Abstract
Background
Relatively few studies have directly addressed the interaction dynamics and consequences of a companion's presence in the medical visit, and their findings have been contradictory.
Objectives
To examine how patient's contribution to the medical dialogue, with or without the presence of a visit companion, is related to the perception of the medical visit as patient-centered.
Design
Observational study using pre- and postvisit questionnaires and audiotape recording of medical visits.
Participants
One hundred and fifty-five patients aged 65 or over; 63 in medical visits that included the presence of a companion and 82 in visits that did not include a companion.
Main Outcome Measure
Patient ratings of visit patient-centeredness.
Results
Long visits (greater than 10 minutes long) and visits in which patients were verbally active were rated as more patient-centered by patients than other visits. Since patients were generally less verbally active in visits that included a companion, accompanied visits, especially if they were less than 10 minutes long, received lower patient-centered ratings than others. The presence of a companion was not related to length of the visit, suggesting that the verbal activity of the companion was off-set by decreased verbal activity of the patient.
Conclusions
Our results have suggested that patients are more likely to perceive their physician and visit as patient-centered when they have an opportunity to engage directly in the medical dialogue. A minimal amount of “talk-time” for patients themselves should be safeguarded even in a short visit, when a companion is present.
Keywords: patient-centeredness, patient participation, patient-physician communication, companion, elderly
With a paradigm shift in medicine during the past few decades, the patient-centered approach has been widely acknowledged as a crucial determinant of high-quality care. Various studies have indicated that at least some elements of patient-centered consultation have positive consequences on patient health outcomes as well as utilization of health care resources.1–4
Exploring both disease and illness experiences and finding common ground between patient and physician are pivotal components of patient-centered care,5 for which mutual dialogue between patient and physician is considered as an essential means. Recent reports indicate that as many as 20% to 57% of patients over the age of 65 are accompanied by a family member or friend to their medical visits.6–9 Furthermore, many of these companions are active participants in the medical dialogue of the visit.10,11 Although there have been few empirical studies that directly examined the influence of the companion's presence on the visit's patient-centeredness, both positive and negative impacts on the visit communication and outcomes have been reported. Previous studies have suggested that companions could improve patient-physician communication by supporting patient's communication.6,10,12 Since companions are likely to be a caregiver or a potential caregiver of the patient, they would have perspectives both as a proxy for the patient and as a care provider at home, which makes it easier for them to bridge the perspectives of patient and physician.7 There is some evidence that when a companion is present, physicians are more informative,9,13 and that both patient and physician understanding of visit communication is enhanced.12 Indeed, it is suggested that patients want their companions to be present during their medical visits and appreciate their help.14
However, there is also some concern that a visit companion may usurp the patient's place in the medical dialogue, undermine patient autonomy, and jeopardize confidentiality.7,15,16 Patients in visits with companions were found to be excluded from companion-physician conversations, were rated as less assertive and expressive, and were less involved in joint decision making than patients in dyadic encounters.17 In short, many investigators fear that the presence of a patient companion during a visit can negatively affect the ability of a physician to provide sensitive and responsive patient-centered care.
Considering demographic projections anticipating continued growth in the elderly population, the presence of a visit companion in medical visits is likely to become even more commonplace. In light of the relatively few studies that have directly addressed the interaction dynamics and consequences of a companion's presence in the visit, the current study was designed to explore these issues. In particular, the study addresses how a companion may affect the patient's experience of care, especially in terms of the patient's engagement in the medical dialogue and perceptions of the visit's patient-centeredness.
METHODS
Study Population and Setting
The study sample is composed of elderly patients who visited a geriatric clinic affiliated with a university hospital in Tokyo, Japan. Nine attending physicians (8 males and 1 female) at this outpatient service volunteered to participate in the study. The average age of the physicians was 40 years (range: 33 to 53 years), and they had 14.3 years of experience on average (range: 8 to 30 years).
Inclusion criteria were that the patient was 1) 65 years of age or older, 2) not considered demented by the treating physician, 3) able to provide consent for participating in the study, and 4) had seen the study physician at least once prior to the targeted consultation. Based on the appointment log of the study physicians, every eligible patient whose consultation was expected to include a companion (including a spouse who may also be a patient) was targeted for recruitment, and 30% to 40% of all other eligible patients were randomly selected for recruitment during the study period of August to October 2002.
Data Collection Procedures
The targeted patients were approached in the waiting room prior to their consultation, and had the purpose and procedures of the study explained. Among the 167 patients approached for recruitment to the study, 146 patients (63 with visit companions and 83 without companions) provided written consent to participate in the study. Patients completed a self-administered questionnaire before and after their consultation. The consultation was recorded using a digital voice recorder openly placed on the desk in the consultation room. Participants were assured that they were free to turn the recorder off during the consultation if they felt uncomfortable at any time. There were no instances in which the recorder was turned off. This study was conducted with the approval of the Ethical Review Committee at the School of Medicine, The University of Tokyo and the Committee on Human Research at the Bloomberg School of Public Health, The Johns Hopkins University.
Measures
Patient Characteristics
Patient agegender were obtained from the appointment log, and other patient variables were obtained through patient self-report in the pre- or postvisit questionnaires. Educational attainment was the highest level of education completed, which was asked with 4 options (9th grade, 12th grade, 2-year college, university or higher) and used as an ordinal variable. Health status was measured using 8 items based on the SF-8. Although the SF-36 had been translated and validated in Japan,18 the official Japanese translation of SF-8 was still under development at the time of this study. Consequently, the translation used was developed for this study. The 8-item scores were simply summed to form a total scale score (Cronbach's α=0.80).
Consultation Length
Consultation length was recorded from the audio file. In the analyses, length was dichotomized at the mean (i.e., shorter consultations ≤10 minutes; longer consultations >10 minutes).
Patient Contribution to the Medical Dialogue
Patient's verbal activity was used as a proxy for patient participation and engagement in the care process. This was calculated as the total number of patient's statements divided by the total number of statements made by all participants during the medical visit (i.e., patient and physician in dyadic visits; patient, companion, and physician in triads). The Roter Interaction Analysis System (RIAS) was used to analyze the recorded communication between physician, patient, and companion, with details of the communication analysis reported elsewhere.11 We examined a number of specific measures of patient dialogue as produced by the RIAS coding, such as the proportion of patient's contribution to the information exchange and the proportion of patient's question asking, in addition to a summary measure of patient verbal activity. Since the findings of the analysis did not substantially change with the measure used, our preference was for the simplest and most straightforward measure. Consequently, we have reported only the findings based on patient verbal activity in the medical dialogue.
The communication between patient and companion was also coded in triads, although it was a small proportion of total talk. The median number of patient utterances to the companion per visit was 1 (lower quartile=0, upper quartile=3), which was also considered as a part of the patient's contribution in the analysis. The reason we did not exclude the patient-companion talk was that patients as well as companions often talked to each other, expecting to be heard by the physician. In fact, it was sometimes observed that the patient talked to the companion, and then the physician responded to the patient. There was no significant difference in the results when these utterances were excluded.
Perceived Patient-Centeredness of the Consultation
Patients were asked to rate the patient-centeredness of the consultation they just experienced in the postvisit questionnaire. A modification of Stewart et al.'s patient-centeredness scale was used to assess patients' judgments of their medical visit and interactions with their physician.4 The scale was developed based on the conceptual model of patient-centered care,5 and specifically addresses the extent to which the disease and illness experience has been explored (e.g., “To what extent was your main problem(s) discussed today?”), the patient and doctor having found common ground about management of the illness (e.g., “To what extent did you agree with the doctor's opinion about the problem?”), and patient having been understood as the whole person (e.g., “How much would you say that this doctor cares about you as a person?”). Two of 14 scale items were dropped based on pilot test results indicating patient confusion with the questions about the patient and physician role in the visit. The final 12-item scale demonstrated good reliability (Cronbach's α=0.91) with a theoretical range of 1–4, with higher scores indicating more patient-centered consultations.
Statistical Analysis
Descriptive statistics were compared between visits with and without companions using χ2 test, t test, or Wilcoxon rank-sum test. Because of the nature of the sampling procedure, patients were nested within physicians. The perceived patient-centeredness score significantly differed between doctors (F=3.20, P=.002), and the intraclass correlation was 0.122. Following the analytical method of previous studies with a similar sampling procedure,10,19,20 Generalized Estimating Equations (GEE) were used in investigating the relationships of communication process variables with perceived patient-centeredness to account for the within-group correlations among the patients seeing the same physician.21 For the statistical analysis, Stata 8.0 (Stata Corporation, College Station, TX) was used.
RESULTS
Sample Description
One patient was excluded from the analysis because of the incomplete recording resulting from a technical problem. Consequently, the study sample included 145 consultations; 63 medical visits with companions and 82 without a companion. Virtually all patients suffered from a chronic disease, most commonly hypertension, osteoporosis, chronic obstructive pulmonary disease, diabetes, hyperlipidemia, and bronchial asthma. Most patients were well known by their physicians, with the majority of patients (77.4%) having seen their physician more than 10 times prior to the study visit. Table 1 shows the characteristics of the patients and companions. Accompanied patients were significantly older, less educated, and had poorer health status than patients who did not have a visit companion.
Table 1.
Characteristics of the Patients by the Accompaniment Status
| Dyads (N=82) | Triads (N=63) | P Value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Patient | |||||
| Gender | |||||
| Male | 31 | 37.8 | 31 | 49.2 | .151 |
| Female | 51 | 62.2 | 32 | 50.8 | |
| Age (years): mean±SD | 74.8±6.7 | 80.4±7.8 | <.001 | ||
| Educational attainment | |||||
| 9th grade | 15 | 18.3 | 17 | 27.0 | .046 |
| 12th grade | 35 | 42.7 | 29 | 46.0 | |
| 2-year college | 13 | 15.8 | 9 | 14.3 | |
| University or higher | 19 | 23.2 | 7 | 11.1 | |
| Missing | 0 | 0.0 | 1 | 1.6 | |
| Health status (SF-8): mean±SD | 30.4±5.8 | 27.7±5.4 | .005 | ||
| Companion | |||||
| Gender | |||||
| Male | 16 | 25.4 | |||
| Female | 47 | 74.6 | |||
| Age (years): mean±SD | 66.1±11.1 | ||||
| Relationship with the patient | |||||
| Spouse | 32 | 50.8 | |||
| Son/daughter | 21 | 33.4 | |||
| Daughter-in-law | 5 | 7.9 | |||
| Other | 5 | 7.9 | |||
SD, standard deviation.
Consultation Process by Accompaniment Status
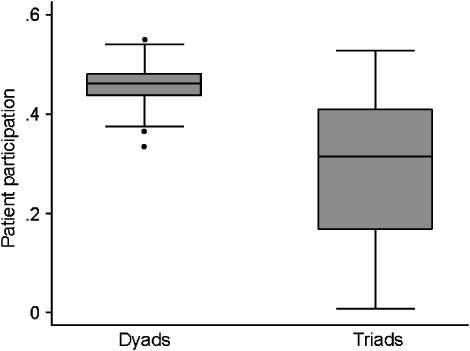
The average consultation length was 10.5 minutes (standard deviation [SD]=5.5). There was no statistically significant difference in consultation length between visits that included a companion and those that did not (median: 10 vs 9 minutes, respectively P=.795). Patient contribution to the medical dialogue, however, was significantly lower when a companion was present. The median patient contribution to the medical dialogue with companions was 32% compared with 46% in visits without a companion (P<.001). This difference was statistically significant, and remained so after controlling for potential confounders including patient age, gender, educational attainment, and health status (P<.001). As shown in Figure 1, it was noteworthy that the interquartile range of patient contribution to the dialogue was relatively narrow in visits without companions, ranging from 33% to 55%, compared with the broad range (1% to 53%) in patient contribution to the dialogue when companions were present.
FIGURE 1.
Patient contribution to the medical dialogue by accompaniment status.
Patient Judgments of Patient-Centeredness
Although the mean score of the perceived patient-centeredness scale was slightly higher in dyads than in triads (3.27±0.49 vs 3.11±0. 47; P=.055), the difference was not statistically significant when controlling for basic patient characteristics.
Length of visit was positively related to patient's ratings of patient-centeredness in both dyads and triads; visits greater than 10 minutes were rated as more patient-centered than shorter visits. When a companion was present during the visit, however, patient's ratings of patient-centeredness and visit length was moderated by the patient's verbal contribution to the medical dialogue. As reflected in Table 2, there was a significant interaction between consultation length and patient contribution to the medical dialogue in the triad sample. That is, patients judged long visits (>10 minutes) as patient-centered regardless of their contribution to the medical dialogue, but short visits (<10 minutes) were rated as patient-centered only when patients were verbally active and engaged. On the other hand, there was no significant interaction between consultation length and patient participation in dyads.
Table 2.
Effect of Patient Contribution to the Medical Dialogue on Perceived Patient-Centeredness
| Dyads (N=82) | Triads (N=63) | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 1 | Model 2 | ||||
| β | P Value | β | P Value | β | P Value | |
| Age | 0.000 | .977 | 0.004 | .536 | 0.010 | .155 |
| Gender | 0.116 | .404 | 0.030 | .772 | 0.017 | .864 |
| Education | 0.000 | .993 | 0.018 | .814 | 0.029 | .556 |
| Health status (SF-8) | 0.014 | .101 | −0.017 | .009 | −0.017 | .032 |
| Consultation length (0: ≤10 minutes, 1: >10 minutes) | 0.435 | .000 | 0.154 | .059 | 0.988 | .007 |
| Patient participation | 0.955 | .656 | 0.849 | .012 | 2.574 | .001 |
| Length × participation | −2.769 | .019 | ||||
DISCUSSION
This study explores the consequences of an increasingly common phenomenon of companion presence during elderly patients' medical visits on the patients' experience of patient-centered care. Our findings suggest that the presence of a companion changes the interaction dynamics of a medical visit and this, in turn, affects patients' perceptions of the physician and the visit. Even after statistically controlling for a variety of characteristics that distinguish patients who are accompanied during the medical visits with those who are not, including older age, gender, education, and health status, patients with visit companions were far less verbally engaged in the medical dialogue than patients who saw their physician alone.
Interestingly, the presence of a companion was not related to significant increases in the length of the visit, suggesting that the verbal activity of the companion was off-set by decreased verbal activity of the patient. It appears that the presence of a patient companion does not necessarily extend visit length. Also, the presence of the companion per se did not decrease the visit patient-centeredness. This is consistent with previous findings suggesting that patient satisfaction and quality of life did not significantly differ between triadic and dyadic encounters after controlling for patient characteristics, although it tended to be lower in triadic encounters.9,13,17
Interestingly, when a companion is present, particularly in brief visits, they may usurp a critical proportion of the patient's “talk time,” resulting in an impression of the visit and the doctor as being less than patient centered. One interpretation of this finding suggests a threshold with regard to patient talk-time that affects judgments of patient-centeredness. This threshold for dialogue appears relatively low and infrequently breached in dyadic encounters of any length. When there are only 2 interactants, it is less likely that patient's contribution to the dialogue would fall below a critical threshold as to affect patient-centered ratings, even in short visits. This interpretation is consistent with several previous studies, all of which are based on dyadic visits which failed to find an association between patient-physician talk ratio and patient satisfaction.19,22,23 In contrast, triads make it easier for one member to refrain from participating in discourse.24 Our previous study has found that companions made a significant contribution to the communication during the visit by providing information and asking the physician questions, in addition to facilitating patient's talk.11 As Beisecker7 has suggested, companions might sometimes take important communication roles away from the patient and reduce the interaction time between physician and patient. As a result, visits with a companion, especially those that are brief, present limited opportunities for even modest patient contribution to the dialogue.
Limitations of This Study
Several limitations and methodologic issues should be noted in interpreting the results of this study. First, the study included a limited number of physicians and patients, attending a single hospital in Tokyo, and agreeing to participate in a tape-recording of their visit. Although relatively few patients and physicians who were asked to participate in the study refused, they may have acted differently than otherwise under these circumstances. Also, the findings may not generalize to other countries and cultures, or other regions and institutions even within Japan. At least, however, our finding of a nonsignificant relationship between patient's talk proportion and perceived patient-centeredness in dyadic consultations is consistent with previous findings from US and the UK research indicating that patient-physician talk ratio was not significantly related to patient satisfaction.22,23 Although social, cultural, or professional education and practice differences between Japanese and Western cultures that may affect the role and influence of the companion should be further explored, our previous study11 found that the functions and contents of the companion's communication role were parallel to the findings of a study in geriatric encounters in the US.10
Second, the relatively small sample size restricts detailed exploration of subgroup differences. In particular, the influence of companion characteristics such as their relationship with the patient should be further explored. Third, because of the lack of visual data, we were not able to distinguish physician's communication toward patients from that toward companions in coding triadic visits. It is plausible that the communication that contains the same function and content differentially affects perceived patient-centeredness depending on to whom it has been directed. Fourth, our study focused on patient satisfaction as an outcome. It is unclear how patient satisfaction and other outcomes of care such as adherence to medical recommendations relate. Additional research will be necessary to establish these connections. Finally, although we have statistically controlled for basic patient characteristics including age, gender, education, and health status, there might have been other factors, such as patient preferences, coping style, and locus of control that could affect patient participation as well as perceived patient-centeredness.25
Implications for Practice and Future Research
Despite the limitations pointed out above, the study findings have implications for both clinical practice and future research in this field. Inasmuch as the population is rapidly aging, accompanied visits are likely to become even more commonplace. It may seem time efficient for physicians to seek and provide information to a companion instead of the elderly patient, especially in time-pressured consultations. However, our findings suggest that this may have a negative impact on patient's perception of the care, in terms of patient-centeredness. Especially in the briefest of visits, it is essential that the opportunity for patient participation in the medical dialogue be safeguarded and that their voice is heard. Since the visit length in Japan is generally shorter than that in the US,26 this finding could be especially true in countries with visit lengths similar to Japan.
It is also possible that the companion presence affects other important outcomes, such as the physician's perception of the visit, regard for the patient and his or her family, or confidence in the effectiveness of the treatment regimen and patient health outcomes. For instance, it has been reported that physicians tend to rely on the accompanying person to manage or supervise the administration of medicines in obtaining compliance with medication regimens from elderly patients.27 In addition, our previous study has suggested that companion's helpfulness was predicted by what patients expected of their companions, and what companions intended and actually did during the visit.28 Further studies at multi-sites with a larger number of participants will be needed to explore the conditions under which the companion may improve or impede visit communication and ultimately the quality of care.
Acknowledgments
This research was supported by a grant from the Pfizer health research foundation. We sincerely thank all physicians, patients, and accompanying persons who participated in this study at the University of Tokyo Hospital, Department of Geriatric Medicine. I express deep gratitude to Drs. Masao Yoshizumi, Koichi Kozaki, Takahide Nagase, and Yasuyoshi Ouchi, who backed up my entry into the field and provided valuable practical advice in conducting the survey.
References
- 1.Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–11. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48:51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 3.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 5.Stewart M, Brown JB, Weston WW, McWhinney IR, McWilliam CL, Freeman TR. Patient-Centered Medicine: TRANSFORMING the Clinical Method. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- 6.Adelman RD, Greene MG, Charon R. The physician-elderly patient-companion triad in the medical encounter: the development of a conceptual framework and research agenda. Gerontologist. 1987;27:729–34. doi: 10.1093/geront/27.6.729. [DOI] [PubMed] [Google Scholar]
- 7.Beisecker AE. The influence of a companion on the doctor-elderly patient interaction. Health Commun. 1989;1:55–70. doi: 10.1207/s15327027hc0101_7. [DOI] [PubMed] [Google Scholar]
- 8.Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Can Fam Physician. 1998;44:1644–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Prohaska TR, Glasser M. Patients' views of family involvement in medical care decisions and encounters. Res Aging. 1996;18:52–69. [Google Scholar]
- 10.Clayman ML, Roter D, issow LS, Bandeen-Roche K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med. 2005;60:1583–91. doi: 10.1016/j.socscimed.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Ishikawa H, Roter DL, Yamazaki Y, Takayama T. Physician-elderly patient-companion communication in Japanese geriatric encounters. Soc Sci Med. 2005;60:2307–20. doi: 10.1016/j.socscimed.2004.08.071. [DOI] [PubMed] [Google Scholar]
- 12.Schilling LM, Scatena L, Steiner JF, Albertson GA, Lin CT, Cyran L, et al. The third person in the room: frequency, role, and influence of companions during primary care medical encounters. J Fam Pract. 2002;51:685–90. [PubMed] [Google Scholar]
- 13.Labrecque MS, Blanchard CG, Ruckdeschel JC, Blanchard EB. The impact of family presence on the physician-cancer patient interaction. Soc Sci Med. 1991;33:1253–61. doi: 10.1016/0277-9536(91)90073-l. [DOI] [PubMed] [Google Scholar]
- 14.Botelho RJ, Lue BH, Fiscella K. Family involvement in routine health care: a survey of patients' behaviors and preferences. J Fam Pract. 1996;42:572–6. [PubMed] [Google Scholar]
- 15.Baker PS, Yoels WC, Clair JM, Allman RM. Laughter in triadic geriatric medical encounters: a transcript-based analysis. Social Perspectives Emotion. 1997;4:179–207. [Google Scholar]
- 16.Coe RM, Prendergast RM. Research note: the formation of coalitions: interaction strategies in triads. Sociol Health Illness. 1985;7:237–47. [Google Scholar]
- 17.Greene MG, Adelman RD, Friedmann E, Charon R. Older patient satisfaction with communication during an initial medical encounter. Soc Sci Med. 1994;38:1279–88. doi: 10.1016/0277-9536(94)90191-0. [DOI] [PubMed] [Google Scholar]
- 18.Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037–44. doi: 10.1016/s0895-4356(98)00095-x. [DOI] [PubMed] [Google Scholar]
- 19.Ishikawa H, Takayama T, Yamazaki Y, Seki Y, Katsumata N. Physician-patient communication and patient satisfaction in Japanese cancer consultations. Soc Sci Med. 2002;55:301–11. doi: 10.1016/s0277-9536(01)00173-3. [DOI] [PubMed] [Google Scholar]
- 20.Wissow LS, Roter D, Larson SM, et al. Mechanisms behind the failure of residents' longitudinal primary care to promote disclosure and discussion of psychosocial issues. Arch Pediatr Adolesc Med. 2002;156:685–92. doi: 10.1001/archpedi.156.7.685. [DOI] [PubMed] [Google Scholar]
- 21.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 22.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102:520–8. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 23.Mead N, Bower P, Hann M. The impact of general practitioners' patient-centredness on patients' post-consultation satisfaction and enablement. Soc Sci Med. 2002;55:283–99. doi: 10.1016/s0277-9536(01)00171-x. [DOI] [PubMed] [Google Scholar]
- 24.Wolf KH. The Sociology of Georg Simmel. New York: Free Press; 1950. [Google Scholar]
- 25.Haug MR, Ory MG. Issues in elderly patient-provider interactions. Res Aging. 1987;9:3–44. doi: 10.1177/0164027587009001001. [DOI] [PubMed] [Google Scholar]
- 26.Stoeckle JD. Encounters Between Patients and Doctors. Cambridge, MA: The MIT Press; 1987. [Google Scholar]
- 27.Coe RM, Prendergast CG, Psathas G. Strategies for obtaining compliance with medications regimens. J Am Geriatr Soc. 1984;32:589–94. doi: 10.1111/j.1532-5415.1984.tb06138.x. [DOI] [PubMed] [Google Scholar]
- 28.Ishikawa H, Roter DL, Yamazaki Y, Hashimoto H, Yano E. Patient perceptions of companion helpfulness during geriatric medical visits. Patient Educ Couns (forthcoming) doi: 10.1016/j.pec.2005.02.010. [DOI] [PubMed] [Google Scholar]