Abstract
OBJECTIVE
The patient-clinician relationship is a central feature of primary care, and recent developments in the delivery of health care have tended to limit continuity of care. The objective of this study was to evaluate the extent to which continuity of care and other factors are related to patient satisfaction.
DESIGN
Cross-sectional, mailed questionnaire study.
SETTING
Primary care clinics at 7 Veterans Affairs medical centers.
PATIENTS/PARTICIPANTS
Patients (N=21,689) participating in the Ambulatory Care Quality Improvement Project who returned the baseline Seattle Outpatient Satisfaction Questionnaire (SOSQ).
MEASUREMENTS AND MAIN RESULTS
We evaluated the association between self-reported continuity and satisfaction, after adjusting for characteristics of patients, clinics, and providers. The humanistic scale of the SOSQ measures patient satisfaction with communication skills and humanistic qualities of providers, whereas the organizational scale measures satisfaction with delivery of health care services. The mean adjusted humanistic score for patients who reported always seeing the same provider was 17.3 (95% confidence interval [CI], 15.5 to 19.1) points higher than for those who rarely saw the same provider. Similarly, the mean adjusted organizational score was 16.3 (95% CI, 14.5 to 18.1) points higher for patients who always saw the same provider compared to rarely. Demographic factors, socioeconomic status, health status, clinic site, and patient utilization of services were all associated with both the adjusted humanistic and organizational scores of the SOSQ.
CONCLUSIONS
Self-reported continuity of care is strongly associated with higher patient satisfaction. This suggests that improving continuity of care may improve patient satisfaction with providers as well as with their health care organization.
Keywords: patient satisfaction, health services research, quality of care, questionnaire design, linear models
Patients' satisfaction with their medical care is predictive of their decisions regarding choice of health care plans,1,2 compliance with prescribed regimens,3,4 and clinical outcomes.5 Several patient characteristics have been associated with general patient satisfaction including demographic factors, socioeconomic status,6–9 and general health status.10–13 In addition to patient characteristics, satisfaction is also influenced by the manner in which health care is delivered. The type of health care setting1,7 and characteristics of the medical provider, such as experience,14 age, and gender,15 are related to patients' satisfaction.
One central aspect of health care delivery that may impact patient satisfaction is continuity of care. A sustained partnership over time between a clinician and patient is considered a fundamental component of primary care.16 This longitudinal relationship ideally leads to a bond between clinician and patient, characterized by trust and a sense of responsibility.17 There is evidence that continuity of care is associated with improved outcomes such as fewer emergency department visits18,19 and hospitalizations,20 improved management of chronic diseases such as diabetes,21 and use of preventive services.22
Changes in the health care system, however, have diminished the ability of patients to choose and remain with an individual primary care provider.23,24 As a result, the degree to which continuity is maintained varies significantly among health care systems,25 and changes in coverage by health insurance plans may result in forced discontinuity, which may result in decreased knowledge of the patient by the physician and worse coordination of care.26 Also, as medical groups have become larger, call arrangements and clinic schedules may make continuity of care more difficult to maintain.27
The degree to which patients value continuity of care appears to vary depending on patient characteristics and the reason for the clinic visit. For an acute problem, many patients would not be willing to wait more than 1 day to see their regular physician.28 Another recent study suggests that increased age, more chronic medical conditions or medication use, and lower health status are associated with a higher value placed on continuity.29 There is evidence that greater continuity is related to improved patient trust in their physician30 and patient satisfaction.29,31 Patients who saw their regular doctor, and who had a longer doctor-patient relationship, were significantly more satisfied with an outpatient visit.32 There appears to be a complex interaction between continuity and satisfaction with care that may depend on the clinical setting, patient characteristics such as age or health status, and provider factors.
We sought to evaluate the relationship between continuity of care and patient satisfaction in a large sample of patients enrolled in outpatient general internal medicine clinics. In addition to continuity, other potential determinants of patient satisfaction considered in this analysis included patient demographics, health status, health care utilization, and clinic and clinician characteristics. A secondary aim of this analysis was to test the reliability and validity of the Seattle Outpatient Satisfaction Questionnaire (SOSQ), a new patient satisfaction questionnaire that was developed for use in the primary care setting.
METHODS
Setting and Data Collection
The data for this analysis were collected as part of the Ambulatory Care Quality Improvement Project (ACQUIP), conducted from February 1997 through December 1999.33 ACQUIP was a randomized trial of quality improvement interventions in general internal medicine clinics (GIMC) at 7 Department of Veterans Affairs (VA) medical centers (Birmingham, AL; Little Rock, AR; San Francisco, CA; West Los Angeles, CA; White River Junction, VT; Richmond, VA; Seattle, WA). The objective of this trial was to determine whether providing visit-based reports about patient self-reported health status, routine clinical data, and guideline recommendations to providers would improve patient care outcomes. The unit of analysis was the clinic team of providers, and all patients were assigned to a single provider within a team. Only baseline data from this study were used in this analysis.
During this study, patients at participating clinics were asked to provide regular assessments of their health and satisfaction with care. These data were linked to inpatient and outpatient administrative data that were regularly extracted from the Veterans' Health Information System Technology Architecture (VistA) computerized medical record system. The study protocol was approved by the Institutional Review Boards of the University of Washington and all participating institutions.
At entry to the ACQUIP study, patients were first sent a baseline health inventory questionnaire asking about demographic information and the presence or absence of common chronic medical conditions. This initial health inventory questionnaire also included 2 general questions about satisfaction that were rated on a 5-point Likert scale from strongly disagree to strongly agree: 1) “I am very satisfied with the medical care I receive,” and 2) “There are some things about the medical care I receive that could be better.” Patients who returned the inventory were then sent the SOSQ and the Medical Outcomes Study Short Form-36 (SF-36), a general measure of health-related quality of life (HRQoL).34
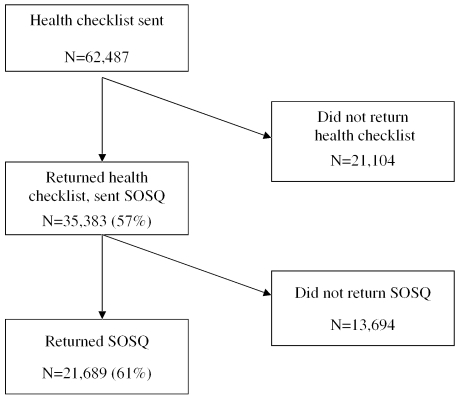
During the study, 62,487 patients were sent the baseline health inventory questionnaire. Of these, 35,383 (57%) responded and were then sent the SOSQ (Fig. 1). Of these, 21,689 (61%) returned the baseline SOSQ and comprised the cohort for the present set of analyses.
FIGURE 1.
Baseline data collection for the mailed questionnaires
Outcome Variable: Seattle Outpatient Satisfaction Questionnaire
The SOSQ was adapted from existing instruments for the ACQUIP study and consists of 21 questions asking patients about their satisfaction with the health care they receive from their primary care provider and the outpatient clinic (see Appendix available online at http://www.jgim.org). The responses to each item are recorded on a 5-point Likert scale from poor to excellent. The items are then summarized into 2 summary measures, the humanistic and organizational scales. Similar to other satisfaction scales, they were converted to scores ranging from 0 (least satisfied) to 100 (most satisfied).10,35
Humanistic Scale
This scale is comprised of 12 questions extracted from the original 23-item American Board of Internal Medicine (ABIM) patient satisfaction questionnaire first developed to assess communication skills and humanistic qualities of residents in internal medicine training programs.36 Using original data from the ABIM, we selected 10 questions with high reproducibility (generalizability coefficient >0.80) and a low percentage of missing values (<10%). Two additional items were selected that were the most relevant to the modifiable behavior of providers and contributed to the overall reliability of the scale. All items referred to the overall health care received from their primary care provider in the GIMC. Other adaptations of the ABIM questionnaire have been found to be valid and reliable measures of satisfaction with primary care physicians.37,38
Organizational Scale
This scale was comprised of 9 questions adapted from the original 47 questions in the Group Health Association of America (GHAA) consumer satisfaction survey,39 focusing on questions regarding satisfaction with health care services. The items included inquiries about access to services and length of time waiting for services. The GHAA measure has been used to assess the effect of gate keeping and utilization review on patient satisfaction7 and to assess satisfaction with access to medical care.40
Potential Determinants of Patient Satisfaction
We considered patient, provider, and health care system variables as potential predictors of patient satisfaction.
Patient-related Variables
Patient factors included demographic and socioeconomic factors, as well as self-reported health status, which has been associated with patient satisfaction.10–13,41 Health status was measured with the SF-36, which was completed by 21,423 (99%) of patients who returned the SOSQ. The 36 items comprising the SF-36 are used to construct 8 health domains that are summarized by Physical Component Summary (PCS) and Mental Component Summary (MCS) scores that are standardized to the U.S. population (mean score, 50; standard deviation [SD], 10).42
Provider-related Variables
Providers in the general internal medicine clinics included physicians, nurse practitioners, and physician assistants. Variables available through the VA administrative database included provider gender, training (staff physician, resident/fellow, or nurse practitioner/physician assistant), and average number of patients assigned per provider (panel size) at the time of the study. There were 738 different providers for the patients in the analysis, and each subject was assigned to only 1 general internal medicine provider at the time the survey was completed. The age of the provider was not available for this analysis.
Health Care Utilization and Organizational Variables
The number of GIMC visits in the 12 months prior to completion of the SOSQ questionnaire was obtained from the administrative database. Duration of receipt of care from the VA GIMC and use of non-VA medical care were obtained via questionnaire. Use of VA services is related to how far the patient lives from the facility.43 To evaluate the effect of distance to the VA medical center on satisfaction, we calculated the straight-line distance44 between the patient's residence and the VA medical center using zip codes to determine longitude and latitude (Geographic Data Technology, Lebanon, NH).
Continuity of Care
This analysis focused on continuity of care with an individual provider.45 Consistent with prior studies, continuity of care was determined by self-report.22,46,47 Patients were asked on the initial health inventory checklist how often they see the same provider when they visit the primary care clinic. The 4 choices were: always, most of the time, sometimes, and rarely or never.
Statistical Analysis
Determinants of Patient Satisfaction
We used t tests and the Wilcoxon rank-sum test for continuous variables, and the χ2 statistic for categorical variables in bivariate analysis. Multivariable linear regression was used to predict the SOSQ score and to determine independent effects of the covariates. Standard errors were determined using robust estimates of variance clustering by provider to account for correlation between observations. Because the analysis accounted for clustering by provider, standardized coefficients could not be calculated, and unstandardized coefficients are presented. To assess the relative contribution of different factors to patient satisfaction, a priori we created 7 categories of variables: continuity, demographics, socioeconomic status, health status, VA clinic site, patient clinic utilization, and provider characteristics. Linear regression models were developed sequentially, adding each category en bloc to determine the incremental explanatory ability of the variables. Age and PCS scores were found to be nonlinear covariates and were therefore modeled as quadratic terms for regression analysis. Stata version SE 7.0 (College Station, TX) statistical software was used for all analyses.
Validation of the SOSQ
We postulated that high patient satisfaction would be associated with the intention to recommend a provider to a family member.36 To test this, the SOSQ was sent again to all 35,383 respondents to the initial health checklist at the end of the ACQUIP study with the exception of those who had died or had explicitly asked to be withdrawn from the study. Of the remaining 32,129 patients sent the SOSQ at the end of the study, 16,572 (52%) patients returned the questionnaire. Included with the final SOSQ was a question asking whether the patient would want their primary care provider to care for a friend or family member. The responses were on a 5-point Likert scale: definitely yes, probably yes, not sure, probably not, definitely not.
The Cronbach's α statistic was calculated to determine the internal consistency of the SOSQ scales. The SOSQ scales were then divided into quartiles and entered in a logistic regression model to estimate the relative odds to “definitely” recommend their provider to friends or family. Logistic regression models were then adjusted for patient, clinic site, and utilization and provider characteristics to determine whether SOSQ scores were independently related to willingness to refer. The area under the receiver-operator curves (AUC) for the logistic regression models were calculated as a measure of discrimination of the SOSQ scales.
RESULTS
Patients who responded to the initial health checklist questionnaire were more likely to be older (mean age, 62 vs 56; P <.0001), married (57% vs 42%; P <.0001), white (77% vs 64%; P <.0001), and not working (75% vs 72%; P <.0001). Similarly, respondents to the second mailing who completed the SOSQ were older (mean age, 64 vs 60), and more likely to be male, married, and white than nonrespondents (Table 1). Respondents had a higher prevalence of chronic medical conditions such as ischemic heart disease (prior myocardial infarction: 18.2% vs 15.9%; P <.001) but less psychiatric illness (depression: 24.5% vs 29.8%; P <.0001). In addition, respondents reported greater continuity with their primary care provider, with 39% replying that they always saw the same provider compared to 34% in the nonrespondents. Respondents were more likely to agree that they were very satisfied with medical care they received (85% vs 80%), and less likely to think that aspects of medical care could be better (48% vs 55%). The mean PCS score for respondents was 35.1 (±12.0), or 1.5 standard deviations lower than the general U.S. population, reflecting significant functional impairment. The mean MCS score was 46.1 (SD,±13.0).
Table 1.
Characteristics of Patients Who Returned the SOSQ Compared to Those Who Did Not
| Did Not Return SOSQ N =13,694 | Returned SOSQ N =21,689 | P Value | |
|---|---|---|---|
| Mean age, y (SD) | 60.0 (13.4) | 64.0 (11.8) | <.0001 |
| Male, % | 95.9 | 96.4 | .018 |
| Married, % | 51.9 | 59.9 | <.0001 |
| White,*% | 69.7 | 81.0 | <.0001 |
| Employment, % | |||
| Not working | 71.9 | 77.1 | |
| Full-time | 18.1 | 13.2 | <.0001 |
| Part-time | 10.1 | 9.8 | |
| Income, % | |||
| <$10,000 | 32.3 | 25.7 | |
| $10,000–$20,000 | 33.0 | 37.2 | <.0001 |
| >$20,000 | 34.7 | 37.2 | |
| Education, % | |||
| <High school | 26.2 | 27.2 | |
| High school/some college | 58.3 | 56.5 | .004 |
| College/graduate school | 15.5 | 16.3 | |
| Followed in GIMC<5 years, % | 48.6 | 46.2 | <.0001 |
| Care outside the VA, % | 36.5 | 38.4 | .001 |
| Median distance to VA, miles (IQR) | 20.0 (7.2–46.8) | 25.3 (8.5–57.4) | <.0001 |
| How often sees same provider, % | |||
| Always | 33.5 | 39.1 | |
| Most of the time | 38.9 | 38.9 | <.0001 |
| Sometimes | 17.5 | 14.6 | |
| Rarely or never | 10.1 | 7.3 | |
| Very satisfied with medical care,†% | 80.0 | 85.3 | <.0001 |
| Aspects of medical care could be better,†% | 54.8 | 48.4 | <.0001 |
| Primary care visits in previous 12 months | |||
| Any visit, % | 68.8 | 71.3 | <.0001 |
| Mean number of visits (SD) | 1.6 (1.7) | 1.8 (1.8) | <.0001 |
| Female provider, % | 52.4 | 51.9 | .391 |
| Type of provider, % | |||
| Staff | 32.7 | 33.8 | |
| Resident/fellow | 42.1 | 39.9 | .001 |
| Nurse practitioner/physician assistant | 25.3 | 26.3 | |
| Provider panel size, % | |||
| 0–75 | 24.8 | 23.0 | |
| 76–175 | 21.2 | 20.2 | <.0001 |
| 176–500 | 22.1 | 23.6 | |
| >500 | 31.9 | 33.2 |
Race missing, n = 2,244 (6%).
Agree/strongly agree.
SOSQ, Seattle Outpatient Satisfaction Questionnaire; SD, standard deviation; GIMC, general internal medicine clinic; VA, Veterans Affairs; IQR, interquartile range.
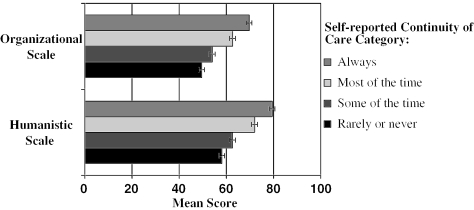
The unadjusted mean SOSQ humanistic score was 72.4 (SD,±23.9), and the mean organizational score was 64.2 (SD,±23.6). Increasing self-reported continuity of care was associated with higher patient satisfaction (Fig. 2). Patients who reported always seeing the same provider had significantly higher mean humanistic scores than those who rarely or never saw the same provider (79.4 vs 58.1; P <.0001). Similarly, mean SOSQ organizational scores were higher for patients who always saw the same provider compared to those who rarely or never did (69.7 vs 49.5; P <.0001).
FIGURE 2.
Unadjusted mean Seattle Outpatient Satisfaction Questionnaire scores by self-reported continuity of care category
Continuity continued to remain strongly associated with patient satisfaction after adjusting for patient, clinic, and provider characteristics (Table 2). Patients who always saw the same provider had mean adjusted humanistic scores that were 17.3 (95% confidence interval [CI], 15.5 to 19.1) points higher than those who rarely/never saw the same provider. Similarly, mean organizational scores were 16.3 (95% CI, 14.5 to 18.1) points higher for patients who always saw the same provider, compared to rarely/never. Among patient demographic characteristics, female gender was associated with improved satisfaction, and increasing age is associated with improved satisfaction until approximately age 70, after which satisfaction plateaus or diminishes slightly.
Table 2.
Final Multivariate Linear Regression Models to Predict SOSQ Scores
| Categories of Predictors of Patient Satisfaction | Humanistic Scale | Organizational Scale | ||
|---|---|---|---|---|
| β | P Value | β | P Value | |
| Constant | 14.31 | .004 | 3.26 | .496 |
| 1) Demographics | ||||
| Age | 0.82 | <.0001 | 0.81 | <.0001 |
| Age2 | −0.006 | <.0001 | −0.005 | <.0001 |
| Female | 3.29 | .004 | 2.26 | .020 |
| White | 0.98 | .111 | −0.69 | .220 |
| Married | 0.12 | .753 | −0.22 | .590 |
| 2) Socioeconomic status | ||||
| Education | ||||
| Less than HS graduate | ref | — | ref | — |
| HS graduate/some college | 0.38 | .401 | −0.005 | .992 |
| College graduate or more | 0.66 | .302 | −1.79 | .007 |
| Annual household income | ||||
| <$10,000 | ref | — | ref | — |
| $10,000–$20,000 | 1.97 | <.0001 | 0.48 | .323 |
| >$20,000 | 2.83 | <.0001 | 1.06 | .058 |
| Employment | ||||
| Not working | ref | — | ref | — |
| Full-time | −0.78 | .228 | −1.54 | .012 |
| Part-time | −0.72 | .206 | −1.04 | .061 |
| 3) Self-reported health | ||||
| PCS | −0.26 | .011 | −0.14 | .169 |
| PCS2 | 0.006 | <.0001 | 0.005 | <.0001 |
| MCS | 0.32 | <.0001 | 0.30 | <.0001 |
| 4) Patient utilization of medical services | ||||
| Enrolled in GIMC<5 years | 1.20 | .001 | 1.62 | <.0001 |
| Receives care outside VA | −3.06 | <.0001 | −4.18 | <.0001 |
| Primary care visits in previous 12 months | 1.27 | .021 | 1.25 | .012 |
| Distance from clinic, miles | ||||
| <10 | ref | — | ref | — |
| 10–30 | −0.15 | .757 | −0.04 | .931 |
| >30 | −0.13 | .802 | 0.37 | .494 |
| 5) VA clinic site | ||||
| 1 | ref | — | ref | — |
| 2 | 7.80 | <.0001 | 9.44 | <.0001 |
| 3 | −1.12 | .525 | 1.48 | .246 |
| 4 | −0.03 | .980 | 4.08 | <.0001 |
| 5 | 6.06 | <.0001 | 7.16 | <.0001 |
| 6 | 6.71 | <.0001 | 9.31 | <.0001 |
| 7 | −0.66 | .575 | 1.21 | .191 |
| 6) Characteristics of provider | ||||
| Female provider | 1.39 | .043 | −0.05 | .923 |
| Provider type | ||||
| Staff physician | ref | — | ref | — |
| Resident/fellow | −0.68 | .347 | −0.93 | .125 |
| Nurse practitioner/physician assistant | −0.79 | .393 | −0.15 | .846 |
| Panel size | ||||
| 0–75 | ref | — | ref | — |
| 76–175 | −0.57 | .437 | 0.22 | .715 |
| 176–500 | −2.17 | .017 | −0.99 | .175 |
| >500 | −0.40 | .761 | −0.14 | .894 |
| 7) Continuity of care | ||||
| How often patient sees the same provider | ||||
| Rarely | ref | — | ref | — |
| Sometimes | 3.57 | <.0001 | 3.28 | <.001 |
| Mostly | 11.48 | <.0001 | 10.41 | <.0001 |
| Always | 17.30 | <.0001 | 16.31 | <.0001 |
β, linear regression coefficient; SOSQ, Seattle Outpatient Satisfaction Questionnaire; VA, Veterans Affairs; HS, high school; SF-36, Short-Form 36; PCS, Physical Component Summary; MCS, Mental Component Summary; GIMC, general internal medicine clinic.
There was significant variability in mean satisfaction between clinic sites, with the largest difference of 7.8 (95% CI, 5.5 to 10.1) points for the humanistic scale, and 9.4 (95% CI, 7.8 to 11.1) points for the organizational scale (Table 2). Furthermore, patients who had received care in the primary care clinics within 12 months of returning the SOSQ questionnaire were more satisfied (humanistic score β, 1.3; 95% CI, 0.2 to 2.4) than those who did not. Among provider characteristics, female clinicians were associated with greater humanistic scores (β, 1.4; 95% CI, 0.04 to 2.7). Provider characteristics were not significantly associated with organizational scores.
The extent to which variance in satisfaction scores was explained by the different patient, clinic, and provider characteristics is shown in Table 3. Continuity of care explained 8.5% of the variance in humanistic scores and 7.7% of the variance in organizational scores. After continuity, health status accounted for the next largest proportion of overall variance, 7% for both SOSQ scales. In the final model that included all other determinants of satisfaction, the addition of continuity of care increased the R2 by 5% (P <.0001) for both SOSQ scores.
Table 3.
Variance Explained in SOSQ Scores by Models Incorporating Patient, Clinic, and Provider Characteristics
| Model | Humanistic Scale | |||
|---|---|---|---|---|
| R2 | Total R2 | Change in R2 | P Value for Change in R2 | |
| 1) Demographics | .019 | .019 | — | — |
| 2) (1)+socioeconomic status | .011 | .031 | .012 | <.0001 |
| 3) (2)+health status | .069 | .084 | .053 | <.0001 |
| 4) (3)+utilization | .010 | .094 | .010 | <.0001 |
| 5) (4)+GIMC site | .042 | .119 | .025 | <.0001 |
| 6) (5)+provider characteristics | .013 | .131 | .012 | 0.569 |
| 7) (6)+continuity | .085 | .186 | .055 | <.0001 |
| Organizational Scale | ||||
| 1) Demographics | .019 | .019 | — | — |
| 2) (1)+socioeconomic status | .004 | .025 | .006 | <.0001 |
| 3) (2)+health status | .071 | .087 | .062 | <.0001 |
| 4) (3)+utilization | .014 | .102 | .015 | <.0001 |
| 5) (4)+GIMC site | .048 | .132 | .030 | <.0001 |
| 6) (5)+provider characteristics | .014 | .143 | .011 | <.01 |
| 7) (6)+continuity | .077 | .193 | .050 | <.0001 |
Total R2, cumulative R2 with addition of each additional block of variables.
GIMC, general internal medicine clinic.
Validation of the SOSQ
The SOSQ was remailed at the end of the ACQUIP study along with a question regarding the patient's willingness to refer a friend or family member to his or her provider. Within this separate sample of 16,572 subjects, the mean humanistic score was 72.4 (±23.9), with a high internal consistency (Cronbach's α, 0.98). The mean organizational score was 62.2 (±23.9) with a Cronbach's α of 0.92. Overall, 7,720 (46.6%) patients stated that they would “definitely refer” to their provider.
Increasing humanistic and organizational scores were associated with incrementally increasing willingness to definitely refer (Table 4). For example, patients with humanistic scores in the highest quartile had an 18-fold increased relative odds of intention to definitely refer compared to those with scores in the lowest quartile. Similarly, those with organizational scores in the highest quartile had a 15-fold increased intention to refer compared to those in the lowest quartile. The relative odds for intention to definitely refer were similar after adjusting for patient, clinic, utilization, and provider factors.
Table 4.
Logistic Regression Models to Predict Intent to Definitely Refer Based on SOSQ Scores
| SOSQ Scale, by Quartiles | Intent to Definitely Refer | ||||
|---|---|---|---|---|---|
| % | OR | 95% CI | Adj. OR* | 95% CI | |
| Humanistic scale | |||||
| Lowest | 15.7 | 1.0 | Referent | 1.0 | Referent |
| Second | 37.2 | 3.17 | (2.86 to 3.51) | 3.37 | (2.94 to 3.87) |
| Third | 61.1 | 8.41 | (7.56 to 9.36) | 8.11 | (7.03 to 9.35) |
| Highest | 77.1 | 18.00 | (16.05 to 20.17) | 19.90 | (17.10 to 23.15) |
| AUC=0.76 | AUC=0.79 | ||||
| Organizational scale | |||||
| Lowest | 16.1 | 1.0 | Referent | 1.0 | Referent |
| Second | 36.6 | 3.01 | (2.70 to 3.35) | 3.02 | (2.59 to 3.52) |
| Third | 56.9 | 6.86 | (6.15 to 7.66) | 6.81 | (5.80 to 8.01) |
| Highest | 73.7 | 14.57 | (13.02 to 16.30) | 15.34 | (12.87 to 18.27) |
| AUC=0.74 | AUC=0.77 | ||||
Adj. OR, adjusted for age, age2, gender, race, marital status, continuity, education, income, employment, PCS, PCS2, MCS, clinic site, length of GIMC enrollment, care outside VA, primary care visit, distance, provider gender, provider type, and provider panel size.
SOSQ, Seattle Outpatient Satisfaction Questionnaire; OR, odds ratio; CI, confidence interval; AUC, area under the receiver operator curve; PCS, Physical Component Summary; MCS, Mental Component Summary; GIMC, general internal medicine clinic; VA, Veterans Affairs.
Receiver operator curves were created based on logistic regression models using the SOSQ scores in quartiles to predict intent to definitely refer. Both the humanistic scores (AUC, 0.76) and organizational scores (AUC, 0.74) demonstrated the ability to discriminate between those who would definitely refer, and those who would not (Table 4).
DISCUSSION
We found that self-reported continuity of care was strongly associated with patients' satisfaction with their provider and with their health care. This association persisted after extensive adjustments for characteristics of patients, providers, and practice setting. Continuity of care was found to account for a substantial proportion of the variance that could be explained by the final model, along with health status and clinic site. This is supported by the fact that the addition of continuity to a model containing all other determinants of satisfaction explained an additional 5% of the variance in both humanistic and organizational satisfaction scores.
Further supporting the strength of the association between self-reported continuity and patient satisfaction is the incremental improvement in satisfaction with increasing continuity of care. The magnitude of the effect of continuity for each category of continuity is large, with the average SOSQ humanistic score 16.8 points higher for patients who always saw their provider compared to those who rarely saw their provider. Patients who mostly saw the same provider had average scores 10 to 11 points higher. This is a larger effect on satisfaction scores than patient gender, socioeconomic status, or utilization variables.
These results are consistent with a prior study in which personal continuity with the provider as well as the length of the doctor-patient relationship were associated with general satisfaction after a specific outpatient encounter.47 A sustained patient-clinician relationship over time is an essential component of primary care.16,48 With recent changes in the organization and delivery of health care, continuity has been difficult to preserve in many settings.23,24,49 There is evidence, however, that continuity with a provider is associated with several benefits such as increased trust of patients in their physician,30 improved physician-patient communication,46 and improved outcomes, including better glycemic control among diabetics21 and less frequent hospitalizations.20,31
In addition to having a doctor who listens and sorts out problems, patients value continuity of care50 and are more likely to think that continuity is important for serious medical problems.51 Patients prefer their own practitioner who is familiar with their unique medical condition and background.51 As described by Hjortdahl and Laerum, the relationship between continuity and satisfaction is complex.47 Patients who have continuity with a provider they like tend to be more satisfied, and satisfaction with a provider helps to determine whether or not they stay with the same provider in the future. We found that continuity was associated with both satisfaction with the provider's humanistic skills and with satisfaction with the organization of, and access to, health care within the one health care system. This suggests that personal continuity with a provider also helps to ensure that the patient is able to interact with the health system more effectively.
The relationship between continuity and satisfaction that we observed did not change significantly after adjusting for other factors including provider characteristics such as gender, type of training, or panel size. Characteristics of the provider were associated with SOSQ humanistic scores, but not organizational scores. This type of survey study precluded the ability to measure individual provider factors such communication skills, which likely would contribute to patient satisfaction with their provider.
Continuity of care may be related to the clinic structure. Within the VA system, all general internal medicine clinics are organized similarly: providers are organized into practice groups, and patients are assigned to individual providers within a group. Patients are permitted to change providers if requested, and may see another provider within the group if they are unable to see their usual primary care provider. Interestingly, even though the clinic structure is the same, there were significant differences in satisfaction among clinic sites, suggesting that there are unmeasured factors within each site that contribute significantly to patient satisfaction. These may include clinic variables such as waiting times to get an appointment with their primary care provider or referral to a specialist, unmeasured differences in patient coexisting illness or health status, or provider characteristics that may have impacted the interaction between patients and their providers.
Consistent with a prior study of dual users of VA and non-VA primary care clinics, we found that patients who obtain some of their care at non-VA clinics were less satisfied with their care.9 Although we adjusted for distance, a factor known to be associated with use of VA facilities, we could not assess other potential reasons for dual use, such as patients who seek primary care from the VA due to generous VA pharmacy benefits but obtain the majority of their care at non-VA clinics.
As seen in prior studies,10–13 we found that health status is an important factor associated with patient satisfaction regarding the humanistic and organizational aspects of their care. Because patients place more importance on continuity of care for more serious illness,51 changing the health care structure to improve continuity of care for the patients with the greatest impairment in functional status due to chronic disease may significantly improve patient satisfaction.
In the final model, only 19% of the total variance could be explained by all potential explanatory variables. This is consistent with several other studies that found that less than 20% of the variance in satisfaction scores can be explained by factors such as patient expectations, health status, demographics, clinic structure, disease severity, or physician specialty.7,11,52,53 This suggests that there are a number of factors that contribute to patient satisfaction that are not routinely measured, and that future research will be needed to elucidate other important determinants of satisfaction.54
In the validation portion of this study, we found that both SOSQ scales have a high internal consistency, were strongly predictive of patient intent to refer a friend or family member to their provider, and were able to discriminate adequately between those who would refer and those who would not. These scales, therefore, appear to be valid instruments to measure patient satisfaction with providers and access to care.
There are several potential limitations to this study. Generally, satisfaction surveys are obtained via mail with varying response rates. Because the surveys in the ACQUIP study were sent sequentially to patients, we were able to assess the difference in satisfaction between responders and nonrespondents based on 2 individual items included in the initial health checklist. We found that general satisfaction, measured with these 2 items, was greater for responders than for nonrespondents. Although statistically significant, the differences in the percentage of patients who were very satisfied were small and may not suggest a clinical difference. Others have found that responders to mailed satisfaction surveys are less satisfied than those who answered onsite.55 Therefore, the method of questionnaire administration and the response rate appear to influence the results of patient satisfaction studies. Because the response rate was approximately 60% to each mailing, there were a large number of patients in ACQUIP for which the SOSQ was unavailable for analysis. Nonrespondents were less likely to be satisfied with their care, and the results of this analysis may not be generalizable to these patients.
In addition, patient continuity of care with their provider was obtained by self-report, which may be affected by recall bias. Patients who are more satisfied with their care may be more likely to report a high degree of continuity. We also had limited information on provider characteristics within the administrative database, and could not assess factors such as age of the provider, years in practice, or communication skills. We used proxies for practitioner experience such as panel size or type of training, but residual confounding may still have been present. Patients were also asked to rate their care from their primary care provider in the clinic; however, we could not confirm whether patients could correctly identify their provider or whether the provider was recently assigned. In addition, it is possible that interactions with providers outside of the GIMC may have affected satisfaction scores. These factors may have accounted for some of the differences in satisfaction seen between sites.
Finally, participants were restricted to a single health care system, the Department of Veteran Affairs, and were predominately male, less affluent, and had poorer overall health than the general U.S. population.56 The variability in satisfaction between VA clinic sites suggests that there are unmeasured factors unique to the VA and may limit generalizability to the non-VA clinic setting. Furthermore, because these VA clinic sites were affiliated with academic institutions and approximately 40% of the providers were physicians in training, these results may not apply to patients seen in other health settings. Strengths of this study include the fact that patients were sampled from a large outpatient clinic population with extensive information regarding nonrespondents, health care utilization, and patient health status.
We found that continuity of health care was strongly associated with higher satisfaction of patients with the humanistic skills of their primary care provider, and with the organization and access to care. Structuring the delivery of care to enable patients to maintain continuity of care with their provider, if desired by the patient, may improve patient satisfaction with health care.
Acknowledgments
The research reported here was supported by the Department of Veteran Affairs, Health Services Research and Development Service grants SDR 96-002, IIR 99-376, RCD 99-319, and RCD 02-170.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE., Jr Patients' ratings of outpatient visits in different practice settings. Results from the Medical Outcomes Study. JAMA. 1993;270:835–40. [PubMed] [Google Scholar]
- 2.Ware JE, Jr, Davies AR. Behavioral consequences of consumer dissatisfaction with medical care. Eval Program Plann. 1983;6:291–7. doi: 10.1016/0149-7189(83)90009-5. [DOI] [PubMed] [Google Scholar]
- 3.Hulka BS, Cassel JC, Kupper LL, Burdette JA. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public Health. 1976;66:847–53. doi: 10.2105/ajph.66.9.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uhlmann RF, Inui TS, Carter WB. Patient requests and expectations. Definitions and clinical applications. Med Care. 1984;22:681–5. doi: 10.1097/00005650-198407000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabet Med. 2003;20:486–90. doi: 10.1046/j.1464-5491.2003.00957.x. [DOI] [PubMed] [Google Scholar]
- 6.Linn MW, Linn BS, Stein SR. Satisfaction with ambulatory care and compliance in older patients. Med Care. 1982;20:606–14. doi: 10.1097/00005650-198206000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Kerr EA, Hays RD, Mitchinson A, Lee M, Siu AL. The influence of gatekeeping and utilization review on patient satisfaction. J Gen Intern Med. 1999;14:287–96. doi: 10.1046/j.1525-1497.1999.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schauffler HH, Rodriguez T. Availability and utilization of health promotion programs and satisfaction with health plan. Med Care. 1994;32:1182–96. doi: 10.1097/00005650-199412000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Borowsky SJ, Cowper DC. Dual use of VA and non-VA primary care. J Gen Intern Med. 1999;14:274–80. doi: 10.1046/j.1525-1497.1999.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Covinsky KE, Rosenthal GE, Chren MM, et al. The relation between health status changes and patient satisfaction in older hospitalized medical patients. J Gen Intern Med. 1998;13:223–9. doi: 10.1046/j.1525-1497.1998.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bidaut-Russell M, Gabriel SE, Scott CG, Zinsmeister AR, Luthra HS, Yawn B. Determinants of patient satisfaction in chronic illness. Arthritis Rheum. 2002;47:494–500. doi: 10.1002/art.10667. [DOI] [PubMed] [Google Scholar]
- 12.Hall JA, Feldstein M, Fretwell MD, Rowe JW, Epstein AM. Older patients' health status and satisfaction with medical care in an HMO population. Med Care. 1990;28:261–70. doi: 10.1097/00005650-199003000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Hall JA, Milburn MA, Epstein AM. A causal model of health status and satisfaction with medical care. Med Care. 1993;31:84–94. doi: 10.1097/00005650-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Hall JA, Dornan MC. What patients like about their medical care and how often they are asked: a meta-analysis of the satisfaction literature. Soc Sci Med. 1988;27:935–9. doi: 10.1016/0277-9536(88)90284-5. [DOI] [PubMed] [Google Scholar]
- 15.Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Satisfaction, gender, and communication in medical visits. Med Care. 1994;32:1216–31. doi: 10.1097/00005650-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Donaldson MS, Yordy KD, Lohr KN, Vanselow NA. Primary Care: America's Health in a New Era. Washington, DC: Institute of Medicine; 1996. [PubMed] [Google Scholar]
- 17.Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1:134–43. doi: 10.1370/afm.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107:524–9. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 19.Gill JM, Mainous AG, III, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med. 2000;9:333–8. doi: 10.1001/archfami.9.4.333. [DOI] [PubMed] [Google Scholar]
- 20.Mainous AG, III, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary clinician? Am J Public Health. 1998;88:1539–41. doi: 10.2105/ajph.88.10.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parchman ML, Pugh JA, Noel PH, Larme AC. Continuity of care, self-management behaviors, and glucose control in patients with type 2 diabetes. Med Care. 2002;40:137–44. doi: 10.1097/00005650-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 22.O'Malley AS, Mandelblatt J, Gold K, Cagney KA, Kerner J. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997;157:1462–70. [PubMed] [Google Scholar]
- 23.Manian FA. Whither continuity of care? N Engl J Med. 1999;340:1362–3. doi: 10.1056/NEJM199904293401712. [DOI] [PubMed] [Google Scholar]
- 24.Hjortdahl P. Continuity of care—going out of style? Br J Gen Pract. 2001;51:699–700. [PMC free article] [PubMed] [Google Scholar]
- 25.Safran DG, Tarlov AR, Rogers WH. Primary care performance in fee-for-service and prepaid health care systems. Results from the Medical Outcomes Study. JAMA. 1994;271:1579–86. [PubMed] [Google Scholar]
- 26.Flocke SA, Stange KC, Zyzanski SJ. The impact of insurance type and forced discontinuity on the delivery of primary care. J Fam Pract. 1997;45:129–35. [PubMed] [Google Scholar]
- 27.Kletke PR, Emmons DW, Gillis KD. Current trends in physicians' practice arrangements. From owners to employees. JAMA. 1996;276:555–60. [PubMed] [Google Scholar]
- 28.Love MM, Mainous AG., III Commitment to a regular physician: how long will patients wait to see their own physician for acute illness? J Fam Pract. 1999;48:202–7. [PubMed] [Google Scholar]
- 29.Nutting PA, Goodwin MA, Flocke SA, Zyzanski SJ, Stange KC. Continuity of primary care: to whom does it matter and when? Ann Fam Med. 2003;1:149–55. doi: 10.1370/afm.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients' trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13:681–6. doi: 10.1046/j.1525-1497.1998.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA. 1984;252:2413–7. [PubMed] [Google Scholar]
- 32.Hjortdahl P, Borchgrevink CF. Continuity of care: influence of general practitioners' knowledge about their patients on use of resources in consultations. BMJ. 1991;303:1181–4. doi: 10.1136/bmj.303.6811.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fihn SD, McDonell MB, Diehr P, et al. Effects of sustained audit/feedback on self-reported health status of primary care patients. Am J Med. 2004;116:241–8. doi: 10.1016/j.amjmed.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 34.Ware JE, Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- 35.Hall JA, Dornan MC. Meta-analysis of satisfaction with medical care: description of research domain and analysis of overall satisfaction levels. Soc Sci Med. 1988;27:637–44. doi: 10.1016/0277-9536(88)90012-3. [DOI] [PubMed] [Google Scholar]
- 36.Webster G. Final Report on the Patient Satisfaction Questionnaire Project. Philadelphia, PA: American Board of Internal Medicine Committee on Evaluation of Clinical Competence; 1989. [Google Scholar]
- 37.Stump TE, Dexter PR, Tierney WM, Wolinsky FD. Measuring patient satisfaction with physicians among older and diseased adults in a primary care municipal outpatient setting. An examination of three instruments. Med Care. 1995;33:958–72. [PubMed] [Google Scholar]
- 38.Harris LE, Swindle RW, Mungai SM, Weinberger M, Tierney WM. Measuring patient satisfaction for quality improvement. Med Care. 1999;37:1207–13. doi: 10.1097/00005650-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Davies A, Ware J. GHAA's Consumer Satisfaction Survey and User's Manual. 2nd ed. Washington, DC: Group Health Association of America; 1991. [Google Scholar]
- 40.Jatulis DE, Bundek NI, Legorreta AP. Identifying predictors of satisfaction with access to medical care and quality of care. Am J Med Qual. 1997;12:11–8. doi: 10.1177/0885713X9701200103. [DOI] [PubMed] [Google Scholar]
- 41.Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52:609–20. doi: 10.1016/s0277-9536(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 42.Ware JE, Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33:AS264–AS279. [PubMed] [Google Scholar]
- 43.Burgess JF, Jr, DeFiore DA. The effect of distance to VA facilities on the choice and level of utilization of VA outpatient services. Soc Sci Med. 1994;39:95–104. doi: 10.1016/0277-9536(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 44.Phibbs CS, Luft HS. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52:532–42. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 45.Lurie N. Studying access to care in managed care environments. Health Serv Res. 1997;32:691–701. [PMC free article] [PubMed] [Google Scholar]
- 46.Love MM, Mainous AG, III, Talbert JC, Hager GL. Continuity of care and the physician-patient relationship: the importance of continuity for adult patients with asthma. J Fam Pract. 2000;49:998–1004. [PubMed] [Google Scholar]
- 47.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304:1287–90. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freeman G, Hjortdahl P. What future for continuity of care in general practice? BMJ. 1997;314:1870–3. doi: 10.1136/bmj.314.7098.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moore G, Showstack J. Primary care medicine in crisis: toward reconstruction and renewal. Ann Intern Med. 2003;138:244–7. doi: 10.7326/0003-4819-138-3-200302040-00032. [DOI] [PubMed] [Google Scholar]
- 50.Lewis JR. Patient views on quality care in general practice: literature review. Soc Sci Med. 1994;39:655–70. doi: 10.1016/0277-9536(94)90022-1. [DOI] [PubMed] [Google Scholar]
- 51.Schers H, Webster S, van den Hoogen H, Avery A, Grol R, van den Bosch W. Continuity of care in general practice: a survey of patients' views. Br J Gen Pract. 2002;52:459–62. [PMC free article] [PubMed] [Google Scholar]
- 52.Linder-Pelz S. Social psychological determinants of patient satisfaction: a test of five hypotheses. Soc Sci Med. 1982;16:583–9. doi: 10.1016/0277-9536(82)90312-4. [DOI] [PubMed] [Google Scholar]
- 53.Linder-Pelz SU. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16:577–82. doi: 10.1016/0277-9536(82)90311-2. [DOI] [PubMed] [Google Scholar]
- 54.Jackson JL, Kroenke K. Patient satisfaction and quality of care. Mil Med. 1997;162:273–7. [PubMed] [Google Scholar]
- 55.Harpole LH, Orav EJ, Hickey M, Posther KE, Brennan TA. Patient satisfaction in the ambulatory setting. Influence of data collection methods and sociodemographic factors. J Gen Intern Med. 1996;11:431–4. doi: 10.1007/BF02600192. [DOI] [PubMed] [Google Scholar]
- 56.Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158:626–32. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]