Abstract
OBJECTIVE
To determine the extent to which chronic illness and disease severity affect patient satisfaction with their primary care provider in general internal medicine clinics.
DESIGN
Cross-sectional mailed questionnaire study.
SETTING
Primary care clinics at 7 Veterans Affairs medical centers.
PATIENTS/PARTICIPANTS
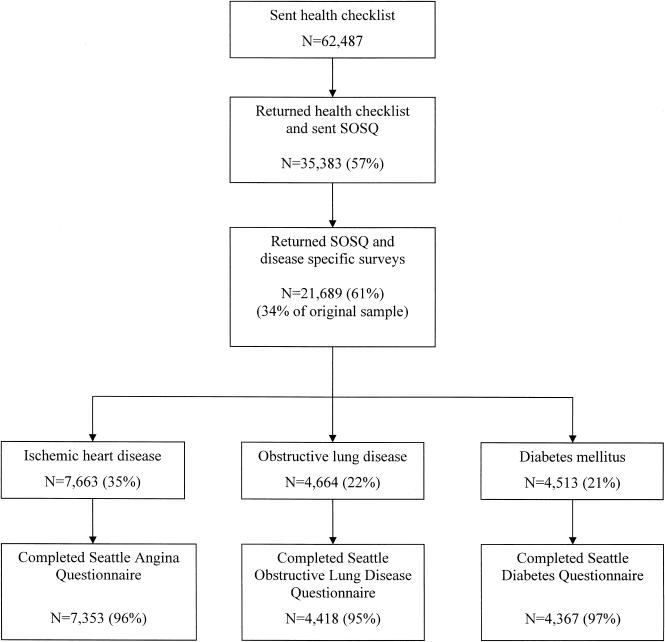
Of 62,487 patients participating in the Ambulatory Care Quality Improvement Project, 35,383 (57%) returned an initial screening questionnaire and were subsequently sent a satisfaction questionnaire. Patients (N=21,689; 61%) who returned the Seattle Outpatient Satisfaction Survey (SOSQ) were included in the final analysis, representing 34% of the original sample.
MEASUREMENTS AND MAIN RESULTS
The organizational score of the SOSQ measures satisfaction with health care services in the internal medicine clinic, and the humanistic scale measures patient satisfaction with the communication skills and humanistic qualities of the primary care physician. For ischemic heart disease (IHD), chronic obstructive pulmonary disease (COPD), and diabetes, patient ability to cope with their disease was more strongly associated with patient satisfaction than disease severity. Among IHD patients, improvement in ability to cope emotionally with their angina was associated with higher SOSQ organizational scores (standardized β=0.18; P<.001) but self-reported physical limitation due to angina was not (β=0.01; P=.65). Similarly, in COPD, improved ability to cope with dyspnea was associated with greater organizational scores (β=0.11; P<.001) but physical function was not (β=−0.03; P=.27). For diabetes, increased education was associated with improved organizational scores (β=0.31; P<.001) but improvement in symptom burden was not (β=0.03; P=.14). Similar results were seen with prediction of SOSQ humanistic scores.
CONCLUSIONS
Patient education and ability to cope with chronic conditions are more strongly associated with satisfaction with their primary care provider than disease severity. Further improvements in patient education and self-management may lead to improved satisfaction and quality of care.
Keywords: patient satisfaction, health services research, quality of care, questionnaire design, linear models
Patients' satisfaction with their health care is an important measure of health care quality.1,2 Among the many factors influencing satisfaction are health care setting,3,4 characteristics of the medical provider such as experience,5 age, or gender,6 and continuity of care.7 Along with patient characteristics such as age, gender, and income,4,8 patients' self-reported general health status has consistently predicted their satisfaction with health care.9–12
Although chronic medical conditions are associated with worse health status,13,14 the degree to which a particular illness relates to an individual patient's satisfaction with health care may vary according to the nature and severity of the condition. In earlier studies of patients with ischemic heart disease (IHD) or chronic obstructive pulmonary disease (COPD), severity of symptoms was associated with satisfaction with care received for those conditions.15,16 However, disease severity was not associated with satisfaction among patients with rheumatoid arthritis or diabetes.10,17,18
For many chronic medical conditions, current therapy may improve but not completely eliminate symptoms. Emotionally coping with chronic disease and managing symptoms may be as important as the degree of actual physical disability in determining satisfaction with care.19 Because of differing results in studies examining the association between disease severity and satisfaction, we sought to determine whether presence and severity of chronic illness was associated with general satisfaction with care among patients followed in general internal medicine clinics (GIMCs). Specifically, our objective was to compare relationships between self-reported disease severity and disease management skills with satisfaction among patients with IHD, COPD, or diabetes.
METHODS
Setting and Data Collection
Data for this analysis were collected as part of the Ambulatory Care Quality Improvement Project (ACQUIP), a randomized trial of a quality improvement intervention conducted at 7 Department of Veterans Affairs (VA) medical centers from February 1997 through December 1999.20 Subjects were enrolled in GIMCs at the participating VAs, and were sent a baseline questionnaire asking about demographics and the presence of common chronic medical conditions (Fig. 1). All patients who returned the baseline health inventory questionnaire were sent a second set of questionnaires including the Seattle Outpatient Satisfaction Questionnaire (SOSQ) and the Medical Outcomes Study Short Form-36 (SF-36), a general measure of health-related quality of life (HRQoL).21 Additionally, patients reporting selected chronic medical conditions were sent condition-specific questionnaires. Specifically, patients reporting a diagnosis of chronic lung disease were sent the Seattle Obstructive Lung Disease Questionnaire (SOLDQ), patients with IHD were sent the Seattle Angina Questionnaire (SAQ), and patients with diabetes were sent the Seattle Diabetes Questionnaire (SDQ).
FIGURE 1.
Questionnaire response and selection of patients for analysis.
Patient survey data were linked to inpatient and outpatient administrative data regularly extracted from the Veterans' Health Information System Technology Architecture (VistA) computerized medical record system. The study protocol was approved by the Institutional Review Boards at the University of Washington and all participating centers.
Outcome Variable: Seattle Outpatient Satisfaction Questionnaire
The SOSQ was adapted from existing instruments for the ACQUIP study and consists of 21 questions regarding patients' satisfaction with the health care they receive from their primary care provider and the outpatient clinic22 (see Appendix available online at http://www.jgim.org). The responses to each item are recorded on a 5-point Likert scale from poor to excellent. The items are then summarized into 2 summary scales, which are transformed to scores ranging from 0 (least satisfied) to 100 (most satisfied).
Humanistic Scale
This scale is comprised of 12 questions extracted from the original 23-item American Board of Internal Medicine (ABIM) patient satisfaction questionnaire first developed to assess communication skills and humanistic qualities of residents in internal medicine training programs.23 All items referred to overall care received from primary care providers in the GIMC. Other adaptations of the ABIM questionnaire have been found to be valid and reliable measures of satisfaction with primary care physicians.24,25
Organizational Scale
This scale contains 9 questions adapted from the Group Health Association of America (GHAA) consumer satisfaction survey26 including questions about access to services and length of time waiting for services. The GHAA measure has been used to assess the effect of gatekeeping and utilization review on patient satisfaction,4 and to assess satisfaction with access to medical care.27
Predictor Variables
Comorbidity
Comorbid conditions were obtained from the baseline inventory of chronic medical conditions. Of the 24 conditions listed on the health inventory, 4 related to coronary artery disease (angina, heart attack, coronary artery disease, and coronary artery bypass operation/balloon angioplasty) were combined into 1 variable: ischemic heart disease (IHD). To assess accuracy of self-reported conditions in the VA population, a chart review of a sample of patients reporting COPD found that a diagnosis of COPD or asthma was documented in 83/85 (97.6%) available charts.28 Similarly, compared to the medical record, the sensitivity and specificity of an IHD diagnosis were 97% and 93%, respectively.29 A diagnosis of diabetes had a sensitivity of 87.5% and a specificity of 96.1%, compared to an International Classification of Diseases, Ninth Revision (ICD-9) diagnosis (unpublished data). Additional coexisting medical conditions included arthritis, hypertension, depression, benign prostatic hypertrophy, gastroesophageal reflux disease, peptic ulcer disease, pneumonia, cancer, kidney disease, posttraumatic stress disorder, stroke, congestive heart failure, liver disease, seizures, osteoporosis, drug abuse, and HIV infection.
Disease severity and functional status for this study's 3 target conditions were ascertained using patients' self-reports on the corresponding questionnaire:
Seattle Angina Questionnaire (SAQ)
The SAQ consists of 19 items summarized into 5 scales (range 0 [worst] to 100 [best]) that measure physical limitation, angina frequency, angina stability, quality of life, and treatment satisfaction.30 Angina frequency, physical limitation due to angina, and anginal stability were used as measures of disease severity and symptom burden. The disease perception scale measured patients' adjustment to, and understanding of, their disease.
Seattle Obstructive Lung Disease Questionnaire (SOLDQ)
Comprised of 29 items, the SOLDQ measures 4 health dimensions: physical function, emotional function, coping skills, and treatment satisfaction.28 Each scale ranges from 0 (worst health) to 100 (best health). The physical function scale measures the degree to which dyspnea limits physical function and was therefore selected to measure symptom severity. The coping skills scale, a measure of COPD self-efficacy, and the emotional function scale were selected as measures of symptom self-management.
Seattle Diabetes Questionnaire (SDQ)
This contains 43 items,31 which are summarized into 7 scales (range 0–100, best possible score 100): diabetic complications, symptom burden, education received, emotional burden, self-care, glucose control, and satisfaction. The diabetes complication scale includes information on diabetic retinopathy, neuropathy, and nephropathy, and was applied as a measure of disease severity. The symptom burden scale was also chosen as a severity measure and includes 6 questions regarding thirst, weakness, numbness or tingling in arms or legs, and light headedness. The remaining scales were used as measures of diabetes self-management ability.
Additional Covariates
Characteristics of patients and study sites that might have confounded the relationship between disease severity and patient satisfaction were considered. Demographic characteristics, self-reported continuity of care, VA clinic site, a recent clinic visit, self-reported length of care in the VA GIMC, and use of non-VA medical care were also included as covariates. All models were adjusted for the 21 self-reported comorbid conditions on the health inventory.
Statistical Analysis
We performed 3 separate analyses restricted to patients with IHD, COPD, and diabetes who had completed the corresponding disease-specific questionnaire. Because most patients had multiple conditions, many were included in more than one subgroup. We first calculated the correlation between each health status scale and the SOSQ scales. To compare the correlations between health status measures and satisfaction, we used the methods described by Efron32 and Hotelling33 to calculate the associated t-statistic.
We then determined the relationship between each individual health status scale and satisfaction using bivariate linear regression. Models were created for each individual health status subscale to predict SOSQ scores. The coefficients are presented for a 10-point change in each health status scale. Although satisfaction scores were not normally distributed, we did not transform the scores for the linear regression models. Given the large sample size for each disease category, the central limit theorem guarantees that the regression coefficients and associated tests are appropriate for large samples.34
Subsequently, for each disease category, all health status subscales were included in the same multivariable linear regression model. This was done to assess the independent association between physical function and symptoms, after controlling for disease management subscales. Standardized coefficients were also calculated based on the multivariable linear regression models in order to compare the strength of association for different scales after adjustment for the other health status scales, comorbidity, and covariates including demographic factors, prior utilization, and factors related to the health care system. Standardized coefficients are obtained when both the outcome and predictor variables are measured in units of standard deviations (z-scores). Thus, standardized coefficients represent change in predicted satisfaction, measured in standard deviations, that results from a 1–standard deviation change in health status, controlling for the covariates in the model.
The health status subscales are correlated, which may cause problems with obtaining valid regression estimates and small enough confidence intervals. We therefore performed an analysis of the final multivariable models, assessing collinearity by calculating the variance inflation factors (VIF). A VIF >10 suggests that collinearity may be a problem and should be investigated.35
RESULTS
Of the 62,487 patients sent the baseline health inventory questionnaire, 35,383 (57%) responded and were mailed the satisfaction questionnaire (Fig. 1). Respondents to this initial screening questionnaire were older than nonrespondents (62.5 vs 56.5; P<.0001), slightly more likely to be male (96.2% vs 95.3%; P<.0001), married (56.8% vs 42.5%; P<.0001), and white (76.1% vs 63.6%). Only the respondents to the first questionnaire were sent the SOSQ and disease-specific questionnaires, of which 21,689 (61%) returned the surveys, representing 34% of the original sample. Nearly all patients who returned the SOSQ also returned the SF-36 (99%) and relevant disease-specific questionnaires (>95%). Respondents to the SOSQ were older than nonrespondents (64 vs 60), and more likely to be white (81% vs 70%) and married (60% vs 52%) (Table 1). There was a high prevalence of chronic medical conditions among subjects in the analysis. Participants reported a mean of 3.3 (±2.2) coexisting illnesses, including 35% who reported IHD, 22% obstructive lung disease, and 21% diabetes mellitus. The prevalence of other self-reported chronic medical conditions ranged from 54.8% (arthritis) to 0.5% (HIV infection).
Table 1.
Characteristics of Patients Who Returned the Seattle Outpatient Satisfaction Questionnaire
| Returned SOSQ | Did Not Return SOSQ | ||
|---|---|---|---|
| Characteristic | N=21,689 | N=13,694 | P Value |
| Mean age, y (SD) | 64.0 (11.8) | 60.0 (13.4) | <.001 |
| Male, % | 96.4 | 95.9 | .018 |
| Married, % | 59.9 | 51.9 | <.001 |
| White,*% | 81.0 | 69.7 | <.001 |
| Employment | |||
| Not working | 77.1 | 71.9 | <.001 |
| Full-time | 13.2 | 18.1 | |
| Part-time | 9.8 | 10.1 | |
| Income, $ | |||
| <10,000 | 25.7 | 32.3 | <.001 |
| 10,000–20,000 | 37.2 | 33.0 | |
| >20,000 | 37.2 | 34.7 | |
| Education | |||
| <High school | 27.2 | 26.2 | .004 |
| High school/some college | 56.5 | 58.3 | |
| College/graduate school | 16.3 | 15.5 | |
| Followed in GIMC >5 years | 53.8 | 51.4 | <.001 |
| Care outside the VA | 38.4 | 36.5 | .001 |
| How often sees same provider | |||
| Always | 39.1 | 33.5 | <.001 |
| Most of the time | 38.9 | 38.9 | |
| Sometimes | 14.6 | 17.5 | |
| Rarely or never | 7.3 | 10.1 | |
Race missing 6%.
SOSQ, Seattle Outpatient Satisfaction Questionnaire; SD, standard deviation; GIMC, general internal medicine clinic; VA, Veterans Affairs.
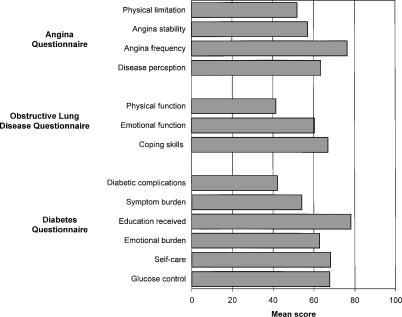
The mean SOSQ humanistic score was 72.5 (±23.9), and mean organizational score was 63.2 (±23.6) among all respondents to the SOSQ. Among IHD patients, mean angina frequency score was 76.7 (±24.5) and mean disease perception score was 63.6 (±25.5) (Fig. 2). For lung disease patients, mean physical function score was 41.9 (±25.0) and coping skills score was 67.1 (±23.8). The mean diabetic complication score was 42.0 (±35.7) and mean education score was 77.9 (±24.4).
FIGURE 2.
Mean scores on disease-specific functional status scales.
The individual health status subscales for each disease category were all significantly correlated with SOSQ satisfaction scores (Table 2). For patients with IHD, correlation between SOSQ organizational score and disease perception (r=.24) was significantly higher than correlation with physical limitation, angina frequency, or angina stability (r=.11 to .15; P<.0001 for comparison between correlations). Similarly, among COPD patients, correlation between both coping skills (r=.17) and emotional function (r=.15) with SOSQ organizational score was higher than physical function (r=.10; P<.0001 for comparison between correlations). Among patients with diabetes, educational scores were more highly correlated with organizational scores than all other scales (P<.0001). A similar pattern was seen for correlations between health status and SOSQ humanistic scores.
Table 2.
Correlations Between Each Disease-specific Health Status Subscale and Patient SOSQ Satisfaction Scores
| SOSQ Scale | ||
|---|---|---|
| Health Status Scales | Organizational | Humanistic |
| Angina questionnaire | ||
| Physical limitation | 0.15 | 0.15 |
| Angina frequency | 0.11 | 0.11 |
| Angina stability | 0.13 | 0.12 |
| Disease perception | 0.24* | 0.24* |
| Obstructive lung disease questionnaire | ||
| Physical function | 0.10* | 0.09* |
| Emotional function | 0.15 | 0.16 |
| Coping skills | 0.17 | 0.18 |
| Diabetes questionnaire | ||
| Diabetic complications | −0.07 | −0.07 |
| Symptom burden | 0.17 | 0.16 |
| Self-care | 0.12 | 0.10 |
| Glucose control | 0.07 | 0.06 |
| Emotional burden | 0.21 | 0.23 |
| Education received | 0.33* | 0.31* |
Based on pairwise tests using the method of Hotelling, this correlation coefficient is significantly different from any of the other correlations in its subset.
<.0001 for all correlation coefficients, meaning that all of the correlation coefficients are significantly different from zero.
SOSQ, Seattle Outpatient Satisfaction Questionnaire.
To determine the effect of health status subscales on patient satisfaction, linear regression models were created to predict the SOSQ organizational (Table 3) and humanistic (Table 4) scores. First, unadjusted coefficients were derived from a bivariate regression model where only one subscale is used to predict satisfaction. In this unadjusted analysis, IHD patients with a 10-point improvement in physical function had a 1.39-point improvement in SOSQ organizational score, whereas a 10-point improvement in disease perception was associated with a 2.25-point increase in organizational score. In COPD, the largest effect on satisfaction was seen in coping skills, where a 10-point increase was associated with a 1.74-point increase in the organizational score of the SOSQ. Among patients with diabetes, all individual scales except for diabetic complications were positively associated with satisfaction in the unadjusted analysis. The largest improvement in organizational scores was seen in the education scale, where a 10-point improvement predicted a 3.15-point improvement in patient satisfaction.
Table 3.
Linear Regression Models with Health Status Scales Predicting SOSQ Organizational Scores
| Unadjusted* | Adjusted† | ||||
|---|---|---|---|---|---|
| Health Status Scales | β‡ | 95% CI | β‡ | 95% CI | β§ |
| Angina questionnaire (N=7,353) | |||||
| Physical limitation | 1.39 | (1.17 to 1.62) | 0.08 | (−0.25 to 0.40) | 0.01 |
| Angina frequency | 1.02 | (0.80 to 1.25) | −0.60 | (−0.94 to−0.25) | −0.06 |
| Angina stability | 1.10 | (0.90 to 1.31) | 0.35 | (0.06 to 0.64) | 0.04 |
| Disease perception | 2.25 | (2.04 to 2.47) | 1.62 | (1.27 to 1.98) | 0.18 |
| Obstructive lung disease questionnaire (N=4,418) | |||||
| Physical function | 0.98 | (0.68 to 1.27) | −0.24 | (−0.71 to 0.23) | −0.03 |
| Emotional function | 1.46 | (1.17 to 1.74) | 0.28 | (−0.30 to 0.87) | 0.03 |
| Coping skills | 1.74 | (1.44 to 2.04) | 1.11 | (0.56 to 1.68) | 0.11 |
| Diabetes questionnaire (N=4,367) | |||||
| Diabetic complications | −0.44 | (−0.64 to−0.25) | −0.12 | (−0.35 to 0.11) | −0.02 |
| Symptom burden | 1.68 | (1.37 to 1.98) | 0.32 | (−0.10 to 0.74) | 0.03 |
| Self-care | 1.00 | (0.74 to 1.25) | −0.06 | (−0.41 to 0.29) | −0.01 |
| Glucose control | 0.53 | (0.30 to 0.76) | −0.41 | (−0.69 to−0.13) | −0.05 |
| Emotional burden | 2.25 | (1.93 to 2.57) | 1.13 | (0.73 to 1.53) | 0.11 |
| Education received | 3.15 | (2.87 to 3.42) | 2.98 | (2.61 to 3.36) | 0.31 |
A separate model was created for each health status subscale within each disease category.
One model was created for each disease category. The 3 models are adjusted for all other disease-specific subscales, comorbidity, age, gender, race, marital status, education, income, employment, VA clinic site, length of care, non-VA care, recent clinic visit, and continuity of care.
Unstandardized coefficients for each 10-point change in health status score.
Standardized coefficients.
SOSQ, Seattle Outpatient Satisfaction Questionnaire; β, linear regression coefficient; CI, confidence interval.
Table 4.
Linear Regression Models with Health Status Scales Predicting SOSQ Humanistic Scores
| Unadjusted* | Adjusted† | ||||
|---|---|---|---|---|---|
| Health Status Scales | β‡ | 95% CI | β‡ | 95% CI | β§ |
| Angina questionnaire (N=7,353) | |||||
| Physical limitation | 1.37 | (1.15 to 1.60) | −0.02 | (−0.34 to 0.31) | −0.002 |
| Angina frequency | 1.11 | (0.87 to 1.33) | −0.47 | (−0.82 to−0.12) | −0.05 |
| Angina stability | 1.04 | (0.83 to 1.25) | 0.20 | (−0.10 to 0.46) | 0.02 |
| Disease perception | 2.33 | (2.11 to 2.55) | 1.71 | (1.34 to 2.07) | 0.18 |
| Obstructive lung disease questionnaire (N=4,418) | |||||
| Physical function | 0.90 | (0.60 to 1.20) | −0.53 | (−1.02 to−0.05) | −0.05 |
| Emotional function | 1.51 | (1.22 to 1.80) | 0.41 | (−0.20 to 1.01) | 0.04 |
| Coping skills | 1.88 | (1.57 to 2.19) | 1.14 | (0.56 to 1.72) | 0.11 |
| Diabetes questionnaire (N=4,367) | |||||
| Diabetic complications | −0.49 | (−0.69 to−0.29) | −0.06 | (−0.29 to 0.17) | −0.01 |
| Symptom burden | 1.64 | (1.33 to 1.95) | 0.33 | (−0.10 to 0.75) | 0.03 |
| Self-care | 0.84 | (0.58 to 1.10) | −0.26 | (−0.62 to 0.09) | −0.03 |
| Glucose control | 0.49 | (0.25 to 0.72) | −0.27 | (−0.55 to 0.02) | −0.03 |
| Emotional burden | 2.47 | (2.15 to 2.79) | 1.43 | (1.43 to 1.84) | 0.13 |
| Education received | 3.03 | (2.75 to 3.31) | 2.73 | (2.35 to 3.11) | 0.28 |
A separate model was created for each health status subscale within each disease category.
One model was created for each disease category. The 3 models are adjusted for all other disease-specific subscales, comorbidity, age, gender, race, marital status, education, income, employment, VA clinic site, length of care, non-VA care, recent clinic visit, and continuity of care.
Unstandardized coefficients for each 10-point change in health status score.
Standardized coefficients.
SOSQ, Seattle Outpatient Satisfaction Questionnaire; β, linear regression coefficient; CI, confidence interval.
To determine whether disease severity continued to be associated with general satisfaction after adjusting for self-management factors, linear regression analyses were performed for each disease category in which all disease-specific subscales were included in the same model (Table 3 and Table 4). Standardized coefficients were calculated to compare the magnitude of the effect of one subscale to another.
For IHD patients, after adjusting for other SAQ scales (physical limitation, angina frequency, and angina stability), better disease perception (standardized β=0.18; P<.001) was associated with improved SOSQ organizational scores. This association was stronger than that for angina frequency (β=−0.06; P=.001) or stability (β=0.04; P<.02). Physical function was unrelated to satisfaction after adjustment for other scales. For comparison, the standardized coefficient for a 1–standard deviation increase in age to predict the SOSQ organizational score in IHD patients was β=0.04 (P=.006).
Among COPD patients, only the coping skills scale was associated with SOSQ organizational scores (β=0.11; P<.001) after adjustment for other SOLDQ scales. For prediction of SOSQ humanistic scores, coping skills again most strongly predicted satisfaction (β=0.11; P<.001) (Table 4). Improved physical function was actually associated with slightly worse humanistic scores after adjusting for emotional function and coping skills (β=−0.05; P<.02).
For patients with diabetes, complications and symptoms were not associated with satisfaction, whereas self-reported education received (standardized β=0.31; P<.001) and emotional burden (β=0.11; P<.001) were the strongest predictors of both SOSQ organizational and humanistic scores. Improved glucose control (β=−0.05; P=.004) was associated with slightly worsening satisfaction. Self-reported self-care practices were not associated with satisfaction in the adjusted analysis.
The VIFs were calculated for all multivariate models and were found to be between 1.30 and 4.08, suggesting collinearity between scales is not a problem in these models. Furthermore, confidence intervals for coefficients were reasonably small due to the large sample size.
DISCUSSION
In a large sample of older patients with multiple chronic medical conditions, we found that disease severity as assessed by physical limitation and symptom burden was only weakly associated with general satisfaction. In contrast, measures such as education, coping skills, or disease perception were consistently associated with greater general satisfaction with care. This suggests that clinician-patient interactions that result in improved disease understanding, but not necessarily improved symptoms, are associated with higher patient satisfaction with care.
Previous studies have focused primarily on the effect of global health status on patient satisfaction, measured with a generic HRQoL instrument such as the SF-36.8,9,11,12,36,37 The presence of chronic illnesses is strongly associated with scores on the SF-36,13 and we explored whether chronic diseases common among VA patients are associated with patient satisfaction. Furthermore, we examined the extent to which symptom burden imposed by these conditions is related to satisfaction. In this analysis of disease-specific health status, we did not adjust for general health-related quality of life, as it is likely part of the causal pathway that leads from chronic illness to satisfaction with care.
Patients value the outcomes and quality of care delivered,27,38 yet patients' expectations and ratings of quality of care may be different for acute self-limited diseases than for life-long, currently incurable medical conditions. Among outpatients presenting to a walk-in clinic, persistence of symptoms was associated with lower satisfaction 2 weeks after the initial visit.37,39 Paradoxically, the presence and severity of symptoms may be less important in determining satisfaction for patients with chronic progressive disease. They may come to accept the enduring nature of symptoms and value information on the nature of their illness and symptom management. In a prior study of outpatient VA GIMC patients, subjects were as interested in understanding their medical problem and being explained the prognosis as in relief of physical discomfort.19 The weak association between physical symptoms and satisfaction suggests that patients with chronic illness have realistic expectations about their disease.
Because of the high prevalence and costs associated with chronic medical conditions in the United States,40 there has been increased interest in improving patient self-management strategies through collaborative management between patients and clinicians.41 Given the cross-sectional design of this study, it is not possible to infer a direct causal relationship between patients' adjustment to, and understanding of, their chronic medical problems and satisfaction with care. This relationship is likely complex, because patients educated by their providers about their disease may be more satisfied with their care, and patients who are more satisfied with their providers may be more likely to adhere to education efforts. Alternatively, receiving education and support may condition their emotional response to illness and their ability to cope with their disease, affecting their satisfaction. This argument supports prior research suggesting that improving physician communication and teaching skills may enhance patient/provider partnerships, and promote better outcomes and higher satisfaction.42
For patients with IHD, improved anginal symptoms were associated with better SOSQ scores in unadjusted analyses, consistent with two prior studies.15,43 However, in adjusted models, we found that how burdensome they perceived their anginal symptoms was more strongly associated with overall satisfaction with care than the actual frequency or stability of symptoms, again suggesting that adjustment to the effects of angina on their quality of life was more important than severity of symptoms.
In the adjusted model, improvement in glucose control was associated with a slight decrease in satisfaction, after adjusting for other health status scales. This may be partly due to the burden of self-care practices such as frequent blood sugar checks or restricted diet. A similar finding was seen for IHD, where improvement in anginal frequency score (reflecting a decrease in anginal symptoms) was also associated with a slight decrease in satisfaction, after adjusting for disease perception. In addition, this may reflect the fact that these two scales measure closely related health domains, although we did not identify significant collinearity in the models. The magnitude of the effect of disease perception on patient satisfaction was larger both in univariate and multivariable linear regression, supporting the concept that enabling patients to understand their disease and cope with anginal symptoms is more important than frequency of symptoms.
For patients with COPD, there is evidence that patients are frequently dissatisfied with the quality and amount of information given to them by their providers about the causes, test results, and prognosis for their disease.16 We found that the ability to cope with dyspnea was a strong independent predictor of satisfaction in this population.
A prior study demonstrated that an index of diabetes complications predicted patient satisfaction.44 In the present analysis, however, the association between diabetic complications or symptoms with satisfaction did not persist after adjusting for diabetes education and emotional burden. This is consistent with a pilot study (n=135) in which those who received between 4 and 12 recommended explanations of their disease and self-care were significantly more satisfied than those who received less than four 17 even after adjusting for severity. Similarly, in a separate study, although comorbid conditions and diabetic symptoms were not associated with patient satisfaction, diabetes counseling and control was significantly predictive.45 Furthermore, patients with diabetes whose providers characterized the patient-clinician relationship as a partnership were more satisfied with their care.46
Our study has several limitations. Because participants in this study were predominantly male, older, less affluent, and in poorer overall health than the general U.S. population,47 the results may not pertain to patients in other health settings. Chronic medical conditions were identified by self-report, and although on chart review the accuracy of a self-reported diagnosis of IHD, lung disease, and diabetes was high, we were unable to assess the accuracy of diagnoses for other chronic medical conditions. In addition, because reliable physiologic markers were not available for all participants, we used self-reported physical function, angina frequency, and diabetes complications to gauge severity. However, for conditions such as IHD or COPD, patient perception of symptoms (e.g., angina or dyspnea) may be as valid and important a measure of severity of disease as physiologic measures. A clinically meaningful difference in satisfaction scores has not been determined for the SOSQ, limiting interpretability of results. Of note, the standardized coefficients are similar or larger in magnitude to other variables previously identified as being associated with satisfaction such as age.
Finally, due to the design of the ACQUIP study, surveys were sent sequentially. Consequently, nonresponders to the first screening questionnaire were not given the opportunity to complete the SOSQ. Although response rates to each questionnaire were approximately 60%, only 34% of patients in the original sample completed the SOSQ. These results may therefore not be generalizable to all patients in the primary care setting.
In conclusion, among patients with IHD, COPD, and diabetes, limitations in physical function and extent of symptoms were less closely related to overall satisfaction than factors such as education about their condition, coping skills, or perceived emotional burden. These results suggest that improving patients' understanding and assistance with self-management of their medical conditions may lead to improved satisfaction and quality of care in patients with chronic medical conditions.
Acknowledgments
The research reported here was supported by the Department of Veterans Affairs, Health Services Research and Development Service grants SDR 96-002, IIR 99-376, RCD 99-319, and RCD 02-170.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
REFERENCES
- 1.Rosenthal GE, Shannon SE. The use of patient perceptions in the evaluation of health-care delivery systems. Med Care. 1997;35:NS58–NS68. doi: 10.1097/00005650-199711001-00007. [DOI] [PubMed] [Google Scholar]
- 2.Davies AR, Ware JE., Jr Involving consumers in quality of care assessment. Health Aff (Millwood) 1988;7:33–48. doi: 10.1377/hlthaff.7.1.33. [DOI] [PubMed] [Google Scholar]
- 3.Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE., Jr Patients' ratings of outpatient visits in different practice settings. Results from the Medical Outcomes Study. JAMA. 1993;270:835–40. [PubMed] [Google Scholar]
- 4.Kerr EA, Hays RD, Mitchinson A, Lee M, Siu AL. The influence of gatekeeping and utilization review on patient satisfaction. J Gen Intern Med. 1999;14:287–96. doi: 10.1046/j.1525-1497.1999.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall JA, Dornan MC. What patients like about their medical care and how often they are asked a meta-analysis of the satisfaction literature. Soc Sci Med. 1988;27:935–9. doi: 10.1016/0277-9536(88)90284-5. [DOI] [PubMed] [Google Scholar]
- 6.Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Satisfaction, gender, and communication in medical visits. Med Care. 1994;32:1216–31. doi: 10.1097/00005650-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Hjortdahl P, Laerum E. Continuity of care in general practice effect on patient satisfaction. BMJ. 1992;304:1287–90. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schauffler HH, Rodriguez T. Availability and utilization of health promotion programs and satisfaction with health plan. Med Care. 1994;32:1182–96. doi: 10.1097/00005650-199412000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Covinsky KE, Rosenthal GE, Chren MM, et al. The relation between health status changes and patient satisfaction in older hospitalized medical patients. J Gen Intern Med. 1998;13:223–9. doi: 10.1046/j.1525-1497.1998.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bidaut-Russell M, Gabriel SE, Scott CG, Zinsmeister AR, Luthra HS, Yawn B. Determinants of patient satisfaction in chronic illness. Arthritis Rheum. 2002;47:494–500. doi: 10.1002/art.10667. [DOI] [PubMed] [Google Scholar]
- 11.Hall JA, Feldstein M, Fretwell MD, Rowe JW, Epstein AM. Older patients' health status and satisfaction with medical care in an HMO population. Med Care. 1990;28:261–70. doi: 10.1097/00005650-199003000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Hall JA, Milburn MA, Epstein AM. A causal model of health status and satisfaction with medical care. Med Care. 1993;31:84–94. doi: 10.1097/00005650-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Kazis LE, Ren XS, Lee A, et al. Health status in VA patients results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 14.Xuan J, Kirchdoerfer LJ, Boyer JG, Norwood GJ. Effects of comorbidity on health-related quality-of-life scores an analysis of clinical trial data. Clin Ther. 1999;21:383–403. doi: 10.1016/S0149-2918(00)88295-8. [DOI] [PubMed] [Google Scholar]
- 15.Beinart SC, Sales AE, Spertus JA, Plomondon ME, Every NR, Rumsfeld JS. Impact of angina burden and other factors on treatment satisfaction after acute coronary syndromes. Am Heart J. 2003;146:646–52. doi: 10.1016/S0002-8703(03)00256-4. [DOI] [PubMed] [Google Scholar]
- 16.Koning CJ, Maille AR, Stevens I, Dekker FW. Patients' opinions on respiratory care do doctors fulfill their needs? J Asthma. 1995;32:355–63. doi: 10.3109/02770909509082760. [DOI] [PubMed] [Google Scholar]
- 17.Gross R, Tabenkin H, Porath A, et al. The relationship between primary care physicians' adherence to guidelines for the treatment of diabetes and patient satisfaction findings from a pilot study. Fam Pract. 2003;20:563–9. doi: 10.1093/fampra/cmg512. [DOI] [PubMed] [Google Scholar]
- 18.Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002;25:458–63. doi: 10.2337/diacare.25.3.458. [DOI] [PubMed] [Google Scholar]
- 19.Joos SK, Hickam DH, Borders LM. Patients' desires and satisfaction in general medicine clinics. Public Health Rep. 1993;108:751–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Fihn SD, McDonell MB, Diehr P, et al. Effects of sustained audit/feedback on self-reported health status of primary care patients. Am J Med. 2004;116:241–8. doi: 10.1016/j.amjmed.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- 22.Fan V, Burman M, McDonell M, Fihn S. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. doi: 10.1111/j.1525-1497.2005.40135.x. doi: 10.1111/j.1525-1497.2005.40135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Webster G. Philadelphia, PA: American Board of Internal Medicine Committee on Evaluation of Clinical Competence; 1989. Final Report on the Patient Satisfaction Questionnaire Project. [Google Scholar]
- 24.Stump TE, Dexter PR, Tierney WM, Wolinsky FD. Measuring patient satisfaction with physicians among older and diseased adults in a primary care municipal outpatient setting. An examination of three instruments. Med Care. 1995;33:958–72. [PubMed] [Google Scholar]
- 25.Harris LE, Swindle RW, Mungai SM, Weinberger M, Tierney WM. Measuring patient satisfaction for quality improvement. Med Care. 1999;37:1207–13. doi: 10.1097/00005650-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Davies A, Ware J. 2nd ed. Washington, DC: Group Health Association of America; 1991. GHAA's Consumer Satisfaction Survey and User's Manual. [Google Scholar]
- 27.Jatulis DE, Bundek NI, Legorreta AP. Identifying predictors of satisfaction with access to medical care and quality of care. Am J Med Qual. 1997;12:11–8. doi: 10.1177/0885713X9701200103. [DOI] [PubMed] [Google Scholar]
- 28.Tu SP, McDonell MB, Spertus JA, Steele BG, Fihn SD. A new self-administered questionnaire to monitor health-related quality of life in patients with COPD. Ambulatory Care Quality Improvement Project (ACQUIP) Investigators. Chest. 1997;112:614–22. doi: 10.1378/chest.112.3.614. [DOI] [PubMed] [Google Scholar]
- 29.Spertus JA, McDonell M, Woodman CL, Fihn SD. Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. Am Heart J. 2000;140:105–10. doi: 10.1067/mhj.2000.106600. [DOI] [PubMed] [Google Scholar]
- 30.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–41. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 31.Reiber GE, McDonell MB, Schleyer AM, Fihn SD, Reda DJ. A comprehensive system for quality improvement in ambulatory care assessing the quality of diabetes care. Patient Educ Couns. 1995;26:337–41. doi: 10.1016/0738-3991(95)00741-h. [DOI] [PubMed] [Google Scholar]
- 32.Efron B. Comparing non-nested linear models. J Am Stat Assoc. 1984;79:791–803. [Google Scholar]
- 33.Hotelling H. The selection of variates for use in prediction with some comments on the general problem of nuisance parameters. Ann Math Stat. 1940;11:271–88. [Google Scholar]
- 34.Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–69. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 35.Kleinbaum DG, Kupper LL, Muller KE, Nizam A. 3rd ed. Pacific Grove, CA: Duxbury Press; 1998. Applied Regression Analysis and Other Multivariable Methods. [Google Scholar]
- 36.Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52:609–20. doi: 10.1016/s0277-9536(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 37.Marple RL, Kroenke K, Lucey CR, Wilder J, Lucas CA. Concerns and expectations in patients presenting with physical complaints. Frequency, physician perceptions and actions, and 2-week outcome. Arch Intern Med. 1997;157:1482–8. [PubMed] [Google Scholar]
- 38.Concato J, Feinstein AR. Asking patients what they like overlooked attributes of patient satisfaction with primary care. Am J Med. 1997;102:399–406. doi: 10.1016/s0002-9343(97)00092-2. [DOI] [PubMed] [Google Scholar]
- 39.Jackson JL, Kroenke K. Patient satisfaction and quality of care. Mil Med. 1997;162:273–7. [PubMed] [Google Scholar]
- 40.Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276:1473–9. [PubMed] [Google Scholar]
- 41.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 42.Clark NM, Gong M. Management of chronic disease by practitioners and patients are we teaching the wrong things? BMJ. 2000;320:572–5. doi: 10.1136/bmj.320.7234.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Plomondon ME, Rumsfeld JS, Humble CG, et al. Factors influencing risk-adjusted patient satisfaction after coronary artery bypass grafting. Am J Cardiol. 2003;92:206–8. doi: 10.1016/s0002-9149(03)00540-x. [DOI] [PubMed] [Google Scholar]
- 44.Kerr EA, Smith DM, Kaplan SH, Hayward RA. The association between three different measures of health status and satisfaction among patients with diabetes. Med Care Res Rev. 2003;60:158–77. doi: 10.1177/1077558703060002002. [DOI] [PubMed] [Google Scholar]
- 45.Piette JD. Satisfaction with care among patients with diabetes in two public health care systems. Med Care. 1999;37:538–46. doi: 10.1097/00005650-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Anderson LA, Zimmerman MA. Patient and physician perceptions of their relationship and patient satisfaction a study of chronic disease management. Patient Educ Couns. 1993;20:27–36. doi: 10.1016/0738-3991(93)90114-c. [DOI] [PubMed] [Google Scholar]
- 47.Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs results from the Veterans Health Study. Arch Intern Med. 1998;158:626–32. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]