Abstract
BACKGROUND
Panic disorder (PD) and generalized anxiety disorder (GAD) are often unrecognized by primary care physicians (PCPs). The Primary Care Evaluation of Mental Disorders (PRIME-MD) has been used as a case-finding instrument for depression. Yet, little is known on its usefulness as a case-finding tool for anxiety disorders within the context of a clinical trial.
OBJECTIVE
To examine the: (1) completion rate of the PRIME-MD by patients approached to enroll in a treatment study for PD and GAD; (2) distribution of anxiety diagnoses generated; (3) severity of PD and GAD episodes thus identified; and (4) level of PCPs' agreement with these diagnoses.
DESIGN
Cross-sectional interview.
PATIENTS
Individuals aged 18 to 64 who presented for care at 4 primary care practices.
MEASUREMENTS
The PRIME-MD, Structured Interview Guide for the Hamilton Anxiety Rating Scale (SIGH-A), and the Panic Disorder Severity Scale (PDSS).
RESULTS
Of the 6,700 patients who completed the PRIME-MD Patient Questionnaire (PQ), 2,926 (44%) screened positive for an anxiety disorder, and 1,216 (42%) met preliminary study eligibility and consented to the PRIME-MD Anxiety Module. Of these, 619 (51%) had either GAD (308), PD (94), or both (217) disorders. Later, 329 completed a telephone interview. Of these, 59% with GAD and 68% with PD reported moderate or greater levels of anxiety symptoms on the SIGH-A and PDSS, respectively, and PCPs agreed with the PRIME-MD diagnosis for 98% of these patients.
CONCLUSIONS
The PRIME-MD can efficiently screen patients for PD and GAD. Although patients thus identified endorse a wide range of anxiety symptoms, PCPs often agree with the diagnosis.
Keywords: anxiety, panic, generalized anxiety disorder, primary care, electronic medical record system
Anxiety disorders are prevalent in primary care practice and generate a significant excess of morbidity, health services utilization, and health care expenditures.1–4 Approximately 12% to 22% of primary care patients present with symptoms of distress related to anxiety.5,6 Among the various anxiety disorders, panic disorder (PD; 1% to 13% prevalence7–11) and generalized anxiety disorder (GAD; 5% to 16% prevalence9,10,12) create the largest burden of illness. Nevertheless, primary care physicians (PCPs), who care for the majority of these individuals, often fail to diagnose these disorders.13–16
Several instruments have been developed to aid PCPs in recognizing the presence of an anxiety disorder.17–26 Among the more prominent of these is the Primary Care Evaluation of Mental Disorders (PRIME-MD), a 2-stage rapid screening and interview procedure that can also generate a Diagnostic and Statistical Manual Version IV (DSM-IV) diagnosis of major depression, somatoform disorders, and alcohol abuse.25 While the PRIME-MD has been used to identify depressed patients within the context of a clinical trial,27 we are unaware of any report documenting its use within the context of a clinical trial for an anxiety disorder. Also unclear is the extent and rapidity with which PCPs will agree with the finding of an anxiety disorder when presented with the PRIME-MD diagnostic formulation. Perhaps most important, no study has used well-validated rating scales to determine the severity of PD and GAD episodes identified by the PRIME-MD. We investigated these issues using data collected as part of a randomized clinical trial to examine the effectiveness of a collaborative care strategy to improve the quality of primary care for PD and GAD.28
METHODS
Study Setting
This research was conducted at 4 primary care practices administered by the University of Pittsburgh Medical Center, implementing a protocol approved by the Institutional Review Board (IRB) of the University of Pittsburgh. These practice sites included the University's main urban faculty practice staffed by board-certified Internists, and 2 suburban and 1 rural practice located 15 to 20 miles east of the Medical Center's campus staffed by non-academic family practitioners. The 4 practices share a common electronic medical record (EMR) system (EpicCare, Madison, Wis) whereby PCPs obtain instant access to their patients' medical information via computer terminals placed in each examination room. This EMR system also facilitated PCP and staff communications through an internal e-mail system.
PARTICIPANTS
Primary Care Physicians
Study investigators presented highlights of our treatment algorithm at an hour-long journal club conference and then met individually with PCPs to discuss the study. All 43 study-eligible PCPs subsequently provided informed consent to enroll.
Primary Care Patients
We used the brief self-administered patient questionnaire (PQ) portion of the PRIME-MD10 to systematically screen patients aged 18 to 64 who presented for care between July 2000 and April 2002 for the presence of an anxiety disorder on days when one of our study recruiters was present in the practice waiting room. In accordance with the classification scheme developed by Spitzer et al.,10 we considered a positive screen as an affirmative response to any 1 of the 3-item anxiety screening questions on the PQ. As part of the eligibility criteria for our clinical trial,28 we required that patients with a positive PQ screen also have: (a) no obvious dementia, psychotic illness, or unstable medical condition; (b) 2 or fewer positive responses on the PQ's CAGE alcohol screening questionnaire29; and (c) no language or other communication barrier. If so, then a research assistant asked the patient for his/her written consent to administer the more comprehensive 14-item Anxiety Module portion of the PRIME-MD to determine whether he/she met DSM-IV criteria for a current episode of PD and/or GAD.10
If the patient met diagnostic criteria for either PD or GAD, the research assistant sought to confirm that the patient: (a) was not in current treatment with a mental health professional; (b) had no history of bipolar disorder; and (c) had no plans to leave the study practice within the following year. When thus confirmed, the research assistant requested the patient's consent to undergo a telephone follow-up assessment to assess the severity of the patient's anxiety symptoms and to confirm study eligibility as described above.
Assessments
When a clinically eligible patient consented to enroll in our treatment trial, a trained researcher telephoned him/her within 1 month to assess the patient's level of anxiety severity on the 14-item Structured Interview Guide for the Hamilton Anxiety Rating Scale (SIGH-A)30 and the 7-item Panic Disorder Severity Scale (PDSS).31 We initially administered the PDSS to only patients meeting the criteria for PD on the PRIME-MD. However, within 6 months after we commenced subject recruitment, we sought and received IRB approval to modify our protocol to administer both the SIGH-A and the PDSS to all patients regardless of which anxiety disorder they experienced because the SIGH-A was insufficiently sensitive to significant elevations of panic symptoms. Those eligible to continue into our clinical trial (SIGH-A≥14 or PDSS≥7) were reimbursed $10 upon completion of their telephone assessment.
Electronic Notification of the Anxiety Diagnosis Procedure
We notified a patient's PCP of the GAD and/or PD diagnosis on the PRIME-MD by means of an interactive e-mail alert (“flag”) generated through our EMR system and via an electronic letter signed by the investigators. These messages were generally transmitted to the PCP within 1 business day of the patient's completion of the PRIME-MD. They asked PCPs to indicate whether they “agreed,”“disagreed,” or were “unsure” of the PRIME-MD finding. However, the PCP was not informed of his/her patient's severity of anxiety symptoms on either the SIGH-A or the PDSS. When PCPs indicated agreement with the diagnostic finding, the researcher entered the specific anxiety disorder into the patient's electronic medical record and recorded the date on which the PCP responded to the flag.
Statistical Analyses
We report the frequency of each diagnosis, and compare baseline sociodemographic, diagnostic, symptom severity, and PCP agreement rates by anxiety disorder. We used t tests for continuous data and χ2 analyses for categorical data. All analyses were performed with SAS version 8.2 (SAS Institute Inc., Cary, NC).
RESULTS
Patient Recruitment
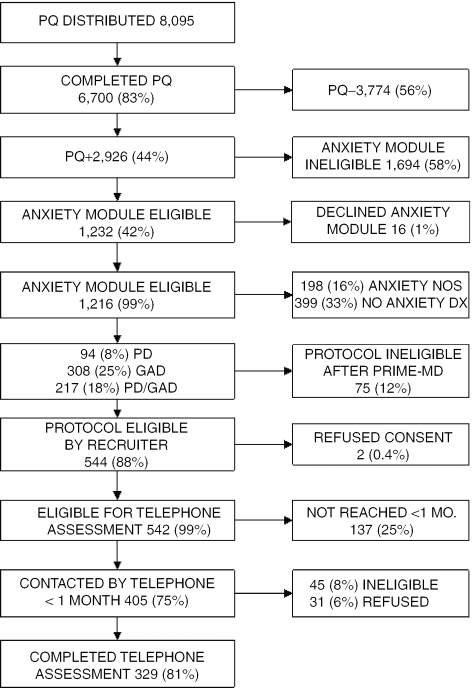
Study recruiters approached 8,095 patients aged 18 to 64 to complete the PQ and 6,700 (83%) did so (Fig. 1). Among the PQ completers, 2,926 (44%) screened positive for an anxiety disorder (PQ+). Of these, 1,694 (58%) were ineligible to continue in our protocol for a variety of reasons. They included: refusal to complete the PRIME-MD Anxiety Module (N=717); in current treatment with a mental health specialist (210); unstable medical condition52; 3 or 4 positive responses on the CAGE questionnaire45; our recruiters were unable to approach before the patient departed the PCP's office (466); and protocol ineligibility for a wide variety of other reasons (204). Overall, 1,232 (42%) met preliminary study eligibility criteria and all but 16 (1%) consented to complete the PRIME-MD Anxiety Module. Of the 619 (51%) with PD, GAD, or both conditions, 75 (12%) were protocol ineligible to continue because of: disclosure that they were actually in treatment with a mental health specialist38; refusal to continue further in our protocol22; and for a variety of other reasons.15 Of the remaining 542 (88%) patients who met a preliminary review of our protocol-eligibility criteria and consented to a further telephone assessment, we were able to later contact 405 (75%) within 1 month of their completing the PRIME-MD. Of these, 329 (81%) agreed to complete the SIGH-A and PDSS over the telephone and did so.
Figure 1.
Recruitment.
Demographic and Clinical Characteristics by Anxiety Disorder
Table 1 presents the demographic and clinical characteristics of the 329 study participants who completed the telephone assessment. Their mean age was 43 years (range 19 to 64), 78% were women, and 95% were white. None of these characteristics differed by type of anxiety disorder.
Table 1.
Baseline Demographic and Clinical Characteristics of Patients Who Completed the Telephone Assessment
| Total (N=329) | PD (N=41) | GAD (N=169) | PD and GAD (N=119) | P | |
|---|---|---|---|---|---|
| Age, mean, (range) | 43 (19 to 64) | 44 (21 to 63) | 43 (19 to 63) | 43 (19 to 64) | .75 |
| Female, % (N) | 78 (255) | 76 (31) | 77 (130) | 79 (94) | .87 |
| White, % (N) | 95 (312) | 95 (39) | 94 (159) | 96 (114) | .89 |
| SIGH-A, mean (SD)* | 16.0 (7.5) | 12.0 (6.1) | 14.4 (6.4) | 19.5 (8.0) | <.001 |
| SIGH-A≥14, % (N) | 54 (184) | 32 (13) | 49 (83) | 73 (87) | <.001 |
| PDSS, mean (SD)†‡ | 6.8 (5.9) | 7.4 (4.3) | 2.7 (4.2) | 10.0 (5.5) | <.001 |
| PDSS≥7, mean (SD) % (N) | 49 (123) | 59 (24) | 18 (17) | 72 (82) | <.001 |
Structured Interview Guide for the Hamilton Anxiety Rating Scale (range: 0 to 56).
Panic Disorder Severity Scale (range: 0 to 28).
N=252.
PD, panic disorder; GAD, generalized anxiety disorder.
Patients with both PD and GAD scored significantly higher on the SIGH-A than those with only PD or GAD (P<.001) and were most likely to score at or above the treatment phase protocol-eligibility criterion of moderate anxiety severity (SIGH-A ≥14 or PDSS ≥7; both P<.001). Additionally, patients with PD alone and PD/GAD tended to score higher on the PDSS than others with GAD alone (P<.001).
Overall, 59% (170/288) of patients who met the criteria for GAD on the PRIME-MD scored ≥14 on the SIGH-A, and only 7% (13/183) of those above this cut-off score did not meet the criteria for GAD. Among those who met the criteria for PD, 68% (106/155) scored ≥7 on the PDSS and only 14% (17/123) of those above this cut-off score did not meet the criteria for PD (Table 2).
Table 2.
Distribution of PRIME-MD Anxiety Disorders by Level of Anxiety Symptoms
| PRIME-MD Diagnosis | Frequency (Row %) | Frequency (Row %) | Total |
|---|---|---|---|
| SIGH-A<14* (mild anxiety) | SIGH-A≥14* (moderate–severe anxiety) | ||
| GAD+ | 118 (41) | 170 (59) | 288 |
| GAD− | 28 (68) | 13 (32) | 41 |
| Total | 146 (44) | 183 (56) | 329 |
| PDSS<7† (mild anxiety) | PDSS≥7† (moderate–severe anxiety) | ||
| PD+ | 49 (32) | 106 (68) | 155 |
| PD− | 80 (82) | 17 (18) | 97 |
| Total | 129 (51) | 123 (49) | 252 |
Structured Interview Guide for the Hamilton Anxiety Rating Scale.
Panic Disorder Severity Scale.
PRIME-MD, Primary Care Evaluation of Mental Disorders; PD, panic disorder; GAD, generalized anxiety disorder.
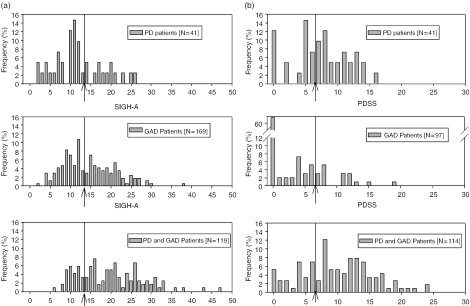
Figure 2, A and B present the full distribution of PDSS and SIGH-A scores by type of PRIME-MD anxiety disorder. Notably, a substantial minority of patients who met the criteria for an anxiety disorder on the PRIME-MD reported few if any anxiety symptoms on the SIGH-A and/or PDSS. A smaller number of GAD patients completed the PDSS than the SIGH-A, reflecting a change in our protocol to administer the PDSS to all patients rather than just to those with PD or PD/GAD.
Figure 2.
Distribution of anxiety severity scores for patients completing a telephone interview by assessment measure and anxiety disorder. Moderate-to-severe levels of anxiety severity are to the right of the arrows. (A) Structured Interview Guide for the Hamilton Anxiety Rating Scale (SIGH-A; range: 0 to 56). (B) Panic Disorder Severity Scale (PDSS; range: 0 to 28).
PCP Agreement to Electronic Notification of PRIME-MD Anxiety Diagnoses
Of the 329 who completed our telephone interview to assess the severity of their anxiety symptoms, PCPs agreed with the PRIME-MD anxiety diagnosis for 98% (321/329). This rate of agreement was similar to that of the 213 patients who provided signed inform consent to undergo our telephone assessment but did not complete the interview (95% (203/213)). PCPs agreed with the PRIME-MD diagnosis for 77% (254/329) of patients within a business day of notification, and neither agreement rate nor speed of agreement differed by type of diagnosis. Again, these agreement patterns were similar for patients who consented to undergo our telephone assessment but did not complete the follow-up interview (77%; 161/209).
DISCUSSION
We conclude from our data that1: (1) the PRIME-MD can be used to screen and diagnose primary care patients for PD and GAD within a variety of busy primary care settings2; (2) patients diagnosed by the PRIME-MD Anxiety Module as having either PD, GAD, or both endorse anxiety symptoms of wide-ranging severity; and3 (3) PCPs rapidly agree with the finding of an anxiety disorder on the PRIME-MD independent of their patients' level of anxiety symptomatology. These findings suggest that health care delivery organizations interested in identifying primary care patients with PD and/or GAD can use the PRIME-MD as a part of a broader strategy to improve quality of care for individuals with these conditions.
We are unaware of other clinical trials that utilized the PRIME-MD to identify patients with an anxiety disorder. However, an entirely self-administered version of the PRIME-MD—the Patient Health Questionnaire (PHQ)—was developed and validated in a large cross-sectional study of primary care patients.26 Still, compared with the PRIME-MD, the PHQ is only capable of making a precise diagnosis of panic disorder and not GAD. Furthermore, the skip-out design of the PHQ's anxiety module does not facilitate its use as an anxiety severity and outcome measure, in contrast to the PHQ's 9-item depression module.32,33 Therefore, when targeting anxiety disorders, the PRIME-MD has some diagnostic advantages over the newer PHQ.
Because PD and GAD are 2 of the most prevalent and treatable anxiety disorders seen in primary care, it is of great interest that PCPs rapidly agreed with the vast majority of PD and GAD cases thus identified by the PRIME-MD, and regardless of the type of anxiety disorder or episode severity. We did not ask PCPs to justify their decision making or otherwise impose any additional burden on them when they disagreed with the PRIME-MD. Therefore, PCPs' agreement with the PD and GAD diagnoses at similar rates and regardless of their patients' actual level of anxiety symptoms possibly suggests that PCPs were either unfamiliar at recognizing these anxiety disorders and/or relied on the PRIME-MD and the clinical investigators to inform them of the diagnosis. This finding is in contrast to our earlier work where PCPs disagreed with the finding of major depression on the PRIME-MD for 23% of patients when presented to them in a similar electronic fashion as in our current trial.34
A substantial minority of patients detected by the PRIME-MD as experiencing PD and GAD had relatively mild levels of anxiety symptoms and it is presently unclear what, if any, treatment is required for these individuals. Additionally, the inclusion of substantial numbers of patients with diagnosable but mild levels of anxiety into a clinical trial or a quality improvement program could adversely affect sample size calculations. Thus, large numbers of patients would need to be enrolled to demonstrate statistically significant, let alone clinically meaningful, symptom improvements. Therefore, we favor administration of a time-efficient case-finding instrument such as the PRIME-MD followed by a measure of distress such as the SIGH-A or PDSS to determine whether a patient's condition is sufficiently severe to warrant active treatment.28,35,36
As is the case for primary care patients with major depression, those treated for PD and GAD in the primary care sector tend to experience poorer than expected clinical outcomes for these conditions despite the availability of efficacious pharmacologic and non-pharmacologic treatments that PCPs can readily provide.35–41 Possible explanations include PCPs' inadequate recognition of anxiety disorders, PCP and/or patient resistance to a psychiatric diagnosis and its associated stigma, and competing demands on PCP's time by patient concerns within the limit of the typical 15-minute clinical encounter.42–44
While tempting to speculate that systematic screening for the presence of an anxiety disorder could help overcome these barriers and improve clinical outcomes, reports from the depression literature suggest otherwise.27,41,45–47 Nevertheless, recognition of the anxiety disorder is a necessary first step. A variety of “collaborative care” strategies48 for treating depressed primary care patients that include a case-finding component and systematic follow-up by a care manager who follows an evidence-based protocol in concert with patients' PCPs have been proven effective.49 Initial studies suggest that these strategies can be clinically effective35,50 and cost-effective 51 at treating anxiety disorders.
This study has several limitations potentially affecting the generalizability of our conclusions. First, our findings may only apply to whites given that they constituted 95% of the study sample (Table 1). This racial pattern reflects the fact that 85% of the subjects were recruited from 3 practices located in suburban-rural Westmoreland County, PA, where, according to the 2000 U.S. Census, only 3.4% of the population was nonwhite. Second, we relied on dedicated patient recruiters stationed in our study practices' reception rooms to administer, score, and collect the PRIME-MD. While this strategy is feasible within the context of research which requires that investigators obtain subjects' signed informed consent, such case identification procedures may not be applicable to routine practice. Nevertheless, administration of the PRIME-MD by nonclinical practice staff has been found to generate significant increases in new psychiatric diagnoses and subsequent PCP interventions at support levels achievable in most clinical settings.52 Third, we did not verify our PRIME-MD diagnoses with a “gold-standard” clinical interview administered by a mental health professional, the procedure utilized to validate the PRIME-MD.10 Fourth, we excluded the majority (58%) of PQ+ patients from the PRIME-MD Anxiety Module interview and a number of patients with PD and/or GAD from our telephone assessment of anxiety severity. Still, this strategy is acceptable for maintaining internal validity within the context of a clinical trial as we did not aim to establish the prevalence of PD and GAD in primary care.
In summary, the PRIME-MD can be used by non-PCP personnel to efficiently screen primary care patients for PD and GAD within a variety of busy primary care settings. Furthermore, patients thus identified by the PRIME-MD as having PD and GAD endorse a wide range of anxiety symptom severity, and PCPs rapidly agree with these diagnoses when presented to them electronically regardless of the severity of their patients' symptomatology. Our findings have important implications for use of the PRIME-MD as a case-finding tool for anxiety disorders within the context of a clinical trial and as part of a quality improvement program.
Acknowledgments
This work was supported by NIMH grant R01 MH59395.
References
- 1.Stein MB, Barrett-Connor E. Quality of life in older adults receiving medications for anxiety, depression, or insomnia. findings from a community-based study Am J Geriatric Psychiatry. 2002;10:568–574. [PubMed] [Google Scholar]
- 2.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Mortality and quality of life 12 months after myocardial infarction. effects of depression and anxiety Psychosomatic Med. 2001;63:221–230. doi: 10.1097/00006842-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Cass AR, Volk RJ, Nease DE., Jr Health-related quality of life in primary care patients with recognized and unrecognized mood and anxiety disorders. Int J Psychiatry Med. 1999;29:293–309. doi: 10.2190/CPYJ-2HBF-RGCN-64V2. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- 5.Regier DA, Boyd JH, Burke JD, Jr, et al. One-month prevalence of mental disorders in the United States. Based on five epidemiologic catchment area sites. Arch Gen Psychiatry. 1988;45:977–986. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- 6.Leon AC, Portera L, Weissman MM. The social costs of anxiety disorders. Br J Psychiatry. 1995;(Suppl):19–22. [PubMed] [Google Scholar]
- 7.Katerndahl DA. Panic attacks and panic disorder. J Fam Practice. 1996;43:275–282. [PubMed] [Google Scholar]
- 8.Sherbourne CD, Jackson CA, Meredith LS, Camp P, Wells KB. Prevalence of comorbid anxiety disorders in primary care outpatients. Arch Fam Med. 1996;5:27–34. doi: 10.1001/archfami.5.1.27. [DOI] [PubMed] [Google Scholar]
- 9.Shear MK, Schulberg HC. Anxiety disorders in primary care. Bull of the Menninger Clinic. 1995;59(suppl A):A73–85. [PubMed] [Google Scholar]
- 10.Spitzer RL, Williams JBW, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. the PRIME-MD 1000 study JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 11.Katon W. Panic disorder. epidemiology, diagnosis, and treatment in primary care J Clin Psychiatry. 1986;47(suppl):21–30. [PubMed] [Google Scholar]
- 12.Sherbourne CD, Wells KB, Judd LL. Functioning and well-being of patients with panic disorder. Am J Psychiatry. 1996;153:213–218. doi: 10.1176/ajp.153.2.213. [DOI] [PubMed] [Google Scholar]
- 13.Andersen SM, Harthorn BH. The recognition, diagnosis, and treatment of mental disorders by primary care physicians. Med Care. 1989;27:869–886. doi: 10.1097/00005650-198909000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Fifer SK, Mathias SD, Patrick DL, Mazonson PD, Lubeck DP, Buesching DP. Untreated anxiety among adult primary care patients in a health maintenance organization. Arch Gen Psychiatry. 1994;51:740–750. doi: 10.1001/archpsyc.1994.03950090072010. [DOI] [PubMed] [Google Scholar]
- 15.Ormel J, Koeter MW, van den Brink W, van de Willige G. Recognition, management, and course of anxiety and depression in general practice. Arch Gen Psychiatry. 1991;48:700–706. doi: 10.1001/archpsyc.1991.01810320024004. [DOI] [PubMed] [Google Scholar]
- 16.Harman JS, Rollman BL, Hanusa BH, Lenze EJ, Shear MK. Physician office visits of adults for anxiety disorders in the United States, 1985–1998. J Gen Intern Med. 2002;17:165–172. doi: 10.1046/j.1525-1497.2002.10409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krasucki C, Ryan P, Ertan T, Howard R, Lindesay J, Mann A. The FEAR. a rapid screening instrument for generalized anxiety in elderly primary care attenders Int J Geriatr Psychiatry. 1999;14:60–68. doi: 10.1002/(sici)1099-1166(199901)14:1<60::aid-gps893>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 18.McQuaid JR, Stein MB, McCahill M, Laffaye C, Ramel W. Use of brief psychiatric screening measures in a primary care sample. Depression Anxiety. 2000;12:21–29. doi: 10.1002/1520-6394(2000)12:1<21::AID-DA3>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 19.Wittchen HU, Boyer P. Screening for anxiety disorders. Sensitivity and specificity of the Anxiety Screening Questionnaire (ASQ-15) Br J Psychiatry. 1998;(Suppl):10–17. [PubMed] [Google Scholar]
- 20.Parkerson GR, Jr, Broadhead WE. Screening for anxiety and depression in primary care with the Duke anxiety–depression scale. Fam Med. 1997;29:177–181. [PubMed] [Google Scholar]
- 21.Leon AC, Olfson M, Weissman MM, et al. Brief screens for mental disorders in primary care. J Gen Intern Med. 1996;11:426–430. doi: 10.1007/BF02600191. [DOI] [PubMed] [Google Scholar]
- 22.Baughman OL. Rapid diagnosis and treatment of anxiety and depression in primary care. the somatizing patient J Fam Practice. 1994;39:373–378. [PubMed] [Google Scholar]
- 23.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29:169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Cleary PD, Goldberg ID, Kessler LG, Nycz GR. Screening for mental disorder among primary care patients. Usefulness of the general health questionnaire. Arch Gen Psychiatry. 1982;39:837–840. doi: 10.1001/archpsyc.1982.04290070065012. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB, et al. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3:774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report version of the PRIME-MD. The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 27.Rollman BL, Hanusa BH, Lowe HJ, Gilbert T, Kapoor WN, Schulberg HC. A randomized trial using computerized decision support to improve the quality of treatment for major depression in primary care. J Gen Intern Med. 2002;17:493–503. doi: 10.1046/j.1525-1497.2002.10421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rollman BL, Herbeck Belnap B, Reynolds C, Schulberg H, Shear M. A contemporary protocol for the treatment of panic and generalized anxiety in primary care. Gen Hosp Psychiatry. 2003;25:74–82. doi: 10.1016/s0163-8343(03)00004-5. [DOI] [PubMed] [Google Scholar]
- 29.Ewing JA. Detecting alcoholism. the CAGE questionnaire JAMA. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 30.Shear MK, Vander Bilt J, Rucci P, et al. Reliability and validity of a structured interview guide for the hamilton anxiety rating scale (SIGH-A) Depression Anxiety. 2001;13:166–178. [PubMed] [Google Scholar]
- 31.Shear MK, Brown TA, Barlow DH, et al. Multicenter collaborative panic disorder severity scale. Am J Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Spitzer RL, Williams JB. The PHQ-9. validity of a brief depression severity measure J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument. sensitivity to change of the Patient Health Questionnaire (PHQ-9) J Affective Dis. 2004;81:61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- 34.Rollman BL, Hanusa BH, Gilbert T, Lowe HJ, Kapoor WN, Schulberg HC. The electronic medical record. a randomized trial of its impact on primary care physicians' initial management of major depression Arch Intern Med. 2001;161:189–197. doi: 10.1001/archinte.161.2.189. [DOI] [PubMed] [Google Scholar]
- 35.Roy-Byrne PP, Katon W, Cowley DS, Russo J. A randomized effectiveness trial of collaborative care for patients with panic disorder in primary care. Arch Gen Psychiatry. 2001;58:869–876. doi: 10.1001/archpsyc.58.9.869. [DOI] [PubMed] [Google Scholar]
- 36.Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive–behavioral therapy, imipramine, or their combination for panic disorder. a randomized controlled trial JAMA. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- 37.Gorman JM. Treatment of generalized anxiety disorder. J Clin Psychiatry. 2002;63(suppl 8):17–23. [PubMed] [Google Scholar]
- 38.Katz IR, Reynolds CF, III, Alexopoulos GS, Hackett D. Venlafaxine ER as a treatment for generalized anxiety disorder in older adults. pooled analysis of five randomized placebo-controlled clinical trials JAGS. 2002;50:18–25. doi: 10.1046/j.1532-5415.2002.50003.x. [DOI] [PubMed] [Google Scholar]
- 39.Schweizer E, Rickels K. Strategies for treatment of generalized anxiety in the primary care setting. J Clin Psychiatry. 1997;58(suppl 3):27–31. discussion 32–3. [PubMed] [Google Scholar]
- 40.Practice Guideline for Treatment of Patients with Panic Disorder and Related Anxiety Disorders. Washington, DC: American Psychiatric Association; 1998. [Google Scholar]
- 41.Stein MB, Sherbourne CD, Craske MG, et al. Quality of care for primary care patients with anxiety disorders. Am J Psychiatry. 2004;161:2230–2237. doi: 10.1176/appi.ajp.161.12.2230. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein MZ. Depression and anxiety in older women. Primary Care; Clin Office Pract. 2002;29:69–80. doi: 10.1016/s0095-4543(03)00074-5. vi. [DOI] [PubMed] [Google Scholar]
- 43.Rost K, Smith R, Matthews DB, Guise B. The deliberate misdiagnosis of major depression in primary care. Arch Fam Med. 1994;3:333–337. doi: 10.1001/archfami.3.4.333. [DOI] [PubMed] [Google Scholar]
- 44.Rost K, Nutting P, Smith J, Coyne JC, Cooper-Patrick L, Rubenstein L. The role of competing demands in the treatment provided primary care patients with major depression. Arch Fam Med. 2000;9:150–154. doi: 10.1001/archfami.9.2.150. [DOI] [PubMed] [Google Scholar]
- 45.Williams JW, Mulrow CD, Jr, Kroenke K, et al. Case-finding for depression in primary care. a randomized trial Am J Med. 1999;106:36–43. doi: 10.1016/s0002-9343(98)00371-4. [DOI] [PubMed] [Google Scholar]
- 46.Reifler DR, Kessler HS, Bernhard EJ, Leon AC, Martin GJ. Impact of screening for mental health concerns on health service utilization and functional status in primary care patients. Arch Intern Med. 1996;156:2593–2599. [PubMed] [Google Scholar]
- 47.Callahan CM, Hendrie HC, Dittus RS, Brater DC, Hui SL, Tierney WM. Improving treatment of late life depression in primary care. a randomized clinical trial J Am Geriatr Soc. 1994;42:839–846. doi: 10.1111/j.1532-5415.1994.tb06555.x. [DOI] [PubMed] [Google Scholar]
- 48.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. essential elements Ann Intern Med. 1997;127:1097–1002. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 49.Neumeyer-Gromen A, Lampert T, Stark K, Kallischnigg G. Disease management programs for depression. a systematic review and meta-analysis of randomized controlled trials Med Care. 2004;42:1211–1221. doi: 10.1097/00005650-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 50.Rollman BL, Belnap BH, Mazumdar S, Zhu F, Schulberg HC, Shear MK. The impact of a collaborative care intervention for panic and generalized anxiety disorder (PD/GAD) on anxiety symptomology, health-related quality of life, and work outcomes at 12–month follow-up. J Gen Intern Med. 2004;19(suppl):219. [Google Scholar]
- 51.Katon WJ, Roy-Byrne P, Russo J, Cowley D. Cost-effectiveness and cost offset of a Collaborative Care intervention for primary care patients with panic disorder. Arch Gen Psychiatry. 2002;59:1098–1104. doi: 10.1001/archpsyc.59.12.1098. [DOI] [PubMed] [Google Scholar]
- 52.Valenstein M, Dalack G, Blow F, Figueroa S, Standiford C, Douglass A. Screening for psychiatric illness with a combined screening and diagnostic instrument. J Gen Intern Med. 1997;12:679–685. doi: 10.1046/j.1525-1497.1997.07141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]