Abstract
BACKGROUND
While the majority of adults are attempting weight loss at any given time, few engage in optimal diet and exercise. We examined factors associated with being in advanced stages of behavior change for weight loss, diet, and exercise.
METHODS
We surveyed primary care patients about their health, health habits, and perception and advice about weight as health risk, and about stage of readiness to lose weight, improve diet (control food portions, limit fat intake, increase fruits and vegetables), and increase planned exercise using the Prochaska Stage of Behavior Change model. We conducted bivariable analyses to describe the association between being at the preparation (change in 1 month), action (changing now), and maintenance (maintaining change) stages of change for weight loss and being at 1 of these 3 advanced stages for improving diet and exercise. We also conducted multivariable analyses to examine factors associated with being at these advanced stages of readiness to concurrently lose weight, improve diet, and increase exercise.
RESULTS
Of 365 patients (response rate of 60%), 33% were overweight (body mass index [BMI], 25.0–29.9 kg/m2) and 27% were obese (BMI, 30.0+kg/m2). Of 199 respondents at the preparation, action, or maintenance stage of losing weight, 61% were also at an advanced stage for improving diet and exercise. Those perceiving weight as a health risk were more likely to be at advanced stages of readiness to concurrently lose weight, improve diet, and increase exercise (adjusted odds ratio [AOR], 5.6; 95% CI, 2.5 to 12.5) after adjustment for confounders; this perception was associated with BMI ([AOR, 1.2; 95% CI, 1.1 to 1.3 for each unit increment in BMI]) and being advised by a physician about weight as a health risk (AOR, 6.7; 95% CI, 3.0 to 15.1). Demographic factors, having obesity-related comorbidities, and mental and physical functioning did not appear important.
CONCLUSIONS
A large proportion of primary care patients are at advanced stages of readiness to lose weight, improve diet, and increase exercise. Future studies should examine the effectiveness of primary care interventions to help patients optimize weight-related behavior.
Keywords: obsity, weight loss, stage of change, diet, exercise
Obesity is a leading cause of preventable deaths and morbidity1 and affects 30% of U.S. adults.2 Many obesity-related health risks can be reduced by modest weight loss.3–5 However, although 64% of men and 78% of women report attempts to control weight, only a minority engage in appropriate dietary habits and physical activity.6 Moreover, few patients have discussions with their physicians about weight or effective strategies to achieve sustainable weight loss.7,8
Given the high prevalence of overweight and obesity, physicians may not be able to counsel all patients at risk. Furthermore, not all patients seen in primary care are “ready” to engage in dietary and exercise behaviors essential to controlling weight.9 The Transtheoretical Model10 postulates that patients' readiness to change behavior can be assigned to 1 of 5 stages. Patients in the first 2 stages—precontemplative and contemplative—are ambivalent about making change. Patients in the 3 advanced stages—preparation, action, and maintenance—have invested some effort in planning or maintaining change and may be more likely to benefit from action-oriented behavioral interventions. While patients at earlier stages may benefit from counseling about the harms of their current behaviors and the benefits of change, patients in the preparation, action, and maintenance stages may be more receptive to advice about specific strategies to effect or sustain behavior change.11,12
Counseling about weight loss includes advice about weight loss, diet, and exercise. Assessing stage of change for multiple weight-related behaviors can be time consuming in clinical practice. Few studies have examined what proportion of patients who are at advanced stages for weight loss are also at an advanced stage for improving diet and exercise.9 One strategy may be to screen initially for patients' readiness to lose weight and then only screen for readiness to improve diet and exercise in patients motivated to lose weight. This approach may create missed opportunities, however, to counsel patients who may not want to lose weight but are motivated to exercise or improve diet.
In this context, we examined the relationship between being at advanced stages for weight loss, diet improvement, and exercise in primary care patients. We also identified factors associated with being at advanced stages of readiness to concurrently lose weight, and improve diet and exercise.
METHODS
Patient Selection and Recruitment
We conducted a telephone survey of patients seen by over 130 attending and resident physicians at one hospital-based general internal medicine practice in Boston between November 2001 and June 2003. Eligible patients were 18 years or older, English speaking, and free from serious or terminal illnesses that would prevent participation. We excluded patients whose record did not include an accurate mailing address or telephone number.
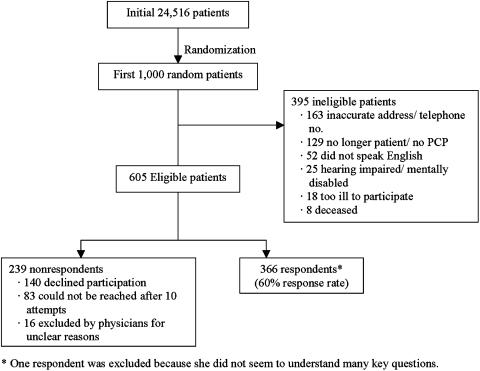
Using a computer program, we generated a randomized electronic list of 24,516 patients who received clinical care (either a visit or telephone contact) from the practice within a 2-year period and sampled the first 1,000 patients (Fig. 1). We obtained physician consent to approach patients by mail, followed by telephone contact. Patients who completed the survey were eligible for a lottery of four cash prizes of $100 each. Of 1,000 patients, our recruitment process identified 395 ineligible patients. We interviewed 366 of the remaining 605 eligible patients (response rate of 60%). Respondents and nonrespondents did not differ significantly by age, gender, or race. The Institutional Review Board at Beth Israel Deaconess Medical Center approved all study procedures.
FIGURE 1.
Sample selection.
Data Collection and Measures
The telephone survey collected information about patient demographics, self-reported height and weight, comorbid illnesses, and health habits. We asked patients how many times in the preceding 2 weeks they participated in vigorous activity and how many minutes on average they were active, adapting items from the National Health Interview Survey.13 We assigned a value of 10 kilocalories (Kcal) for each minute of vigorous activity and converted to an estimate of total Kcal expended per week.14 In addition, we assessed patients' perception of weight, how easy it would be to lose weight equivalent to 10% of their weight, and whether a doctor had ever told them that their weight was a health risk. Quality of life was assessed using the Medical Outcomes Study Short Form-36 (SF-36).15
We assessed patients' readiness to lose weight and to change several weight-related behaviors (reduce portion size; reduce fat intake; increase fruit and vegetable intake; and increase planned exercise) based on Logue et al.'s application of the Prochaska's stage of change conceptual framework.9 Logue selected these behaviors because they represented behaviors the research literature and public health guidelines emphasize as important to produce a negative energy balance.9 Logue's single-item stage of change measures for portion control, dietary fat, fruit and vegetable intake, and physical activity have been shown to correlate cross-sectionally with body mass index (BMI) and abdominal girth.9 We classified respondents into 5 different stages for each behavior: precontemplative (no plans to change for the next 6 months), contemplative (thinking about changing in the next 6 months), preparation (thinking about changing in the next month), action (attempting change currently), and maintenance (changed behavior and attempting to maintain change).
Respondents initially classified as in the maintenance stage for dietary behavior and planned exercise were reclassified as precontemplative if their current behavior was not at targeted levels. Specifically, we reclassified respondents: for portion control and fat intake if they limited fat intake and food portions “some of the time,”“rarely,” or “almost never” instead of “most of the time” or “all of the time”; for fruit and vegetable intake if they reported less than 5 servings per day; and for planned exercise if they expended less than 1,000 Kcal/week of vigorous activity as recommended by guidelines.14 Similarly, respondents classified as precontemplative for dietary and physical activity behavior but who were at the target levels of that behavior were reclassified as being in the maintenance stage.
We were interested in describing patients who were concurrently at 1 of the 3 advanced stages of change for weight loss, exercise, and dietary improvement. Therefore, we further classified patients into 2 groups: the first group was comprised of patients at advanced stages of readiness defined as being in the preparation, action, or maintenance stage of readiness to lose weight, increase planned exercise, and engage in at least 1 of 3 dietary behaviors (reduce portion size, reduce fat intake, or increase fruits and vegetables); we believed respondents at these stages would be most receptive to and potentially more likely to benefit from clinical advice about specific strategies to achieve and sustain weight loss and behavioral changes. All other patients were categorized into a second group.
Data Analysis
In bivariable analyses, we used the χ2 statistic to examine the unadjusted relationship between several factors and being at advanced stages of readiness to concurrently lose weight and improve diet and exercise. Factors of interest included sociodemographic factors (age, gender, race, educational level), BMI (weight in kg/[height in m]2), having at least 1 major obesity-related comorbidity (see Table 1), the physical and mental component scores of the SF-36, patients' perception of weight as a health risk, having been told by a doctor that their weight was a health risk, and whether respondents thought losing weight equivalent to 10% of their initial weight “was easy” (strongly agree, agree, disagree, strongly disagree). We developed a logistic regression model, using forward selection to retain factors of interest in the model at or below a P value of .10 and backward elimination to eliminate factors at or exceeding a P value of .05. We included as confounders factors that when added to the model altered the coefficient of independent predictors by 10% or more. We repeated our analysis among patients with a BMI 25 kg/m2 or higher. In post hoc analysis, we used a similar approach to examine factors associated with perception of weight as a health risk among respondents with a BMI 25 kg/m2 or higher. Finally, we used the χ2 statistic to examine the unadjusted relationship between being at an advanced stage to lose weight and being at these stages to improve diet and exercise.
Table 1.
Baseline Characteristics and Stage of Readiness to Concurrently Lose Weight and Change Diet and Exercise
| Percent of Sample | Percent at Advanced Stages for Weight Loss and Change in Diet and Exercise* | |
|---|---|---|
| Gender | ||
| Men | 35 | 37 |
| Women | 65 | 42 |
| Race | ||
| White | 74 | 40 |
| Black | 22 | 43 |
| Hispanic | 4 | 36 |
| Education† | ||
| High school or less | 21 | 30 |
| Some college | 25 | 44 |
| College graduate | 54 | 42 |
| Weight status†‡ | ||
| Normal weight (BMI 18.5–24.9 kg/m2) | 39 | 25 |
| Overweight (BMI 25.0–29.9 kg/m2) | 33 | 46 |
| Obese (BMI 30.0+kg/m2) | 27 | 53 |
| Perceive weight as health risk† | ||
| Yes | 36 | 60 |
| No | 64 | 28 |
| MD discussed weight as health risk† | ||
| Yes | 24 | 53 |
| No | 76 | 36 |
| Health status | ||
| Very good to excellent | 51 | 40 |
| Good | 32 | 42 |
| Fair to poor | 16 | 38 |
| Obesity-related conditions§ | ||
| Yes | 64 | 37 |
| No | 36 | 45 |
| Vigorous exercise | ||
| At least 1,000 Kcal/week† | ||
| Yes | 25 | 47 |
| No | 75 | 35 |
| Diet | ||
| Control portions all/most of the time† | ||
| Yes | 32 | 48 |
| No | 68 | 33 |
| Limit fat all/most of the time† | ||
| Yes | 37 | 45 |
| No | 63 | 31 |
| Five or more servings of fruits and vegetables per day | ||
| Yes | 34 | 36 |
| No | 66 | 39 |
| Smoker† | ||
| Current | 13 | 27 |
| Former | 34 | 37 |
| Never | 52 | 46 |
Column presents percentage of adults within each category of a characteristic who are at the preparation, action, and maintenance stages to lose weight, improve diet, and increase exercise.
P<.05 for comparisons of those at preparation/action/maintenance stages versus precontemplative/contemplative stages across the categories for each characteristic.
There were no underweight respondents; percents of our overall sample do not add to 100% because of rounding.
Obesity-related conditions include self-reported coronary artery disease, hypertension, asthma, obstructive sleep apnea, hypercholesterolemia, and gastroesophageal reflux disease.
BMI, body mass index.
We used SAS version 8.12 (SAS Institute, Cary, NC) to conduct all analyses. We considered P values<.05 statistically significant.
RESULTS
Sample Characteristics and Weight Control Behavior
Table 1 displays characteristics of the 365 patients in our study, who were cared for by 95 physicians. Their mean age was 49 years. In addition, 36% of respondents believed that their weight was a health risk including 8% of normal weight, 34% of overweight, and 79% of obese patients.
Figure 2 shows the distribution of patients at various stages of change for several health behaviors. Over half of all patients were in the preparation, action, or maintenance stages for all behaviors examined; the proportion was significantly higher among overweight and obese patients than among normal weight patients. Of 199 respondents at the preparation, action, or maintenance stage for weight loss, 61% were also at an advanced stage of readiness to improve diet and exercise; they represented 38% of all patients surveyed. Among overweight and obese patients (n=220), 72% were at advanced stages for weight loss and 47% were also at these stages for improving diet and exercise.
FIGURE 2.
Stage of readiness distribution for weight-related behaviors among primary care patients. (A) All patients. (B) Normal weight patients only. (C) Overweight and obese patients only.
The majority of patients who were at an advanced stage to lose weight were also at the preparation, action, or maintenance stages of improving diet and exercise (Table 2). However, 35% of all patients in our study (127 out of 362) were at advanced stages to improve diet and 26% (95 out of 363) were at advanced stages to increase planned exercise but were at the precontemplative or contemplative stages for losing weight; among overweight and obese patients, 13% were at advanced stages for dietary change and 20% were at advanced stages for planned exercise but were precontemplative or contemplative for weight loss.
Table 2.
Relationship Between Stage of Readiness to Lose Weight and Stage of Readiness to Engage in Weight-related Behaviors*
| Number of Patients at Advanced Stages to Lose Weight | ||
|---|---|---|
| Yes (%) | No (%) | |
| All patients (n=362) | ||
| Advanced stages for exercise | ||
| Yes | 144 (72) | 95 (58) |
| No | 55 (28) | 68 (42) |
| Advanced stages for dietary change | ||
| Yes | 190(95) | 127(78) |
| No | 9(5) | 35(22) |
| Advanced stages for exercise and dietary change | ||
| Yes | 138(69) | 81(50) |
| No | 61 (31) | 81 (50) |
| Overweight and obese patients (n=220) | ||
| Advanced stages for exercise | ||
| Yes | 108(69) | 28(44) |
| No | 49(31) | 35(56) |
| Advanced stages for dietary change | ||
| Yes | 151(96) | 45(71) |
| No | 6(4) | 18(29) |
| Advanced stages for exercise and dietary change | ||
| Yes | 104(66) | 32(58) |
| No | 53(34) | 26(42) |
Advanced stage was defined as being in the preparation, action, or maintenance stage for each behavior. Percentages are relative to column totals for each behavior. P<.001 (global χ2) for all associations between stage of readiness to change behaviors and stage of readiness to lose weight.
Factors Associated with Advanced Stage of Behavior Change
Table 1 also shows the unadjusted relationship between baseline factors and being at an advanced stage of readiness to concurrently lose weight, and improve diet and exercise. After adjusting for age, gender, education, health status, BMI, obesity-related conditions, physical functioning, and physician advice to lose weight, however, only perception of weight as a health risk was significantly associated with being at an advanced stage of change (adjusted odds ratio [AOR], 5.6; 95% CI, 2.5 to 12.5). Race and smoking were not associated with the outcome nor were they confounders. Results were similar when we restricted adjusted analyses to overweight and obese respondents.
Education, BMI, self-reported health, and receiving physician advice that their weight was a health risk were all significantly associated with perception of weight as a health risk among overweight and obese patients prior to adjustment. After adjustment for race, however, the only 2 factors significantly associated with perception of weight as a health risk were physician advice about weight as a health risk (AOR, 6.7; 95% CI, 3.0 to 15.1) and BMI (AOR, 1.2; 95% CI, 1.1 to 1.3; for each unit increment in BMI). Other factors were neither independent correlates nor confounders.
DISCUSSION
We found that nearly half of all patients and three quarters of overweight and obese patients seen at a primary care practice were in the preparation, action, or maintenance stages for weight loss. Moreover, almost half of overweight and obese patients were concurrently at one of these advanced stages for weight loss and improving diet and exercise. Awareness of their weight as a health risk was the only factor associated with being at an advanced stage for weight loss and improving diet and exercise concurrently. Furthermore, physician advice about weight as a health risk was strongly associated with patients' awareness of this health risk. While the majority of obese patients had this insight, only one third of overweight patients perceived their weight as a potential health risk. Taken together, these findings suggest that physicians should advise all overweight and obese patients about weight as a health risk and provide counseling about ways to improve diet, exercise, and weight management.
The Transtheoretical Stages of Behavior Change Model has been shown to predict behavior modification such as smoking cessation16–18 and, to a lesser degree, predict weight-related behaviors.19,20 Because patients at the 2 earlier stages10 are ambivalent about behavior change, they are unlikely to benefit from counseling about specific strategies to effect change. In the preparation stage, individuals plan to initiate action in the near future. Patients in the action stage are already changing their behavior, while patients in the maintenance stage are trying to maintain their new behavior. For behaviors such as smoking cessation where the desired behavior is well-defined, the distinction between action and maintenance is clear and the effort put forth by patients in the maintenance stage is modest relative to those in the action stage. For this reason, Prochaska suggested that patients in the preparation and action stages of change are most appropriate for action-oriented interventions.10 However, for behaviors such as weight control, diet, and physical activity, the targeted optimum behavior lies on a continuum and the risk of relapse is high, even after 6 months21; consequently, the distinction between action and maintenance stages becomes blurred. Patients in the maintenance stage may need to expend more effort than those in the action stage, and studies suggest that maintenance of desired outcomes such as sustained weight loss requires continued intervention and treatment.3 For these reasons, patients at the preparation, action, and maintenance stages are similarly likely to benefit from detailed advice on goal setting and on strategies to initiate or maintain behavior change.
Because of the ambiguity of constructs such as “eating a low-fat diet” or “increasing physical activities,” assessing stage of change for weight loss and related behaviors has presented methodological and conceptual challenges.12,22 Most studies develop and use different algorithms and items making results difficult to compare across studies. Earlier studies found different stage of change distributions for weight loss, diet, and exercise than our study. A mailed survey of HMO patients in 1991 found only 18% to 24% of respondents at the preparation and action stages for these behaviors while 31% to 50% were at maintenance stages.23 A 1994 telephone survey of U.S. adults found similar distributions.23 Neither survey presented BMI or weight data, making it difficult to speculate whether these differences were due to the different questions used, body weight of the populations, or secular trends.
Instead of trying to stage patients based on global constructs of diet and activity, Logue suggests staging participants based on behaviors reflecting effort, such as reducing portion size, increasing fruits and vegetables, and increasing planned exercise.9 Logue's survey of 284 obese patients from a primary care practice demonstrated that 80% of patients were at the preparation, action, or maintenance stages for planned exercise, portion control, and reduced fat. In contrast to our findings in overweight and obese patients, however, patients in Logue's study were primarily in the preparation stages of change (43% to 51%); fewer patients (22% to 24%) were in the action stages. Logue's use of a convenience sample, in-person administration of the survey, and inclusion of only obese patients may explain the differences between the two studies.
In our study, we tried to identify a smaller group of patients who were at an advanced stage for weight loss and also for improving diet and exercise. However, contrary to our hypothesis, a very high proportion of patients who were in the preparation, action, or maintenance stage for weight loss were also at one of these stages for improving diet and exercise. As with previous studies, our results are likely overestimates because patients tend to be optimistic about their behavior and intentions. Nevertheless, while imperfect, self-report is the only means of capturing patients' stage of behavior change. Despite the high prevalence of patients at advanced stages of change, using stage of change for weight loss as an initial screener for readiness to improve diet and exercise would have resulted in missed opportunities to intervene on a sizable minority of patients who were not ready to lose weight but were otherwise potentially motivated to improve diet and exercise.
The high prevalence of patients at an advanced stage for weight loss and improving diet and exercise does suggest important opportunities for primary care clinicians to assist patients in controlling weight. Recent clinical trials such as the Diabetes Primary Prevention Program suggest that even modest weight loss achieved through behavioral approaches can have substantial health implications in a relatively short period of time.3 In that study, risk of developing diabetes was reduced by 58% in high-risk patients over a 3-year period. Whether similarly intensive behavioral approaches can be adapted in primary care settings warrants study.
We also found that patients' perception of weight as a health risk was the only factor significantly associated with being at an advanced stage for weight control, and improving diet and exercise at the same time. This perception was strongly associated with physician's past advice that weight was a health risk, but not with patient's having weight-related conditions. Hence, clinicians can play an important role in motivating patients by helping shape patients' perception of weight-related health risk. While our findings are cross-sectional, other studies suggest patients are likely to advance in stage of behavior change after receiving physician counseling.24
Our study has important limitations. Our study was conducted at one primary care practice and results may not be generalizeable. All data were self-reported and results related to diet, physical activity, weight, and stage of change may be overly optimistic. We were also not able to use validated instruments to assess dietary behaviors. Finally, our modest sample size may have been underpowered to detect all factors important to stage of change.
In summary, our study suggests that over half of all primary care patients appear to be at the preparation, action, and maintenance stages of readiness for weight loss. A large majority of this subset is also at an advanced stage for improving diet and exercise. Having the perception that their weight is a health risk appears to be the most important factor associated with being at advanced stages of change. Future studies should examine whether primary care–based behavioral interventions and targeted physician counseling are effective in controlling weight and improving weight-related health behaviors.
Acknowledgments
Dr. Wee and this study are supported by a grant from the National Institute of Diabetes, Digestive, and Kidney Diseases (K23 DK02962) and a pilot and feasibility grant from the Boston Obesity and Nutrition Research Center (P30 DK46200). Dr. Phillips is supported by a Mid-Career Investigator Award from the National Institutes of Health (K24 AT00589).
The authors thank Ashley Bourland for administrative support and assistance with manuscript preparation, and Irene Zuffante and Mary Michaels for conducting the telephone interviews.
REFERENCES
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 3.Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: A randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279:839–46. doi: 10.1001/jama.279.11.839. [DOI] [PubMed] [Google Scholar]
- 5.Blumenthal JA, Sherwood A, Gullette EC, et al. Exercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioning. Arch Intern Med. 2000;160:1947–58. doi: 10.1001/archinte.160.13.1947. [DOI] [PubMed] [Google Scholar]
- 6.Serdula MK, Mokdad AH, Williamson DF, Galuska DA, Mendlein JM, Heath GW. Prevalence of attempting weight loss and strategies for controlling weight. JAMA. 1999;282:1353–1358. doi: 10.1001/jama.282.14.1353. [DOI] [PubMed] [Google Scholar]
- 7.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 282:1576–1578. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 8.Wee CC, McCarthy EP, Davis RB, Phillips RS. Physician counseling about exercise. JAMA. 1999;282:1583–1588. doi: 10.1001/jama.282.16.1583. [DOI] [PubMed] [Google Scholar]
- 9.Logue E, Sutton K, Jarjoura D, Smucker W. Obesity management in primary care: assessment of readiness to change among 284 family practice patients. J Am Board Fam Pract. 2000;13:164–171. doi: 10.3122/15572625-13-3-164. [DOI] [PubMed] [Google Scholar]
- 10.Prochaska JO. Strong and weak principles for progressing from precontemplation to action on the basis of twelve problem behaviors. Health Psychol. 1994;13:47–51. doi: 10.1037//0278-6133.13.1.47. [DOI] [PubMed] [Google Scholar]
- 11.Hill JO, Wyatt H. Outpatient management of obesity: a primary care perspective. Obes Res. 2002;10(suppl 2):124S–130S. doi: 10.1038/oby.2002.205. [DOI] [PubMed] [Google Scholar]
- 12.Sutton K, Logue E, Jarjoura D, Baughman K, Smucker W, Capers C. Assessing dietary and exercise stage of change to optimize weight loss interventions. Obes Res. 2003;11:641–652. doi: 10.1038/oby.2003.92. [DOI] [PubMed] [Google Scholar]
- 13.Botman SL, Moore TF, Moriarty CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995–2004. National Center for Health Statistics. Vital Health Stat. 2000;2(130) [PubMed] [Google Scholar]
- 14.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-city Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Kosinski M, Dewey JE. How to Score Version 2 of the SF-36® Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- 16.Dino G, Kamal K, Horn K, Kalsekar I, Fernandes A. Stage of change and smoking cessation outcomes among adolescents. Addict Behav. 2004;29:935–40. doi: 10.1016/j.addbeh.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Riemsma RP, Pattenden J, Bridle C, et al. Systematic review of the effectiveness of stage based interventions to promote smoking cessation. BMJ. 2003;326:1175–7. doi: 10.1136/bmj.326.7400.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lando H, Hennrikus D, McCarty M, Vessey J. Predictors of quitting in hospitalized smokers. Nicotine Tob Res. 2003;5:215–22. doi: 10.1080/0955300031000083436. [DOI] [PubMed] [Google Scholar]
- 19.Kristal AR, Glanz K, Tilley BC, Li S. Mediating factors in dietary change: understanding the impact of a worksite nutrition intervention. Health Educ Behav. 2000;27:112–25. doi: 10.1177/109019810002700110. [DOI] [PubMed] [Google Scholar]
- 20.van Sluijs EM, van Poppel MN, van Mechelen W. Stage-based lifestyle interventions in primary care: are they effective? Am J Prev Med. 2004;26:330–43. doi: 10.1016/j.amepre.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 21.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74:579–84. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 22.Povey R, Conner M, Sparks P, James R, Shepherd R. Interpretations of healthy and unhealthy eating, and implications for dietary change. Health Educ Res. 1998;13:171–83. doi: 10.1093/her/13.2.171. [DOI] [PubMed] [Google Scholar]
- 23.Laforge RG, Velicer WF, Richmond RL, Owen N. Stage distributions for five health behaviors in the United States and Australia. Prev Med. 1999;28:61–74. doi: 10.1006/pmed.1998.0384. [DOI] [PubMed] [Google Scholar]
- 24.Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med. 1996;25:225–33. doi: 10.1006/pmed.1996.0050. [DOI] [PubMed] [Google Scholar]