Abstract
Background
In response to proposed federal legislation, the Accreditation Council for Graduate Medical Education limited resident work-hours in July 2003. The cost may be substantial but, if successful, the reform might lower preventable adverse event costs in hospital and after discharge.
Objectives
This study sought to estimate the reform's net cost in 2001 dollars, and to determine the reduction in preventable adverse events needed to make reform cost neutral from teaching hospital and societal perspectives.
Design
Cost analysis using published literature and data. Net costs were determined for 4 reform strategies and over a range of potential effects on preventable adverse events.
Results
Nationwide, transferring excess work to task-tailored substitutes (the lowest-level providers appropriate for noneducational tasks) would cost $673 million; mid-level providers would cost $1.1 billion. Reform strategies promoting adverse events would increase net teaching hospital and societal costs as well as mortality. If task-tailored substitutes decrease events by 5.1% or mid-level providers decrease them by 8.5%, reform would be cost neutral for society. Events must fall by 18.5% and 30.9%, respectively, to be cost neutral for teaching hospitals.
Conclusions
Because most preventable adverse event costs occur after discharge, a modest decline (5.1% to 8.5%) in them might make residency work-hours reform cost neutral for society but only a much larger drop (18.5% to 30.9%) would make it cost neutral for teaching hospitals, unless additional funds are allocated. Future research should evaluate which reform approaches prevent adverse events and at what cost.
Keywords: graduate medical education (GME), decision analysis, injury prevention, quality/performance improvement, accreditation, work-hours
As of July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) strictly limits work-hours for trainees in accredited graduate medical education programs.1 Although the ACGME has had duty-hour standards for many years, recent events brought resident fatigue and patient safety to the fore nationally and seemingly prompted this reform.2–4
Interest in resident work-hours arose in New York State after a 1984 death in a teaching hospital. Following a grand jury investigation and an Ad Hoc Advisory Committee review, New York limited resident work-hours in July 1989.2 Surprise inspectors revealed noncompliance at 12 hospitals in 1998, prompting the State to impose fines.5
Also, during the late 1990s, the media exposed several egregious medical errors, increasing public interest in patient safety.6 The Institute of Medicine report To Err Is Human ascribed 44,000 to 98,000 deaths per year to preventable adverse events in hospitals,7 garnering further attention.6 Federal policymakers responded by allocating funds for patient safety research8 and introducing legislation.9
Within this context, in April 2001, the Occupational Safety and Health Administration received a petition arguing that excessive work-hours endanger residents as well as patients and that regulators should intervene.10 Seven months later, legislators in the House of Representatives introduced the Patient and Physician Safety and Protection Act of 2001, proposing federal work-hour limits.11 Attempting to forestall its passage,3 the ACGME announced the current reform in June 2002.4,12 Senators and representatives reintroduced but did not pass the legislation in 2003.13,14
The ACGME and federal reforms are quite similar: both restrict residents to 80-hour work-weeks, limit shifts to 24 hour plus handoffs, limit in-hospital call to every third night, and provide one day off in seven. The ACGME, however, averages some limits over 4 weeks and allows 88-hour work-weeks for certain programs. The legislation allots less time for handoffs but requires that quality of care be maintained, and it adds 1 weekend off per month. Noncompliance leads to fines under the legislation but loss of accreditation under the ACGME reform12–14; Medicare requires accreditation for graduate medical education support.3
One key difference is that the legislation offered funding.12–14 Arguably, policymakers should weigh the costs and benefits of patient safety reforms as they do for other health care policies, i.e., via cost-utility analyses. In patient safety, however, cost implications differ for the society and hospitals: a reform that is costly for hospitals could be cost neutral or even cost saving for society because most economic effects of preventable adverse events occur after discharge.15 Therefore, policymakers should consider net costs from hospital and societal perspectives as well as the nonmonetary benefits that the society accrues when morbidity and mortality are averted. If a reform is cost saving or cost effective from a societal perspective but cost increasing from a hospital perspective, allocation of government funds may be justifiable.
Under residency work-hours reform, ACGME-accredited hospitals (“teaching hospitals”) will incur personnel costs if they transfer excess resident work to substitute providers, often promoted as the preferred strategy.16–20 To date, such costs appear unpublished. Savings would also occur if reform reduces preventable adverse events (“events”), which generate substantial costs in hospital15,21 and greater ones after discharge.15 For the current analysis, our objective was to determine the decline in events needed to make reform cost neutral for teaching hospitals and for society. We also considered mortality but available data precluded cost-utility analysis.
METHODS
Overview
Pursuant to these objectives, we estimated net reform costs nationwide for the year 2001, considering 4 reform strategies from teaching-hospital and societal perspectives. To calculate net costs, we summed personnel costs because of reform and costs because of hypothetical changes in events. When net costs were zero, reform was cost neutral. The teaching-hospital perspective included costs incurred by teaching hospitals nationwide, meaning personnel costs plus inpatient event costs. The societal perspective included these costs plus additional costs incurred by teaching-hospital patients nationwide, meaning post-discharge event costs.
Decision Models
Four decision models incorporated 4 strategies for limiting resident work-hours to 80 per week, transferring excess work: (1) to attending physicians, (2) to mid-level providers (nurse practitioners and physician assistants), (3) to task-tailored substitutes (the lowest-level providers appropriate for noneducational tasks), and (4) among existing residents.
Data Sources and Assumptions
We used published literature and data, searching MEDLINE and references in published articles, reports, and bibliographies.22–26 We defined “resident” as the ACGME does: a physician at any level of graduate medical education in an ACGME-accredited program.27
To estimate personnel costs, we determined baseline resident work-hours, considered which providers might perform resident tasks, and obtained wages and benefits for these providers. We assumed the following: an 80-hour work-week would make other reform features possible at no additional cost; reform would not affect length of stay, test ordering, or other hospitalization cost determinants; residents and substitutes work at the same speed; residents work 49 weeks per year; and enforcement costs would be negligible.
To ascertain baseline work-hours, we searched MEDLINE (work-hours, work-hour, duty hours, resident* reform) and contacted J. Faerberg (Director, Graduate Medical Education Track, Association of American Medical Colleges (AAMC), personal communication, January 22, 2004). The 1998 New York State inspection provided the only published data addressing multiple specialties, teaching hospitals, and class years. After interviewing residents, reviewing schedules, and examining hospital records, inspectors concluded that 37% of 391 residents worked over 85 and 20% worked over 95 hours per week.5 Extrapolating to 96,976 residents in ACGME-accredited programs in 2001,28 we assumed baseline work-hours of 100 per week for 20% of residents and 90 per week for 17%. Excess work equaled baseline work-hours minus 80. We ignored residents working under 90 per week.
Although attending physicians might assume the excess work, many resident tasks are performed equally well by nonphysicians.29–33 Mid-level providers represent prototypical resident substitutes, being used by half of New York State surgery programs after 198916 and incorporated into a 1994 proposal to eliminate 23,000 specialty residency positions nationwide.32 Nurses and ancillary providers could perform 10% to 12% of medical and surgical resident tasks.29–31,33 One study determined that nursing aides could assume 6.1% of Internal Medicine resident work-hours, laboratory technicians 1.2%, nurses 4.5%, and mid-level providers 7.4%.29
We incorporated these considerations in the 4 decision models, surmising that excess work from multiple residents would naturally distribute among substitutes within each hospital. For task-tailored substitution, we extrapolated the Internal Medicine model to all specialties.29 According to the Bureau of Labor Statistics, in 2001, hourly wages were as follows: nursing aides $9.34, laboratory technicians $14.52, licensed vocational nurses $15.14, mid-level providers $30.00, and physicians $60.1434,35; benefits were 37.8% of wages.36 We assumed that shifting excess work among existing residents would not affect the cost of employing them.
To estimate event incidence, mortality, and costs, we extrapolated from a prior study that found that preventable adverse events occurred during 1.9% of hospital admissions and that 6.9% of the events were fatal. Those authors estimated incremental health care costs, lost wages, and lost household production attributable to each event, projecting across all Utah and Colorado hospitals in 1996.15
Because cost of living and wages are higher nationally, we applied geographic inflation factors. Using 1996 Census Bureau data37 and published cost-of-living indices,38 we created population-weighted cost-of-living indices, yielding a factor of 1.045 for medical costs. Using 1997 mean wages from the Bureau of Labor Statistics (1996 was unavailable) yielded a factor of 1.075 for lost wages and household production.39
For temporal inflation in medical costs, Consumer Price Index components40 produced the following inflation factors: hospital and nursing home care 1.255, physician care 1.172, rehabilitation and home health care 1.141, and drugs and equipment 1.177. Although health care consumption in the U.S. also rose between 1996 and 2001, we ignored this. The Employment Cost Index yielded an inflation factor of 1.197 for lost wages and household production.41,42
For the teaching-hospital perspective, inpatient event costs included hospital and physician costs nationwide. Malpractice costs were ignored. For the societal perspective, event costs included inpatient event costs plus outpatient medical care, lost wages, and lost household production nationwide. Teaching hospitals had 15,490,520 admissions in 2001.43
Surmising that reform might affect event rates but not severity or costs, we examined 5 hypothetical changes in event rates under reform: +20%,+10%, 0%, −10%, and −20%.
CALCULATIONS
From these data and assumptions, we calculated personnel costs, event costs, and net reform costs.
To estimate personnel costs for each decision model, we calculated excess work for each resident annually, transferred that work to substitutes hour for hour, and calculated substitutes' wages and benefits, yielding annual reform costs per resident. We multiplied by the number of residents affected to determine annual costs across all teaching hospitals.
We extrapolated the Utah/Colorado study's event incidence, mortality, and costs15 to teaching hospitals in 2001. Adapting costs involved deriving average per-event costs in Utah and Colorado in 1996, inflating for geography and time, allocating costs to teaching hospital and societal perspectives, and projecting across teaching-hospital admissions nationwide.
Next, we determined changes in event incidence, mortality, and costs for the 5 hypothetical changes in event rates under reform. To calculate net reform costs for each decision model and perspective, we added personnel costs and changes in event costs.
As additional analyses, we determined the thresholds at which net reform costs were zero. When reform reduced events but increased costs for society, we estimated cost per death averted. Few studies were available to guide sensitivity analyses so we arbitrarily varied the following by 30%: personnel costs, baseline event rates, and baseline event costs.
RESULTS
Nationwide, accomplishing the ACGME reform with attending physicians would cost $2.2 billion ($144.90 per admission), mid-level providers $1.120 billion ($72.28 per admission), and task-tailored substitutes $673 million ($43.43 per admission) in 2001 dollars (Table 1).
Table 1.
Personnel Costs Because of Reform
| Decision Model | Baseline Resident Hours | Cost Per Resident, 2001* | Cost Across Teaching Hospitals, 2001 |
|---|---|---|---|
| Attending substitutes | 90 | $40,606 | $669,435,462 |
| 100 | $81,213 | $1,575,118,377 | |
| Sum=$2,244,553,839 | |||
| Mid-level substitutes | 90 | $20,257 | $333,950,308 |
| 100 | $40,513 | $785,753,514 | |
| Sum=$1,119,703,822 | |||
| Task-tailored substitutes | 90 | $8,027 | $132,336,089 |
| 100 | $27,862 | $540,381,357 | |
| Sum=$672,717,446 | |||
| Existing residents | 90 | $0 | $0 |
| 100 | $0 | $0 | |
| Sum=$0 |
We estimated that 294,320 preventable adverse events occurred at teaching hospitals in 2001, and that 20,308 were fatal. Nationally, these events cost teaching hospitals $3.6 billion ($12,328 each) and society $13.2 billion ($45,008 each) (Table 2).
Table 2.
Preventable Adverse Event Costs at Teaching Hospitals
| Type of Cost | Cost Across Utah & Colorado Hospitals, 1996* | Cost Per Event, 2001 | Cost Across Teaching Hospitals, 2001 |
|---|---|---|---|
| Costs to Hospitals | |||
| ICU | $17,575,000 | $2,602 | $765,820,640 |
| Inpatient non-ICU | $62,492,000 | $9,251 | $2,722,754,320 |
| Inpatient physician | $3,438,000 | $475 | $139,802,000 |
| Sum=$3,628,376,960 | |||
| Additional Costs to Society | |||
| Nursing home | $60,158,000 | $8,906 | $2,621,213,920 |
| Rehabilitation | $7,715,000 | $1,038 | $305,504,160 |
| Home health care | $4,449,000 | $599 | $176,297,680 |
| Outpatient physician | $1,765,000 | $244 | $71,814,080 |
| Drugs | $1,106,000 | $154 | $45,325,280 |
| Equipment | $547,000 | $76 | $22,368,320 |
| Lost wages | $63,309,000 | $9,196 | $2,706,566,720 |
| Household production | $85,828,000 | $12,467 | $3,669,287,440 |
| Sum=$13,246,754,560 | |||
Estimated 8,859 events across the two states.15
ICU, intensivecare unit.
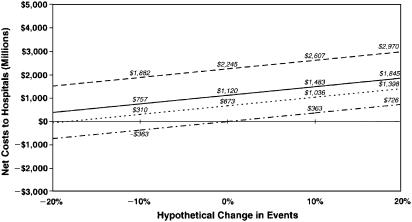
Figure 1 presents net reform costs from the teaching-hospital perspective. To be cost neutral, reform must decrease events by 61.9% using attending physicians, 30.9% using mid-level providers, and 18.5% using task-tailored substitutes. Under the sensitivity analysis most favorable to reform (30% lower personnel costs), events must drop by 43.3%, 21.6%, and 13.0%, respectively. Under the least favorable sensitivity analysis (30% lower event incidence or costs at baseline), reductions of 88.4%, 44.1%, and 26.5% would be required, respectively.
FIGURE 1.
Net costs of reform from the teaching-hospital perspective. Net costs of using attending substitutes are indicated by (––––), mid-level substitutes by (——), task-tailored substitutes by (---), and existing residents by (–.).
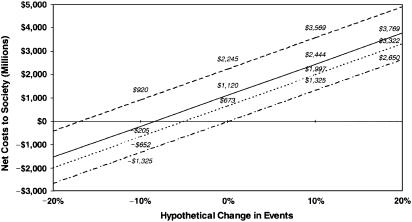
Figure 2 presents net reform costs from the societal perspective. To be cost neutral, reform must decrease events by 16.9% using attending physicians, 8.5% using mid-level providers, and 5.1% using task-tailored substitutes. Under the sensitivity analysis most favorable to reform (30% lower personnel costs), events need to decrease by 11.9%, 5.9%, and 3.6%, respectively. Under the least favorable sensitivity analysis (30% lower event incidence or costs at baseline), events must fall 24.2%, 12.1%, and 7.3%, respectively.
FIGURE 2.
Net costs of reform from the societal perspective. Net costs of using attending substitutes are indicated by (––––), mid-level substitutes by (———), task-tailored substitutes by (---), and existing residents by (–.).
A 10% decrease in events would avert 2,031 deaths nationwide. Using attending physician substitutes and achieving this decline would cost society $452,978 per life saved.
DISCUSSION
To summarize our findings, the ACGME residency work-hours reform could cost $673 million to $1.1 billion per year nationwide if excess resident work is transferred to nonphysician providers. Preventable adverse events appear far more expensive, costing teaching hospitals $3.6 billion and society $13.2 billion per year—and claiming over 20,000 lives. Reform strategies promoting these events will increase mortality and costs, even if personnel costs are nil. Because most economic effects of preventable adverse events occur after discharge,15 strategies using lower- and mid-level providers are more likely to be cost neutral for society than for teaching hospitals: a 5.1% to 8.5% decline in events would be needed from the societal perspective, while 18.5% to 30.9% would be from the teaching-hospital perspective.
Although patient safety was, ostensibly, the impetus for reform, prior efforts to limit resident work-hours have had mixed outcomes.44–47 This suggests that the success of reform may depend on the approach but, unfortunately, few studies have explored how to optimize clinical or educational outcomes under reform. One recent randomized trial added more residents to intensivecare unit teams, reducing weekly hours and shortening shifts, and substantially decreasing serious errors.47 Because of implications for physician supply and Balanced Budget Act caps on residency positions,48 hiring additional residents seems unfeasible nationwide. Changes in New York State surgery programs after 1998 illustrate the range of possibilities: half increased resident cross-coverage, 42% instituted a night-float system, 35% transferred work from junior residents to seniors, 14% recruited new residents or reassigned existing ones, 14% permitted nonteaching patients, 54% increased mid-level providers' roles, and 11% increased lower-level providers' roles.16 Several editorialists argue that, of these, transferring noneducational tasks to lower and mid-level providers would best promote resident education and patient safety.17–20
Two points support the hypothesis that this approach would benefit resident education. Eliminating menial tasks may alleviate stress,49 encouraging learning. More importantly, it should allow programs to reduce work-hours without affecting education. A recent metaanalysis found that residents working 84.5 hours weeks spend 29.5 hours in patient-care activities of marginal or no educational value.24 In contrast with substitution strategies, redistributing work among residents may encroach upon conference attendance, independent reading, and elective rotations.
If substitution best preserves education, would it also promote patient safety? Reform may reduce sleep deprivation,46 but discontinuity in care has a potentially larger effect on patient outcomes.50 Studies suggest alleviating fatigue might diminish error commission rates: one reform effort lowered medication errors by 29%,44 and a few studies found 20% to 100% more errors on postcall days.23 Most convincingly, the randomized trial mentioned above found that interns working 85-hour weeks slept less, had more than twice the attentional failures,46 and committed 35.9% more serious errors than those working 65-hour weeks.47 However, most errors are intercepted or happen to not cause harm. In that trial, more than half of the serious errors were intercepted. And while the interns working longer hours committed 56.6% more nonintercepted serious errors, injuries because of these errors (i.e., preventable adverse events) were unchanged. The study was not powered to address preventable adverse events47 but its results suggest that reducing sleep deprivation might prevent many errors and, possibly, a smaller number of adverse events.
Discontinuities of care appear potentially more dangerous than sleep deprivation: one study found that preventable adverse events climbed 500% on days that interns were cross-covering.50 Standardized sign-out mitigated this risk in a follow-up study and in the above trial.47,51 This suggests that preventable adverse events could rise under the ACGME reform if handoffs are not handled carefully because adding days off and limiting call must increase cross-coverage. In addition to standardizing sign-out, programs can mitigate discontinuity risks by minimizing the transfer of work among residents.
Substantial improvements in efficiency, perhaps via technological innovation, might reduce hours without shifting work among residents or to substitute providers. Today, however, curtailing residents' hours without redistributing the work seems likely to erode education, implicitly transfer work to attending physicians, or jeopardize patient care.
Even if substitution with nonphysician providers preserves education and quality of care, cost is a major drawback. Such strategies could cost up to $40,000 per resident annually and boost admission costs by $43.43 to $72.28 each. Teaching hospitals may be reluctant to undertake this expenditure without subsidies, particularly because their economic condition worsened after the Balanced Budget Act.48,52 Resident substitution would be much more appealing if it were cost neutral.
If reform succeeds at preventing adverse events, it could save teaching hospitals money through lower hospitalization costs or decreased litigation. The latter seems unlikely because malpractice claims follow only 1.5% of negligent adverse events (a subset of preventable ones)53 and neither adverse events nor negligence predict payments to claimants.54 Although lower hospitalization costs appear plausible, preventable adverse events must fall 18.5% to 30.9% to make substitution cost neutral for teaching hospitals; this magnitude reduction may not be attainable.
In contrast, a modest decline in preventable adverse events, 5.1% to 8.5%, might make resident substitution cost neutral for society. Reform strategies this effective could also save about 1,000 to 1,700 lives annually. The 56.6% decline in nonintercepted serious medical errors observed in the above trial 47 suggests that a modest decline in preventable adverse events might be achievable. Because substitution would still be cost increasing from a teaching-hospital perspective, government subsidies could be justifiable. Although not reintroduced to date in 2005,9“The Patient and Physician Safety and Protection Act of 2003” did allocate funds for reform.13,14 The proposed legislation might increase federal graduate medical education payments by 7.6% to 12.5% relative to fiscal year 2002,48 assuming that personnel costs would be the same as under the ACGME policy.
Unfortunately, the quality of available data tempers the strength of our conclusions. First, we estimated pre-reform work-hours from 1998 New York State data—i.e., after reform; however, these estimates appear higher than 2001 AAMC data for first-year residents nationally.5,55 Second, we extrapolated an Internal Medicine substitution model29 to all specialties. Third, we arbitrarily transferred work to substitutes hour for hour when the actual effect on workload is unknown. Fourth, because negligent adverse event rates are similar at major teaching and nonteaching hospitals,56 we assumed that preventable adverse event rates would be too. Fifth, event costs may be higher at teaching hospitals, although we identified no literature addressing this. Sixth, we assumed that enforcement costs would be negligible, which is unlikely. Finally, we share the limitations of the Utah and Colorado study, which used implicit review methods to determine incremental event costs and omitted transportation, informal caregiving, and the friction costs of litigation.15
Our analysis was limited to monetary costs and mortality; we did not account for the potential effect of reducing adverse events on length and quality of life. Although this would not alter findings from the teaching-hospital perspective, it could affect those from the societal perspective. We did not have the data, however, to conduct cost-utility or cost-benefit analyses. Further, one study suggested that preventable adverse events may have a modest effect on length or quality of life.57
CONCLUSION
Protecting patients from iatrogenic injury should be the principal goal of residency work-hours reform. Future research should evaluate which reform strategies improve patient outcomes and at what cost. Our data suggest that even an expensive reform approach like resident substitution could be cost neutral to society if modestly effective at preventing adverse events. However, such approaches appear less likely to be cost neutral for teaching hospitals, unless additional funds are allocated.
Acknowledgments
The authors wish to acknowledge the assistance of Lee Hilborne, MD, MPH, in the preparation of this article. This work was supported, in part, by a National Research Service Award Primary Care Fellowship.
References
- 1.Accreditation Council for Graduate Medical Education. ACGME Duty Hours Standards Now In Effect for All Residency Programs, July 1, 2003. Available at http://www.acgme.org/Media/NewsRelease.asp Accessed May 18, 2004.
- 2.Steinbrook R. “The debate over residents” work-hours. N Engl J Med. 2002;347:1296–302. doi: 10.1056/NEJMhpr022383. [DOI] [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. The ACGMEs Role in Protecting Education, Patient Safety and Resident Safety: ACGMEs Response to HR 3236 and Similar Calls for Regulation to Address Resident Hours. Available at http://www.acgme.org/New/conyerscom.pdf Accessed May 18, 2004.
- 4.Philibert I, Friedmann Pl, Williams WT. New requirements for resident duty hours: report of the ACGME Work Group on Resident Duty Hours. JAMA. 2002;288:1112–4. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 5.DeBuono BA, Osten WM. The medical resident workload: the case of New York State. JAMA. 1998;280:1882–3. [PubMed] [Google Scholar]
- 6.Millenson ML. Pushing the profession: how the news media turned patient safety into a priority. Qual Saf Healthcare. 2002;11:57–63. doi: 10.1136/qhc.11.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kohn L, Corrigan J, Donaldson M. To Err Is Human: Building a Safer Health System. Committee on Quality of Healthcare in America. Institute of Medicine. Washington, D.C.: National Academy Press; 1999. [Google Scholar]
- 8.The Agency for Healthcare Research and Quality. Patient Safety Research Initiatives: Fiscal Year 2001. Available at http://www.ahrq.gov/qual/ps2001.htm Accessed May 18, 2004.
- 9.Congressional Text Record. Thomas: Legislative Information on the Internet. Available at http://thomas.loc.gov Accessed May 16, 2005.
- 10.Gurjala A, Lurie P, Haroona L, et al. Petition to the occupational safety and health administration requesting that limits be placed on hours worked by medical residents (HRG Publication #1570). 2001. Available at http://www.citizen.org/publications/print_release.cfm?ID=6771 Accessed March 11, 2003.
- 11.Conyers J, Waxman HA, Stark FP, et al. H.R. 3236, Patient and Physician Protection Act of 2001. 107th Congress, 1st Session.
- 12.Accreditation Council for Graduate Medical Education. Resident duty hours language, final requirements, February 13, 2003. Available at http://www.acgme.org/DutyHours/dutyHoursLang_final.asp Accessed May 18, 2004.
- 13.Conyers J. H.R. 1228, Patient and Physician Protection Act of 2003. 108th Congress, 1st Session.
- 14.Corzine JS. H.R. 952, Patient and Physician Protection Act of 2003. 108th Congress, 1st Session.
- 15.Thomas EJ, Studdert DM, Newhouse JP. Costs of medical injuries in Utah and Colorado. Inquiry. 1999;36:255–64. [PubMed] [Google Scholar]
- 16.Whang EE, Mello MM, Ashley SW, Zinner MJ. Implementing resident work hour limitations: lessons from The New York state experience. Ann Surg. 2003;237:449–55. doi: 10.1097/01.SLA.0000059966.07463.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole DJ, Bertagnolli MM, Nussbaum M. Society of university surgeons statement on surgical resident work-hours and education. Surgery. 2002;132:115–8. doi: 10.1067/msy.2002.126012. [DOI] [PubMed] [Google Scholar]
- 18.Darosa DA, Bell RHJ, Dunnington GL. Residency program models, implications, and evaluation: results of a think tank consortium on resident work-hours. Surgery. 2003;133:13–23. doi: 10.1067/msy.2003.67. [DOI] [PubMed] [Google Scholar]
- 19.Greenfield LJ. Limiting resident duty hours. Am J Surg. 2003;185:10–2. doi: 10.1016/s0002-9610(02)01144-3. [DOI] [PubMed] [Google Scholar]
- 20.Weinstein DF. Duty hours for resident physicians—tough choices for teaching hospitals. N Engl J Med. 2002;347:1275–8. doi: 10.1056/NEJMsb022065. [DOI] [PubMed] [Google Scholar]
- 21.Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290:1868–74. doi: 10.1001/jama.290.14.1868. [DOI] [PubMed] [Google Scholar]
- 22.Philibert I, Vasilias J. Accreditation Council for Graduate Medical Education. An Annotated Bibliography of Selected Articles on Resident and Physician Duty Hours. August 2002. Available at http://www.acgme.org/DutyHours/dutyHrs_Index.asp Accessed November 11, 2003.
- 23.Veasey S, Rosen R, Barzansky B, Rosen I, Owens J. Sleep loss and fatigue in residency training: a reappraisal. JAMA. 2002;288:1116–24. doi: 10.1001/jama.288.9.1116. [DOI] [PubMed] [Google Scholar]
- 24.Boex JR, Leahy PJ. Understanding residents' work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78:939–44. doi: 10.1097/00001888-200309000-00022. [DOI] [PubMed] [Google Scholar]
- 25.Jha AK, Duncan BW, Bates DW. Fatigue, sleepiness, and medical errors. In: Shojania KG, Duncan BW, McDonald KM, Wachter RM, editors. Making Healthcare Safer: A Critical Analysis of Patient Safety Practices. Vol 43. Rockville, Md: Agency for Healthcare Research and Quality; 2001. pp. 519–33. [Google Scholar]
- 26.Gaba DM, Howard SK. Patient safety: fatigue among clinicians and the safety of patients. N Engl J Med. 2002;347:1249–55. doi: 10.1056/NEJMsa020846. [DOI] [PubMed] [Google Scholar]
- 27.Accreditation Council for Graduate Medical Education. A glossary of selected terms, essentials of accredited residencies in graduate medical education, Section II, GME Useful Information. Available at http://www.acgme.org/GmeDir/Sect2.asp#gloss Accessed May 18, 2004.
- 28.Accreditation Council for Graduate Medical Education. Number of all accredited programs for a specific academic year (excluding combined programs). June 30, 2002. Available at http://www.acgme.org/adspublic/reports/accredited_programs_2001.html Accessed March 10, 2003.
- 29.Knickman JR, Lipkin MJ, Finkler SA, Thompson WG, Kiel J. The potential for using non-physicians to compensate for the reduced availability of residents. Acad Med. 1992;67:429–38. doi: 10.1097/00001888-199207000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz RJ, Dubrow TJ, Rosso RF, Williams RA, Butler JA, Wilson SE. Guidelines for surgical residents' working hours. Intent vs reality. Arch Surg. 1992;127:778–82. doi: 10.1001/archsurg.1992.01420070030008. (discussion 782–773) [DOI] [PubMed] [Google Scholar]
- 31.Scher KS, Peoples JB. A study of the on-duty hours of surgical residents. Surgery. 1990;108:393–7. [PubMed] [Google Scholar]
- 32.Stoddard JJ, Kindig DA, Libby D. Graduate medical education reform. Service provision transition costs. JAMA. 1994;272:53–8. [PubMed] [Google Scholar]
- 33.Dolan KL, Rosner F, Spiegel K. Survey of nonphysician tasks performed by medicine residents at a municipal hospital. J Natl Med Assoc. 1990:629–33. [PMC free article] [PubMed] [Google Scholar]
- 34.U.S. Department of Labor: Bureau of Labor Statistics. National occupational employment and wage estimates: healthcare practitioners and technical occupations. 2001. Available at http://www.bls.gov./oes/2001/oes_29He.htm Accessed December 12, 2002.
- 35.U.S. Department of Labor: Bureau of Labor Statistics. National Compensation Survey. 2001. Available at http://www.bls.gov Accessed April 3, 2003.
- 36.U.S. Department of Labor, Bureau of Labor Statistics. Employer cost for employee compensation, annual data for 2001. Available at http://data.bls.gov Accessed May 18, 2004.
- 37.U.S. Census Bureau, Population Division, Population Estimates Program. ST-99-# state population estimates: annual time series: July 1, 1990 to July 1 1999. Available at http://eire.census.gov/popest/archives/state/st-99-3.txt Accessed April 2, 2003.
- 38.Berry WD, Richard C, Fording, Russel LH. Cost of Living Index For The United States, 1960–2000. Ann Arbor, Mich: Inter-University Consortium for Political and Social Research; 2003. Available at http://ssdc.ucsd.edu/ssdc/icp01275.html Accessed April 2, 2003. [Google Scholar]
- 39.U.S. Department of Labor: Bureau of Labor Statistics. National compensation survey, March 10, 2003. Available at http://data.bls.gov Accessed April 3, 2003.
- 40.U.S. Department of Labor: Bureau of Labor Statistics. Consumer price index, all urban consumers. Available at http://data.bls.gov Accessed April 2, 2003.
- 41.U.S. Department of Labor: Bureau of Labor Statistics. Employment cost index, June 2001. Available at ftp://ftp.bls.gov/pub/news.release/History/eci.07262001.news Accessed April 4, 2003.
- 42.U.S. Department of Labor: Bureau of Labor Statistics. Employment cost index, June 1996. Available at ftp://ftp.bls.gov/pub/news.release/History/eci.07262001.news Accessed April 4, 2003.
- 43.Chicago: Health Forum, an American Hospital Association Affiliate. Custom Report Compiled by American Hospital Association Resource Center. Chicago, Ill: American Hospital Association Annual Survey; March 2003. [Google Scholar]
- 44.Gottlieb DJ, Parenti CM, Peterson CA, Lofgren RP. Effect of a change in house staff work schedule on resource utilization and patient care. Arch Intern Med. 1991;151:2065–70. [PubMed] [Google Scholar]
- 45.Laine C, Goldman L, Soukup JR, Hayes JG. The impact of a regulation restricting medical house staff working hours on the quality of patient care. JAMA. 1993;269:374–8. [PubMed] [Google Scholar]
- 46.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 47.Landrigan CP, Rothschild JM, Cronin JW. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–4. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 48.Knapp RM. Complexity and uncertainty in financing graduate medical education. Acad Med. 2002:1076–83. doi: 10.1097/00001888-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Schwartz AJ, Black ER, Goldstein MG, Jozefowicz RF, Emmings FG. Levels and causes of stress among residents. J Med Educ. 1987;62:744–53. doi: 10.1097/00001888-198709000-00006. [DOI] [PubMed] [Google Scholar]
- 50.Petersen LA, Brennan TA, O'Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72. doi: 10.7326/0003-4819-121-11-199412010-00008. [DOI] [PubMed] [Google Scholar]
- 51.Petersen LA, Orav EJ, Teich JM, O'Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24:77–87. doi: 10.1016/s1070-3241(16)30363-7. [DOI] [PubMed] [Google Scholar]
- 52.The Economic Health of Teaching Hospitals Continues to Decline. AAMC fact sheet; 2000: 4(3).
- 53.Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study iii. N Engl J Med. 1991;325:245–51. doi: 10.1056/NEJM199107253250405. [DOI] [PubMed] [Google Scholar]
- 54.Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. N Engl J Med. 1996;335:1963–7. doi: 10.1056/NEJM199612263352606. [DOI] [PubMed] [Google Scholar]
- 55.Brotherton SE, Simon FA, Etzel SI. US graduate medical education, 2001–2002: changing dynamics. JAMA. 2002;288:1073–8. doi: 10.1001/jama.288.9.1073. [DOI] [PubMed] [Google Scholar]
- 56.Patients, doctors, and lawyers: medical injury, malpractice litigation, and patient compensation in New York. The report of the Harvard Medical Practice Study to the state of New York. 1990.
- 57.Hayward RA, Hofer TP. Estimating hospital deaths due to medical errors: preventability is in the eye of the reviewer. JAMA. 2001;286:415–20. doi: 10.1001/jama.286.4.415. [DOI] [PubMed] [Google Scholar]