Abstract
Context
Obesity is a fast-growing threat to public health in the U.S., but information on trends in professional advice to lose weight is limited.
Objective
We studied whether rising obesity prevalence in the U.S. was accompanied by an increasing trend in professional advice to lose weight among obese adults.
Design and Participants
We used the Behavioral Risk Factor Surveillance System, a cross-sectional prevalence study, from 1994 (n=10,705), 1996 (n=13,800), 1998 (n=18,816), and 2000 (n=26,454) to examine changes in advice reported by obese adults seen for primary care.
Measurements
Self-reported advice from a health care professional to lose weight.
Results
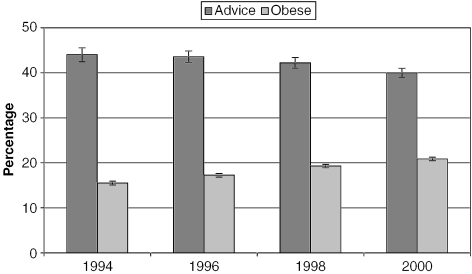
From 1994 to 2000, the proportion of obese persons receiving advice to lose weight fell from 44.0% to 40.0%. Among obese persons not graduating from high school, advice declined from 41.4% to 31.8%; and for those with annual household incomes below $25,000, advice dropped from 44.3% to 38.1%. In contrast, the prevalence of advice among obese persons with a college degree or in the highest income group remained relatively stable and high (>45%) over the study period.
Conclusions
Disparities in professional advice to lose weight associated with income and educational attainment increased from 1994 to 2000. There is a need for mechanisms that allow health care professionals to devote sufficient attention to weight control and to link with evidence-based weight loss interventions, especially those that target groups most at risk for obesity.
Keywords: physician behavior, health care delivery, obesity, weight management, socioeconomic status
Obesity is now recognized as a grave health problem for many Americans, with an adult prevalence of 19.8% in 2000 and 20.9% in 2001, estimated from a telephone survey.1 Poor nutrition and physical inactivity are leading actual causes of preventable deaths in the United States.2 Obesity contributes to serious illnesses such as hypertension,1,3 diabetes,1,3,4 breast cancer,5 asthma,1,6 gall bladder disease,3 as well as depression7,8 and poor health related quality of life (HRQL).9–12 Moreover, obesity is costly in terms of medical expenses,13 lost productivity in the workplace,14–17 and foregone earnings because of premature mortality.15
In spite of the growing obesity problem, half or more of obese patients in the United States do not report being counseled about weight loss by their physicians.18–23 Reported counseling from a health care professional about weight, diet, or exercise among overweight and obese adults is lower for some racial/ethnic minorities,23 persons with lower income24,25 or less education,20,21,24 younger persons,23,24 and men21,23 than their counterparts.
Surveys of physicians support this picture; physicians report that they often fail to counsel patients regarding weight,26 diet,27–29 or exercise,27,30 and often do not assess body mass during office visits.26 Patients are more likely to be counseled about health behaviors like diet and exercise if the visit is long31 or if other risk factors are present.27,31–33 Physicians cite many factors, including lack of time during office visits,27,28,30 inadequate training in preventive care,27,28 no reimbursement for treatment and prevention,28,34 and the belief that the advice would have little effect on patient behavior27–30,35 as prominent barriers to counseling. However, studies reveal that patients counseled regarding their weight or strategies for improving diet and exercise are substantially more likely to report that they are working on these areas,20,21,36,37 and may be more likely to lose weight.37,38 Finally, a review of randomized control trials indicates that coordination of weight loss efforts with a health professional may result in greater success among overweight or obese patients.39 The U.S. Preventive Services Task Force recently concluded that there is some evidence that high-intensity counseling about diet, exercise, or both in conjunction with behavioral interventions produces modest, sustained weight loss in adults who are obese.40
This study was designed to analyze recent trends in physician's advice to lose weight among obese adults, using data from the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System (BRFSS). Because obesity prevalence has risen during the past decade and the health implications of obesity have gained wider recognition,1,3 we hypothesized that the prevalence of health care professionals advising their obese patients about their weight might have increased as well.
METHODS
Sample and Subjects
This study examines all adult respondents determined to be obese by self-reported height and weight and who had at least one doctor visit for a routine checkup during the preceding 12 mo. Obesity is defined as having a body mass index (BMI) ≥30 kg/m2. Data from 1994 (n=10,705, 10.1% of BRFSS sample), 1996 (n=13,800, 11.3% of BRFSS sample), 1998 (n=18,816, 12.8% of BRFSS sample), and 2000 (n=26,454, 14.7% of BRFSS sample) were used to study trends since questions about weight loss were included in the core questionnaire in even years until 2000. Overall, 73.4 % of obese persons surveyed in these years reported a checkup visit during the prior year. The next year in which weight loss questions were included in the core questionnaire was 2003; however, a key selection item was dropped (“About how long has it been since you last visited a doctor for a routine checkup?”), and we were therefore unable to include 2003 data in the analysis.
In 1984, the CDC established BRFSS for monitoring health-risk behaviors.41 BRFSS collects data annually on health-related behaviors that are useful for planning, initiating, monitoring, and evaluating health promotion and disease-prevention programs. BRFSS is a state-based, random-digit-dialed telephone survey of the noninstitutionalized U.S. adult population aged 18 years and older. BRFSS is conducted in the 50 states as well as the District of Columbia, Guam, Puerto Rico, and the Virgin Islands. This study focuses on 49 states and the District of Columbia; a nonpublic use dataset obtained by written request from the CDC allowed us to determine rural/urban residence for all states but Alaska, which was therefore excluded from analyses. The median response rates were 69.9% in 1994, 63.1% in 1996, 59.2% in 1998, and 48.9% in 2000. The BRFSS is designed to monitor time trends and includes a poststratification weighting procedure to correct for nonresponse bias.42
The University of Washington Institutional Review Board approved this study.
Dependent Measure
Whether someone was advised to lose weight was determined through self-report. Respondents were asked, “In the past 12 months, has a doctor, nurse, or other health professional given you advice about your weight?” and possible responses included “Yes, lose weight,”“Yes, gain weight,”“Yes, maintain current weight,” and “No.” A dichotomous measure for being advised to lose weight versus no advice about weight was constructed, excluding the responses for gaining or maintaining weight. In any year, fewer than 2% of obese adults with a primary care visit reported being advised to maintain their weight, and fewer than one half of a percent reported being advised to gain weight.
Independent Measures
Survey year was the primary independent measure and is a nominal variable with one category for each year. Other measures included: race/ethnicity (non-Hispanic white, non-Hispanic African American, American Indian, Asian/Pacific Islander, Hispanic); sex; age (18 to 34, 35 to 49, 50 to 64, and 65 years or older); educational attainment (less than high school, high school graduate/equivalent with or without some college, college degree, or greater); annual household income (less than $25,000, $25,000 to $49,999, $50,000 to $74,999, $75,000 or greater, missing); and whether the respondent had been diagnosed with diabetes. Because Alaska was excluded from these analyses, the term American Indian is used in lieu of American Indian/Alaska Native, although some BRFFS respondents residing outside of Alaska may be Alaska Natives. Factors controlled for in multivariate analyses but not presented were self-reported health status (excellent, very good, good, fair, poor), smoking status (current smoker, former smoker, never smoked), whether the respondent had health insurance, and whether the respondent lived in a rural or an urban county. Models predicting receipt of weight control counseling were based on the Behavioral Model of Andersen and colleagues,43,44 and included predisposing (age, gender, race/ethnicity, education), enabling (health insurance, income), need (health status, diabetes, smoking), and environmental (rural/urban residence) factors.
Analytical Plan
Estimates were weighted using the BRFSS poststratification weighting formula, which includes the sex, age, and race/ethnicity distributions of the population in each state. Significance tests were calculated using SUDAAN software,45 which adjusts the standard errors to account for the complex sampling design of the BRFSS. Logistic regression analyses calculating the odds of being advised to lose weight were restricted to obese respondents who reported having had a health care checkup within the past 12 months. Body mass index was derived from height and weight, and obesity was defined as having a BMI ≥30 kg/m2. Trend analyses presenting the interaction of survey year with each covariate are adjusted for all other covariates. To facilitate interpretation of logistic regression results, predicted percentages (i.e., marginal effects) are presented.46
RESULTS
In Table 1, we present unadjusted findings for 2000, the most recent year of data. Fewer than half of obese adults having a checkup in the previous year reported being advised to lose weight by a health care professional. Age was strongly associated with physician advice to lose weight, peaking with the 50 to 64-year-old group; advice to lose weight was nearly as low for those 65 and older as for the youngest group. Greater educational attainment and household income were both positively associated with reported health care professional advice. Those with a college degree were much more likely to be advised to lose weight than those without a high school diploma. There was no difference in reported advice to lose weight for those in the bottom three income categories, but advice was higher for those earning at least $75,000 per year. Diabetics were far more likely than nondiabetics to be advised to lose weight and they had the highest prevalence of any group.
Table 1.
Actual Percent of Obese Adults Advised to Lose Weight (2000)
| Factor | Number of Respondents | % (SE) |
|---|---|---|
| Overall | 25,458 | 41.0 (0.5) |
| Race | ||
| White | 18,902 | 41.0 (0.6) |
| African American | 3,535 | 42.8 (1.3) |
| Asian/Pacific Islander | 218 | 51.1 (7.6) |
| American Indian | 674 | 38.0 (3.9) |
| Hispanic | 1,789 | 38.5 (2.2) |
| Gender | ||
| Male | 9,822 | 40.8 (0.9) |
| Female | 15,636 | 41.3 (0.7) |
| Age | ||
| 18 to34 | 4,800 | 30.9 (1.1)† |
| 35 to 49 | 8,203 | 43.3 (1.0) |
| 50 to 64 | 7,499 | 49.4 (1.0) |
| 65+ | 4,913 | 36.1 (1.2) |
| Education | ||
| <high school | 3,928 | 36.2 (1.5)† |
| High school | 15,909 | 41.2 (0.7) |
| College degree | 5,583 | 44.5 (1.1) |
| Household income | ||
| <25K | 8,454 | 40.5 (1.0)* |
| ≥25K, <50K | 7,955 | 40.6 (0.9) |
| ≥50K, <75K | 3,352 | 40.2 (1.4) |
| 75K+ | 2,664 | 46.1 (1.6) |
| Missing | 3,033 | 39.4 (1.5) |
| Diabetic status | ||
| Yes | 4,124 | 56.5 (1.6)† |
| No | 21,285 | 38.0 (0.6) |
P<.05
p><.001.
Table 2 shows adjusted trends in professional advice to lose weight for obese adults between 1994 and 2000. Overall, there was a significant decline in advice over the period. As shown graphically in Figure 1, this occurred while the prevalence of obesity among adults with a checkup during the prior 12 months increased over the same period (see the Appendix for adjusted estimates of obesity prevalence, available online). There are few clear patterns by race, although a trend test showed a significant decline in advice for obese whites that mirrors the overall decline. Prevalence of advice was higher for obese women compared with obese men in 1994; however, reporting advice to lose weight declined nearly twice as much for women as for men. A trend test for women was highly significant. All age groups except 35 to 49 year olds showed a significant decline in being advised to lose weight over the study period, and obese persons 65 and older experienced the largest and most significant decline of all age groups.
Table 2.
Trend in Adjusted Percent of Obese Adults Advised to Lose Weight (1994–2000)
| Factor* | 1994 | 1996 | 1998 | 2000 |
|---|---|---|---|---|
| % (SE) | % (SE) | % (SE) | % (SE) | |
| Overall | 44.0 (0.8) | 43.6 (0.7) | 42.2 (0.6) | 40.0 (0.5)§ |
| Race | ||||
| White | 44.0 (0.9) | 42.7 (0.7) | 41.8 (0.7) | 39.8 (0.6)§ |
| African American | 45.0 (1.7) | 47.0 (1.7) | 41.4 (1.4) | 42.1 (1.3) |
| Asian/Pacific Islander | 45.2 (10.8) | 33.1 (7.1) | 35.4 (8.6) | 49.6 (6.8) |
| American Indian | 47.6 (6.3) | 40.6 (6.0) | 42.4 (6.9) | 37.3 (4.5) |
| Hispanic | 41.2 (3.2) | 45.8 (2.8) | 46.5 (2.5) | 38.0 (2.4) |
| Gender | ||||
| Male | 41.6 (1.2) | 41.2 (1.0) | 41.2 (0.9) | 38.7 (0.9) |
| Female | 46.0 (1.0) | 45.4 (0.8) | 43.1 (0.8) | 41.0 (0.7)§ |
| Age | ||||
| 18 to 34 | 39.7 (1.7) | 37.8 (1.5) | 38.0 (1.3) | 34.8 (1.2)† |
| 35 to 49 | 44.9 (1.4) | 46.8 (1.2) | 45.2 (1.1) | 43.4 (1.1) |
| 50 to 64 | 48.5 (1.5) | 48.8 (1.2) | 46.6 (1.1) | 45.3 (1.0)† |
| 65+ | 40.8 (1.7) | 37.1 (1.4) | 35.6 (1.3) | 32.4 (1.2)§ |
| Education | ||||
| <High school | 41.4 (1.7) | 40.7 (1.5) | 39.6 (1.5) | 31.8 (1.5)§ |
| High school | 44.0 (1.0) | 42.7 (0.8) | 41.3 (0.7) | 40.8 (0.7)‡ |
| College degree | 45.7 (1.8) | 49.0 (1.5) | 47.7 (1.3) | 44.8 (1.1) |
| Household income | ||||
| <25K | 44.3 (1.1) | 43.2 (1.1) | 41.3 (1.0) | 38.1 (1.1)§ |
| ≥25K, <50K | 44.3 (1.5) | 45.8 (1.2) | 42.2 (1.0) | 41.1 (0.9)‡ |
| ≥50K, <75K | 47.1 (2.4) | 44.3 (1.9) | 45.1 (1.6) | 40.3 (1.4)‡ |
| 75K+ | 45.4 (3.6) | 45.9 (2.4) | 47.2 (2.1) | 45.2 (1.6) |
| Missing | 36.5 (2.3) | 35.8 (1.8) | 38.1 (1.7) | 37.7 (1.5) |
| Diabetic status | ||||
| Yes | 60.8 (2.3) | 59.6 (1.8) | 56.2 (1.6) | 51.5 (1.7)§ |
| No | 41.2 (0.8) | 40.9 (0.7) | 39.8 (0.6) | 38.0 (0.6)§ |
Variables included in analyses but not presented were general health, smoking status, health coverage, and rural/urban residence.
Test for time trend:
P<.05
P<.01
P<.001.
FIGURE 1.
Overall trends in obesity prevalence and professional advice to lose weight for obese persons. Y-axis label: “percentage, 95% confidence interval.” Label for dark gray bars: “advice.” Label for light gray bars: “Obese.”“Source: See Table 2 and Appendix.”
Not only was advice to lose weight less frequent for those with lower educational attainment, it declined substantially over time, while there was little overall change for those with at least a college degree. The gap in counseling between college graduates and those who did not graduate high school tripled between 1994 and 2000. The substantially higher probability of being advised to lose weight was paired with lower obesity prevalence for the most highly educated, while for the least educated group, the declining probability of advice from 1994 to 2000 accompanied significantly higher obesity prevalence. Household income revealed a pattern similar to that of educational attainment. Obese adults with less than $25,000/year in household income experienced a significant decline in professional advice to lose weight, while those with incomes of at least $75,000/year experienced no significant net change, resulting in a growing gap in advice between high- and low-income groups between 1994 and 2000. Those with incomes of at least $75,000 experienced both lower obesity prevalence and higher prevalence of advice to lose weight compared with those in the lowest income group.
Reported advice to lose weight was substantially higher in every year for obese diabetics compared with nondiabetics; however, the decline in counseling over time was much larger for diabetics, despite their more rapid increase in prevalence of obesity between 1994 and 2000.
DISCUSSION
Advice from health care professionals to lose weight should be uniformly high for those with a serious weight problem, regardless of the proportion of obese persons in the population or the sociodemographic characteristics of the patient. We expected that as obesity prevalence rose in the population, coupled with growing awareness of its associated health problems, providers would devote more attention to weight loss advice, but in fact the opposite occurred. As prevalence of obesity increased, obese adults with a recent primary care visit were less likely to report being advised to lose weight.
Results of our adjusted analyses for 2000 were consistent with findings from other national studies using data from the same period,18,24 in particular, that lower rates of professional advice to lose weight were associated with youth, lower income, less education, and being male. Trend analyses showed that receipt of advice to lose weight was low for all subgroups in all years. Only diabetics exceeded an adjusted advice prevalence of 50% in any year; the only other groups to approach 50% were Asian and Pacific Islanders, those aged 50 to 64, and the college educated. However, the evidence of a growing divide in advice to lose weight between the richest and poorest and between the most and the least educated is cause for concern, particularly when obese persons in groups with the greatest obesity burdens are also the least likely to receive any professional intervention, even if they receive routine care. Moreover, the low and rapidly falling prevalence of advice to obese elderly persons, who are most at risk from chronic diseases, is an issue that merits urgent attention. Finally, the significant decline in advice reported by obese diabetics is worrisome, since weight control is a key factor in managing this chronic illness.
These findings are subject to several limitations. BRFSS does not sample persons living in institutions or persons living in households without a telephone. Persons living in households without a telephone may be less likely to receive professional advice regarding weight or regular health care and be more likely to be obese, as having a telephone reflects socioeconomic status. Prevalence estimates and trend data could have been affected by low response rates; however, BRFSS uses poststratification weights to minimize this problem.42 The race/ethnicity groupings available in BRFSS data do not allow any important differences between subgroups within these broad categories to be revealed. Another limitation is the use of self-reported, rather than measured, height and weight for determining obesity, the misreporting of which has been shown to be influenced by age, gender, and actual weight.47–49 However, there is no suggestion that this tendency has changed over time, and the tendency of individuals to underreport their weight49 increases confidence that those classified as obese by the BRFSS would be so classified through objective assessment. Finally, we had to rely on respondent self-report of professional advice to lose weight and receipt of a checkup within the previous year, both of which may suffer from imprecise recall or a tendency to report more socially desirable answers. Patients counseled about nutrition and exercise are more likely to recall the advice if the advice is of a relatively long duration or relevant to a current health problem.50 However, the possibility that advice recall may be biased simply underscores the likelihood that those who cannot remember being advised are no different in effect from those who were not advised at all, in that neither group received adequate counseling to be effective for weight loss. Also, there is no evidence that any such bias has changed over time.
This study is unique and important because it demonstrates that not only is there inadequate attention to weight loss for obese patients within a health care setting,18–23,26–30 but there is actually a downward trend in weight loss advice at the same time that the prevalence of obesity is increasing. The rapid increase in obesity prevalence may contribute to physicians' feeling that their efforts are fruitless. Moreover, the “fen-phen” controversy in the 1990s may have discouraged physicians from counseling their obese patients about weight loss, particularly if they felt that counseling without medications was ineffective, although this tendency might be countered by the growing popularity of bariatric surgery as a solution for the most obese patients.
The demand for preventive care services from physicians is so high as to preclude provision of all needed services in many circumstances, and new services are continually being recommended.51 In addition, counseling for diet, which is ranked by the U.S. Preventive Services Task Force (USPSTF) as less strongly evidence based than counseling for tobacco cessation or injury prevention,52 is also estimated to require the most time of any USPSTF-recommended counseling service.51 Finally, persons of low socioeconomic status have a greater burden of disease53–55 and are more prone to depression,56 which might leave little time during a routine visit to discuss nutrition, exercise, and weight loss. More study is needed to determine whether the link between low socioeconomic status and falling prevalence of reporting advice from a health care professional may be related to time pressure from increased preventive care demands, shifting professional beliefs about the efficacy of counseling for these individuals, developments in surgical and pharmaceutical options, or even to changes in the settings in which these persons seek care.
Studies have shown that professional advice and follow-up with obese patients influence their motivation to make changes in diet and exercise and may promote successful weight loss.20,21,36–40 There is a need for reimbursement mechanisms that allow providers to give their patients sufficient weight reduction counseling and that link this counseling with reimbursement for intensive, evidence-based, behavioral interventions to lose weight.28,34 Also, training in nutrition and exercise guidelines would give physicians a foundation for and perhaps a greater disposition toward addressing these problems with patients. Finally, given the difficulties in changing physician behavior, programs need to be developed that specifically target groups that are unlikely to be counseled regarding diet and exercise, and yet are at high risk for obesity or obesity-related chronic illnesses.
Acknowledgments
This University of Washington Rural Health Research Center study was funded by the Federal Office of Rural Health Policy, Health Resources and Services Administration, Department of Health and Human Services (Cooperative Agreement #U1CRH00035-03).
REFERENCES
- 1.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 2.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270:2207–12. [PubMed] [Google Scholar]
- 3.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 4.Hahn RA, Heath GW, Chang MH. Cardiovascular disease risk factors and preventive practices among adults—United States, 1994: a behavioral risk factor atlas. Behavioral Risk Factor Surveillance System State Coordinators. MMWR CDC Surveill Summ. 1998;47:35–69. [PubMed] [Google Scholar]
- 5.Hu FB. Overweight and obesity in women: health risks and consequences. J Women's Health (Larchmt) 2003;12:163–72. doi: 10.1089/154099903321576565. [DOI] [PubMed] [Google Scholar]
- 6.Camargo CA, Jr, Weiss ST, Zhang S, et al. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–8. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 7.Dixon JB, Dixon ME, O'Brien PE. Depression in association with severe obesity: changes with weight loss. Arch Intern Med. 2003;163:2058–65. doi: 10.1001/archinte.163.17.2058. [DOI] [PubMed] [Google Scholar]
- 8.Palinkas LA, Wingard DL, Barrett-Connor E. Depressive symptoms in overweight and obese older adults: a test of the “jolly fat” hypothesis. J Psychosom Res. 1996;40:59–66. doi: 10.1016/0022-3999(95)00542-0. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan MB, Sullivan LG, Kral JG. Quality of life assessment in obesity: physical, psychological, and social function. Gastroenterol Clin North Am. 1987;16:433–42. [PubMed] [Google Scholar]
- 10.Fontaine KR, Cheskin LJ, Barofsky I. Health-related quality of life in obese persons seeking treatment. J Fam Pract. 1996;43:265–70. [PubMed] [Google Scholar]
- 11.Fontaine KR, Barofsky I, Andersen RE, et al. Impact of weight loss on health-related quality of life. Qual Life Res. 1999;8:275–7. doi: 10.1023/a:1008835602894. [DOI] [PubMed] [Google Scholar]
- 12.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev. 2001;2:173–82. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- 13.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff (Millwood) 2003;(>suppl):W3-219–26. doi: 10.1377/hlthaff.w3.219. [DOI] [PubMed] [Google Scholar]
- 14.Thompson D, Edelsberg J, Kinsey KL, et al. Estimated economic costs of obesity to U. S. business. Am J Health Promot. 1998;13:120–7. doi: 10.4278/0890-1171-13.2.120. [DOI] [PubMed] [Google Scholar]
- 15.Colditz GA. Economic costs of obesity and inactivity. Med Sci Sports Exerc. 1999;31:S663–7. doi: 10.1097/00005768-199911001-00026. [DOI] [PubMed] [Google Scholar]
- 16.Burton WN, Chen CY, Schultz AB, et al. The costs of body mass index levels in an employed population. Stat Bull Metrop Insur Co. 1999;80:8–14. [PubMed] [Google Scholar]
- 17.Bungum T, Satterwhite M, Jackson AW, et al. The relationship of body mass index, medical costs, and job absenteeism. Am J Health Behav. 2003;27:456–62. doi: 10.5993/ajhb.27.4.17. [DOI] [PubMed] [Google Scholar]
- 18.Mokdad AH, Bowman BA, Ford ES, et al. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 19.Potter MB, Vu JD, Croughan-Minihane M. Weight management: what patients want from their primary care physicians. J Fam Pract. 2001;50:513–8. [PubMed] [Google Scholar]
- 20.Sciamanna CN, Tate DF, Lang W, et al. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160:2334–9. doi: 10.1001/archinte.160.15.2334. [DOI] [PubMed] [Google Scholar]
- 21.Galuska DA, Will JC, Serdula MK, et al. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 22.Nawaz H, Adams ML, Katz DL. Weight loss counseling by health care providers. Am J Public Health. 1999;89:764–7. doi: 10.2105/ajph.89.5.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman C, Brownson RC, Peterson DE, et al. Physician advice to reduce chronic disease risk factors. Am J Prev Med. 1994;10:367–71. [PubMed] [Google Scholar]
- 24.Wee CC, McCarthy EP, Davis RB, et al. Physician counseling about exercise. JAMA. 1999;282:1583–8. doi: 10.1001/jama.282.16.1583. [DOI] [PubMed] [Google Scholar]
- 25.Taira DA, Safran DG, Seto TB, et al. The relationship between patient income and physician discussion of health risk behaviors. JAMA. 1997;278:1412–7. [PubMed] [Google Scholar]
- 26.Stafford RS, Farhat JH, Misra B, et al. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9:631–8. doi: 10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 27.Tsui JI, Dodson K, Jacobson TA. Cardiovascular disease prevention counseling in residency: resident and attending physician attitudes and practices. J Natl Med Assoc. 2004;96:1080–3. 1088–91. [PMC free article] [PubMed] [Google Scholar]
- 28.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24:546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 29.Kottke TE, Foels JK, Hill C, et al. Nutrition counseling in private practice: attitudes and activities of family physicians. Prev Med. 1984;13:219–25. doi: 10.1016/0091-7435(84)90053-7. [DOI] [PubMed] [Google Scholar]
- 30.Hiddink GJ, Hautvast JG, van Woerkum CM, et al. Nutrition guidance by primary-care physicians: perceived barriers and low involvement. Eur J Clin Nutr. 1995;49:842–51. [PubMed] [Google Scholar]
- 31.Eaton CB, Goodwin MA, Stange KC. Direct observation of nutrition counseling in community family practice. Am J Prev Med. 2002;23:174–9. doi: 10.1016/s0749-3797(02)00494-4. [DOI] [PubMed] [Google Scholar]
- 32.Podl TR, Goodwin MA, Kikano GE, et al. Direct observation of exercise counseling in community family practice. Am J Prev Med. 1999;17:207–10. doi: 10.1016/s0749-3797(99)00074-4. [DOI] [PubMed] [Google Scholar]
- 33.Silagy C, Muir J, Coulter A, et al. Lifestyle advice in general practice: rates recalled by patients. BMJ. 1992;305:871–4. doi: 10.1136/bmj.305.6858.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jackson Y, Dietz WH, Sanders C, et al. Summary of the 2000 Surgeon General's listening session: toward a national action plan on overweight and obesity. Obes Res. 2002;10:1299–305. doi: 10.1038/oby.2002.176. [DOI] [PubMed] [Google Scholar]
- 35.Sherman SE, Hershman WY. Exercise counseling: how do general internists do? J Gen Intern Med. 1993;8:243–8. doi: 10.1007/BF02600089. [DOI] [PubMed] [Google Scholar]
- 36.Mehrotra C, Naimi TS, Serdula M, et al. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med. 2004;27:16–21. doi: 10.1016/j.amepre.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 37.Nawaz H, Adams ML, Katz DL. Physician–patient interactions regarding diet, exercise, and smoking. Prev Med. 2000;31:652–7. doi: 10.1006/pmed.2000.0760. [DOI] [PubMed] [Google Scholar]
- 38.Bowerman S, Bellman M, Saltsman P, et al. Implementation of a primary care physician network obesity management program. Obes Res. 2001;9(Suppl 4):321S–325S. doi: 10.1038/oby.2001.137. [DOI] [PubMed] [Google Scholar]
- 39.Blackburn GL. Comparison of medically supervised and unsupervised approaches to weight loss and control. Ann Intern Med. 1993;119:714–8. doi: 10.7326/0003-4819-119-7_part_2-199310011-00017. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139:157. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 41.Marks JS, Hogelin GC, Gentry EM, et al. The behavioral risk factor surveys: I. State-specific prevalence estimates of behavioral risk factors. Am J Prev Med. 1998;1:1–8. [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Overview: BRFSS 2000, 2000. Available at http://www.cdc.govAccessed June 2, 2005.
- 43.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51:95–124. [PubMed] [Google Scholar]
- 44.Phillips KA, Morrison KR, Andersen R, et al. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–96. [PMC free article] [PubMed] [Google Scholar]
- 45.SUDAAN: Professional Software for SUrvey DAta ANalysis. Research Triangle Park, NC: Research Triangle Institute; 2001. [Google Scholar]
- 46.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–9. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 47.Villanueva EV. The validity of self-reported weight in US adults: a population based cross-sectional study. BMC Public Health. 1 doi: 10.1186/1471-2458-1-11. 11. E-pub 2001 November 6, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. quiz 35–6. [DOI] [PubMed] [Google Scholar]
- 49.Palta M, Prineas RJ, Berman R, et al. Comparison of self-reported and measured height and weight. Am J Epidemiol. 1982;115:223–30. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- 50.Flocke SA, Stange KC. Direct observation and patient recall of health behavior advice. Prev Med. 2004;38:343–9. doi: 10.1016/j.ypmed.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 51.Yarnall KS, Pollak KI, Ostbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.U.S. Preventive Services Task Force. Behavioral counseling in primary care to promote a healthy diet: recommendations and rationale. Am J Prev Med. 2003;24:93–100. doi: 10.1016/s0749-3797(02)00581-0. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention: Indicators for chronic disease surveillance. MMWR Recomm Rep. 2004;53:1–6. [PubMed] [Google Scholar]
- 54.Fein O. The influence of social class on health status: American and British research on health inequalities. J Gen Intern Med. 1995;10:577–86. doi: 10.1007/BF02640369. [DOI] [PubMed] [Google Scholar]
- 55.Adler NE, Boyce WT, Chesney MA, et al. Socioeconomic inequalities in health. No easy solution. JAMA. 1993;269:3140–5. [PubMed] [Google Scholar]
- 56.Taylor RR, Jason LA, Jahn SC. Chronic fatigue and sociodemographic characteristics as predictors of psychiatric disorders in a community-based sample. Psychosom Med. 2003;65:896–901. doi: 10.1097/01.psy.0000088580.28749.7f. [DOI] [PubMed] [Google Scholar]