Abstract
Objective
To report rates of cost-related skipping of medications and other treatments, assess correlates of skipping, examine changes in skipping between 1998 and 2000, and identify factors associated with changes in skipping.
Design, Setting, and Participants
Cross-sectional and longitudinal analyses of surveys of a probability sample of Medicare beneficiaries in 13 states in 1998 and 2000.
Main Outcome Measure
Self-reported rates of skipping medications and other treatments.
Results
Cost-related skipping rates increased from 9.5% in 1998 to 13.1% in 2000. In separate multivariable models using 1998 and 2000 data, higher out-of-pocket costs, lower physician-patient relationship quality, low income, and lacking prescription drug coverage were associated with more skipping (P<.05 for all). Better physical and mental health, and greater age were associated with less skipping (P<.05). HMO membership was not associated with higher rates of skipping in 1998 (P=.84), but was in 2000 (P<.0004). In longitudinal analyses, increased medication costs and HMO membership were associated with the observed increase cost-related skipping between 1998 and 2000.
Conclusions
Cost-related skipping was associated with several factors, including drug coverage, poverty, poor health, and physician-patient relationship quality. The important role of physician-patient relationships in cost-related skipping has not been shown previously. Physicians should be aware of these risk factors for cost-related skipping, and initiate dialogue about problems paying for prescription medications and other treatments.
Keywords: aged, cohort studies, insurance, pharmaceutical services, prescription fees, patient compliance
There are many reasons why people do not adhere to prescribed regimens for medications and other treatments, including costs, side effects, and inconvenience.1–3 From a health policy perspective, perhaps the most concerning of these for seniors is cost. If beneficiaries underuse medications and other treatments that might improve their health because of cost, then it is important to understand the magnitude of this problem and to identify potential remedies. The recent passage of the Medicare Modernization Act will reduce out-of-pocket medication costs for some seniors, but for many others, out-of-pocket costs are likely to remain a serious problem. Furthermore, little is known about the impact of other factors such as health status, HMO membership, and physician-patient relationship quality on cost-related underuse.
Most previous work has focused on cost-related underuse of medications. It is clear that Medicare beneficiaries who do not have prescription drug coverage use fewer medications than those who do have coverage,4–9 and to that cost-related underuse of medications is associated with worse health outcomes.10,11 Furthermore, recent work shows that cost-related medication underuse is common among adults with chronic illness.12 However, only 3 papers that we are aware of directly examine the problem of cost-related medication skipping in seniors.10,13,14 Neither of these studies were longitudinal nor were they designed to understand whether physician-patient relationship quality or HMO membership was associated with underuse of medications or other treatments.
To fill in these gaps, we analyzed data from The Study of Choice and Quality in Senior Health Care, a longitudinal study of Medicare beneficiaries aged 65 and older in 13 states.15 We surveyed beneficiaries in both traditional Medicare and Medicare HMOs in 1998 and 2000. Our analyses had 3 goals: (1) to provide estimates of the rate of cost-related skipping of medications and other treatments in these 13 states, (2) to determine sociodemographic and clinical characteristics associated with skipping, and (3) to determine whether the rate of skipping increased between 1998 and 2000, and if so, why.
METHODS
Study Design and Sampling
The Study of Choice and Quality in Senior Health Care is a longitudinal observational study of Medicare beneficiaries aged 65 and older in states with a history of substantial Medicare HMO enrollment (Arizona, California, Colorado, Florida, Illinois, Massachusetts, Minnesota, New Mexico, New York, Oregon, Pennsylvania, Texas, Washington). The sampling strategy is described in detail elsewhere.15 In these states, we sampled HMOs with risk contracts and at least 3,000 enrollees at the time of sampling. We then sampled beneficiaries from HMOs. Once the HMO sample was drawn, fee-for-service (FFS) beneficiaries were matched to HMO beneficiaries on age, sex, and residential zip code, and randomly sampled in a 1-to-2 ratio (FFS:HMO). Eligibility for sampling included age ≥65 years, having Medicare Part B, continuous enrollment in either traditional Medicare or an HMO for ≥1 year. The starting sample had 10,666 Medicare HMO enrollees and 5,332 traditional Medicare enrollees (total N=15,998). All protocols were approved by the Tufts-New England Medical Center Institutional Review Board (IRB).
Data Collection and Survey Response
We used a 5-stage mail and telephone survey protocol.16 The fall 1998 baseline survey yielded 9,625 responses (response rate 64%), and the 2-year fall 2000 follow-up yielded 6,127 responses (retention rate 71%). Baseline nonresponse and subsequent loss to follow-up were associated with older age, female gender, and minority race/ethnicity (http://www.nemc.org/dccr/PrimaryCareQuality.pdf). Additionally, those lost to follow-up were older, more socioeconomically disadvantaged, and sicker than those retained. Patterns and rates of nonresponse were identical among FFS and HMO enrollees.
Study Variables
To assess cost-related skipping, we asked: “Do you ever skip medications or treatments because they are too expensive?” Response options were Yes, often, Yes, occasionally, and No, never, and were dichotomized into yes (often or occasionally) versus no for analyses.
We used Andersen's access model17,18 to select potential predictors of cost-related skipping. Predisposing factors included age, gender, race (white vs nonwhite), education (less than high school vs high school or greater), and marital status (married vs other). Enabling factors included costs (cost of medications and medical care), ability to pay, use of medical services, and physician-patient relationship quality. Respondents reported monthly out-of-pocket medication costs, with response options: no charge for medications, $1 to $24, $25 to $49, $50 to $99, $100 to $199, and $200 or more. We measured monthly health plan premium costs using the same response categories. We asked patients whether they had “insurance that covers any of the costs of prescription medication” (yes vs no). We used income as a proxy for ability to pay, dichotomized at $20,000. For utilization, we measured visits to doctors' offices in the last 6 months and overnight hospitalizations in the last 12 months. We used an indicator for traditional fee-for-service Medicare versus Medicare HMO derived from the CMS database. To measure physician-patient relationship quality, we created a summary score of dimensions of the Primary Care Assessment Survey (PCAS).19 Four of the 11 PCAS scales (communication, trust, comprehensiveness, and interpersonal care) form a relationship quality factor,20 which we divided into quartiles. To assess need, we measured the number of medications taken, the number of chronic medical conditions, and health status. For chronic conditions, we used a checklist of 11 conditions (hypertension, angina, congestive heart failure, recent myocardial infarction (MI), heart arrhythmia or valve disorder, stroke, asthma, diabetes, arthritis, any cancer, and depression).21 We measured physical and mental health status using the Physical (PCS) and Mental Component Score (MCS) of the SF-36.22
Analyses
The analytic sample included only survey respondents who reported using 1 or more prescription medications (7,130 for 1998 and 4,630 for 2000). To compare patient characteristics in 1998 and 2000, we used t tests for continuous variables and χ2 tests for dichotomous and class variables. To determine correlates of cost-related medication skipping, we first conducted bivariate analyses using χ2 tests for dichotomous and categorical variables, Wilcoxon rank sum test for ordered variables, and t tests for continuous variables. Because bivariate relationships were similar for 1998 and 2000, only the 1998 relationships are presented. We included age, gender, race, education, marital status, medication cost, prescription drug coverage, income, membership in an HMO, outpatient visits, inpatient visits, PCS, MCS, disease count, number of prescription medication, and physician-patient relationship quality as covariates in multivariable logistic regression models. We used the missing indicator method to account for missing values.23 We estimated separate multiple logistic regression models using 1998 and 2000 data.
For analyses that examined reasons for changes in cost-related medication skipping over the 2-year study period, and factors associated with these changes, we used patients who responded to surveys in 1998 and 2000, and had no missing data, an observed sample size of 3,043. This approach minimizes the possibility that any differences seen are the result of unmeasured differences between beneficiaries. Because individual beneficiaries' financial and health status can change over time, we adjusted for medication cost, prescription drug coverage, income, membership in an HMO, outpatient visits, inpatient visits, PCS, MCS, disease count, and physician-patient relationship quality.
To determine which variables in our multivariable model were associated with the observed changes in cost-related skipping, we followed a 2-step process. First, we compared the cross-sectional models from 1998 and 2000 to determine whether the odds ratios (ORs) for any of the independent variables had changed significantly. Next, we estimated the impact of these changes on rates of cost-related skipping. We used seemingly unrelated regression,24 a technique for testing coefficients across different multiple regression models estimated on the same sample, to determine whether the changes seen between 1998 and 2000 in the ORs for variables in our model were statistically significant. To quantify the impact on cost-related skipping of the variables that had changed significantly, we estimated separate multiple linear regression models for 1998 and 2000 using the variables described above. We estimated the impact of a given variable on the rate of cost-related medication skipping by multiplying the regression coefficient by the mean of the variable. We then subtracted the 2000 product from the 1998 product and compared this difference with the change in the rate of cost-related skipping between 1998 and 2000.
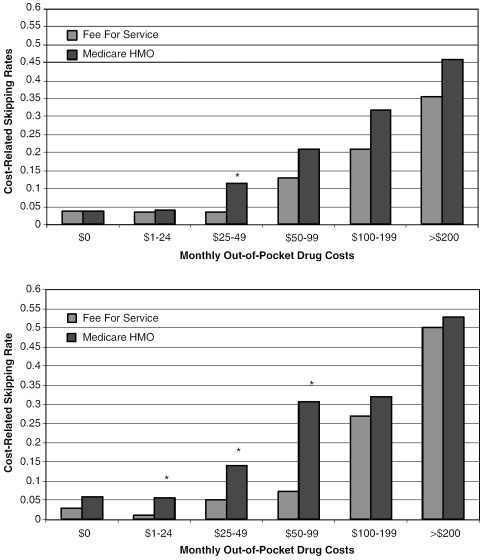
To illustrate trends in cost-related skipping, we produced adjusted bar charts of cost-related skipping in 1998 and 2000 by type of Medicare (fee-for-service vs HMO) and out-of-pocket cost group. The percentages in the graphs were adjusted via logistic regression using the same set of variables listed above for the individual 1998 and 2000 multivariable models. Percentages in HMOs were tested with corresponding percentages in FFS within year and out-of-pocket spending category through a joint logistic regression with a full set of system, spending, and year interactions.
We weighted all analyses to reflect the sampling probability. Results should be construed as generalizable to Medicare patients in the 13 study states who have been in their current health plan (either traditional Medicare or an HMO) for 1 or more years. All analyses were carried out using STATA, version 7.0 (College Station, Tex.).
RESULTS
Participant Characteristics
The mean age of beneficiaries represented by our sample in 1998 was 75.3 years (Table 1). Between 1998 and 2000, beneficiaries reported increases in the number of prescription medications (4.0 to 4.4, P=.0002), out-of-pocket costs (25% spending ≥$50 out-of-pocket per month to 35%, P<.0001), and premiums ($46 to $57, P<.0001). Rates of cost-related skipping increased from 9.5% in 1998 to 13.1% in 2000 (P<.0001).
Table 1.
Patient Characteristics*
| Patient Characteristics | 1998 | 2000 | P Value |
|---|---|---|---|
| Age (years, mean (SD)) | 75.3 (6.5) | 76.4 (6.0) | <.0001 |
| Female (%) | 60 | 59 | .71 |
| White (%) | 87 | 90 | .002 |
| High school graduate (%) | 78 | 81 | .006 |
| Low income (%<$20,000/y) | 42 | 36 | <.0001 |
| Married (%) | 58 | 57 | .55 |
| Health status† | |||
| Physical component scale (mean (SD)) | 40.1 (12.0) | 39.8 (11.9) | .38 |
| Mental component scale (mean (SD)) | 52.0 (9.7) | 52.1 (9.6) | .63 |
| Disease count | 2.2 (1.7) | 2.3 (1.6) | .08 |
| Number of prescription medications | 4.0 (2.7) | 4.4 (2.8) | .0002 |
| Monthly out-of-pocket medication costs (%) | |||
| $0 | 15 | 8 | <.0001 |
| $1-$24 | 41 | 33 | <.0001 |
| $25-$49 | 19 | 24 | .0003 |
| $50-99 | 13 | 17 | .0001 |
| $100-200 | 8.3 | 11.8 | .0002 |
| >$200 | 3.9 | 6.1 | .001 |
| Monthly premium costs ($, mean (SD)) | 46 (67) | 57 (75) | <.0001 |
| Medicare HMO (%) | 34 | 36 | .04 |
| Prescription drug coverage (%) | 71 | 73 | .19 |
| Number of outpatients visits in last 6 months (mean (SD)) | 3.6 (3.6) | 3.3 (3.2) | .005 |
| Inpatient stay in last 12 months (1 or more, %) | 31 | 19 | <.0001 |
| Physician-patient relationship quality‡ (mean (SD)) | 74.8 (16.4) | 73.7 (16.8) | .03 |
| Cost-related medication skipping rate (%) | 9.5 | 13.1 | <.0001 |
We applied sampling weights to all results to correct for difference in sampling probabilities across the strata. The observed sample size was 7,130 for 1998 and 4,630 for 2000.
Both the physical and mental component scales have a mean of 50 and an SD of 10. Higher scores indicate better health.
0 to 100 scale with 100 representing the best possible physician patient relationship quality.
Bivariate Relationships
Compared with those who reported no cost-related skipping, those who did skip had lower PCS (Table 2, 34.7 vs 40.7, P<.0001) and MCS (46.8 vs 52.5, P<.0001) scores, and were on more prescription medications (4.6 vs 4.0, P=.003). More skipping was reported by low- than high-income beneficiaries (15.2% vs 6.2%), and by those without any versus no prescription drug coverage (16.1% vs 6.8%, P<.0001). Just under 6% of beneficiaries with no out-of-pocket medication costs reported skipping compared with 19.6% costs of $50 or more and 28.2% of those with costs of >$200 (P<.0001). A similar gradient was seen for the physician-patient relationship quality score.
Table 2.
Bivariate Relationships with Cost-related Medication Skipping (1998 Data)*
| Patient characteristics | |||
|---|---|---|---|
| Continuous variables (mean) | Skipping | No skipping | P Value |
| Age (years) | 74.8 | 75.4 | .17 |
| Health status | |||
| Physical component scale | 34.7 | 40.7 | <.0001 |
| Mental component scale | 46.8 | 52.5 | <.0001 |
| Number of prescription medications | 4.6 | 4.0 | .003 |
| Disease count | 2.5 | 2.2 | .003 |
| Number of outpatients visits in last 6 months | 3.8 | 3.6 | .32 |
| Premium costs ($) | 49.7 | 46.0 | .42 |
| Categorical variables (% skipping) | Mean % Skipping | P Value |
|---|---|---|
| Female | .13 | |
| Male | 8.5 | |
| Female | 10.2 | |
| Race | .09 | |
| White | 9.1 | |
| Nonwhite black | 11.9 | |
| Income | <.0001 | |
| Low | 15.2 | |
| High | 6.2 | |
| High school graduate | .0003 | |
| Yes | 8.0 | |
| No | 13.8 | |
| Married | .036 | |
| Yes | 8.5 | |
| No | 10.9 | |
| HMO member | .54 | |
| Yes | 9.1 | |
| No | 9.7 | |
| Drug coverage | <.0001 | |
| Yes | 6.8 | |
| No | 16.1 | |
| Inpatient stay (1 or more) | .55 | |
| Yes | 9.9 | |
| No | 9.1 | |
| Monthly out-of-pocket medication costs | <.0001 | |
| $0 | 5.6 | |
| $1 to $24 | 5.7 | |
| $25 to $49 | 8.1 | |
| $50 to $99 | 16.0 | |
| $100 to $199 | 19.6 | |
| >$200 | 28.2 | |
| Physician-patient relationship quality (quartiles) | <.0001 | |
| 1 (highest quality) | 6.0 | |
| 2 | 6.6 | |
| 3 | 8.4 | |
| 4 | 14.7 |
We applied sampling weights to all results to correct for difference in sampling probabilities across the strata. The observed sample size was 7,130 for 1998
Multivariable Relationships in 1998 and 2000
Higher monthly medication costs in 1998 were associated with more cost-related skipping of medication and other treatments. Compared with those with no out-of-pocket costs, the ORs for skipping for those spending $50 to $99, $100 to $199, and $200 or more per month were 3.2, 4.0, and 6.1 (all P≤.0001, Table 3). Beneficiaries in the lowest quartile of the physician-patient relationship score had significantly higher odds of skipping (OR 2.2, P=.001) compared with those in the highest quartile. Low-income beneficiaries reported more skipping than high-income beneficiaries (OR 2.2, P<.0001). Beneficiaries lacking prescription medication coverage reported more skipping than those with insurance (OR 1.8, P<.0001). Older beneficiaries skipped less often than younger beneficiaries (OR for each 10-year increment 0.61, P<.0001). Finally, better health was associated with less cost-related skipping for both physical (OR 0.69 for each 10-point increment) and mental health (OR 0.67 for each 10-point increment).
Table 3.
Multivariable Correlates of Cost-related Medication Skipping in 1998 and 2000*
| 1998 | 2000 | P Value for Change§ | |||
|---|---|---|---|---|---|
| OR [95% CI] | P Value | OR [95% CI] | P Value | ||
| Monthly medication costs ($ per month) | <.0001 | ||||
| $0 | Reference group | Reference group | |||
| $1 to $24 | 1.3 [0.74, 2.3] | .34 | 1.5 [0.74, 3.1] | .26 | |
| $25to $49 | 1.6 [0.9, 2.8] | .11 | 4.1 [2.1, 8.3] | .0001 | |
| $50 to $99 | 3.2 [1.8, 5.7] | .0001 | 6.0 [3.0, 12] | <.0001 | |
| $100 to $199 | 4.0 [2.1, 7.4] | <.0001 | 11 [5.5, 24] | <.0001 | |
| $200 and greater | 6.1 [2.9, 12.9] | <.0001 | 16 [7.4, 35] | <.0001 | |
| Lowest quartile of physician-patient relationship quality† | 2.2 [1.4, 3.4] | .001 | 2.1 [1.4, 3.2] | .0003 | .007 |
| Low income | 2.2 [1.6, 3.0] | <.0001 | 1.4 [1.0, 2.0] | .04 | .96 |
| No prescription medication coverage | 1.8 [1.3, 2.4] | .0001 | 1.7 [1.3, 2.3] | .0001 | .89 |
| Age† | 0.61 [0.49, 0.76] | <.0001 | 0.54 [0.42, 0.69] | <.0001 | .38 |
| Physical component scale‡ | 0.69 [0.60, 0.79] | <.0001 | 0.77 [0.66, 0.89] | .0005 | .09 |
| Mental component scale‡ | 0.67 [0.58, 0.77] | <.0001 | 0.73 [0.64, 0.83] | <.0001 | .03 |
| HMO member | 1.0 [0.80, 1.3] | .84 | 1.5 [1.2, 2.0] | .0004 | .001 |
| Disease count | 0.94 [0.86, 1.02] | .12 | 0.99 [0.91, 1.1] | .83 | .16 |
| Number of prescriptions | 0.97 [0.91, 1.02] | .25 | 0.99 [0.92, 1.1] | .85 | .31 |
| Inpatient stay | 0.91 [0.65, 1.3] | .58 | 0.93 [0.63, 1.4] | .73 | .43 |
| Outpatient visits | 0.98 [0.89, 1.1] | .75 | 0.91 [0.81, 1.02] | .11 | .60 |
| Female | 1.0 [0.77, 1.3] | .96 | 0.89 [0.67, 1.2] | .42 | .38 |
| Caucasian race | 0.98 [0.67, 1.4] | .90 | 1.2 [0.82, 1.7] | .35 | .22 |
| High school education | 0.97 [0.91, 1.03] | .33 | 0.93 [0.89, 0.98] | .008 | .03 |
| Married | 1.04 [0.77, 1.4] | .79 | 0.76 [0.56, 1.03] | .08 | .50 |
We applied sampling weights to all results to correct for difference in sampling probabilities across the strata. The observed sample size was 7,130 for 1998 and 4,630 for 2000
Reference group is the top quartile of the physician-patient relationship score
The OR is the odds of reporting cost-related medication skipping for each 10-point improvement in physical or mental health, and each 10-year increment in age
P value for the change in the OR from 1998 to 2000, using seemingly unrelated regression method
OR, odds ratio; CI, confidence interval
The ORs for 5 variables in the model changed significantly between 1998 and 2000: out-of-pocket costs, physician-patient relationship quality, the mental component scale, HMO membership, and high school education. The largest changes were seen in the ORs associated with out-of-pocket medication costs. For those in Medicare HMOs, the OR increased from 1.0 to 1.5 (P<.0001 for the difference). We report in more detail on changes in physician-patient relationship quality elsewhere.25
Trends in Cost-related Skipping of Medications and Other Treatments
To understand which of the independent variables that we studied were associated with this increase in cost-related skipping, we examined changes in the aggregate impact of the variables whose ORs changed significantly between 1998 and 2000 (out-of-pocket costs, physician-patient relationship quality, the mental component scale, HMO membership, and high school education). The increase in out-of-pocket costs between 1998 and 2000 (see Table 1) combined with the increase in the OR associated with out-of-pocket costs for the same period (see Table 3) explained approximately two thirds of the increase in cost-related skipping. The remaining third was explained by the increase in the OR associated with belonging to a Medicare HMO.
Rates of cost-related skipping in fee-for-service and HMOs are compared in 1998 (see Fig. 1). In 1998, the rate of cost-related medication skipping was greater in HMOs than fee-for-service in each out-of-pocket cost category, but the only statistically significant difference was seen in the $25 to $49 per month category (P<.001). However, in 2000, there were statistically significant differences in the $1 to $24, $25 to $49, and $50 to $99 categories (all P<.001). The other variables for which the OR changed significantly between 1998 and 2000 (physician-patient relationship quality, MCS, and education) had a negligible impact on changes in skipping rates.
Figure 1.
Adjusted rates of cost-related medication skipping in fee-for-service and Medicare HMOs in 1998 (top) and 2000 (bottom). The *signifies P<.001for the difference between fee-for-service and Medicare HMO
DISCUSSION
There were 3 main findings from this work. First, cost-related skipping of medications and other treatments is relatively common, and increasing. Second, increases in out-of-pocket medication costs and HMO membership explained most of the increase in cost-related skipping between 1998 and 2000. Third, better physician-patient relationship quality is associated with less cost-related skipping.
The mean rates of cost-related skipping of medications and other treatments were 9.5% in 1998 and 13.1% in 2000. These average figures conceal strikingly high rates of skipping in high-risk subgroups. Using our models, the estimated skipping rate for a 65 year old with MCS and PCS of 40, no prescription drug coverage, out-of-pocket costs of >$50 per month, low income, and a poor physician-patient relationship was 81%. It is difficult to compare our cost-related skipping rates with those of other, contemporaneous studies of patients over 65 because of differences in item content and sampling, but our rates were similar to others. We previously reported data from a 2001 study in which cost-related mediation nonadherence rates varied from 7% to 41% depending on the survey item used and the patient subgroup assessed.13 Steinman et al. assessed cost-related medication skipping in 1995–1996 and found a rate of 8%,14 and Mojtabai and Olfson found a rate of 7% using data from 2000. 10 More importantly, this is the first study we are aware of that assessed cost-related underuse longitudinally, and we document a 38% 2-year increase.
Prescription drug costs rose at a rate that far exceeded the Consumer Price Index between 1998 and 2000,26–29 which probably explains why the strongest correlate of the increase in cost-related skipping between 1998 and 2000 was rising out-of-pocket drug costs. But, in addition, we observed an increase in odds of skipping for patients with out-of-pocket costs greater than $25. The aggregate impact of increased out-of-pocket costs on cost-related skipping is the product of these two factors. The increase in the OR for out-of-pocket costs may be because many of these patients have fixed incomes. Up to a certain point, they may pay for increases in out-of-pocket drug costs out of savings or other assets. But once a cost threshold is reached, drug costs may compete directly with other necessities like food and utilities.
The HMO finding was unexpected, and may be a selection effect. HMO members in this analysis had lower incomes than those in traditional Medicare ($3,072 less in 1998 and $3,876 less in 2000), and probably differed in other ways as well. They may have enrolled in an HMO because of the drug benefit. Changes in HMO prescription drug policies between 1998 and 2000—including fewer offering a pharmacy benefit, drug caps, use of formularies, and increasing copays30—may have resulted in increased cost-related skipping for low-income beneficiaries. Coverage arrangements for other treatments (e.g., physical therapy) may have increased in HMOs during these years, but any such changes would likely have been dwarfed in magnitude by changes in drug costs.30 Further studies of cost-related medication skipping and HMO membership are needed.
Recent data from several other studies suggest that physician-patient communication about prescription medication costs is suboptimal.31,32 Our findings, for the first time, directly link physician-patient relationship quality to cost-related skipping of medications and other treatments. Better physician-patient communication may help patients make more informed spending decisions or reveal lower cost medication options. Our findings suggest that physicians discuss cost-related underuse of medications and other therapies with all their patients.
There are several study limitations. First, we do not know whether our findings generalize to states where Medicare HMOs were less well established. Second, because vulnerable subgroups of seniors, such as minorities and those with low income, are underrepresented here because of higher rates of nonresponse and loss to follow-up, our results may understate rates of cost-related skipping. Third, self-selection of seniors into traditional Medicare versus HMOs may bias system comparisons if important differences between the populations are not captured by the study design and analytic methods. Fourth, self-reported medication skipping of medications and other therapies may underestimate actual skipping. Fifth, we could not separate rates of medication skipping from rates of skipping of other therapies. However, we believe that most of the skipping that we are capturing with the survey item we used is medication related. Over 90% of beneficiaries use prescription medications, whereas only 10% use outpatient therapy services,33 and out-of-pocket medication costs were a strong correlate of cost-related skipping.
As important as the new prescription drug benefit embodied by the Medicare Modernization Act may be for seniors, we show that cost-related skipping of medications and other treatments is associated with several different factors, including poverty and poor health. If a prescription drug plan requires significant cost sharing, certain vulnerable subgroups will almost certainly continue to experience relatively high cost-related medication skipping rates, particularly low-income seniors whose income or assets may not qualify for any low-income subsidies because their income or assets make them ineligible.13 An important new finding from this research is that better physician-patient relationships are independently associated with less cost-related skipping. We believe that physicians should initiate discussions about out-of-pocket costs, prescription drug coverage, and cost-related underuse of medications and other therapies with all of their patients. In some cases, it will be possible to substitute high-cost medications with equally effective, lower-cost alternatives.34
Acknowledgments
This research was supported by grant number R01 HS09622 from the Agency for Healthcare Research and Quality and the National Institute on Aging. The authors gratefully acknowledge the valuable comments of Tricia Neuman of the Kaiser Family Foundation and Barbara Cooper of the Commonwealth Fund on an earlier draft of this manuscript.
References
- 1.Myers LB, Midence K. Concepts and issues in adherence. In: Myers LB, Midence K, editors. Adherence to Treatment in Medical Conditions. Amsterdam: Harwood Academic Publishers; 1998. pp. 1–24. [Google Scholar]
- 2.Shumaker SA, Schron EB, Ockene JK, McBee WL, editors. The Handbook of Health Behavior Change. 2nd ed. New York: Springer Publishing Company, Inc.; 1998. [Google Scholar]
- 3.Haynes RB. Strategies to improve compliance with referrals, appointments, and prescribed medical regimens. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Baltimore, Md: The Johns Hopkins University Press; 1979. pp. 121–43. [Google Scholar]
- 4.Poisal JA, Murray L. Growing differences between Medicare beneficiaries with and without drug coverage. Health Aff (Millwood) 2001;20:74–85. doi: 10.1377/hlthaff.20.2.74. [DOI] [PubMed] [Google Scholar]
- 5.Stuart B, Grana J. Ability to pay and the decision to medicate. Med Care. 1998;36:202–11. doi: 10.1097/00005650-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Blustein J. Drug coverage and drug purchases by Medicare beneficiaries with hypertension. Health Aff (Millwood) 2000;19:219–30. doi: 10.1377/hlthaff.19.2.219. [DOI] [PubMed] [Google Scholar]
- 7.Adams AS, Soumerai SB, Ross-Degnan D. Use of antihypertensive drugs by Medicare enrollees: does type of drug coverage matter? Health Aff (Millwood) 2001;20:276–86. doi: 10.1377/hlthaff.20.1.276. [DOI] [PubMed] [Google Scholar]
- 8.Lillard LA, Rogowski J, Kington R. Insurance coverage for prescription drugs: effects on use and expenditures in the Medicare population. Med Care. 1999;37:926–36. doi: 10.1097/00005650-199909000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health & Human Services. Report to the President: Prescrition Drug Coverage, Spending, Utilization, and Prices. 2000. http://www.aspe.hhs.gov/health/reports/drugstudy.
- 10.Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff (Millwood) 2003;22:220–9. doi: 10.1377/hlthaff.22.4.220. [DOI] [PubMed] [Google Scholar]
- 11.Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42:626–34. doi: 10.1097/01.mlr.0000129352.36733.cc. [DOI] [PubMed] [Google Scholar]
- 12.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94:1782–7. doi: 10.2105/ajph.94.10.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: how well are states closing the gap. Health Aff (Millwood) 2002:W253–67. doi: 10.1377/hlthaff.w2.253. [DOI] [PubMed] [Google Scholar]
- 14.Steinman MA, Sands LP, Covinsky KE. Self-restriction of medications due to cost in seniors without prescription coverage. J Gen Intern Med. 2001;16:793–9. doi: 10.1111/j.1525-1497.2001.10412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safran DG, Wilson IB, Rogers WH, Montgomery JE, Chang H. Primary care quality in the Medicare Program: comparing the performance of Medicare health maintenance organizations and traditional fee-for-service medicare. Arch Intern Med. 2002;162:757–65. doi: 10.1001/archinte.162.7.757. [DOI] [PubMed] [Google Scholar]
- 16.Dillman DA. Mail and Telephone Surveys: the Total Design Method. New York, NY: John Wiley & Sons; 1978. [Google Scholar]
- 17.Aday LA, Andersen R. Development of Indices of Access to Medical Care. Ann Arbor, Mich: Health Administration Press; 1975. [Google Scholar]
- 18.Andersen RM. A Behavioral Model of Families' Use of Health Services, Research Series No. 25. Chicago, Ill: Center for Health Administration Studies, University of Chicago; 1968. [Google Scholar]
- 19.Safran DG, Kosinski M, Tarlov AR, et al. The primary care assessment survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Murphy J, Chang H, Montgomery JE, Rogers WH, Safran DG. The quality of physician–patient relationships. Patients' experiences 1996–1999. J Fam Pract. 2001;50:123–9. [PubMed] [Google Scholar]
- 21.National Center for Health Statistics. Current Estimates from the National Health Interview Survey. Washington, DC: U.S. Government; 1993. [Google Scholar]
- 22.McHorney CA, Ware JEJ, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Jones MP. Indicator and stratification methods for missing explanatory variables in multiple linear regression. J Am Stat Assoc. 1996;91:222–30. [Google Scholar]
- 24.Greene WH. Econometric Analysis 1993. New York, NY: Macmillan Publishing Company; 1993. [Google Scholar]
- 25.Safran DG. Defining the future of primary care: what can we learn from patients? Ann Intern Med. 2003;138:248–55. doi: 10.7326/0003-4819-138-3-200302040-00033. [DOI] [PubMed] [Google Scholar]
- 26.Report to the Congress: Selected Medicare Issues. Washington, DC: Medicare Payment Advisory Commission; 2000. [Google Scholar]
- 27.Pear R. 17 percent increase in prescription drug costs hit elderly hardest, study finds. The New York Times. June 27, 2002.
- 28.Strunk BC, Ginsburg PB, Gabel JR. Tracking health care costs. Health Aff (Millwood) 2002;(suppl):W39–50. doi: 10.1377/hlthaff.w1.39. [DOI] [PubMed] [Google Scholar]
- 29.Connolly C. Pharmaceutical spending continues stady increase: a few heavily advertised and high-priced “blockbuster” medications drive 17 percent increase. Washington Post. March 29, 2002:09.
- 30.Achman L, Gold M. Trends in Medicare+Choice: Benefits and Premiums, 1999–2002. New York, NY: The Commonwealth Fund; 2002. [PubMed] [Google Scholar]
- 31.Alexander GC, Casalino LP, Meltzer DO. Patient–physician communication about out-of-pocket costs. JAMA. 2003;290:953–8. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 32.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164:1749–55. doi: 10.1001/archinte.164.16.1749. [DOI] [PubMed] [Google Scholar]
- 33.Maxwell S, Baseggio C. Outpatient Therapy Services Under Medicare: Background and Policy Issues. Washington, DC: The Urban Institute; 2000. [Google Scholar]
- 34.Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) ALLHAT Collaborative Research Group. JAMA. 2002;288:2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]