensitivity analysis was used to assess the impact of varying time-to-defibrillation intervals and corresponding changes in arrest survival rates on overall cost-effectiveness.
Effectiveness of Strategy 2
The benefit of in-home AEDs is directly related to any increase in survival that they confer (strategy 2) relative to EMS-D-based care (strategy 1). No published studies have examined the impact of in-home AEDs on cardiac arrest survival. However, studies examining the impact of AED deployment in public locations (PAD) on cardiac arrest survival are highly applicable.17–19 Based upon these studies and an average time-to-defibrillation interval of 5 minutes, cardiac arrest survival with an in-home AED was estimated to be 30% in the base-case.57–59
Life Gained Among Arrest Survivors
Cardiac arrest survivors have an annual mortality of approximately 15% per year.3,60–62 Survivors of cardiac arrest were assigned to 1 of 3 cerebral performance categories (CPC) based upon published data: CPC-1, unimpaired with no residual deficit; CPC-2, moderately impaired with minimal deficits, but able to live independently; or CPC-3/4, severely impaired, requiring institutional care.60,63–66 Utility scores for unimpaired survivors were based upon studies by Nichol et al.67 and Granja et al.65 Utility scores for the moderately and severely impaired survivors were estimated based upon published data from stroke survivors with similar levels of functional impairment.68
Sensitivity Analysis
Because of uncertainty regarding the precise values of many of the model inputs, a series of 3 sensitivity analyses were performed. First, one-way sensitivity analyses were performed across the range of values available for each of the model inputs. Next, two-way sensitivity analyses were conducted using combinations of model variables to further assess the impact of uncertainty on our findings. Finally, Monte Carlo simulation was conducted to allow all variables to vary simultaneously in further effort to assess the robustness of our findings. For this analysis, variables related to costs and survival were assigned log-normal distributions, while all others were given normal distributions.53,69
RESULTS
Cost-effectiveness of In-home AED
The cost-effectiveness of the 4 alternative strategies for in-home AED deployment is shown in Table 2. Providing in-home AEDs to all adults 60 years of age (0.4% probability of SCD) costs an incremental $5,175 per person and results in a gain of 0.024 quality-adjusted life-year (QALYs), leading to a cost per QALY gained of $216,000. Limiting distribution of in-home AEDs to specific populations at increased risk of SCD results in improved cost-effectiveness ratios: individuals with multiple SCD risk factors (2% probability of SCD) cost $132,000 per QALY; individuals who had suffered a previous myocardial infarction (4% probability of SCD) cost $104,000 per QALY; and individuals with ischemic cardiomyopathy who were unable/unwilling to receive an ICD (6% probability of SCD) cost $88,000 per QALY.
Table 2.
Risk Factors for Sudden Cardiac Death
| Population | Probability of Sudden Cardiac Death | Probability of Death | Incremental Cost* ($) | Incremental Effectiveness* (QALYs) | Cost per QALY Gained ($) | Reference |
|---|---|---|---|---|---|---|
| All adults age 60 | .004 | .01 | 5175 | .024 | 216,000 | (1, 27) |
| Multiple SCD risk factors | .02 | .04 | 4930 | .037 | 132,000 | (28–31) |
| Previous MI | .04 | .06 | 4925 | .047 | 104,000 | (8, 32–34) |
| Ischemic cardiomyopathy | .06 | .10 | 4720 | .054 | 88,000 | (3, 5, 35–37) |
In-home AED compared to EMS-D.
QALY, quality-adjusted life-year; SCD, sudden cardiac death; MI, myocardial infarction; AED, automated external defibrillator; EMS-D, emergency medical services equipped with AEDs.
One-way Sensitivity Analyses
Results of one-way sensitivity analyses for selected variables performed on 2 of the selected patient cohorts (multiple SCD risk factors and ischemic cardiomyopathy) are shown in Table 3. The results were sensitive to the probability that the arrest occurred at home, the probability that the available AED was used, and the probability of suffering SCD, as demonstrated above. The cost-effectiveness of in-home AED deployment was also sensitive to changes in the relative benefit of AED deployment (strategy 2) compared to EMS-D care (strategy 1). For example, for individuals with multiple SCD risk factors, as the probability of survival to hospital discharge with EMS-D decreased from 29% to 3% (corresponding to a time-to-defibrillation delay increasing from 5 minutes to 20 minutes), the cost-effectiveness ratio for in-home AEDs decreased from $5,140,000 to $86,000 per QALY gained when compared with EMS-D. Likewise for individuals with multiple SCD risk factors, as the probability of arrest survival with an in-home AED increased from 20% to 50% (corresponding to a time-to-defibrillation delay decreasing from 7 minutes to 3 minutes), the cost per QALY gained decreased from $328,000 to $76,000. The cost-effectiveness of in-home AED deployment was relatively insensitive to variations in all cost parameters.
Table 3.
Results of One-way Sensitivity Analyses for Selected Variables
| Input | Range | Cost per QALY Gained ($) | |
|---|---|---|---|
| Multiple SCD risk factors (2% risk of SCD) | Ischemic cardiomyopathy (6% risk of SCD) | ||
| Probabilities | |||
| Probability arrest will occur at home | .4–.7 | 157,000–103,000 | 103,000–72,000 |
| Probability AED is used | .25–.75 | 193,000–84,000 | 123,000–62,000 |
| Probability of resuscitation with EMS | .15–.59 | 100,000–2,900,000 | 71,000–1,600,000 |
| Probability of resuscitation with AED | .40–.80 | 197,000–78,000 | 125,000–58,000 |
| Probability of surviving to hospital discharge with EMS | .03–.29 | 86,000–5,100,000 | 62,000–2,960,000 |
| Probability of surviving to hospital discharge with AED | .20–.50 | 328,000–76,000 | 198,000–57,000 |
| Probability of surviving arrest unimpaired | .50–.85 | 173,000–120,000 | 116,000–81,000 |
| Life expectancy of cardiac arrest survivor | 3–8 | 225,000–100,000 | 69,000–146,000 |
| Costs | |||
| AED cost | 250–2,500 | 84,000–145,000 | 55,000–98,000 |
| AED maintenance | 20–80 | 126,000–144,000 | 86,000–93,000 |
| AED training course | 25–100 | 124,000–147,000 | 85,000–95,000 |
| AED training time | 35–140 | 121,000–153,000 | 84,000–97,000 |
| Hospitalization costs: in-hospital death | 3,000–30,000 | 135,000–128000 | 91,000–84,000 |
| Hospitalization costs: survive to discharge | 40,000–100,000 | 128,000–144,000 | 85,000–100,000 |
| Future medical costs (per annum) | 9,000–20,000 | 125,000–142,000 | 82,000–99,000 |
QALY, quality-adjusted life-year; SCD, sudden cardiac death; AED, automated external defibrillator; EMS, emergency medical services.
Two-way Sensitivity Analyses
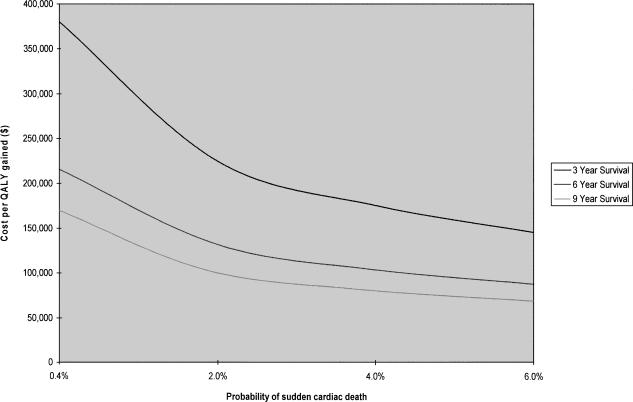
Figure 2 illustrates a two-way sensitivity analysis involving the probability of an individual suffering SCD and the life expectancy of cardiac arrest survivors. Depending upon the population considered, the annual probability of SCD in a cohort 60 years of age may range from 0.4% (all adults) to 6% (adults with ischemic cardiomyopathy). In addition, while the base-case assumed that cardiac arrest survivors would live an additional 6 years, available evidence suggests that life expectancy may be as little as 3 years or as great as 9 years. Assuming life expectancy for cardiac arrest survivors of 9 and 6 years, the cost-effectiveness ratio crosses the $100,000/QALY threshold at annual probabilities of cardiac arrest of 2% and 4%, but never falls beneath the $50,000/QALY threshold.
FIGURE 2.
Two-way sensitivity analysis involving probability of SCD and life expectancy for arrest survivors
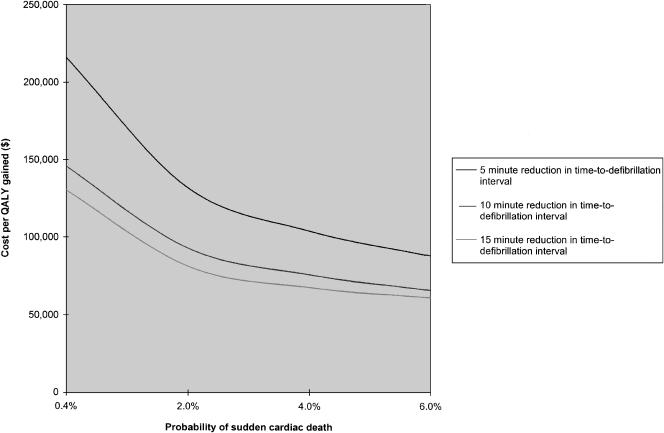
Figure 3 illustrates the impact of a two-way sensitivity analysis involving the probability of an individual suffering SCD and the absolute reduction in the time-to-defibrillation interval afforded by an in-home AED compared to EMS-D care. In the base-case, it was assumed that cardiac arrest survival with EMS-D was 15% versus 30% with an in-home AED; this corresponds to a time-to-defibrillation interval of 10 minutes for EMS-D and 5 minutes for an in-home AED (a 5-minute “time-savings” with an in-home AED). If, however, the reduction in the time-to-defibrillation interval with an in-home AED is greater, the cost-effectiveness ratio becomes more favorable. For example, if the time savings with an in-home AED is 15 minutes (i.e., time-to-defibrillation interval of 20 minutes and survival of 3% with EMS-D vs time-to-defibrillation interval of 5 minutes and survival of 30% with AED) rather than 5 minutes, the cost per QALY gained for providing in-home AEDs to individuals with a 2% probability of SCD falls from $132,000 to $86,000.
FIGURE 3.
Two-way sensitivity analysis involving probability of SCD and the reduction in the time-to-defibrillation interval offered by in-home AEDs
Multiway Sensitivity Analysis
Monte Carlo simulation conducted while holding the annual risk of cardiac arrest constant at 2% demonstrated a mean cost of $176,000 per QALY gained (standard deviation $5,800; median $159,000). The simulation demonstrated that the cost per QALY gained fell below $100,000 in 23% of all trials and below $50,000 in 4%. Monte Carlo simulation conducted while holding the annual risk of cardiac arrest constant at 4% revealed mean and median costs per QALY gained of $131,000 and $105,000, respectively; increasing the probability of cardiac arrest to 6% resulted in mean and median of $105,000 and $88,000.
Alternatively, changing 3 of our base-case assumptions simultaneously: 1) increasing the probability that an in-home AED will be used from 40% to 60%; 2) decreasing the probability of cardiac arrest survival with EMS from 15% to 10%; and 3) increasing the probability of cardiac arrest survival with an in-home AED from 30% to 40% while holding the annual probability of cardiac arrest constant at 2% reduced the cost per QALY gained from $132,000 to $65,000. Maintaining these 3 changes and simultaneously increasing the annual probability of cardiac arrest to 4% and 6% resulted in costs per QALY gained of $56,000 and $50,000, respectively.
DISCUSSION
The current analysis suggests that the cost-effectiveness of in-home AED is intimately linked to an individual's risk of cardiac arrest. While purchase of in-home AEDs may be reasonable for adults with increased risk of SCD, providing in-home AEDs to all adults is expensive when compared to commonly accepted cost-effectiveness thresholds70,71; our findings also demonstrate that the cost-effectiveness of in-home defibrillators is particularly sensitive to the reduction in the time-to-defibrillation interval that an in-home AED provides relative to EMS-D-based care. Although the decision to recommend an in-home AED to an individual patient is complex, the results of our cost-effectiveness analysis suggest that several specific clinical factors (e.g., patient risk, distance/time from EMS care) should be considered prior to making such a decision.
The fact that the cost-effectiveness of an in-home AED is sensitive to the probability of an individual suffering a cardiac arrest demonstrates that risk assessment is critical. While accurately predicting an individual's risk for SCD is currently difficult, it is possible to risk stratify individuals using widely available information such as age, cardiac risk factors, and history of coronary artery disease. The importance of an individual's risk also reinforces the importance of continued research to allow for more accurate individualized risk assessment.8,72 Also, our findings demonstrate the importance of considering the expected time-to-defibrillation interval at an individual's home. Individuals living in congested urban or remote rural areas are likely to experience prolonged delays to defibrillation and thus low survival rates in the absence of an in-home AED. Conversely, individuals living in close proximity to trained first responders are likely to experience shorter delays and receive less benefit from an in-home AED.
In discussing the current analysis, it is important to note the limitations of our work. We were deliberately conservative in all of our model estimates to avoid overestimating the effectiveness of in-home AEDs, but consequently may have underestimated the benefits offered by in-home AEDs. For example, our estimation of 15% survival of cardiac arrest with EMS-D was based upon an optimized program, but reported survival rates in most communities are 5% to 10%. We also assumed that an in-home AED would only benefit the individual for whom the device had been purchased. However, data are already emerging to suggest that in-home AEDs are likely to benefit individuals other than the person for whom the device was purchased.73,74 Modifying the model in the aforementioned ways would enhance the cost-effectiveness of in-home AEDs. In addition, the current analysis did not incorporate the fact that in-home AEDs could increase anxiety for both patients and family members, thereby worsening the cost-effectiveness of the intervention. However, such anxiety has not been previously demonstrated. Finally, our analysis did not capture potential complications resulting from in-home AED deployment, but this appears to be justified based upon the safety record of modern AEDs; the ongoing Home Use AED (HAT) trial will help to clarify the frequency of such complications.
In conclusion, in-home AEDs may be a reasonable investment for individuals at increased risk of SCD, but population-based deployment to all adults 60 years of age is relatively expensive. However, modest modifications of our conservative base-case assumptions make population-based in-home defibrillators appear more cost-effective when compared to other home safety devices that are commonly purchased. FDA approval of over-the-counter AEDs will force patients and providers to explicitly assess the risk and value that in-home AEDs provide.
References
- 1.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 2.Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2000;102(suppl):1–370. [PubMed] [Google Scholar]
- 3.A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The Antiarrhythmics Versus Implantable Defibrillators (AVID) Investigators. N Engl J Med. 1997;337:1576–83. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 4.Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med. 1996;335:1933–40. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 5.Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–83. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 6.Ezekowitz JA, Armstrong PW, McAlister FA. Implantable cardioverter defibrillators in primary and secondary prevention:a systematic review of randomized, controlled trials. Ann Intern Med. 2003;138:445–52. doi: 10.7326/0003-4819-138-6-200303180-00007. [DOI] [PubMed] [Google Scholar]
- 7.Myerburg RJ, Interian A, Jr, Mitrani RM, Kessler KM, Castellanos A. Frequency of sudden cardiac death and profiles of risk. Am J Cardiol. 1997;80:10F–19F. doi: 10.1016/s0002-9149(97)00477-3. [DOI] [PubMed] [Google Scholar]
- 8.Huikuri HV, Tapanainen JM, Lindgren K, et al. Prediction of sudden cardiac death after myocardial infarction in the beta-blocking era. Am Coll Cardiol. 2003;42:652–8. doi: 10.1016/s0735-1097(03)00783-6. [DOI] [PubMed] [Google Scholar]
- 9.Goldenberg I, Jonas M, Tenenbaum A, et al. Current smoking, smoking cessation, and the risk of sudden cardiac death in patients with coronary artery disease. Arch Intern Med. 2003;163:2301–5. doi: 10.1001/archinte.163.19.2301. [DOI] [PubMed] [Google Scholar]
- 10.Gillum RF. Sudden coronary death in the United States:1980–1985. Circulation. 1989;79:756–65. doi: 10.1161/01.cir.79.4.756. [DOI] [PubMed] [Google Scholar]
- 11.Cobb LA, Fahrenbruch CE, Walsh TR, et al. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA. 1999;281:1182–8. doi: 10.1001/jama.281.13.1182. [DOI] [PubMed] [Google Scholar]
- 12.Ladwig KH, Schoefinius A, Danner R, et al. Effects of early defibrillation by ambulance personnel on short-and long-term outcome of cardiac arrest survival:the Munich experiment. Chest. 1997;112:1584–91. doi: 10.1378/chest.112.6.1584. [DOI] [PubMed] [Google Scholar]
- 13.Stiell IG, Wells GA, Field BJ, et al. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program:Opals study phase II. Ontario prehospital advanced life support. JAMA. 1999;281:1175–81. doi: 10.1001/jama.281.13.1175. [DOI] [PubMed] [Google Scholar]
- 14.Lombardi G, Gallagher J, Gennis P. Outcome of out-of-hospital cardiac arrest in New York City. The pre-hospital arrest survival evaluation (phase) study. JAMA. 1994;271:678–83. [PubMed] [Google Scholar]
- 15.Weaver WD, Peberdy MA. Defibrillators in public places—one step closer to home. N Engl J Med. 2002;347:1223–4. doi: 10.1056/NEJMp020108. [DOI] [PubMed] [Google Scholar]
- 16.Cram P, Vijan S, Fendrick AM. Cost-effectiveness of automated external defibrillator deployment in selected public locations. J Gen Intern Med. 2003;18:745–54. doi: 10.1046/j.1525-1497.2003.21139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Public Access Defibrillation Trial Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 18.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–7. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 19.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–9. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 20.Eisenberg MS. Is it time for over-the-counter defibrillators? JAMA. 2000;284:1435–8. doi: 10.1001/jama.284.11.1435. [DOI] [PubMed] [Google Scholar]
- 21.Ornato JP, McNeill SE, Craren EJ, Nelson NM. Limitation on effectiveness of rapid defibrillation by emergency medical technicians in a rural setting. Ann Emerg Med. 1984;13:1096–9. doi: 10.1016/s0196-0644(84)80331-5. [DOI] [PubMed] [Google Scholar]
- 22.Eisenberg MS, Mengert TJ. Cardiac resuscitation. N Engl J Med. 2001;344:1304–13. doi: 10.1056/NEJM200104263441707. [DOI] [PubMed] [Google Scholar]
- 23.Moore JE, Eisenberg MS, Andresen E, Cummins RO, Hallstrom A, Litwin P. Home placement of automatic external defibrillators among survivors of ventricular fibrillation. Ann Emerg Med. 1986;15:811–2. doi: 10.1016/s0196-0644(86)80379-1. [DOI] [PubMed] [Google Scholar]
- 24.Lee TH. A shock at home can save a life. For some people, it makes sense to have an automated external defibrillator at home. Harv Heart Lett. 2003;13:6–7. [PubMed] [Google Scholar]
- 25.Rosenberg D. Home defibrillators—taking technology to heart:a portable defibrillator in every home? The Wall Street Journal. 2003:R13. March 31. [Google Scholar]
- 26.Kissel M. Taking doctors' orders out of defibrillators. The Wall Street Journal. 2004:B1. July 26. [Google Scholar]
- 27.National Center for Health Statistics. United States life tables. 2001. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr52/nvsr52_14.pdf. Accessed July 27, 2004. [PubMed]
- 28.Lindholm LH, Ibsen H, Dahlof B, et al. Cardiovascular morbidity and mortality in patients with diabetes in the losartan intervention for endpoint reduction in hypertension study (life): a randomised trial against atenolol. Lancet. 2002;359:1004–10. doi: 10.1016/S0140-6736(02)08090-X. [DOI] [PubMed] [Google Scholar]
- 29.Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death. Structure, function, and time-dependence of risk. Circulation. 1992;85(suppl):I2–I10. [PubMed] [Google Scholar]
- 30.Lindholm LH, Dahlof B, Edelman JM, et al. Effect of losartan on sudden cardiac death in people with diabetes:data from the life study. Lancet. 2003;362:619–20. doi: 10.1016/S0140-6736(03)14183-9. [DOI] [PubMed] [Google Scholar]
- 31.Haider AW, Larson MG, Benjamin EJ, Levy D. Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. J Am Coll Cardiol. 1998;32:1454–9. doi: 10.1016/s0735-1097(98)00407-0. [DOI] [PubMed] [Google Scholar]
- 32.Lloyd-Jones DM, Camargo CA, Allen LA, Giugliano RP, O'Donnell CJ. Predictors of long-term mortality after hospitalization for primary unstable angina pectoris and non-ST-elevation myocardial infarction. Am J Cardiol. 2003;92:1155–9. doi: 10.1016/j.amjcard.2003.07.022. [DOI] [PubMed] [Google Scholar]
- 33.Chang WC, Kaul P, Westerhout CM, et al. Impact of sex on long-term mortality from acute myocardial infarction vs unstable angina. Arch Intern Med. 2003;163:2476–84. doi: 10.1001/archinte.163.20.2476. [DOI] [PubMed] [Google Scholar]
- 34.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction:a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–9. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 35.Josephson ME, Callans DJ, Buxton AE. The role of the implantable cardioverter-defibrillator for prevention of sudden cardiac death. Ann Intern Med. 2000;133:901–10. doi: 10.7326/0003-4819-133-11-200012050-00015. [DOI] [PubMed] [Google Scholar]
- 36.Greenberg H, Case RB, Moss AJ, Brown MW, Carroll ER, Andrews ML. Analysis of mortality events in the multicenter automatic defibrillator implantation trial. J Am Coll Cardiol. 2004;43:1459–65. doi: 10.1016/j.jacc.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 37.Sanders GD, Hlatky MA, Every NR, et al. Potential cost-effectiveness of prophylactic use of the implantable cardioverter defibrillator or amiodarone after myocardial infarction. Ann Intern Med. 2001;135:870–83. doi: 10.7326/0003-4819-135-10-200111200-00007. [DOI] [PubMed] [Google Scholar]
- 38.Beck JR, Kassirer JP, Pauker SG. A convenient approximation of life expectancy. Validation of the method. Am J Med. 1982;73:883–8. doi: 10.1016/0002-9343(82)90786-0. [DOI] [PubMed] [Google Scholar]
- 39.Holmberg M, Holmberg S, Herlitz J. The problem of out-of-hospital cardiac-arrest prevalence of sudden death in Europe today. Am J Cardiol. 1999;83:88D–90D. doi: 10.1016/s0002-9149(98)01008-x. [DOI] [PubMed] [Google Scholar]
- 40.Callahan CM, Stump TE, Stroupe KT, Tierney WM. Cost of health care for a community of older adults in an urban academic healthcare system. J Am Geriatr Soc. 1998;46:1371–7. doi: 10.1111/j.1532-5415.1998.tb06003.x. [DOI] [PubMed] [Google Scholar]
- 41.Ackermann RT, Cheadle A, Sandhu N, Madsen L, Wagner EH, LoGerfo JP. Community exercise program use and changes in healthcare costs for older adults. Am J Prev Med. 2003;25:232–7. doi: 10.1016/s0749-3797(03)00196-x. [DOI] [PubMed] [Google Scholar]
- 42.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes:impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 43.Eisenstein EL, Shaw LK, Anstrom KJ, et al. Assessing the clinical and economic burden of coronary artery disease:1986–1998. Med Care. 2001;39:824–35. doi: 10.1097/00005650-200108000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Stroupe KT, Teal EY, Weiner M, Gradus-Pizlo I, Brater DC, Murray MD. Health care and medication costs and use among older adults with heart failure. Am J Med. 2004;116:443–50. doi: 10.1016/j.amjmed.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 45. Philips HeartStart home defibrillator. Available at: http://www.heartstarthome.com/content/heartstart_home.asp. Accessed April 21, 2004.
- 46.Groeneveld PW, Kwong JL, Liu Y, et al. Cost-effectiveness of automated external defibrillators on airlines. JAMA. 2001;286:1482–9. doi: 10.1001/jama.286.12.1482. [DOI] [PubMed] [Google Scholar]
- 47. Bureau of Labor Statistics average wage report. Available at: http://www.bls.gov/ncs/ocs/sp/ncbl0539.pdf. Accessed April 15, 2004.
- 48.Mushlin AI, Hall WJ, Zwanziger J, et al. The cost-effectiveness of automatic implantable cardiac defibrillators: results from MADIT. Circulation. 1998;97:2129–35. doi: 10.1161/01.cir.97.21.2129. [DOI] [PubMed] [Google Scholar]
- 49.Larsen G, Hallstrom A, McAnulty J, et al. Cost-effectiveness of the implantable cardioverter-defibrillator versus antiarrhythmic drugs in survivors of serious ventricular tachyarrhythmias:results of the antiarrhythmics versus implantable defibrillators (AVID) economic analysis substudy. Circulation. 2002;105:2049–57. doi: 10.1161/01.cir.0000015504.57641.d0. [DOI] [PubMed] [Google Scholar]
- 50.Weiss JP, Saynina O, McDonald KM, McClellan MB, Hlatky MA. Effectiveness and cost-effectiveness of implantable cardioverter defibrillators in the treatment of ventricular arrhythmias among Medicare beneficiaries. Am J Med. 2002;112:519–27. doi: 10.1016/s0002-9343(02)01078-1. [DOI] [PubMed] [Google Scholar]
- 51.Nichol G, Hallstrom AP, Ornato JP, et al. Potential cost-effectiveness of public access defibrillation in the United States. Circulation. 1998;97:1315–20. doi: 10.1161/01.cir.97.13.1315. [DOI] [PubMed] [Google Scholar]
- 52. Healthcare inflation index. Available at: http://www.cms.hhs.gov/statistics/health-indicators/t9.asp. Accessed March 11, 2004.
- 53.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996. eds. [Google Scholar]
- 54.Eisenberg MS, Horwood BT, Cummins RO, Reynolds-Haertle R, Hearne TR. Cardiac arrest and resuscitation: a tale of 29 cities. Ann Emerg Med. 1990;19:179–86. doi: 10.1016/s0196-0644(05)81805-0. [DOI] [PubMed] [Google Scholar]
- 55.Becker LB, Ostrander MP, Barrett J, Kondos GT. Outcome of CPR in a large metropolitan area—where are the survivors? Ann Emerg Med. 1991;20:355–61. doi: 10.1016/s0196-0644(05)81654-3. [DOI] [PubMed] [Google Scholar]
- 56.Stults KR, Brown DD, Schug VL, Bean JA. Prehospital defibrillation performed by emergency medical technicians in rural communities. N Engl J Med. 1984;310:219–23. doi: 10.1056/NEJM198401263100403. [DOI] [PubMed] [Google Scholar]
- 57.Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions:a logistic regression survival model. Circulation. 1997;96:3308–13. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 58.Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest:a graphic model. Ann Emerg Med. 1993;22:1652–8. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 59.Valenzuela TD, Spaite DW, Meislin HW, Clark LL, Wright AL, Ewy GA. Emergency vehicle intervals versus collapse-to-CPR and collapse-to-defibrillation intervals:monitoring emergency medical services system performance in sudden cardiac arrest. Ann Emerg Med. 1993;22:1678–83. doi: 10.1016/s0196-0644(05)81305-8. [DOI] [PubMed] [Google Scholar]
- 60.Bunch TJ, White RD, Gersh BJ, et al. Long-term outcomes of out-of-hospital cardiac arrest after successful early defibrillation. N Engl J Med. 2003;348:2626–33. doi: 10.1056/NEJMoa023053. [DOI] [PubMed] [Google Scholar]
- 61.Kuilman M, Bleeker JK, Hartman JA, Simoons ML. Long-term survival after out-of-hospital cardiac arrest:an 8-year follow-up. Resuscitation. 1999;41:25–31. doi: 10.1016/s0300-9572(99)00016-7. [DOI] [PubMed] [Google Scholar]
- 62.Connolly SJ, Hallstrom AP, Cappato R, et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. Eur Heart J. 2000;21:2071–8. doi: 10.1053/euhj.2000.2476. [DOI] [PubMed] [Google Scholar]
- 63.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 64.de Vos R, de Haes HCJM, Koster RW, de Haan RJ. Quality of survival after cardiopulmonary resuscitation. Arch Intern Med. 1999;159:249–54. doi: 10.1001/archinte.159.3.249. [DOI] [PubMed] [Google Scholar]
- 65.Granja C, Cabral G, Pinto AT, Costa-Pereira A. Quality of life 6-months after cardiac arrest. Resuscitation. 2002;55:37–44. doi: 10.1016/s0300-9572(02)00203-4. [DOI] [PubMed] [Google Scholar]
- 66.Sedgwick ML, Watson J, Dalziel K, Carrington DJ, Cobbe SM. Efficacy of out of hospital defibrillation by ambulance technicians using automated external defibrillators. The HeartStart Scotland Project. Resuscitation. 1992;24:73–87. doi: 10.1016/0300-9572(92)90175-c. [DOI] [PubMed] [Google Scholar]
- 67.Nichol G, Stiell IG, Hebert P, Wells GA, Vandemheen K, Laupacis A. What is the quality of life for survivors of cardiac arrest? A prospective study. Acad Emerg Med. 1999;6:95–102. doi: 10.1111/j.1553-2712.1999.tb01044.x. [DOI] [PubMed] [Google Scholar]
- 68.Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med. 1996;156:1829–36. [PubMed] [Google Scholar]
- 69.Doubilet P, Begg CB, Weinstein MC, Braun P, McNeil BJ. Probabilistic sensitivity analysis using Monte Carlo simulation. Med Decis Making. 1985;5:157–77. doi: 10.1177/0272989X8500500205. [DOI] [PubMed] [Google Scholar]
- 70.Hirth R, Chernew M, Miller E, Fendrick A, Weissert W. Willingness to pay for a quality-adjusted life year:in search of a standard. Med Decis Making. 2000;20:332–42. doi: 10.1177/0272989X0002000310. [DOI] [PubMed] [Google Scholar]
- 71.Ubel PA, Hirth RA, Chernew ME, Fendrick AM. What is the price of life and why doesn't it increase at the rate of inflation? Arch Intern Med. 2003;163:1637–41. doi: 10.1001/archinte.163.14.1637. [DOI] [PubMed] [Google Scholar]
- 72.Bailey JJ, Berson AS, Handelsman H, Hodges M. Utility of current risk stratification tests for predicting major arrhythmic events after myocardial infarction. J Am Coll Cardiol. 2001;38:1902–11. doi: 10.1016/s0735-1097(01)01667-9. [DOI] [PubMed] [Google Scholar]
- 73.Jorgenson DB, Skarr T, Russell JK, Snyder DE, Uhrbrock K. AED use in businesses, public facilities and homes by minimally trained first responders. Resuscitation. 2003;59:225–33. doi: 10.1016/s0300-9572(03)00214-4. [DOI] [PubMed] [Google Scholar]
- 74.Cram P, Vijan S, Wolbrink A, Fendrick AM. The impact of including passive benefits in cost-effectiveness analysis:the case of automated external defibrillators on commercial aircraft. Value in Health. 2003;6:466–73. doi: 10.1046/j.1524-4733.2003.64224.x. [DOI] [PubMed] [Google Scholar]
- 75.Wassertheil J, Keane G, Fisher N, Leditschke JF. Cardiac arrest outcomes at the Melbourne Cricket Ground and Shrine of Remembrance using a tiered response strategy—a forerunner to public access defibrillation. Resuscitation. 2000;44:97–104. doi: 10.1016/s0300-9572(99)00168-9. [DOI] [PubMed] [Google Scholar]
- 76.Page RL, Joglar JA, Kowal RC, et al. Use of automated external defibrillators by a U.S. airline. N Engl J Med. 2000;343:1210–6. doi: 10.1056/NEJM200010263431702. [DOI] [PubMed] [Google Scholar]