Abstract
OBJECTIVE
To assess the perceived preparedness of residents in adult primary care specialties to counsel patients about preventive care and psychosocial issues.
DESIGN
Cross-sectional national mail survey of residents (63% response rate).
PARTICIPANTS
Nine hundred twenty-eight final-year primary care residents in Internal Medicine (IM), family practice (FP), and Obstetrics/Gynecology (OB/GYN) at 162 U.S. academic health centers.
MEASUREMENTS
Residents self-rated preparedness to counsel patients about smoking, diet and exercise, substance abuse, domestic violence, and depression.
RESULTS
Residents felt better prepared to counsel about smoking (62%) and diet and exercise (53%) than about depression (37%), substance abuse (36%), or domestic violence (21%). In most areas, females felt better prepared than males. Rates of counseling preparedness varied significantly by specialty after adjustment for gender, race, medical school location, and percent of training spent in ambulatory settings. FP residents felt better prepared than OB/GYN residents to counsel about smoking, diet and exercise, and depression, while OB/GYN residents felt better prepared to address domestic violence than IM or FP residents. IM residents' perceptions of preparedness were between the other 2 specialties. Proportion of training spent in ambulatory settings was not associated with residents' perceived preparedness.
CONCLUSIONS
Physicians completing residencies in adult primary care did not feel very well prepared to counsel patients about preventive and psychosocial issues. Significant differences exist among specialties, even after adjusting for differences in time spent in ambulatory settings. Increasing residency time in ambulatory settings may not alone be sufficient to ensure that residents emerge with adequate counseling skills.
Keywords: primary care, medical education, prevention, patient-doctor communication
Physicians have a key role to play in helping to achieve national health goals as outlined in Healthy People 2010.1 For 2010, the Healthy People goals call for increasing to 85% the proportion of physicians who counsel their patients about smoking and physical activity and increasing overall the percentage of patients who get counseled about health behaviors (e.g., nutrition and alcohol use). Healthy People goals also include reducing the harm due to domestic violence and increasing the identification and treatment of adults with depression. Although the majority of physicians endorse their role in educating patients about preventive care,2 primary care physicians often fail to use their opportunity to counsel patients about smoking,3–8 substance use,9–13 and nutrition and physical activity.14–18 Primary care physicians also do not routinely screen or counsel for depression19–22 or domestic violence.23–25
One strategy for addressing these deficits is to ensure that medical training prepares all new physicians entering practice to address these issues. The ability to provide comprehensive preventive and psychosocial care was included in a landmark compilation of requisite residency training components published in 1994.26 Current program requirements for residencies in the 3 specialties that train physicians to deliver adult primary care include nearly all of the training components recommended in the 1994 document.27–30 The Accreditation Council on Graduate Medical Education's (ACGME) required curriculum for family practice training targets training in human behavior and mental health, and Obstetrics/Gynecology and Internal Medicine also include targeted training in preventive care and psychosocial issues.28–30 ACGME training programs' requirements also set minimum standards for training in outpatient settings as a way to achieve these goals. The required curriculum for family practice emphasizes training in outpatient settings.28 Internal Medicine residents must spend at least one third of their training, and Obstetrics/Gynecology residents must spend at least 10% of their training in ambulatory care settings.29,30
Despite the ACGME primary care training standards in preventive care and counseling, deficits continue to be seen in physicians' counseling behaviors. In 1998, a national survey of residents in their final year of training assessed residents' perceptions of their preparedness to provide a wide array of common clinical services,31 and residents rated themselves as prepared to manage most common clinical conditions. This paper focuses on residents' perceived preparedness to counsel patients about preventive and psychosocial issues and explores the variability in residents' perceptions among the 3 specialties that provide adult primary care (Internal Medicine, family practice, and Obstetrics and Gynecology). We hypothesized that family practice residents, compared to Internal Medicine and Obstetrics/Gynecology residents, would feel better prepared to counsel for preventive health and psychosocial issues because family practice programs have historically emphasized ambulatory care, and training in an ambulatory environment is believed to promote skills in primary and preventive care. We also hypothesized that, regardless of specialty, residents who spent a greater proportion of their training in ambulatory care settings would feel better prepared to address preventive and psychosocial care. Finally, we hypothesized that female residents would feel better prepared to counsel their patients than male residents, because previous work demonstrates that female physicians are more likely to counsel patients about behavioral and mental health issues.32–35
METHODS
Sample Selection
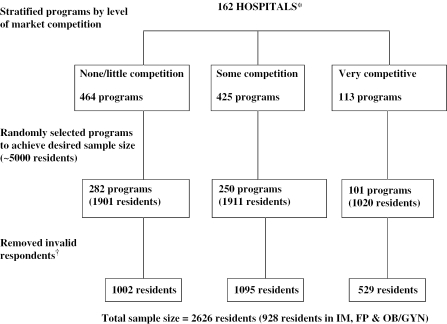
The sampling and survey methods for this study have been described in previous publications.31 The study population was a stratified sample of residents from 8 specialties (anesthesiology, psychiatry, Obstetrics/Gynecology, pediatrics, general surgery, orthopedic surgery, family practice, Internal Medicine) who were in their final year of residency. The sample was obtained by a 3-step process: selection of hospitals, residency programs, and residents (see Fig. 1). The 162 hospitals were selected by combining 1) a list of integrated academic medical center hospitals from the Association of American Medical Colleges; 2) a list of the major teaching hospitals that were most closely affiliated with U.S. medical schools; and 3) a list of the 100 hospitals with the largest numbers of residents based on Medicare cost reports. The final list of academic health centers included 162 U.S. hospitals that had trained 40,000 of the 98,000 residents in 1998.36
FIGURE 1.
Survey data collection diagram. *Hospitals were selected if they were one of the following: 1) an academic health center with a medical school affiliation, 2) a major teaching hospital affiliated with a medical school, or 3) among the 100 hospitals with the largest number of residents. All programs (anesthesiology, psychiatry, Obstetrics/Gynecology, pediatrics, general surgery, orthopedic surgery, family practice, Internal Medicine) at selected hospitals were included. †Invalid (e.g., not in final year of residency, incorrect information).
In each hospital, all training programs in the 8 selected specialties were identified using the American Medical Associates Graduate Medical Education database. Additionally, hospitals were stratified by competitiveness of market using the University Health System Consortium's market evolution model (1/2=none or little competition, 3=some competition, 4=very competitive). Finally, for each specialty, programs were randomly selected within each market stage, and all residents from the selected programs were chosen until we met the quota for that stage.
Although this survey was given to 8 different specialties, the focus of this paper is on the 928 residents who provided adult primary care. This included 279 Internal Medicine (IM) residents in 25 programs, 326 family practice (FP) residents in 75 programs, and 323 Obstetrics/Gynecology (OB/GYN) residents in 114 programs. The overall adjusted response rate for primary care residents was 63% (n=928; 59% IM, 68% FP, and 63% OB/GYN).
Survey Design and Administration
Based on focus groups, a literature review, a review of the ACGME policies, and expert opinions, a survey was developed and pilot tested. The survey took approximately 15 minutes to complete. The protocol was approved by the Massachusetts General Hospital Institutional Review Board. The survey was administered by Datastat, Inc. (Ann Arbor, MI). Surveys were administered in the spring of 1998.
Residents received advance notification about the survey and multiple survey mailings. To enhance survey completion, strategies included telephone follow-up, flexible scheduling, cash prizes, and payments. Telephone administration of the surveys was conducted for individuals who had not completed the mailed survey.
Measures
The outcome measure was perceived preparedness to counsel patients about preventive care and psychosocial issues. Residents were asked to “rate the extent to which you feel prepared to counsel patients about…“ smoking, diet and exercise, substance abuse, depression, and domestic violence, using a 4-point scale ranging from very unprepared to very prepared. Because final-year residents are expected to be very prepared to counsel patients in these areas, the 5 outcome measures were dichotomized for analysis into 2 categories: very prepared or not very prepared (very unprepared, somewhat unprepared, somewhat prepared).
Background information collected included gender, race/ethnicity (white non-Hispanic, black non-Hispanic, Hispanic, Asian, or Alaska Native/American Indian), medical school location (U.S. medical school graduate vs international medical school graduate), and medical specialty (FP, IM, OB/GYN). Residents were also asked to report the percentage of training time they had spent in ambulatory settings. For analysis, racial and ethnic variables were collapsed into white non-Hispanic, Asian, and underrepresented minorities.
Data Analysis
Analyses were conducted using SUDAAN software (version 7.5.1, specialized software which controls for clustering and complex sample design; Research Triangle Institute, Research Triangle Park, NC) and SAS software (version 8.2; SAS Institute, Cary, NC). Analyses were weighted to adjust for differences in sampling and response rates within each stratum (specialty/market stage/program). Bivariate analyses compared the outcome variable, preparedness to counsel, by each background variable, using the χ2 test to assess statistical significance. Multivariate analyses were adjusted to account for the multistage sampling design. Logistic regression models were constructed to examine the relationship between each preventive counseling behavior and each specialty, adjusting for the effects of gender, race/ethnicity, medical school location (United States vs international), and percentage of residency training time spent in ambulatory settings (continuous variable); variables were selected on an a priori basis.
RESULTS
Sample Characteristics
The respondents included 928 residents in Internal Medicine (N=279), family practice (N=326), and Obstetrics/Gynecology (N=323). The characteristics of the sample are displayed in Table 1. Fifty-nine percent were male. Sixty-one percent of residents were white and 29% Asian. Sixty-nine percent of residents had completed medical school training in the United States. Family practice residents spent approximately half of their time in ambulatory settings; Internal Medicine residents spent 27% and Obstetrics/Gynecology residents spent 22% of their time in ambulatory settings. The 3 primary care specialties differed significantly in respondents' gender, race/ethnicity, likelihood of having graduated from a U.S. medical school, and proportion of residency training time spent in an ambulatory setting.
Table 1.
Characteristics of Respondents by Specialty
| Characteristic | All Adult-care Residents | Internal Medicine Residents | Family Practice Residents | Obstetrics/Gynecology Residents | P Value* | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | Wgt % | N | Wgt % | N | Wgt % | N | Wgt % | ||
| Total | 928 | 279 | 326 | 323 | |||||
| Personal characteristics | |||||||||
| Gender | |||||||||
| Male | 473 | 59 | 176 | 64 | 173 | 54 | 124 | 38 | |
| Female | 454 | 41 | 103 | 36 | 153 | 46 | 198 | 62 | <.001 |
| Race/ethnicity | |||||||||
| White | 629 | 61 | 156 | 55 | 234 | 71 | 239 | 75 | |
| Asian | 178 | 29 | 94 | 36 | 46 | 15 | 38 | 12 | |
| URM | 109 | 10 | 22 | 8 | 45 | 14 | 42 | 13 | .001 |
| Training characteristics | |||||||||
| Graduate of U.S. medical school | |||||||||
| Yes | 747 | 69 | 185 | 61 | 258 | 78 | 304 | 94 | |
| No | 181 | 31 | 94 | 39 | 68 | 22 | 19 | 6 | <.001 |
| Mean percentage of training time based in the ambulatory setting | 27 | 48 | 22 | ||||||
| Training time in ambulatory setting, % | |||||||||
| 0 | 15 | 15 | 30 | ||||||
| 1–25 | 72 | 44 | 58 | ||||||
| 26+ | 13 | 41 | 12 | ||||||
N=number of respondents. Data are missing for gender (n=1) and race/ethnicity (n=12).
Wgt %=sample size–adjusted percentage reflecting relative population and response bias.
P value fromχ2analysis comparing Internal Medicine residents, family practice residents, and Obstetrics/Gynecology residents.
URM, underrepresented minorities (e.g., African Americans, Hispanics, Native Americans, Aleutian Natives).
Preventive Counseling by Specialty
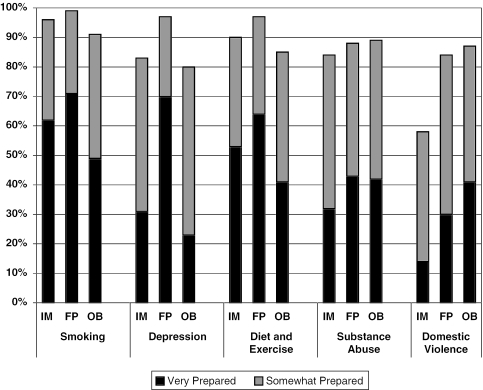
Residents' perceived preparedness to counsel varied by the 5 preventive counseling behaviors. Residents felt best prepared to counsel about smoking (62%) and diet and exercise (53%) and less well prepared to counsel about depression (37%), substance abuse (36%), and domestic violence (21%). Figure 2 displays residents' perceived preparedness to deliver preventive counseling by specialty.
FIGURE 2.
Percent of adult primary residents who are “very prepared” and “somewhat prepared” to deliver preventive counseling by specialty.
Predictors of Preventive Counseling
Table 2 shows the relationship between each counseling behavior and each specialty, after adjustment for gender, race/ethnicity, training location, and percentage of training time spent in hospital or community-based ambulatory settings. Female residents felt better prepared than male residents to counsel about all topics except smoking, for which both males and females felt well prepared. Residents' race/ethnicity affected only their perceived preparedness to counsel about depression; Asians felt significantly less prepared to counsel about depression than whites or underrepresented minorities.
Table 2.
Multivariate Analyses for Counseling Outcomes: % Reporting “Very Prepared” to Counsel
| Characteristic | Smoking | Diet and Exercise | Depression | Substance Abuse | Domestic Violence | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | OR (CI) | % | OR (CI) | % | OR(CI) | % | OR (CI) | % | OR (CI) | |
| Total | 62 | 53 | 37 | 36 | 21 | |||||
| Personal characteristics | ||||||||||
| Gender | ||||||||||
| Male | 59 | – | 47 | – | 31 | – | 30 | – | 15 | – |
| Female | 66 | 1.4 (0.9 to 2.3) | 62 | 2.0 (1.4 to 2.9) | 46 | 2.1 (1.4 to 3.1) | 43 | 1.8 (1.2 to 2.6) | 29 | 2.1 (1.5 to 2.9) |
| Race/ethnicity | ||||||||||
| White | 63 | – | 51 | – | 42 | – | 38 | – | 21 | – |
| Asian | 60 | 1.0 (0.7 to 1.5) | 57 | 1.1 (0.8 to 1.6) | 22 | 0.4 (0.2 to 0.6) | 29 | 0.7 (0.4 to 1.1) | 22 | 1.0 (0.6 to 1.8) |
| URM | 62 | 1.1 (0.6 to 2.1) | 52 | 1.0 (0.5 to 1.8) | 51 | 1.4 (0.6 to 3.4) | 45 | 1.3 (0.7 to 2.5) | 27 | 1.2 (0.5 to 3.0) |
| Training characteristics | ||||||||||
| Graduate of U.S. medical school | ||||||||||
| Yes | 65 | – | 51 | – | 41 | – | 37 | – | 19 | – |
| No | 55 | 0.6 (0.4 to 1.0) | 57 | 1.3 (0.8 to 2.2) | 29 | 0.8 (0.5 to 1.3) | 32 | 1.0 (0.7 to 1.5) | 25 | 2.4 (1.4 to 4.2) |
| Specialty | ||||||||||
| Internal medicine | 62 | 0.8 (0.5 to 1.4) | 53 | 0.6 (0.4 to 1.1) | 31 | 0.3 (0.2 to 0.5) | 32 | 0.6 (0.3 to 1.2) | 14 | 0.5 (0.3 to 0.9) |
| Family practice | 71 | – | 64 | – | 70 | – | 43 | – | 30 | – |
| Obstetrics/gynecology | 49 | 0.4 (0.2 to 0.7) | 41 | 0.4 (0.2 to 0.6) | 23 | 0.1 (0.1 to 0.3) | 42 | 0.8 (0.5 to 1.4) | 41 | 2.2 (1.2 to 4.0) |
| Mean percentage of training time based in an ambulatory setting | 30 | 1.2 (0.3 to 4.9) | 31 | 1.7 (0.5 to 5.9) | 35 | 4.8 (1.4 to 16.8) | 30 | 0.9 (0.3 to 2.9) | 32 | 2.1 (0.3 to 14.4) |
%=sample size–adjusted percentage reflecting relative population and response bias.
URM, underrepresented minorities (e.g., African Americans, Hispanics, Native Americans, Aleutian Natives).
There was little difference between U.S. and foreign-trained medical school graduates; foreign medical school graduates felt better prepared to counsel about domestic violence but less well prepared to counsel about depression than graduates of U.S. medical schools. Internal Medicine and Obstetrics/Gynecology residents were less likely than family practice residents to feel well prepared to counsel about depression. Obstetrics/Gynecology residents also felt less prepared than family practice residents to counsel about smoking and diet and exercise, but they felt more prepared to counsel about domestic violence than family practice or Internal Medicine residents. There were no statistically significant differences by specialty in preparedness to counsel for substance abuse. The percentage of training that occurred in an ambulatory or community setting was not associated with greater perceived preparedness to counsel, with the exception of counseling about depression.
DISCUSSION
Using a national survey, we examined final-year residents' perceived preparedness to counsel about preventive and psychosocial issues. Ideally, all final-year residents in the specialties that provide adult primary care should feel well prepared to address these topics, but this was not the case. Less than half of respondents felt well prepared to counsel patients about depression, substance abuse, and domestic violence, and less than two thirds felt well prepared to counsel about tobacco use or diet and exercise. It appears that the next generation of physicians may not be well prepared to address these priority national health promotion issues.
Residents' perceived preparedness to counsel about preventive behaviors and psychosocial issues varied by specialty, even after adjustment for other differences among specialties. As hypothesized, family practice residents felt better prepared than Obstetrics/Gynecology residents to address smoking, depression, and diet and exercise, but the reverse was true for counseling about domestic violence. No differences were seen by specialty in preparedness to counsel about substance abuse. Internal Medicine residents generally felt less prepared than family practice residents, but the differences were statistically significant only for depression and domestic violence counseling.
Our finding that Obstetrics/Gynecology residents felt best prepared to counsel about domestic violence echoes previous studies demonstrating that Obstetrics/Gynecology providers, compared to family practitioners and Internists, report a higher level of domestic violence screening.24,37 So, although ACGME guidelines for family practice and Internal Medicine also require instruction in the recognition and management of domestic violence, our findings suggest that Obstetrics/Gynecology programs place greater emphasis on domestic violence training than the other primary care programs. In addition, it is likely that Obstetrics/Gynecology residents have more opportunity to practice domestic violence counseling because all of their patients are female. The low rates of Internal Medicine and family practice residents' perceived preparedness to address domestic violence indicate a need for residency training in these fields to improve training on this important topic.
Although the ACGME program requirements for the primary care specialties all state that instruction is required in preventive and psychosocial counseling, there needs to be a focus on assessing and evaluating these counseling competencies. Studies have shown that physicians' self-assessment skills tend to overestimate their actual skill level.38 Although residents are more accurate at self-assessment than practicing physicians, residents also report that their activity and skill levels are higher than they actually are. Therefore, it is likely that the residents' self-perceived preparedness ratings in this study are overly favorable and that there is a greater deficit in preparedness than is actually reported.
Overall, residents' perceived preparedness to counsel about preventive and psychosocial issues was associated primarily with medical specialty rather than with the proportion of time a resident spent in ambulatory settings. Counter to our hypothesis, the proportion of residency time spent in an ambulatory setting was only related to perceived preparedness to counsel for depression. Increasing the amount of time spent in ambulatory settings may be necessary but is not sufficient to guarantee residents' preparedness in the areas of smoking, diet and exercise, substance abuse, and domestic violence. The implication is that not only the amount but also the content of the ambulatory training matters.
We believe that the movement toward competency-based assessment, with a focus on evaluating residents on the ACGME Outcome Project's 6 core competencies (patient care, medical knowledge, communication skills, practice-based learning and improvement, professionalism, and systems-based practice),39,40 is needed. Each residency program should evaluate whether or not its instruction in preventive and psychosocial counseling is achieving needed outcomes and also whether residents are being allocated time needed for counseling activities. Many of our findings of residents' perceived preparedness deficits are consistent with the literature on the counseling behaviors of physicians in practice.5,8,12,13,18,21,37,41–43 Variations by specialty are also consistent with the literature on practicing physicians' counseling behaviors.3,24,37,44–47 Within each specialty, the deficits in residents are similar to the deficits in practicing physicians, indicating a need to improve residency training and faculty development.
This study had several limitations. Our results are based on self-reported preparedness, and it is unknown how this subjective assessment relates to performance. However, research on physician behavior change indicates that confidence in one's ability to make a change (e.g., self-efficacy) is related to the likelihood of doing so.5,43,46 In addition, Internal Medicine training is a common pathway for both primary care internists and those who plan to specialize. Many Internal Medicine residency programs have separate tracks for those individuals who plan to go into primary care. Our survey did not differentiate between these tracks. It is possible that residents in primary care Internal Medicine feel more prepared to counsel about preventive and psychosocial issues than their specialty-bound colleagues. Finally, the generalizability of our findings is limited to residents at academic health centers in 1998; these data will be an important basis for comparison with upcoming data from the ACGME evaluation efforts.
In summary, the majority of adult primary care residents do not feel very well prepared to counsel patients about preventive care and psychosocial issues, and extent of preparedness varies by specialty. Identified strengths of family practice and Obstetrics/Gynecology programs may serve as models to direct future residency training in preventive counseling.
Acknowledgments
The authors greatly acknowledge the contributions of Eric G. Campbell, PhD. Dr. Campbell oversaw all of the data collection and advised us on the survey design for the resident academic health center survey. We also would like to thank the Massachusetts General Hospital Multicultural Affairs Office's Summer Research Trainee Program for supporting this project.
This work was supported by a grant from the Commonwealth Fund, New York City, as part of the activities of the Commonwealth Task Force on Academic Health Centers, and by a grant (K24-HL04440) from the National Heart, Lung, and Blood Institute.
References
- 1.U.S. Department of Health and Human Services. Healthy People 2010. Washington, DC: Office of Disease Prevention and Health Promotion; 2000. [Google Scholar]
- 2.Wechsler H, Levine S, Idelson RK, Schor EL, Coakley E. The physician's role in health promotion revisited—a survey of primary care practitioners. N Engl J Med. 1996;34:996–8. doi: 10.1056/NEJM199604113341519. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein MG, DePue JD, Monroe AD, et al. A population-based survey of physician smoking cessation counseling practices. Prev Med. 1998;27:720–9. doi: 10.1006/pmed.1998.0350. [DOI] [PubMed] [Google Scholar]
- 4.Gottlieb NH, Guo J, Blozis SA, Huang PP. Individual and contextual factors related to family practice residents' assessment and counseling for tobacco cessation. J Am Board Fam Pract. 2001;14:343–51. [PubMed] [Google Scholar]
- 5.Park ER, DePue JD, Goldstein MG, et al. Assessing the transtheoretical model of change constructs for physicians counseling smokers. Ann Behav Med. 2003;25:120–6. doi: 10.1207/S15324796ABM2502_08. [DOI] [PubMed] [Google Scholar]
- 6.Pollack KI, Arredondo EM, Yarnall KSH, et al. How do residents prioritize smoking cessation for young “high-risk“ women? Factors associated with addressing smoking cessation. Prev Med. 2001;33:292–9. doi: 10.1006/pmed.2001.0884. [DOI] [PubMed] [Google Scholar]
- 7.Moran S, Thorndike AN, Armstrong K, Rigotti NA. Physicians' missed opportunities to address tobacco use during prenatal care. Nicotine Tob Res. 2003;5:363–8. doi: 10.1080/1462220031000094150. [DOI] [PubMed] [Google Scholar]
- 8.Thorndike AN, Rigotti NA, Stafford RS, Singer DE. National patterns in the treatment of smokers by physicians. JAMA. 1998;279:604–8. doi: 10.1001/jama.279.8.604. [DOI] [PubMed] [Google Scholar]
- 9.Arndt S, Schultz SK, Turvey C, Petersen A. Screening for alcoholism in the primary care setting: are we talking to the right people? J Fam Pract. 2002;51:41–6. [PubMed] [Google Scholar]
- 10.Buchsbaum DG, Buchanan RG, Poses RM, Schnoll SH, Lawton MJ. Physician detection of drinking problems in patients attending a general medicine practice. J Gen Intern Med. 1992;7:517–21. doi: 10.1007/BF02599456. [DOI] [PubMed] [Google Scholar]
- 11.Fleming MF. Strategies to increase alcohol screening in health care settings. Alcohol Health Res World. 1997;21:340–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Friedmann PD, McCullough D, Chin MH, Saitz R. Screening and intervention for alcohol problems. A national survey of primary care physicians and psychiatrists. J Gen Intern Med. 2000;15:84–91. doi: 10.1046/j.1525-1497.2000.03379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spandorfer JM, Yedy I, Turner BJ. Primary care physicians' views on screening and management of alcohol abuse: inconsistencies with national guidelines. J Fam Pract. 1999;48:899–902. [PubMed] [Google Scholar]
- 14.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 15.Glasgow RE, Eakin EG, Fisher EB, Bacak SJ, Brownson RC. Physician advice and support for physical activity: results from a national survey. Am J Prev Med. 2001;21:189–96. doi: 10.1016/s0749-3797(01)00350-6. [DOI] [PubMed] [Google Scholar]
- 16.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24:546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 17.Nawaz H, Adams ML, Katz DL. Weight loss counseling by health care providers. Am J Public Health. 1999;89:764–7. doi: 10.2105/ajph.89.5.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stafford RS, Farhat JK, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9:631–8. doi: 10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 19.Coyne JC, Schwenk TL, Fechner-Bates S. Nondetection of depression by primary care physicians reconsidered. Gen Hosp Psychiatry. 1995;17:3–12. doi: 10.1016/0163-8343(94)00056-j. [DOI] [PubMed] [Google Scholar]
- 20.Docherty JP. Barriers to the diagnosis of depression in primary care. J Clin Psychiatry. 1997;58:5–10. [PubMed] [Google Scholar]
- 21.Penn JV, Boland R, McCartney JR, Kohn R, Mulvey T. Recognition and treatment of depressive disorders by Internal Medicine attendings and housestaff. Gen Hosp Psychiatry. 1997;19:179–84. doi: 10.1016/s0163-8343(97)00005-4. [DOI] [PubMed] [Google Scholar]
- 22.Simon GE, Von Korff M. Recognition, treatment, management and outcomes of depression in primary care. Arch Fam Med. 1995;4:99–105. doi: 10.1001/archfami.4.2.99. [DOI] [PubMed] [Google Scholar]
- 23.Caralis PV, Musialowski R. Women's experiences with domestic violence and their attitudes and expectations regarding medical care of abuse victims. South Med J. 1997;90:1075–80. doi: 10.1097/00007611-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Elliott L, Nerney M, Jones T, Friedmann PD. Barriers to screening for domestic violence. J Gen Intern Med. 2002;17:112–6. doi: 10.1046/j.1525-1497.2002.10233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamberger LK, Saunders DG, Hovey M. Prevalence of domestic violence in community practice and rate of physician inquiry. Fam Med. 1992;24:283–7. [PubMed] [Google Scholar]
- 26.Rivo ML, Saultz JW, Wartman SA, DeWitt TG. Defining the generalist physician's training. JAMA. 1994;271:1499–504. [PubMed] [Google Scholar]
- 27.Seltzer VL, Fishburne JI, Jonas HS. Obstetrics and gynecology residencies: education in preventive and primary health care for women. Obstet Gynecol. 1998;91:305–10. doi: 10.1016/s0029-7844(97)00628-5. [DOI] [PubMed] [Google Scholar]
- 28.Accreditation Council on Graduate Medical Education. Residency review committee. Program requirements for residency education in family practice. Available at: http://www.acgme.org. Accessed July 2001.
- 29.Accreditation Council on Graduate Medical Education. Residency review committee. Program requirements for residency education in internal medicine. Available at: http://www.acgme.org. Accessed July 2001.
- 30.Accreditation Council on Graduate Medical Education. Residency review committee. Program requirements for residency education in obstetrics/gynecology. Available at: http://www.acgme.org. Accessed July 2001.
- 31.Blumenthal D, Gokhale M, Campbell EG, Weissman JS. Preparedness for clinical practice: reports of graduating residents academic health centers. JAMA. 2001;286:1027–34. doi: 10.1001/jama.286.9.1027. [DOI] [PubMed] [Google Scholar]
- 32.Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Med Care. 1995;33:407–16. doi: 10.1097/00005650-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Frank E, Kunovich-Frieze T. Physician's prevention counseling behaviors: current status and future directions. Prev Med. 1995;24:543–5. doi: 10.1006/pmed.1995.1086. [DOI] [PubMed] [Google Scholar]
- 34.Henderson JT, Weiss CS. Physician gender effects on preventive screening and counseling: an analysis of male and female patients' health care experiences. Med Care. 2001;39:1281–92. doi: 10.1097/00005650-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Laube DW, Ling FW. Primary care in obstetrics and gynecology resident education: a baseline survey of residents' perceptions and experiences. Obstet Gynecol. 1999;94:632–6. doi: 10.1016/s0029-7844(99)00350-6. [DOI] [PubMed] [Google Scholar]
- 36.Graduate Medical Education Database 1996–1997. Chicago, IL: American Medical Association; 1996. [Google Scholar]
- 37.Rodriguez MA, Bauer H, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse: practices and attitudes of primary care physicians. JAMA. 1999;282:468–74. doi: 10.1001/jama.282.5.468. [DOI] [PubMed] [Google Scholar]
- 38.Biernat K, Simpson D, Duthie E, Jr, Bragg D, London R. Primary care residents self assessment skills in dementia. Adv Health Sci Educ. 2003;8:105–10. doi: 10.1023/a:1024961618669. [DOI] [PubMed] [Google Scholar]
- 39.Accreditation Council on Graduate Medical Education. 2000. ACGME Outcome Project. Available at: http://www.acgme.org/outcome.
- 40.Goroll AH, Sirio C, Duffy FD, et al. A new model for accreditation of residency programs in internal medicine. Ann Intern Med. 1995;173:381–6. doi: 10.7326/0003-4819-140-11-200406010-00012. [DOI] [PubMed] [Google Scholar]
- 41.Parsons LH, Zaccaro D, Wells B, Stovall TG. Methods of and attitudes toward screening obstetrics and gynecology patients for domestic violence. Am J Obstet Gynecol. 1995;173:381–6. doi: 10.1016/0002-9378(95)90256-2. [DOI] [PubMed] [Google Scholar]
- 42.Schmidt L, Greenberg BD, Holzman GB, Schulkin J. Treatment of depression by obstetrician-gynecologists: a survey study. Obstet Gynecol. 1997;90:296–300. doi: 10.1016/S0029-7844(97)00255-X. [DOI] [PubMed] [Google Scholar]
- 43.Goldstein MG, Niaura R, Willey-Lessne C, et al. Physicians counseling smokers. A population-based survey of patients' perceptions of health care provider-delivered smoking cessation interventions. Arch Intern Med. 1997;157:1313–9. doi: 10.1001/archinte.157.12.1313. [DOI] [PubMed] [Google Scholar]
- 44.Frank E, Wright EH, Serdula MK, Elon LK, Baldwin G. Personal and professional nutrition-related practices of U.S. female physicians. Am J Clin Nutr. 2002;75:326–32. doi: 10.1093/ajcn/75.2.326. [DOI] [PubMed] [Google Scholar]
- 45.Nichols GA, Brown JB. Following depression in primary care: do family practice physicians ask about depression at different rates than internal medicine physicians? Arch Fam Med. 2000;9:478–82. doi: 10.1001/archfami.9.5.478. [DOI] [PubMed] [Google Scholar]
- 46.Sciamanna CN, DePue JD, Goldstein MG, et al. Nutrition counseling in the promoting cancer prevention in primary care study. Prev Med. 2002;35:437–46. doi: 10.1006/pmed.2002.1099. [DOI] [PubMed] [Google Scholar]
- 47.Williams JW, Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ, Cornell J. Primary care physicians' approach to depressive disorders. Arch Fam Med. 1999;8:58–67. doi: 10.1001/archfami.8.1.58. [DOI] [PubMed] [Google Scholar]