Abstract
Background
Emergency department (ED) patients often fail to follow-up with referrals to outpatient clinics and physicians.
Objective
To compare the effects of 2 ED discharge instructional methods on outpatient follow-up compliance and to evaluate sociodemographic characteristics as possible factors affecting outpatient follow-up compliance.
Design and Participants
Randomized trial of ED patients. At discharge, the intervention group had their follow-up appointment made and the standard group was given our hospital's referral service phone number to make their own follow-up appointment.
Measurements
Outpatient clinics were called 1 month after each subject's ED discharge to ascertain if they followed-up. Poisson regression was used to examine the effects of sociodemographic factors on follow-up compliance.
RESULTS
Of 287 eligible subjects, 250 (87%) agreed to participate. Follow-up rates were 59% for the intervention group and 37% for the standard group (P<.001). Having a primary care physicians appeared to increase ED patients' outpatient follow-up compliance and having Medicaid insurance appeared to decrease outpatient follow-up compliance, but neither of these findings was statistically significant.
Conclusions
In our ED, patients who have their outpatient follow-up appointment made at discharge have a significantly greater probability of follow-up compliance compared with patients given standard discharge instructions. Most sociodemographic characteristics do not affect our ED patients' follow-up compliance.
Keywords: emergency department, follow-up compliance, outpatient
There are 110 million emergency department (ED) patient visits in the United States each year.1 Approximately 45% of these patients are referred for outpatient follow-up with another physician or clinic. Follow-up for these ED patients is important for several reasons, including ensuring proper treatment continuation of the initial condition, identification of misdiagnoses, management of treatment failures and complications, and recognition of patient noncompliance to therapeutic plans.2 Notwithstanding these reasons, compliance with recommended follow-up by ED patients in the United States is frequently very poor and has been estimated to be between 26% and 56% depending on the ED population.3–7
Prior studies have found that providing ED patients with outpatient appointments before their discharge significantly improves follow-up compliance.6,7 These studies, however, were limited by their observational design and potential for confounding. To more definitively assess the effect of making follow-up appointments for patients in a general adult ED population, we conducted a randomized trial to compare follow-up compliance for ED patients with 2 different discharge instructional methods. We also evaluated several patient sociodemographic characteristics as possible factors affecting greater outpatient follow-up compliance.
MATERIALS AND METHODS
Study Design and Setting
We conducted a randomized trial comparing the effect of 2 ED discharge instructional methods on outpatient follow-up compliance: (1) follow-up appointment made for the patient at the time of their ED discharge (intervention group) and (2) follow-up appointment made by the patient after ED discharge with our standard instructions (standard group). The trial was conducted at Northwestern Memorial Hospital, a large university-based urban teaching hospital with a demographically diverse ED census of approximately 70,000 patient visits per year. The trial was conducted between 8:00 am and 4:00 pm during weekdays when there are 3 or 4 attending emergency physicians and 4 to 6 resident physicians in our ED. Patient assignment to physicians is not based on medical complaint. The study was approved by the Northwestern University Institutional Review Board.
Selection of Study Participants
The study population included ED patients 18 years of age and older with medical conditions warranting follow-up within 1 month in an outpatient clinical setting as determined by the attending physician. From February through April 2002, eligible subjects were identified and selected consecutively by research assistants (based on their availability) during hours when outpatient clinics were open (i.e., weekdays between 8:00 am and 4:00 pm) so follow-up appointments could be made directly with outpatient clinic office personnel. Patients seen during this time period represent about 30% of all patients seen in our ED. Their diverse medical conditions were classified into major disease categories using International Classification of Diseases-9-Clinical Modification (ICD-9-CM) code ranges.1
We included only patients living in Chicago who had an institution-affiliated primary care physicians (PCP) or who were willing to be referred to an institution-affiliated physician. Insurance status was not a determinant for selection. Subjects were excluded if they had any of the following: (1) psychiatric problems or a history of substance abuse; (2) scheduled ED return visit for short-term follow-up (e.g., for wound check or suture removal); (3) were admitted to the hospital; or (4) language barriers making understanding of discharge instructions questionable. Written informed consent was obtained from each participating study subject.
Randomization and Intervention
Subjects were randomly assigned to the intervention group or the standard group by the research assistant based on the last digit of their medical record number. Attending physicians, residents, and nurses were blinded to this method. Odd numbers were assigned to the intervention group and even numbers were assigned to the standard group. Subjects in the intervention group had an outpatient appointment with their PCP or referral physician made (at the time of their ED discharge) by a research assistant based upon the recommendations of the attending physician to fit with the subject's schedule as best as possible. Subjects in the standard group were asked to follow-up with their PCP or with the hospital referral physician recommended to them (i.e., our standard discharge instruction). Both intervention and standard groups were given written discharge instructions for their follow-up. They were also given written instructions regarding prescribed medications and the need to return to the ED if symptoms worsened. For each subject, the outpatient referral clinic was contacted at 1 month to determine if they complied with the recommended follow-up appointment. This determination was successful for all subjects.
Other Study Variables
Using the same study population, we conducted a multivariate analysis to assess possible effects of patient sociodemographic characteristics on outpatient follow-up compliance. Information concerning the sociodemographic variables was collected by the research assistants using a standardized data collection instrument. This included age, race, gender, education level, diagnosis category, insurance status, and distance from home to the referred outpatient clinic. Age was categorized as less than 35, 35 to 54, and greater than 54 years of age to represent young, middle-aged, and elderly adults, respectively. Race was categorized as nonwhite versus white. Education level was categorized as less than college degree versus college degree or greater. ICD-9-CM classification was categorized as noninjury versus injury. Insurance status was categorized as having standard insurance, health maintenance organization (HMO), Medicare, Medicaid, and not having insurance. Patients with standard insurance included 88 with preferred provider organization, 19 with fee-for-service, 6 with point-of-service, preferred provider organization, 5 with worker's compensation. While preferred provider organization and point-of-service insurance are technically types of HMO insurance, like fee-for service and worker's compensation insurance, they typically allow patients the opportunity to choose from most physicians without referral from their PCP. Distance from outpatient clinic was arbitrarily categorized as less than 7 miles versus 7 miles or greater. This was estimated comparing the average distance from the study subject's ZIP Code to the outpatient clinic using a distance calculator provided by ZipFind®.8
Statistical Analyses
Crosstabular univariate analyses with χ2 tests were conducted to estimate crude relative risk measures for the effects of the intervention and the sociodemographic variables on the outcome of outpatient follow-up compliance. Poisson multivariate regression modeling was used to estimate adjusted relative risks and confidence intervals (CIs) for the intervention and the sociodemographic variables on the outcome of outpatient follow-up compliance. Terms for all the sociodemographic characteristics were included in the regression equation making the relative risk estimates for the study variables mutually adjusted. Statistical analyses were performed using Stata Statistical Software, version 7.0.9
RESULTS
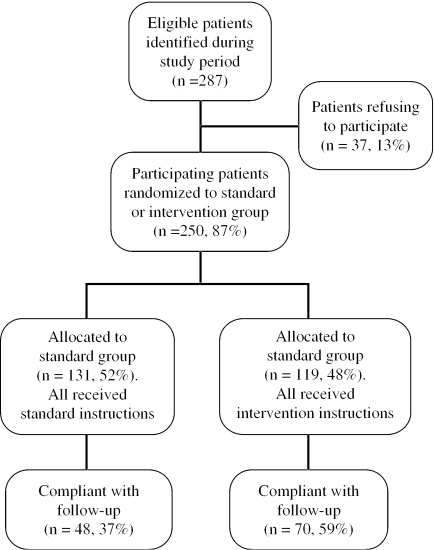
Of 287 eligible subjects identified during the study period, 250 (87.1%) agreed to participate: 119 (48%) were assigned to the intervention group and 131 (52%) were assigned to the standard group (Fig. 1). There were no significant differences between the standard and intervention groups with regards to age, gender, race/ethnicity, education level, distance from the outpatient clinic, disease category, or insurance status. However, subjects in the standard group were more likely to have a PCP (63% of standard group vs 50% of intervention group, P=.039). Follow-up status for all subjects was determined at 1 month. The distribution of the study subjects by major disease category and ICD-9-CM code range is presented in Table 1. Most of the study subjects were noninjury patients (66%) compared with injury patients (34%).
FIGURE 1.
Flow Diagram of Emergency Department Patients in a Randomized Trial Comparing Standard Versus the Intervention Groups
Table 1.
Distribution of Study Subjects by Major Disease Category and ICD-9-CM Code Range
| Major Disease Category | ICD-9-CM Code Range | Number of Subjects (%) |
|---|---|---|
| Noninjury categories | ||
| Infectious and parasitic diseases | 001 to 139 | 7 (2.8) |
| Endocrine, metabolic diseases, and immunity disorders | 240 to 279 | 3 (1.2) |
| Diseases of the blood and blood forming organs | 280 to 289 | 2 (0.8) |
| Diseases of the nervous system and sense organs | 320 to 389 | 12 (4.8) |
| Diseases of the circulatory system | 390 to 459 | 6 (2.4) |
| Diseases of the respiratory system | 460 to 519 | 13 (5.2) |
| Diseases of the digestive system | 520 to 579 | 6 (2.4) |
| Diseases of the genitourinary system | 580 to 629 | 16 (6.4) |
| Complications of pregnancy, childbirth, and the puerperium | 630 to 677 | 2 (0.8) |
| Diseases of the skin and subcutaneous tissue | 680 to 709 | 16 (6.4) |
| Diseases of the musculoskeletal and connective tissue | 710 to 739 | 33 (13.2) |
| Symptoms, signs, and ill-defined conditions | 780 to 799 | 49 (19.6) |
| Injury categories | ||
| Fractures | 800 to 829 | 34 (13.6) |
| Sprains | 840 to 848 | 26 (10.4) |
| Open wounds | 870 to 897 | 13 (5.2) |
| Contusions | 920 to 924 | 7 (2.8) |
| Burns | 940 to 943 | 3 (1.2) |
| Poisoning and toxic effects | 960 to 989 | 2 (0.8) |
| Total | 250 |
As illustrated in Table 2, the overall compliance with follow-up rates were 59% for the intervention group and 37% for the standard group (P<.001). However, the intervention was much more effective in the subgroup of patients that did not have a PCP (53% vs 17%, P<.001). After mutually adjusting for the sociodemographic characteristics with multivariate analysis (Table 3), only being in the intervention group (adjusted relative risk=1.84%, 95% CI 1.24 to 2.13) was associated with increased compliance with outpatient follow-up. Having a PCP appeared to increase ED patients' outpatient follow-up compliance and having Medicaid insurance appeared to decrease outpatient follow-up compliance, but neither of these findings was statistically significant. Patients greater that 54 years of age appeared to follow-up at a greater rate than patients younger than 35 years of age with univariate analysis, but this association was significantly less with implementation of multivariate analysis.
Table 2.
Proportion of Patients That Followed Up with Their Outpatient Referral Appointment by Method of Discharge Instructions*
| Study Group | Followed-Up (%) | Did Not Follow-Up (%) | Total Subjects | Relative Risk for Follow-Up (95% CI) |
|---|---|---|---|---|
| Subjects with a PCP | ||||
| Intervention group | 39 (65) | 21 (35) | 60 | 1.35 |
| Standard group | 40 (48) | 43 (52) | 83 | (95% CI 1.01 to 1.80) |
| Subjects without a PCP | ||||
| Intervention group | 31 (53) | 28 (47) | 59 | 3.15 |
| Standard group | 8 (17) | 40 (83) | 48 | (95% CI 1.60 to 6.21) |
| All subjects | ||||
| Intervention group | 70 (59) | 49 (41) | 119 | 1.61 |
| Standard group | 48 (37) | 83 (63) | 131 | (95% CI 1.22 to 2.10) |
Subjects in the intervention group had an outpatient appointment with their PCP or referral physician made before discharge. Subjects in the standard group were asked to follow-up with their PCP or with the referral physician recommended to them.
PCP, primary care physicians; CI, confidence interval
Table 3.
Crude and Adjusted Relative Risks Estimates of the Effect of Study Subjects' Sociodemographic Characteristics on Outpatient Follow-Up Compliance
| Sociodemographic Characteristic (n=250) | Crude Relative Risk for Follow-Up (95% CI) | Adjusted Relative Risk for Follow-Up (95% CI) |
|---|---|---|
| Age: 35 to 54 y (n=101) compared with less than 35 y (n=107) | 1.01 (0.75 to 1.38) | 0.85 (0.55 to 1.31) |
| Age: greater than 54 (n=42) compared with less than 35 y (n=107) | 1.41 (1.02 to 1.94) | 1.08 (0.57 to 2.03) |
| Gender: female (n=108) compared with male (n=142) | 0.90 (0.69 to 1.18) | 0.91 (0.60 to 1.38) |
| Race/ethnicity: nonwhite (n=125) compared with white (n=123) | 0.87 (0.67 to 1.14) | 0.99 (0.65 to 1.52) |
| Education level: less than college degree (n=130) compared with college degree or greater (n=112) | 0.83 (0.63 to 1.09) | 0.99 (0.64 to 1.51) |
| Distance from clinic: 7 or more miles (n=108) compared with 7 or more miles (n=142) | 0.87 (0.66 to 1.14) | 0.87 (0.58 to 1.30) |
| PCP: having a PCP (n=143) compared with not having a PCP (n=107) | 1.52 (1.13 to 2.03) | 1.52 (0.95 to 2.43) |
| Disease category: injury (n=85) compared with noninjury (n=165) | 1.07 (0.82 to 1.41) | 0.99 (0.65 to 1.50) |
| Insurance status: HMO (n=43) compared with standard (n=118) | 1.01 (0.71 to 1.42) | 0.94 (0.55 to 1.58) |
| Insurance status: no insurance (n=39) compared with standard (n=118) | 0.76 (0.51 to 1.13) | 0.78 (0.45 to 1.37) |
| Insurance status: Medicare (n=21) compared with standard (n=118) | 1.22 (0.83 to 1.78) | 0.99 (0.47 to 2.09) |
| Insurance status: Medicaid (n=16) compared with standard (n=118) | 0.37 (0.13 to 1.04) | 0.25 (0.06 to 1.04) |
| Discharge instruction: intervention (n=119) compared with standard (n=131)* | 1.61 (1.22 to 2.10) | 1.84 (1.24 to 2.13) |
Subjects in the intervention group had an outpatient appointment with their PCP or referral physician made before discharge. Subjects in the standard group were asked to follow-up with their PCP or with the referral physician recommended to them.
PCP, primary care physicians; CI, confidence interval; HMO, health maintenance organization.
DISCUSSION
We found that patients seen during weekday hours in our ED are significantly more likely to comply with outpatient follow-up instructions if their appointment is made before discharge. This intervention is particularly effective for patients without a PCP, increasing outpatient follow-up compliance in these patients threefold. Of the several sociodemographic factors that we evaluated, only having a PCP appeared to increase ED patients' outpatient follow-up compliance and having Medicaid insurance appeared to decrease outpatient follow-up compliance, but neither of these findings was statistically significant.
Prior studies have identified similar findings. Thomas et al.7 in a multicenter prospective cohort study, found that patients who had their appointment made at the time of ED discharge were significantly more likely to comply with follow-up instructions. The same study suggested that patients with a regular physician were more likely to follow-up, but this finding was not statistically significant. A retrospective cohort study by Magnusson et al.10 also found that arranging outpatient follow-up significantly improved compliance. Notwithstanding their observational study designs and potential for confounding, both of these prior studies were consistent with our main finding that arranging outpatient follow-up from the ED significantly improves compliance. The main advantage of our randomized trial is the limitation of potential confounding on the measured effect of the intervention on outpatient follow-up compliance. In addition, a study by Barlas et al.11 found that inability to obtain an appointment was cited by 34.4% of those who did not obtain follow-up care as instructed.
Our study also has some limitations. First, it is not clear as to what extent our findings can be extrapolated to weeknight and weekend patients, as well as to patients at other institutions such as community hospital EDs. It is possible our weekday patients have characteristics that may influence the effect of the intervention on compliance with follow-up. From our multivariate analysis, however, it did not appear that age, race, gender, education level, or distance from clinic had independent effects on compliance with outpatient follow-up from the ED. In addition, our findings are consistent with the findings of Thomas et al.7 and Magnusson et al.10, suggesting the measured effect of the intervention may be valid. Unfortunately, both of these prior studies were also conducted at urban teaching hospitals, leaving the question of generalizability of our findings to community hospital EDs unanswered.
Second, while our study had adequate power show the effect of the intervention, the sample size was too small to elucidate the definitive effects of the sociodemographic characteristics on compliance with outpatient follow-up. For example, having a PCP appeared to increase ED patients' outpatient follow-up compliance and having Medicaid insurance appeared to decrease outpatient follow-up compliance, but neither of these findings was statistically significant. Prior studies have suggested that insurance status does not affect outpatient follow-up compliance,7 and that having PCP is a stronger predictor for access to care among patients presenting to EDs.10
Last, our study did not evaluate the effect that individual physicians have on outpatient follow-up compliance. Prior research has shown that effective physician-patient communication that increases patient knowledge and provides clear instructions can improve patient health outcomes, including compliance with planned treatment regimens.2,12,13 Improving physician communication with ED patients will also likely enhance outpatient follow-up compliance. Unfortunately, we did not assess this possible factor because our ED has over 20 attending physicians and discharge instructions are typically given to our patients by nurses.
Despite these limitations, we believe it is reasonable to conclude that ED patients who have their outpatient follow-up appointment made at the time of discharge are more likely to comply with outpatient follow-up care. Determining the complex relations among all the factors that influence outpatient follow-up from different types of EDs will require a large multicenter study. Regardless, emergency physicians and PCPs should find ways to improve patient follow-up compliance whenever possible, including arranging the follow-up appointment when feasible and encouraging ED patients to establish relationships with PCPs.
Acknowledgments
This study was supported by an Excellence in Academic Medicine grant from the State of Illinois Department of Public Aid and Northwestern Memorial Hospital.
References
- 1.McCaig LF, Burt CW. National hospital ambulatory medical care survey: 2002 emergency department summary. Adv Data. 2004;340:1–34. [PubMed] [Google Scholar]
- 2.Becker MH. Patient adherence to prescribed therapies. Med Care. 1985;23:539–55. doi: 10.1097/00005650-198505000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Straus JH, Orr ST, Charney E. Referrals from an emergency room to primary care practices at an urban hospital. Am J Public Health. 1983;73:57–61. doi: 10.2105/ajph.73.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vukmir RB, Kremen R, Dehart DA, Menegazzi J. Compliance with emergency department patient referral. Am J Emerg Med. 1992;10:413–7. doi: 10.1016/0735-6757(92)90065-6. [DOI] [PubMed] [Google Scholar]
- 5.Vukmir RB, Kremen R, Eliis GL, Dehart DA, Plewa MC, Menegazzi J. Compliance with emergency department referral: the effect of computerized discharge instructions. Ann Emerg Med. 1993;22:819–23. doi: 10.1016/s0196-0644(05)80798-x. [DOI] [PubMed] [Google Scholar]
- 6.Magnusson AR, Hedges JR, Vanko M, McCarten K, Moorhead JC. Follow-up compliance after emergency department evaluation. Ann Emerg Med. 1993;22:560–7. doi: 10.1016/s0196-0644(05)81942-0. [DOI] [PubMed] [Google Scholar]
- 7.Thomas EJ, Burstein HR, O'Neil AC, Orav EJ, Brennan TA. Patient noncompliance with medical advice after the emergency department visit. Ann Emerg Med. 1996;27:49–55. doi: 10.1016/s0196-0644(96)70296-2. [DOI] [PubMed] [Google Scholar]
- 8. ZipFind® Central Web Site http://link-usa.com/zipcode.
- 9.Stata Statistical Software. Release 7.0. Collegestation, Tex, USA: Stata Corporation; 2001. [Google Scholar]
- 10.Sox CM, Swartz K, Burstin HR, Brennan TA. Insurance or a regular physician: which is the most powerful predictor of health care? Am J Public Health. 1998;88:364–70. doi: 10.2105/ajph.88.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barlas D, Homan CS, Rakowski J, Houck M, Thode HC. How well do patients obtain short-term follow-up care after discharge from the emergency department. Ann Emerg Med. 1999;34:667–9. doi: 10.1016/s0196-0644(99)70163-0. [DOI] [PubMed] [Google Scholar]
- 12.Steward MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 13.Teutsch C. Patient-doctor communication. Med Clin N Am. 2003;87:1115–45. doi: 10.1016/s0025-7125(03)00066-x. [DOI] [PubMed] [Google Scholar]