Abstract
The Cancer Risk Intake System (CRIS), a computerized program that “matches” objective cancer risks to appropriate risk management recommendations, was designed to facilitate patient-clinician discussion. We evaluated CRIS in primary care settings via a single-group, self-report, pretest-posttest design. Participants completed baseline telephone surveys, used CRIS during clinic visits, and completed follow-up surveys 1 to 2 months postvisit. Compared with proportions reporting having had discussions at baseline, significantly greater proportions of participants reported having discussed tamoxifen, genetic counseling, and colonoscopy, as appropriate, after using CRIS. Most (79%) reported CRIS had “caused” their discussion. CRIS is an easily used, disseminable program that showed promising results in primary care settings.
Many individuals with elevated colorectal, breast, and ovarian cancer risks can benefit from surveillance,1–7 chemoprevention,8–12 and genetic counseling.13–16 Accordingly, the American Society of Clinical Oncology (ASCO) recommends that individuals at elevated cancer risk be counseled regarding surveillance (i.e., earlier, more frequent, or more extensive screening), chemoprevention, and prophylaxis.17 Although ASCO does not specify who should provide counseling, primary care clinicians are a likely source to whom patients will turn.18,19 Research has shown that clinician recommendation is the strongest predictor of cancer risk management behaviors20–23; there is support for focusing on patient-clinician discussions to encourage consideration of and participation in these behaviors.
However, identifying which cancer risk management topics should be discussed is challenging and time consuming in primary care settings. Determining for whom surveillance, chemoprevention, or genetic counseling is appropriate involves consideration of multiple personal and familial factors that affect cancer risk and can thus be beyond clinicians' training or time constraints. For example, colon cancer surveillance guidelines are complex and require analysis of personal and familial risk to determine which test is recommended, when it should be initiated, and at what intervals to repeat it.6 Appropriate chemoprevention recommendations involve assessment of risk, potential contraindications, and personal preferences. Whether a patient might benefit from genetic counseling is based on personal risk and family history.
It is not surprising, then, that too few at-risk individuals receive cancer risk management recommendations. Appropriate referral for and participation in cancer genetic counseling is inconsistent24,25; too few high-risk individuals are informed of the purpose and benefits of cancer genetic counseling.26,27 Not only is appropriate surveillance not achieved among individuals with elevated colorectal cancer risk, even their participation in routine screening is low.22,28,29
We sought to develop a system for efficiently facilitating patient-clinician discussions about cancer risk and risk management. Our computerized Cancer Risk Intake System (CRIS) assesses personal health history and medical conditions, family cancer history, and other risk factors for breast, ovarian, and colorectal cancers; a complex set of CRIS algorithms then uses these data to generate, for individuals and primary care clinicians, printed information tailored by the patient's risk. If objective risk is high enough, the tailored printout includes recommendations to consider one or more of the following: breast cancer chemoprevention via tamoxifen, genetic counseling, and colon cancer surveillance.
In this study, patients completed baseline surveys by phone prior to clinic visits, used CRIS during the visit, and completed follow-up telephone interviews postvisit. We sought to answer the following questions:
Following CRIS completion, were proportions of participants who reported having had discussions with their clinicians about tamoxifen, genetic counseling, or colon cancer surveillance significantly greater than the proportions reporting having done so at baseline?
Did participants who reported having had such discussions following CRIS completion perceive that CRIS had “caused” the discussions?
Which characteristics differentiated those who did versus did not have such discussions following CRIS completion?
Analyses regarding tamoxifen discussion were performed among females whose breast cancer risk was high enough to warrant receipt of a tailored tamoxifen message. Analyses for genetic counseling discussions were performed among participants whose breast, ovarian, or colon cancer risk was high enough to warrant a tailored genetic counseling message. Analyses regarding discussions about colon cancer surveillance were performed among participants with high enough risk to warrant colonoscopy but who were currently nonadherent.
METHODS
Cancer Risk Intake System
Participants used CRIS—a stand-alone application running on a touch-screen, tablet computer—in clinic waiting rooms prior to scheduled appointments. CRIS's complex algorithms select, from a library of 162 potential messages with average length of 125 words, up to 3 messages for inclusion in tailored printouts, which are generated by CRIS, printed on a portable printer, and given to participants and clinicians to aid discussions during appointments.
Tailoring Algorithm
CRIS identified patients who could benefit from discussing cancer risk and risk management with clinicians due to factors in patients' personal or family history. Whether and which tailored tamoxifen message a woman received depended on her 5-year breast cancer risk (calculated using the modified Gail model)8 and possible tamoxifen contraindications (e.g., current raloxifene administration or history of endometrial cancer, uterine hyperplasia, or clotting problems).8 Criteria for determining who to refer for cancer genetic counseling vary.30 Hence, we relied on expert opinion* to select features in patients' personal and family history that were sufficient to warrant consideration of genetic counseling. Age at diagnosis, number and degree (i.e., first-degree, second-degree) of affected relatives, and number and type of primary cancers within one individual were taken into account; these factors are generally agreed upon as important when considering whether cancer is hereditary.30 Whether and what type of tailored colon cancer testing was recommended in the printout were based on factors recommended by Burt,3 Winawer et al.,6 and the American Cancer Society (ACS).7 Specifically, a colonoscopy message was given to participants who had any of the following: a personal history of colon cancer, inflammatory bowel disease or adenomatous colon polyps, a first-degree relative with colon cancer, or more than two second-degree relatives with colon cancer.
Tailored Printouts
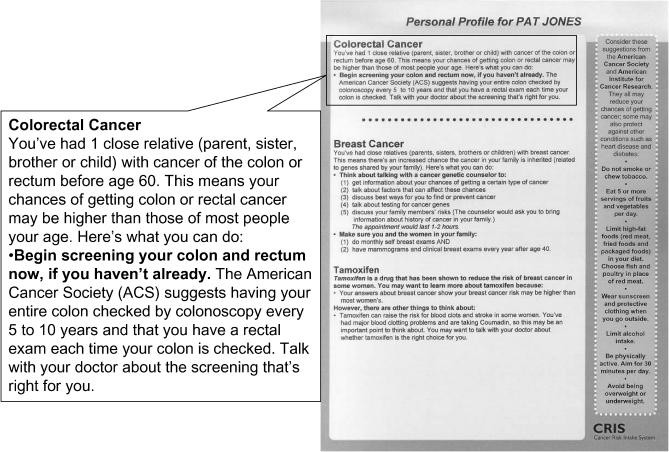
Patients' printouts used nonmedical language; clinicians' printouts used standard medical terminology and abbreviations to minimize reading time. Recommendations were stated as possible considerations for discussion. The intent was to provide patient-specific evidence-based tailored information that could be used by the patient and clinician to determine appropriate courses of action. Rather than encouraging particular behavioral decisions (“you should” meet with a genetic counselor), CRIS highlighted issues to consider and discuss. For example, a person with no personal history of colon cancer and a single first-degree relative diagnosed with colorectal cancer before age 60 received the message excerpted in Figure 1.
Figure 1.
Colorectal cancer surveillance message from sample patient printout.
Data Collection Sites and Eligibility Criteria
Participants were recruited from one clinic in North Carolina and two in Indianapolis. Clinics varied in types of patients (Medicare/Medicaid, private insurance), staff (residents, attendings, nurse practitioners, physician assistants), and practice (internal medicine, family medicine).
Individuals with primary care appointments were invited to participate if they met eligibility criteria, which included, for females, being 40 to 85 years old and not undergoing current treatment for breast, ovarian, or colon cancer, and, for males, personal or family history of breast or colon cancer. Eligibility criteria differed by gender because, in addition to topics both genders could discuss (cancer genetic counseling and colonoscopy), female participants could discuss tamoxifen, which is recommended for discussion with a broader section of the population.10 Individuals perceived by research assistants to be unable to understand informed consent, either because of language barrier or cognitive impairment, were ineligible; those with serious comorbidities, who cancelled appointments, or whose appointment conflicted with that of an already enrolled study participant were also ineligible.
Procedures
Study procedures were approved by Institutional Review Boards. During review of clinic databases, only information necessary to ascertain appointment dates and contact information was obtained. Weekly clinic database review yielded 1,290 potentially eligible patients. Research assistants mailed letters describing the study 2 to 3 weeks before individuals' appointments; upon receipt, those not interested in participating could decline by calling the project office. Baseline survey telephone contacts were attempted 1 week before scheduled appointments and continued, if necessary, until the day before appointments; 880 individuals were reached (68% of potentially eligible patients). Participants reached by telephone who did not decline (n =375, 43% of those reached) completed baseline telephone interviews and agreed to meet research assistants in clinic 20 minutes before their appointments.
At the clinics, research assistants gave participants $10 gift certificates for completing baseline interviews, reviewed the study, obtained written informed consent, explained how to use CRIS, and, after participants completed CRIS, printed and distributed patient and clinician printouts. Participants who completed CRIS (n =227, 61% of baseline completers) were contacted 31 to 60 days later for a follow-up telephone interview; follow-up completers (n =215, 95% of CRIS completers) received another $10 gift certificate.
Measures
Baseline surveys assessed whether participants had previous cancer risk–related discussions with clinicians, their perceived 5-year incidence risks for breast, ovarian, and colon cancer, and whether they had recently or planned to in the future: use tamoxifen for chemoprevention; participate in genetic counseling; or undergo colon cancer surveillance. Follow-up surveys assessed the same variables. For topics patients reported discussing with clinicians post-CRIS, the follow-up survey asked whether they thought CRIS “caused” the discussion or whether they “would have talked about it anyway.”
Analysis
Analyses compared baseline and follow-up proportions of participants who reported discussing tamoxifen, cancer genetic counseling, or colonoscopy with clinicians. McNemar's χ2 test34 was used for these analyses. Analyses were performed for 1) women whose breast cancer risk warranted receipt of a tailored tamoxifen message; 2) participants whose cancer risks warranted receipt of a tailored cancer genetic counseling message; and 3) participants whose colon cancer risk and adherence status warranted a tailored colonoscopy message. For the same subgroups, we calculated proportions who felt CRIS “caused” the discussions. Bivariate analyses determined whether race, education, marital status, perceived health, perceived breast cancer risk, perceived colon cancer risk, or perceived overall cancer risk differed significantly between those who did versus did not discuss tamoxifen, cancer genetic counseling, or colonoscopy.
RESULTS
Participant Characteristics
Participants were predominantly female, African American, and not college graduates; most perceived their health as good or excellent (Table 1). Although most did not perceive themselves likely to get breast, ovarian, or colon cancer in the next 5 years, significant proportions reported not knowing their cancer risks.
Table 1.
Patient Characteristics*
| Factors | |
|---|---|
| Gender, % (n) | |
| Female | 83 (179) |
| Male | 17 (36) |
| Average age, y (n) | 56.5 (212) |
| Race/ethnicity, % (n) | |
| White, non-Latino | 40 (85) |
| Black, non-Latino | 55 (118) |
| Other | 5 (11) |
| Highest education level completed, % (n) | |
| Grade school/junior high | 8 (18) |
| Some high school | 14 (29) |
| High school graduate | 39 (83) |
| Trade school | 4 (9) |
| Some college | 24 (51) |
| College graduate/graduate degree | 11 (24) |
| Marital status, % (n) | |
| Married | 39 (84) |
| Living with partner | 1 (3) |
| Single and never married | 17 (37) |
| Divorced | 21 (44) |
| Separated | 8 (16) |
| Widowed | 14 (31) |
| Perceived current health, % (n) | |
| Excellent | 11 (23) |
| Good | 46 (99) |
| Fair | 30 (65) |
| Poor | 13 (27) |
| Perceived breast cancer risk in next 5 years, % (n) | |
| Very unlikely | 17 (31) |
| Somewhat unlikely | 27 (48) |
| Average chance | 30 (54) |
| Somewhat likely | 6 (10) |
| Very likely | 4 (7) |
| Don't know | 16 (29) |
| Perceived ovarian cancer risk in next 5 years, % (n) | |
| Very unlikely | 30 (53) |
| Somewhat unlikely | 30 (52) |
| Average chance | 19 (33) |
| Somewhat likely | 3 (5) |
| Very likely | 1 (2) |
| Don't know | 18 (31) |
| Perceived colon cancer risk in next 5 years, % (n) | |
| Very unlikely | 20 (42) |
| Somewhat unlikely | 27 (56) |
| Average chance | 24 (51) |
| Somewhat likely | 4 (8) |
| Very likely | 2 (5) |
| Don't know | 23 (47) |
Due to missing values, not all categories sum to 215.
Primary Outcomes
Because the goal was to facilitate patient-clinician discussions, analyses compared whether more participants had such discussions after, compared to before, using CRIS. Table 2 shows these proportions at baseline and follow-up.
Table 2.
Baseline and Follow-up Discussion of Tamoxifen, Genetic Counseling, and Colonoscopy
| % Discussed at Baseline (Proportion) | % Discussed at Follow-up (Proportion) | χ2 | P Value | |
|---|---|---|---|---|
| Tamoxifen | 4.82 (4/83) | 27.71 (23/83) | 13.37 | .00026 |
| Cancer genetic counseling | 2.82 (2/71) | 28.17 (20/71) | 14.72 | .00012 |
| Colonoscopy | 16.13 (5/31) | 45.16 (14/31) | 5.40 | .0201 |
Of 177 women participants, 83 (47%) had Gail-calculated breast cancer risk high enough to warrant receipt of tailored messages on tamoxifen. Of these, a significantly greater proportion (27.7% vs 4.8%, or 23 participants vs 4 participants) reported having had discussions after receiving a tailored tamoxifen message (at follow-up), compared with baseline (P =.00026). Twenty-one of the 23 women (91.3%) who discussed tamoxifen with their clinician after receiving a tailored tamoxifen message reported the discussion was “caused” by CRIS.
Of 215 total participants, 71 (33%) had breast, ovarian, or colon cancer risk high enough to warrant receipt of tailored messages on genetic counseling. Of these, a significantly greater proportion (28.2% vs 2.8%, or 20 participants vs 2 participants) reported having had discussions after receiving a tailored genetic counseling message (at follow-up), compared with baseline (P =.00012). Sixteen of 20 participants (80%) who discussed genetic counseling with their clinician after receiving a tailored message reported the discussion was “caused” by CRIS.
Of 215 total participants, 31 (14%) had colon cancer risk high enough to warrant surveillance via colonoscopy and were currently nonadherent. Of these, a significantly greater proportion (45.2% vs 16.1%, or 14 participants vs 5 participants) reported having had discussions after receiving a tailored colonoscopy message (at follow-up), compared with baseline (P =.0201) (Table 2). Eleven of the 14 (78.6%) who discussed colonoscopy with their clinician after receiving tailored messages reported the discussion was “caused” by CRIS.
Potential Covariates
For odds ratios greater than or equal to 2.5, our study was adequately powered to detect differences by potential covariates (race, education, marital status, perceived health, and perceived cancer risk) between those who reported, at follow-up, having discussed the three topics post-CRIS versus those who did not. No differences were significant at this level.
DISCUSSION
We evaluated a computerized cancer risk intake system—CRIS—designed to facilitate patient-clinician discussions of cancer risk and risk management topics (tamoxifen for breast cancer chemoprevention, cancer genetic counseling, and colorectal cancer surveillance) and found that 1) few patients reported discussing these topics with primary care physicians prior to using CRIS and 2) significantly greater proportions reported discussing appropriate topics with clinicians after using CRIS compared with proportions reporting pre-CRIS discussions.
Percentages of appropriate patients who had discussed tamoxifen and cancer genetic counseling with clinicians increased from less than 5% to more than 25% following the CRIS intervention. Percentages of those nonadherent for colonoscopy who discussed the procedure with their clinician increased from 16% to 45%. More than three quarters of those who discussed these topics post-CRIS reported that CRIS “caused” these discussions. Although increases were highly significant, they were less than perfect; our methodology did not allow us to explain this lack of discussion but available evidence gives clues. Both patients35 and primary care physicians36 have shown limited interest in discussing risks and benefits of tamoxifen, even among high-risk women. Studies have found many primary physicians lack confidence in discussing cancer genetic counseling with patients.37–39 And, although awareness of colorectal cancer screening among U.S. physicians is high,40 discussion of screening is most common during preventive visits, compared with acute or chronic care visits.41 None of the visits in the current study were for acute care, but there could have been a preponderance of chronic care visits over preventive care visits.
Although it was not a specific goal of this project to do so, findings suggest estimates of primary care patients who might benefit from information addressed by CRIS. Almost half (47%) of all female participants had breast cancer risk high enough to warrant consideration of tamoxifen. Among males and females, 33% had risk profiles suggesting consideration of genetic counseling; 14% had risk profiles indicating benefit from, but nonadherence for, colonoscopy. The sample included more African-American and lower-education participants than are generally seen in primary care populations, but neither race nor education was associated with differences in post-CRIS discussion. Hence, one might reasonably generalize our findings to other groups of primary care patients. That there was a small but definite increased risk subgroup for each category supports the approach of using a computerized intake system to screen and identify patients for whom such cancer risk issues are important. This approach is more efficient than bringing up the topics with all patients and taking time away from discussions that, for most, would be more salient. That only small percentages of patients for whom CRIS topics were appropriate reported previous discussion with their clinicians suggests a need for such risk intake programs.
Our study produced promising findings but had several limitations. First, although patient-clinician discussion is an important starting point, real cancer control benefits only stem from appropriate behaviors; however, measuring resulting behaviors was beyond the scope of this study. For example, knowing the number of women who began taking tamoxifen would not indicate success or lack of success because, for many women, the tailored printouts highlighted contraindications for taking the drug. As highlighted by ASCO, the important factor is that patients make an informed decision, in conjunction with their primary care clinicians. We cannot determine whether having had one conversation led to “an informed decision,” but we do suggest that at least one discussion is a step in the right direction, especially considering how few participants reported having talked at all about such topics prior to using CRIS.
In addition to the limitations noted above, patient report of what was discussed with clinicians should be interpreted with caution. It is possible that participants wanted to respond favorably to interviewers regarding cancer screening history, post-CRIS discussion of cancer risk management topics, and impact of CRIS on these discussions. And, although few data on the reliability of patient report of clinician discussion of cancer risk and risk management exist, evidence from other areas of study suggests patients tend to overreport discussions.42–46 That more discussions were reported after using the CRIS intervention than at baseline may be both because 1) CRIS intervention spurred discussions and 2) due to recall bias, patients were more likely to remember recent discussions (at follow-up) than more distal discussions (at baseline). Therefore, it is possible that the intervention effect size is exaggerated. Clearly, more extensive testing through a randomized clinical trial would produce a clearer picture of CRIS's value in clinical practice.
The CRIS is not meant to be a stand-alone tool that replaces clinical judgment. Rather, it should help triage and identify patients who might benefit from additional information, and to give both them and their clinicians information to use as a starting point for discussion. Not measured in this study is whether there was a benefit in clinicians receiving information showing which topics were not relevant for particular patients. For example, was it useful to be informed that, because Ms. Smith's Gail score was under 1.66%, tamoxifen need not be discussed?
The Cancer Risk Intake System evaluated in this study is a portable, disseminable program that can be easily used in primary care settings. Such systems should continue to be evaluated; more thorough investigations of whether they facilitate efficiency in clinical practice and appropriate cancer control behavior change should be conducted.
Acknowledgments
The authors thank David Farrell, MPH, of Durham, NC's People Designs for technical development of the CRIS program, P. Kelly Marcom, MD, for consultation, research and clinic staff for assisting with data collection and CRIS intervention delivery, and Shannon D. Eaton for assisting with manuscript preparation.
Footnotes
REFERENCES
- 1.Myles J, Duffy S, Nixon R, et al. Initial results of a study into the effectiveness of breast cancer screening in a population identified to be at high risk. Revue de Epidemiologie et de Sante Publique. 2001;49:471–5. [PubMed] [Google Scholar]
- 2.Tilanus-Linthorst MM, Bartels CC, Obdeijn AI, Oudkerk M. Earlier detection of breast cancer by surveillance of women at familial risk. Eur J Cancer. 2000;36:514–9. doi: 10.1016/s0959-8049(99)00337-8. [DOI] [PubMed] [Google Scholar]
- 3.Burt RW. Colon cancer screening. Gastroenterology. 2000;119:837–53. doi: 10.1053/gast.2000.16508. [DOI] [PubMed] [Google Scholar]
- 4.Lieberman D. Screening/early detection model for colorectal cancer. Why screen? Cancer. 1994;74:2023–7. doi: 10.1002/1097-0142(19941001)74:7+<2023::aid-cncr2820741706>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 5.Brekelmans CT, Seynaeve C, Bartels CC, et al. Effectiveness of breast cancer surveillance in BRCA1/2 gene mutation carriers and women with high familial risk. J Clin Oncol. 2001;19:924–30. doi: 10.1200/JCO.2001.19.4.924. [DOI] [PubMed] [Google Scholar]
- 6.Winawer S, Fletcher R, Rex D, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale—update based on new evidence. Gastroenterology. 2003;124:544–60. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 7.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society. American Cancer Society guidelines for the early detection of cancer, 2003. CA Cancer J Clin. 2003;53:27–43. doi: 10.3322/canjclin.53.1.27. [DOI] [PubMed] [Google Scholar]
- 8.Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371–88. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- 9.Kinsinger LS, Harris R, Woolf SH, Sox HC, Lohr KN. Chemoprevention of breast cancer: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:59–69. doi: 10.7326/0003-4819-137-1-200207020-00017. [DOI] [PubMed] [Google Scholar]
- 10.Freedman AN, Graubard BI, Rao SR, McCaskill-Stevens W, Ballard-Barbash R, Gail MH. Estimates of the number of US women who could benefit from tamoxifen for breast cancer chemoprevention. J Natl Cancer Inst. 2003;95:526–32. doi: 10.1093/jnci/95.7.526. [DOI] [PubMed] [Google Scholar]
- 11.Pichert G, Bolliger B, Buser K, Pagani O. Swiss Institute for Applied Cancer Research Network for Cancer Predisposition Testing and Counseling. Evidence-based management options for women at increased breast/ovarian cancer risk. Ann Oncol. 2003;14:9–19. doi: 10.1093/annonc/mdg030. [DOI] [PubMed] [Google Scholar]
- 12.Gail MH, Costantino JP, Bryant J, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst. 1999;91:1829–46. doi: 10.1093/jnci/91.21.1829. [DOI] [PubMed] [Google Scholar]
- 13.Biesecker BB, Boehnke M, Calzone K, et al. Genetic counseling for families with inherited susceptibility to breast and ovarian cancer. JAMA. 1993;269:1970–4. [PubMed] [Google Scholar]
- 14.Morris KT, Johnson N, Krasikov N, Allen M, Dorsey P. Genetic counseling impacts decision for prophylactic surgery for patients perceived to be at high risk for breast cancer. Am J Surg. 2001;181:431–3. doi: 10.1016/s0002-9610(01)00603-1. [DOI] [PubMed] [Google Scholar]
- 15.Meiser B, Butow PN, Barratt AL, et al. Long-term outcomes of genetic counseling in women at increased risk of developing hereditary breast cancer. Patient Educ Couns. 2001;44:215–25. doi: 10.1016/s0738-3991(00)00191-9. [DOI] [PubMed] [Google Scholar]
- 16.Meiser B, Halliday JL. What is the impact of genetic counselling in women at increased risk of developing hereditary breast cancer? A meta-analytic review. Soc Sci Med. 2002;54:1463–70. doi: 10.1016/s0277-9536(01)00133-2. [DOI] [PubMed] [Google Scholar]
- 17.American Society of Clinical Oncology. American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol. 2003;21:2397–406. doi: 10.1200/JCO.2003.03.189. [DOI] [PubMed] [Google Scholar]
- 18.Collins FS. BRCA1—lots of mutations, lots of dilemmas. N Engl J Med. 1996;334:186–8. doi: 10.1056/NEJM199601183340311. [DOI] [PubMed] [Google Scholar]
- 19.Worthen HG. Inherited cancer and the primary care physician. Barriers and strategies. Cancer. 1999;86:2583–8. doi: 10.1002/(sici)1097-0142(19991201)86:11+<2583::aid-cncr16>3.3.co;2-8. [DOI] [PubMed] [Google Scholar]
- 20.Friedman LC, Woodruff A, Lane M, Weinberg AD, Cooper HP, Webb JA. Breast cancer screening behaviors and intentions among asymptomatic women 50 years of age and older. Am J Prev Med. 1995;11:218–23. [PubMed] [Google Scholar]
- 21.Love RR, Brown RL, Davis JE, Baumann LJ, Fontana SA, Sanner LA. Frequency and determinants of screening for breast cancer in primary care group practice. Arch Intern Med. 1993;153:2113–7. [PubMed] [Google Scholar]
- 22.Vernon SW. Participation in colorectal cancer screening: a review. J Natl Cancer Inst. 1997;89:1406–22. doi: 10.1093/jnci/89.19.1406. [DOI] [PubMed] [Google Scholar]
- 23.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9:426–33. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- 24.Sweet KM, Bradley TL, Westman JA. Identification and referral of families at high risk for cancer susceptibility. J Clin Oncol. 2002;20:528–37. doi: 10.1200/JCO.2002.20.2.528. [DOI] [PubMed] [Google Scholar]
- 25.Westman J, Hampel H, Bradley T. Efficacy of a touchscreen computer based family cancer history questionnaire and subsequent cancer risk assessment. J Med Genet. 2000;37:354–60. doi: 10.1136/jmg.37.5.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryan EL, Skinner CS. Risk beliefs and interest in counseling: focus-group interviews among first-degree relatives of breast cancer patients. J Cancer Educ. 1999;14:99–103. doi: 10.1080/08858199909528589. [DOI] [PubMed] [Google Scholar]
- 27.Todora HM, Skinner CS, Gidday L, Ivanovich JL, Rawl S, Whelan AJ. Perceptions of genetic risk assessment and education among first degree relatives of colorectal cancer patients and implications for physicians. Fam Pract. 2001;18:367–72. doi: 10.1093/fampra/18.4.367. [DOI] [PubMed] [Google Scholar]
- 28.Harris MA, Byles JE. A survey of screening compliance among first degree relatives of people with colon cancer in New South Wales. J Med Screen. 1997;4:29–34. doi: 10.1177/096914139700400110. [DOI] [PubMed] [Google Scholar]
- 29.Richardson JL, Danley K, Mondrus GT, Deapen D, Mack T. Adherence to screening examinations for colorectal cancer after diagnosis in a first-degree relative. Prev Med. 1995;24:166–70. doi: 10.1006/pmed.1995.1030. [DOI] [PubMed] [Google Scholar]
- 30.Hampel H, Sweet K, Westman JA, Offit K, Eng C. Referral for cancer genetics consultation: a review and compilation of risk assessment criteria. J Med Genet. 2004;41:81–91. doi: 10.1136/jmg.2003.010918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berry DA, Iversen ES, Jr, Gudbjartsson DF, et al. BRCAPRO validation, sensitivity of genetic testing of BRCA1/BRCA2, and prevalence of other breast cancer susceptibility genes. J Clin Oncol. 2002;20:2701–12. doi: 10.1200/JCO.2002.05.121. [DOI] [PubMed] [Google Scholar]
- 32.Parmigiani G, Berry D, Aguilar O. Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet. 1998;62:145–58. doi: 10.1086/301670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry D, Parmigiani G, Sanchez J, Schildkraut J, Winer E. Probability of carrying a mutation of breast-ovarian cancer gene BRCA1 based on family history. J Natl Cancer Inst. 1997;89:227–38. doi: 10.1093/jnci/89.3.227. [DOI] [PubMed] [Google Scholar]
- 34.Stokes M, David C, Koch G. Categorical Data Analysis Using the SAS System. 2nd ed. Cary, NC: SAS Institute Inc.; 2000. pp. 10–41. [Google Scholar]
- 35.Bastian LA, Lipkus IM, Kuchibhatla MN, et al. Women's interest in chemoprevention for breast cancer. Arch Intern Med. 2001;161:1639–44. doi: 10.1001/archinte.161.13.1639. [DOI] [PubMed] [Google Scholar]
- 36.Haas JS, Kaplan C, Gregorich S, Perez-Stable E, Des Jarlais G. Do physicians tailor their recommendations for breast cancer risk reduction based on patient's risk? J Gen Intern Med. 2004;19:302–9. doi: 10.1111/j.1525-1497.2004.30280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Campbell H, Holloway S, Cetnarskyj R, et al. Referrals of women with a family history of breast cancer from primary care to cancer genetics services in south-east Scotland. Br J Cancer. 2003;89:1650–6. doi: 10.1038/sj.bjc.6601348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watson E, Austoker J, Lucassen A. A study of GP referrals to a family cancer clinic for breast/ovarian cancer. Fam Pract. 2001;18:131–4. doi: 10.1093/fampra/18.2.131. [DOI] [PubMed] [Google Scholar]
- 39.Fry A, Campbell H, Gudmunsdottir H, et al. GPs' views on their role in cancer genetics services and current practice. Fam Pract. 1999;16:468–74. doi: 10.1093/fampra/16.5.468. [DOI] [PubMed] [Google Scholar]
- 40.Klabunde CN, Frame PS, Meadow A, Jones E, Nadel M, Vernon SW. A national survey of primary care physicians' colorectal cancer screening recommendations and practices. Prev Med. 2003;36:352–62. doi: 10.1016/s0091-7435(02)00066-x. [DOI] [PubMed] [Google Scholar]
- 41.Patel P, Forjuoh S, Avots-Avotins A, Patel T. Identifying opportunities for improved colorectal cancer screening in primary care. Prev Med. 2004;39:239–46. doi: 10.1016/j.ypmed.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 42.Ward J, Sanson-Fisher R. Does a 3-day workshop for family medicine trainees improve preventive care? A randomized control trial. Prev Med. 1996;25:741–7. doi: 10.1006/pmed.1996.0114. [DOI] [PubMed] [Google Scholar]
- 43.Daskalakis C, Goldberg RJ, Ockene JK, Kalan K, Hosmer DW, Jr, Pbert L. Comparison of patients' and their resident physicians' responses regarding smoking-cessation interventions. Acad Med. 1993;68:168–70. doi: 10.1097/00001888-199302000-00018. [DOI] [PubMed] [Google Scholar]
- 44.Nicholson JM, Hennrikus DJ, Lando HA, McCarty MC, Vessey J. Patient recall versus physician documentation in report of smoking cessation counselling performed in the inpatient setting. Tob Control. 2000;9:382–8. doi: 10.1136/tc.9.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roter DL, Russell NK. Validity of physician self-report in tracking patient education objectives. Health Educ Q. 1994;21:27–38. doi: 10.1177/109019819402100105. [DOI] [PubMed] [Google Scholar]
- 46.Pbert L, Adams A, Quirk M, Hebert JR, Ockene JK, Luippold RS. The patient exit interview as an assessment of physician-delivered smoking intervention: a validation study. Health Psychol. 1999;18:183–8. doi: 10.1037//0278-6133.18.2.183. [DOI] [PubMed] [Google Scholar]