Abstract
Background
Gender differences in inpatient quality of care are well known. However, whether men and women receive equivalent ambulatory care is less well understood.
Objective
To study gender differences in quality of care for patients receiving primary care in the Veterans Affairs (VA) Health Care System.
Design
Cross-sectional samples of VA enrollees during fiscal years 1999 to 2000.
Participants
Samples of 6,442 to 86,405 men and women treated at VA facilities for whom at least 1 of 9 quality measures was available.
Measurements
Appropriate general preventive services (pneumococcal vaccination, influenza vaccination, colorectal cancer screening), and specific services for diabetes (annual hemoglobin A1c [HbA1c] testing, good glycemic control, annual diabetic eye exam), hypertension (good blood pressure control), or prior myocardial infarction (use of β-blockers or aspirin).
Results
In adjusted analyses, there were no substantial gender differences in rates of appropriate care. For women compared with men, the adjusted relative risk for appropriate care ranged from 0.96 for blood pressure control (95% confidence interval: 0.93 to 0.99; P=.02) to 1.05 for HbA1c≤8.0% (95% confidence interval: 1.03 to 1.07; P<.01). Analyses stratified by age demonstrated equivalent care between men and women in 9 of the 14 subgroups evaluated.
Conclusions
In this large national health care system that predominantly serves men, the quality of ambulatory care is equivalent for women and men on numerous measures.
Keywords: gender, quality, veterans, prevention, diabetes mellitus
Men and women do not always receive equivalent care,1,2 and these differences may be because of nonclinical factors. Women often receive poorer care after admission for congestive heart,1 coronary heart disease,3–5 and other common medical conditions.2 In contrast, gender differences in the quality of ambulatory medical care are largely unexplored, although limited data suggest that disparities may exist in this setting as well.6
The Department of Veterans Affairs (VA) runs the largest integrated health care system in the United States. Although men make up a large majority of veterans who receive care in the VA, women now comprise nearly 10% of the 4 million users and are a rapidly rising group. Given the rising numbers of women in military service in recent decades, the number of women seeking care in the VA is expected to grow. While recent data suggest dramatic improvement in quality of care for veterans,7 it is unclear whether men and women have shared equally in this advancement. Using common indicators, we sought to determine whether gender differences exist in the quality of ambulatory care in this large, national health care system.
METHODS
Design
We used data from VA External Peer Review Program8 to assess quality of care during fiscal years 1999 to 2000 (October 1, 1998 to September 30, 2000). External Peer Review Program data are derived from cross-sectional samples of medical records reviewed by trained abstractors with high interrater reliability scores (κ 0.90)7 and oversight both from the Congressional committees of VA and the Government Accounting Office.9 The study protocol was approved by the Institutional Review Boards of the Boston VA Health Care System and Brigham and Women's Hospital.
Patients with 2 years of continuous enrollment in the VA and at least 1 ambulatory visit in the previous 12 months were eligible for sampling. A random sample of all patients within each of the 22 regional networks was obtained annually in adequate numbers to ensure reproducible precision for estimated rates in each network.10 In addition, random samples of patients with prevalent chronic diseases (e.g., diabetes, ischemic heart disease, and chronic obstructive pulmonary disease) were selected in each network, and women were oversampled.
Quality Indicators
We studied 9 quality measures that are equally appropriate for women and men, including 3 preventive measures (vaccinations and cancer screening tests) and 6 chronic disease management measures (e.g., annual retinal exams in diabetics) (Appendix, available online). These indicators were developed by the VA and are similar to measures developed by the National Committee for Quality Assurance to assess health plans in the Health Plan Employer Data and Information Set (HEDIS).11 Each of the quality measures reflects recommendations made in national guidelines.12–14
Statistical Analysis
We measured the association between gender and individual quality measures using prevalence ratios and χ2 tests. This study had a statistical power of greater than 95% power to detect a 3% difference in adherence rates in each of the quality markers, except for patients with prior myocardial infarction (MI) (aspirin and β-blocker use), where this study had 80% power to detect a 6% difference in rates.
Subsequently, using multivariate logistic regression and generalized estimating equations to adjust for age and institutional characteristics (number of housestaff, number of hospital beds, and region of the country), we assessed whether gender was independently associated with each quality measure and converted odds ratios (ORs) to relative risks using standard methods.15 We tested for interactions of gender with age and hospital characteristics as predictors of adherence to quality indicators. Because we were aware a priori that women were younger and that age was related to adherence to quality indicators, we chose to stratify our multivariate analyses by age (<65 vs ≥65 years), except for post-MI use of aspirin and β-blockers because fewer than 100 women were eligible for these measures. All analyses were performed using Stata 7.0 (College Station, TX).
RESULTS
The sample sizes for the 9 quality measures ranged from 6,695 post-MI patients to 86,405 patients eligible for pneumococcal vaccination (see Appendix). Women represented between 13% and 23% of the samples (Appendix) for most of the quality measures, except for post-MI patients (1.4%). Women were younger than men. There were small although statistically significant differences in facility and geographic characteristics for men and women sampled for these quality measures (Table 1).
Table 1.
Baseline Characteristics of Men and Women in the EPRP Sample*
| Characteristics | Women, % (n) | Men, % (n) | P Value |
|---|---|---|---|
| Age (y) | 59.9 | 66.4 | <.001 |
| Region | <.001 | ||
| Northeast | 25 (2,000) | 21 (15,006) | |
| Midwest | 25 (1,934) | 33 (23,450) | |
| South | 26 (2,063) | 27 (19,335) | |
| West | 24 (1,847) | 20 (14,244) | |
| Hospital size (no. of beds) | 309 | 307 | .85 |
| Urban hospital % (n) | 38 (9,027) | 34 (72,879) | <.001 |
| High technology % (n) | 32 (7,615) | 33 (69,429) | <.001 |
| Academic hospital % (n) | 40 (10,114) | 42 (69,445) | <.001 |
For those eligible for the pneumococcal vaccine.
EPRP, External Peer Review Program.
Adherence to quality indicators ranged from 47% for blood pressure control to 98% for aspirin among patients with a prior MI (Table 2). In unadjusted analyses, women were less likely to receive 5 of the 9 appropriate services and more likely to receive the other 4. Adjusting for differences in age and hospital characteristics, we found that women and men received comparable care, with relative risks for women compared with men ranging from 0.96 for adequate blood pressure control to 1.05 for good glycemic control (Table 2). While some of the differences between men and women were statistically significant, the magnitude and differences direction of these differences were small and inconsistent.
Table 2.
Percentage of Enrollees Receiving Appropriate Care by Gender with Prevalence Ratios
| Quality Indicator | Women, % | Men, % | Unadjusted Relative Risk | P Value | Adjusted Relative Risk (95% CI) | P Value |
|---|---|---|---|---|---|---|
| Pneumococcal vaccination | 74.0 | 79.7 | 0.93 | <.01 | 0.98 (0.97–0.99) | <.01 |
| Influenza vaccination | 73.4 | 76.5 | 0.96 | <.01 | 0.99 (0.97–1.00) | .03 |
| Colorectal cancer screening | 68.9 | 69.9 | 0.99 | .03 | 0.99 (0.97–1.00) | .10 |
| Diabetic eye exam screen | 67.0 | 68.6 | 0.98 | .01 | 0.98 (0.96–1.00) | .10 |
| Annual HbA1c | 94.7 | 94.3 | 1.01 | .30 | 1.00 (0.99–1.01) | .71 |
| HbA1c <8.0 % | 61.1 | 62.0 | 0.99 | .20 | 1.05 (1.03–1.07) | <.01 |
| Aspirin after MI | 97.8 | 97.3 | 1.01 | .74 | 1.00 (0.96–1.02) | .72 |
| β-blocker after MI | 95.7 | 95.0 | 1.01 | .78 | 1.01 (0.95–1.03) | .75 |
| Blood pressure ≤140/90 mmHg | 48.0 | 47.4 | 1.01 | .47 | 0.96 (0.93–0.99) | .02 |
MI, myocardial infarction; HbA1c, hemoglobin A1c; CI, confidence interval.
Adjusted for age, region of country, hospital size, hospital location (urban vs nonurban), academic status of hospital or clinic.
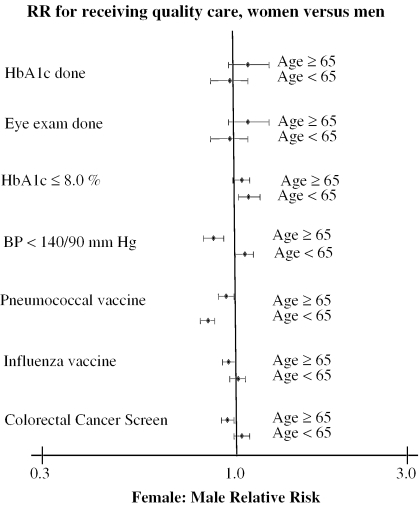
In additional multivariable analyses stratified by age, men and women received comparable care in nearly all subgroups (Fig. 1). Among the 14 subgroups, women had higher rates of appropriate care for 7 measures, while men had higher rates for the other 7. The odds ratios (women compared with men) for the subgroups ranged from 0.78 (pneumococcal vaccination among those less than 65 years old) to 1.13 (hemoglobin A1c (HbA1c) control among those younger than 65 years old). Differences in 5 of these 14 subgroup analyses were statistically significant. Among those younger than 65 years of age, women were more likely to receive appropriate HbA1c testing (OR 1.13, 95% confidence interval 1.03 to 1.25) and adequate hypertension control (OR 1.09, 95% confidence interval 1.00 to 1.18) but less likely to receive a pneumococcal vaccine (OR 0.78, 95% confidence interval 0.73 to 0.83). Among older patients, women were less likely to receive adequate hypertension control (OR 0.82, 95% confidence interval 0.75 to 0.90) and pneumococcal vaccination (OR 0.92, 95% confidence interval 0.86 to 0.99).
FIGURE 1.
Risk ratio with 95% confidence interval (CI) for receiving quality care, stratified by age. Post-myocardial infarction (MI) patients not analyzed in subgroups because of small sample size and lack of interaction by age group.
DISCUSSION
Among patients treated in the VA health care system, we found remarkably similar quality of ambulatory care for women and men for both preventive services and chronic disease management. Quality of care was high for most services, but even in situations where care was less than optimal (e.g., blood pressure management), men and women received similar care.
Although gender differences in the quality of ambulatory care are largely unexplored, prior studies suggest that women may receive lower quality of care in these settings. Women receive low rates of secondary cardiac prevention,16 although few studies have performed direct comparisons with men. Among known gender differences in the quality of ambulatory care, women with coronary heart disease have lower rates of cardiac referral17,18 after an admission for an MI and may receive lower rates of appropriate diabetes care19 than men. One recent evaluation of 10 commercial and 9 Medicare health plans found that women were less likely to receive β-blockers after an MI and that women receive lower rates of diabetes preventive measures. 6 Herlholz et al.20 similarly found lower rates of critical cardiovascular drug use among women discharged with an acute MI. Schneider et al.21 found no variation in HEDIS measures by sex among Medicare managed care patients.
Equal care for men and women should be interpreted in the context of significant gains in quality that the VA has achieved over the past 8 years.7,22,23 In the middle of the 1990s, the VA undertook a major reengineering program to improve quality by decentralizing clinical management to 22 regional networks, instituting performance measurement programs, and creating a data collection system to monitor quality.7 Further, in an effort to improve care to women, VA dedicated special primary care clinics for women only. Over half of VA hospitals have specialized Women's Health Clinics, although a majority of women enrollees receive most or nearly all their care in general medical clinics.24 Veterans Affairs quality improvement efforts targeted gender-specific measures, which led to VA outperforming the private sector with higher rates of both mammography and cervical cancer screening.7 It may be that broad-based quality improvement efforts may reduce variations in care and this may help explain the gender parity in quality of ambulatory care.
Our study has important limitations. First, we were unable to adjust for several potentially important confounders such as socioeconomic status, comorbidities and health status, and utilization rates, all of which could be associated with quality of care. However, female enrollees in the VA are more likely to be poor and unemployed,25 have lower functional status24, and health status26 than male enrollees. Further, adjusted for age, women enrollees have lower rates of VA utilization than their male counterparts.27 Therefore, these factors are likely to bias us toward finding worse care for women. Second, while we found generally high-quality care, there were still areas where men and women both received less than optimal care, such as hypertension management. While the quality of hypertension care improved in the VA from 1995 through 2000, and while rates of adequate blood pressure control in the VA are comparable with the private sector,22 these are still areas that require improvement. Finally, because we used process measures to assess quality of care, we could not discern whether women and men have equal outcomes.
In conclusion, we found remarkably similar quality of care for women and men in outpatient preventive services and chronic disease management in the VA. This equal care may be related to the large strides in quality that the VA has achieved in the past decade.
Supplementary Material
The following supplementary material is available for this article online:
Quality Indicators and Sampling Frame for Men and Women in the EPRP Dataset.
Acknowledgments
The data were provided by the Office of Quality and Performance, VA Central Office. Dr. Jha was funded in part by the Office of Quality and Performance, Veterans Health Administration, and by an Institutional National Research Service Award (#5T32HS00020-16) from the Agency for Healthcare Research and Quality. We are indebted to Drs. Jennifer Haas and Eric Schneider for their thoughtful comments and suggestions on an earlier draft of the manuscript.
References
- 1.Ayanian JZ, Weissman JS, Chasan-Taber S, Epstein AM. Quality of care by race and gender for congestive heart failure and pneumonia. Med Care. 1999;37:1260–9. doi: 10.1097/00005650-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Jha AK, Kuperman GJ, Rittenberg E, Bates DW. Gender and utilization of ancillary services. J Gen Intern Med. 1998;13:476–81. doi: 10.1046/j.1525-1497.1998.00137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udvarhelyi IS, Gatsonis C, Epstein AM, Pashos CL, Newhouse JP, McNeil BJ. Acute myocardial infarction in the medicare population. Process of care and clinical outcomes. JAMA. 1992;268:2530–6. [PubMed] [Google Scholar]
- 4.Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–5. doi: 10.1056/NEJM199107253250401. [DOI] [PubMed] [Google Scholar]
- 5.Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–100. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 6.Bird CE, Fremont A, Wickstrom S, Bierman AS, McGlynn E. Improving women's quality of care for cardiovascular disease and diabetes. Women's Health Issues. 2003;13:150–7. doi: 10.1016/s1049-3867(03)00035-5. [DOI] [PubMed] [Google Scholar]
- 7.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the veterans affairs health care system on the quality of care. N Engl J Med. 2003;348:2218–27. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 8.Veteran's Health Administration. Performance Measurement System Technical Manual. Washington, DC: Office of Quality and Performance; 2000. [Google Scholar]
- 9.General Accounting Office. VA Hospitals: Issues and Challenges for the Future. Washington, DC: General Accounting Office; 1998. pp. 1–328. [Google Scholar]
- 10.Perlin JB, Kolodner RM, Roswell RH. The veterans health administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manage Care. 2004;10:828–36. [PubMed] [Google Scholar]
- 11.Health Plans Employer Data and Information Set (HEDIS) National Committee for Quality Assurance (NCQA) Measuring the quality of America's health care, item # 10235–100–00.
- 12.Adult immunizations 1994. Task force on adult immunization. Ann Intern Med. 1994;121:540–1. [PubMed] [Google Scholar]
- 13.Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN. Screening for colorectal cancer in adults at average risk: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:132–41. doi: 10.7326/0003-4819-137-2-200207160-00015. [DOI] [PubMed] [Google Scholar]
- 14.Pignone MP, Gaynes BN, Rushton JL, et al. Screening for depression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136:765–76. doi: 10.7326/0003-4819-136-10-200205210-00013. [DOI] [PubMed] [Google Scholar]
- 15.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 16.Vittinghoff E, Shlipak MG, Varosy PD, et al. Risk factors and secondary prevention in women with heart disease: the heart and estrogen/progestin replacement study. Ann Intern Med. 2003;138:81–9. doi: 10.7326/0003-4819-138-2-200301210-00007. [DOI] [PubMed] [Google Scholar]
- 17.Ayanian JZ, Landrum MB, Guadagnoli E, Gaccione P. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. N Engl J Med. 2002;347:1678–86. doi: 10.1056/NEJMsa020080. [DOI] [PubMed] [Google Scholar]
- 18.Rathore SS, Berger AK, Weinfurt KP, et al. Race, sex, poverty, and the medical treatment of acute myocardial infarction in the elderly. Circulation. 2000;102:642–8. doi: 10.1161/01.cir.102.6.642. [DOI] [PubMed] [Google Scholar]
- 19.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 20.Herholz H, Goff DC, Ramsey DJ, et al. Women and mexican americans receive fewer cardiovascular drugs following myocardial infarction than men and non-hispanic whites: the corpus christi heart project, 1988–1990. J Clin Epidemiol. 1996;49:279–87. doi: 10.1016/0895-4356(95)00572-2. [DOI] [PubMed] [Google Scholar]
- 21.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA. 2002;287:1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 22.Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the veterans affairs health care system and commercial managed care: the triad study. Ann Intern Med. 2004;141:272–81. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 23.Luck J, Peabody JW. Improving the public sector: can reengineering identify how to boost efficiency and effectiveness at a VA medical center? Health Care Manage Rev. 2000;25:34–44. doi: 10.1097/00004010-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Yano EM, Washington DL, Goldzweig C, Caffrey C, Turner C. The organization and delivery of women's health care in Department Of Veterans Affairs Medical Center. Womens Health Issues. 2003;13:55–61. doi: 10.1016/s1049-3867(02)00198-6. [DOI] [PubMed] [Google Scholar]
- 25.Klein RE Data on the Socioeconomic Status of veterans and VA Program Usage. Veterans Health Administration. October 24, 2002.
- 26.Skinner K, Sullivan LM, Tripp TJ, et al. Comparing the health status of male and female veterans who use VA health care: results from the VA women's health project. Women Health. 1999;29:17–33. doi: 10.1300/J013v29n04_02. [DOI] [PubMed] [Google Scholar]
- 27.Hoff RA, Rosenheck RA. Female veterans' use of Department of Veterans Affairs health care services. Med Care. 1998;36:1114–9. doi: 10.1097/00005650-199807000-00017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Quality Indicators and Sampling Frame for Men and Women in the EPRP Dataset.