Abstract
Background
Thus far, incident reporting in health care has relied on health professionals. However, patients too may be able to signal the occurrence of undesirable events.
Objective
To estimate the frequency of undesirable events reported by recently discharged patients, and to identify correlates of undesirable events.
Design
Mailed patient survey.
Setting
Swiss public teaching hospital.
Participants
Adult patients (N=1,518) discharged from hospital.
Measurements
Self-reports of 27 undesirable events during hospitalization, including 9 medical complications, 9 interpersonal problems, and 9 incidents related to the health care process.
Results
Most survey respondents (1,433, 94.4%) completed the section about undesirable events, and 725 (50.6%) reported at least 1 event. The most frequent events were phlebitis (11.0%), unavailable medical record (9.5%), failure to respect confidentiality (8.4%), and hospital-acquired infection (8.2%). The odds of an unfavorable rating increased with each additional interpersonal problem (odds ratio [OR] 1.6, 95% confidence interval [CI] 1.3 to 1.8), each additional process-related problem (OR 1.5, 95% CI 1.3 to 1.9), but not with each additional medical complication (OR 1.0, 95% CI 0.9 to 1.2). Longer duration of stay, poor health, and depressed mood were all related to a greater reported frequency of undesirable events.
Conclusion
Patients are able to report undesirable events that occur during hospital care. Such events occur in about a half of the hospitalizations, and have a negative impact on satisfaction with care.
Keywords: incidents, complications, patient safety, patient satisfaction, hospitalization
Undesirable events in health care attract increasing attention.1–5 So far, the focus has been on medical errors and complications such as adverse drug events,6–8 hospital-onset infections,9,10 pressure ulcers,11,12 and perioperative complications.13,14 Most current knowledge is based on reviews of medical records1–4 and on reports of incidents by health care staff.14–17 Both sources of information have strengths, but also weaknesses.18–20 Whether a given incident is reported will depend on factors such as the safety culture of the organization, the likelihood of personal blame or of a malpractice procedure, the ease of completing the report, and how interesting the incident appears to those involved.21 Similarly, medical records are also imperfect sources of data about adverse events, because many events may go unrecorded.
An untapped source of information about undesirable events are the patients themselves.22 Patients are prime witnesses to the health care they receive, and most are capable of noticing problems or incidents.23–25 Most currently used patient satisfaction or patient report questionnaires inquire about the general pattern of care, averaged over the hospital stay, not about discrete exceptional or atypical events. Patients may be particularly apt to report on interpersonal problems, such as lack of respect or insufficient information, and on incidents related to the delivery of care, such as the scheduling of tests or the distribution of medications. On the other hand, patients may be less likely to notice deficiencies in technical quality of health care and in the appropriateness of medical decisions.
In this study, we asked patients about the frequency of undesirable events that may occur in hospital, and identified patient and hospital stay characteristics that are associated with such reports. We also examined the association between the occurrence of incidents and the global assessment of the hospital stay.
METHODS
Design and Setting
Data were obtained as part of the 2001 routine patient opinion survey at Geneva University Hospitals, in Geneva, Switzerland.26,27 Participants were all adult patients discharged alive from hospital. Because it carried minimal risk, the project was exempted from formal review by the hospital research ethics committee.
Study Variables
The core of the questionnaire was the Picker patient opinion instrument,28,29 in French.30 This questionnaire includes mostly patient report questions on various aspects of care received at the hospital. An example is an item that asks the patient whether he or she felt treated with respect and dignity during the hospital stay, with possible answers “yes, always,”“yes, sometimes,”“no.” The questionnaire also includes evaluative questions, particularly a global rating of hospital care, dichotomized for this analysis as unfavorable (“good,”“fair” or “poor”) versus favorable (“excellent” or “very good”). Only these 2 items from the Picker survey—respect and dignity, and the global rating—were analyzed in this paper.
The main variables in this analysis were patient reports of undesirable events. We sought to develop a list of undesirable events that are noticeable to patients and that occur commonly in a general hospital. The list was compiled based on the literature, a review of common patient complaints and incidents reported within the hospital, and on patient comments during pretests. Undesirable events were described in lay language. The event list was pretested iteratively among about 15 hospitalized patients in total. The pretest focused on the understanding patients had of the proposed items, and on their opinions of which undesirable events should be included. Several event descriptions were modified as a result. The main problem we encountered was with negatively worded statements, such as “You were given a drug that was not intended for you,” which some respondents had trouble answering by yes or no. Rephrasing the statement in the positive whenever possible, or bolding the negative (“You were given a drug that was not intended for you”), appeared to reduce these difficulties.
The section on undesirable events started thus: “Complications, problems, or unexpected or unpleasant situations sometimes happen during a hospital stay. Please indicate whether you encountered the following situations during your stay. (Check one answer on each line) Yes-No.” Followed a single list of 27 undesirable events: 9 interpersonal problems, 9 medical complications, and 9 process problems (Table 1).
Table 1.
Frequencies of Undesirable Events During Hospitalization Reported by Former Inpatients (N=1,433) and Unadjusted Associations With Unfavorable Overall Assessment of Care (N=1,417), Geneva, Switzerland, 2001
| N (%) | Odds Ratio (95% CI) for Unfavorable Rating of Care* | ||
|---|---|---|---|
| Interpersonal problems | |||
| Doctors or nurses did not respect confidentiality | 120 (8.4) | 1.4 | (1.0 to 2.1) |
| Doctors or nurses neglected information you gave them | 99 (6.9) | 6.4 | (3.9 to 10.6) |
| Your consent was not obtained before a test or an intervention | 87 (6.1) | 2.1 | (1.3 to 3.3) |
| You were handled or moved with roughness | 78 (5.4) | 5.2 | (3.0 to 8.9) |
| You were not given due respect | 77 (5.4) | 5.9 | (3.4 to 10.3) |
| You felt rejected by health care team | 58 (4.0) | 9.7 | (4.5 to 20.6) |
| You were pushed to undergo a test or a treatment against your wish | 47 (3.3) | 3.9 | (2.0 to 7.4) |
| You were addressed informally without your agreement | 36 (2.5) | 2.5 | (1.3 to 5.1) |
| You felt physically abused | 27 (1.9) | 5.3 | (2.1 to 13.1) |
| Medical complications | |||
| You developed an inflammation of a vein (phlebitis) because of an intravenous line | 158 (11.0) | 1.7 | (1.2 to 2.4) |
| You acquired an infection in the hospital | 118 (8.2) | 2.0 | (1.3 to 2.9) |
| You experienced an allergic reaction to a drug | 110 (7.7) | 1.3 | (0.9 to 1.9) |
| You bled a lot after an operation or a catheterism | 77 (5.4) | 1.0 | (0.6 to 1.6) |
| You were transferred to intensive care because of a complication that occurred in hospital | 69 (4.8) | 1.4 | (0.9 to 2.3) |
| You developed a pressure ulcer (skin wound) in hospital | 68 (4.7) | 1.5 | (0.9 to 2.5) |
| You had to be reoperated urgently within 3 days of an initial operation | 46 (3.2) | 1.4 | (0.8 to 2.6) |
| You were injured (fracture, wound, …) in a fall at the hospital | 32 (2.2) | 2.1 | (1.0 to 4.2) |
| You tolerated very poorly a blood transfusion | 22 (1.5) | 1.3 | (0.6 to 3.2) |
| Health care process problems | |||
| Your medical record or radiograms were unavailable when needed | 136 (9.5) | 1.8 | (1.3 to 2.6) |
| You did not receive enough painkillers | 92 (6.4) | 5.4 | (3.3 to 8.9) |
| Doctors made a wrong diagnosis | 56 (3.9) | 3.9 | (2.1 to 7.1) |
| A test could not be done because of equipment breakdown | 52 (3.6) | 1.4 | (0.8 to 2.4) |
| A test was repeated needlessly, by mistake | 52 (3.6) | 4.6 | (2.4 to 8.7) |
| You were given a drug that was not intended for you | 35 (2.4) | 4.2 | (1.9 to 9.1) |
| You were confused with another patient during a test or a treatment | 27 (1.9) | 2.5 | (1.1 to 5.6) |
| A test was cancelled by mistake | 25 (1.7) | 3.2 | (1.4 to 7.4) |
| You were operated on the wrong side | 10 (0.7) | 2.2 | (0.6 to 7.8) |
Care rated as poor, fair, or good, versus very good or excellent.
Other patient characteristics we examined in relation to reports of undesirable events were patient age, sex, length of hospital stay, perceived health status, and “feeling downhearted and blue” in the past 4 weeks. The latter measures were single items from the SF-36 health survey version 2,31 translated into French.32
Data Analysis
First, we compared respondents who skipped the section on undesirable events to those who completed it. Among the latter, we determined the frequency of each adverse event.
Second, we analyzed the proportions of patients who rated their care unfavorably according to the occurrence of each adverse event. We computed unadjusted odds ratios (ORs) of rating care unfavorably for each adverse event. Then we built a multiple logistic regression model to identify events that were independently associated with unfavorable assessments. We used a forward modeling procedure, starting with the events that were most strongly associated with unfavorable ratings, adding or withdrawing covariates one by one.
Then, we analyzed the association between patient's characteristics and the occurrence of any (one or more) of the 9 medical complications, any 9 interpersonal problems, and any 9 health care process problems proposed in our list, using logistic regression.
Finally, to explore the consistency of patient reports, we examined frequencies of the 9 interpersonal problems across answers to the Picker item on feeling treated with respect and dignity. For all regression models, we used a likelihood ratio test for significance testing; P<.05 was considered statistically significant.
RESULTS
Of 2,156 eligible patients, 1,518 (70.4%) returned the questionnaire, and 1,433 (66.5%) answered the section about undesirable events. Respondents were on average 56 years old (SD 19.3, range 18 to 98). There were more women than men among the respondents (Table 2, column 1). The mean length of stay was 13.2 days (median 7, interquartile range: 4, 14). Patients were discharged from departments of surgery (446, 31.1%), medicine (386, 26.9%), neurosciences-dermatology (223, 15.6%), gynecology-obstetrics (204, 14.2%), psychiatry (91, 6.4%), and geriatrics (83, 5.8%). At the time of the survey, about a quarter of the respondents described their health as fair or poor, and about 15% reported feeling downhearted and blue all or most of the time (Table 2).
Table 2.
Distributions of Patient Characteristics and Associations with the Occurrence of One or More Undesirable Events of each Category (Univariate Odds Ratios)
| N (%) | Interpersonal Problems | Complications | Process Problems | ||||
|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | ||
| Sex | |||||||
| Female | 797 (55.6) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Male | 636 (44.4) | 0.9 | 0.7 to 1.2 | 1.1 | 0.8 to 1.4 | 1.1 | 0.8 to 1.4 |
| Age (years)* | |||||||
| 18 to 44 | 475 (33.1) | 1.8 | 1.3 to 2.4 | 0.6 | 0.5 to 0.8 | 1.4 | 1.0 to 1.8 |
| 45 to 64 | 419 (29.2) | 1.2 | 0.9 to 1.6 | 0.8 | 0.6 to 1.1 | 1.5 | 1.1 to 2.0 |
| ≥ 65 | 539 (37.6) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Length of stay (days)* | |||||||
| 2 to 10 | 927 (64.7) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| 11 to 30 | 385 (26.9) | 1.3 | 1.0 to 1.8 | 1.5 | 1.2 to 2.0 | 1.0 | 0.7 to 1.4 |
| Over 30 | 121 (8.4) | 1.6 | 1.1 to 2.6 | 3.3 | 2.2 to 4.9 | 1.9 | 1.2 to 2.9 |
| Perceived health status*‡ | |||||||
| Excellent or very good | 370 (26.5) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
| Good | 654 (46.8) | 1.2 | 0.9 to 1.6 | 1.6 | 1.2 to 2.2 | 2.0 | 1.4 to 2.9 |
| Fair or poor | 373 (26.7) | 1.8 | 1.3 to 2.5 | 2.2 | 1.6 to 3.1 | 3.0 | 2.1 to 4.4 |
| Feeling downhearted and blue during the past 4 weeks*§ | |||||||
| All or good part of the time | 212 (15.3) | 3.6 | 2.5 to 5.0 | 1.5 | 1.1 to 2.1 | 2.7 | 1.9 to 3.8 |
| Some of the time | 517 (37.1) | 1.7 | 1.3 to 2.2 | 1.2 | 0.9 to 1.6 | 1.5 | 1.1 to 1.9 |
| A little of the time or never | 666 (47.7) | 1.0 | Reference | 1.0 | Reference | 1.0 | Reference |
Test for linear trend statistically significant (P<.05) for all 3 dependent variables.
Missing: 85.
Missing: 36.
Missing: 38.
Nonrespondents
Among the 1,518 survey participants, 85 (5.6%) skipped the section on undesirable events inappropriately. Those who skipped this section were older (61.5 vs 55.6 years, P=.007) than those who answered it, and less likely to have had a previous hospitalization during the last 6 months (17% vs 30.6%, P=.034). The distributions of other sociodemographic characteristics were similar in the 2 groups, as was the overall satisfaction with care (59.4% respondents rated their care as “excellent” or “very good” vs 61.8% among nonrespondents, P=.67).
Undesirable Events
Participants reported 1,814 undesirable events, or 1.3 per person (Table 1). Only 708 (49.4%) reported none, 328 (22.9%) reported 1 event, 171 (11.9%) 2 events, 92 (6.4%) 3 events, 48 (3.3%) 4 events, 33 (2.3%) 5 events, and 53 (3.8%) more than 5 events. Among the latter, 4 participants (0.3%) reported 20 or more events. While these responses appear implausible, they were included in further analysis. About one quarter of respondents signaled at least 1 interpersonal problem (337, 23.5%), medical complication (429, 29.9%), and process-related problem (337, 23.5%).
Association with Global Rating of Care
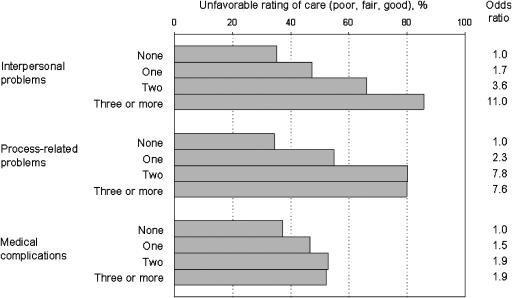
The mean number of undesirable events was associated with the global rating of care (“excellent:” 0.7 events, “very good:” 0.9 events, “good:” 1.4 events, “fair:” 3.6 events, “poor:” 7.2 events, P for linear trend <.001). The proportion of patients who rated their health care unfavorably (poor, fair or good, as opposed to very good or excellent) increased with increasing numbers of interpersonal and process-related problems, but less so with increasing numbers of medical complications (Fig. 1). In a multiple logistic regression model that included 3 variables representing the numbers of each type of event, the odds of an unfavorable rating increased with each additional interpersonal problem (OR 1.6, 95% confidence interval (CI) 1.3 to 1.8), each additional process-related problem (OR 1.5, 95% CI 1.3 to 1.9), but not with each additional medical complication (OR 1.0, 95% CI 0.9 to 1.2).
FIGURE 1.
Proportions of patients who rated health care received in hospital as poor, fair, or good (as opposed to very good or excellent) across increasing numbers of undesirable events, for interpersonal problems, process-related problems, and medical complications.
When events were examined one by one (Table 1), all 9 interpersonal problems, 7 of the process-related problems, and 3 among the medical complications were associated with significantly higher odds of rating care unfavorably (as “poor,”“fair,” or “good”). The associations were particularly strong, with ORs in excess of 5, for 5 of the interpersonal problems, 1 process-related problem, and none of the medical complications. In multivariate analysis, the following events were independently associated with an unfavorable assessment: having felt rejected by the health care team (OR 4.3, 95% CI 1.9 to 9.7), reporting that health care staff neglected important information (OR 3.5, 95% CI 2.0 to 5.9), not getting enough painkillers (OR 3.5, 95% CI 2.1 to 6.0), needless repetition of a test (OR 2.8, 95% CI 1.4 to 5.7), and having been handled with roughness (OR 2.6, 95% CI 1.4 to 4.7). Adjustment for patient characteristics (age, sex, health status, feeling depressed) and for the hospital department did not change these results (data not shown).
Risk Factors for Undesirable Events
The frequency of reports of undesirable events was similar for men and for women (Table 2). On the other hand, the occurrence of all categories of undesirable events was associated with longer hospital stays, worse perceived health, and higher level of sadness. Older patients reported more medical complications but fewer interpersonal and process problems than younger patients. Depressed mood was most strongly associated with interpersonal problems.
Interpersonal Problems
We examined reports of undesirable events across answers to the global Picker survey item related to respect and dignity (Table 3). All 9 problem reports were associated with the more global assessment of the Picker survey, but the strength of the association varied considerably among events. The strongest associations were with reports of disrespect (which is understandable given the similar wording), feeling rejected by the team, being handled with roughness, and neglect of information given to doctors and nurses.
Table 3.
Reports of Interpersonal Problems Across Answers to the Item on Respect and Dignity from the Picker Survey
| Interpersonal Problem | Percent Respondents who Reported the Undesirable Event Across Levels of Picker Item | ||
|---|---|---|---|
| Felt Treated with Respect and Dignity During the Hospital Stay* | |||
| Yes, Always (N=1,197) | Yes, Sometimes (N=159) | No (N=93) | |
| Doctors or nurses did not respect confidentiality | 7.8 | 7.5 | 30.2 |
| Doctors or nurses neglected information you gave them | 4.2 | 13.8 | 58.1 |
| Your consent was not obtained before a test or an intervention | 4.8 | 13.2 | 16.3 |
| You were handled or moved with roughness | 2.7 | 13.8 | 48.8 |
| You were not given due respect | 1.7 | 15.1 | 72.1 |
| You felt rejected by health care team | 0.8 | 14.5 | 55.8 |
| You were pushed to undergo a test or a treatment against your wish | 2.3 | 5.0 | 23.3 |
| You were addressed informally without your agreement | 1.6 | 4.4 | 18.8 |
| You felt physically abused | 0.8 | 4.4 | 23.3 |
All linear trend tests <0.001.
DISCUSSION
About half of former inpatients reported at least 1 undesirable event during their hospitalization, whether a medical complication, an interpersonal problem, or a health care process problem. Undesirable events that reflected interpersonal problems were most strongly associated with unfavorable ratings of care overall, in contrast with medical complications, which influenced only weakly the global ratings.
How Trustworthy are Patient Reports of Undesirable Events?
A key issue in this study is the validity of the information obtained. The prevalence of undesirable events reported by patients was near 50%, considerably higher than estimates derived from reviews of medical records.1–4 This raises a red flag. However, this estimate is in the same range as the cumulated incidence of 46% of adverse events noted by ethnographers who observed routine patient care.33 Possibly, record reviews underestimate the frequency of undesirable events, and patient reports provide a more realistic picture.
There is good reason to believe that patient reports of interpersonal problems are trustworthy, since such events can only be meaningfully assessed by patients. The increasing number of interpersonal problems across a more global statement of feeling treated with respect and dignity can be interpreted as evidence of construct validity for both the event reports and the Picker survey item. Similarly, patients can be considered as trustworthy reporters of those process problems that are noticeable. In contrast, patients are probably not in a position to signal other process-related problems, such as errors in medical decision making.
Whether patients can meaningfully assess medical complications is debatable. Limited independent evidence suggests that patients were not far off. For instance, 8% of patients reported a nosocomial infection, consistent with the prevalence of 11% measured at this hospital.10 Patient reported frequency of skin lesions was 4.9%, as compared with a prevalence at our hospital of 3.1% for pressure ulcers of stage 2 or greater.11 The patient-reported frequency of drug-related events of 8% is also compatible with the literature.34 However, we cannot exclude a combination of underreporting by some patients and over-reporting by others to account for this concordance.
On the other hand, other self-reports appear problematic. A handful of respondents reported >20 types of undesirable events. A surprising total of 10 patients (0.7%) reported a wrong site operation, including 3 who were discharged from psychiatry, 3 from internal medicine, and 1 from geriatrics. We do not know if these patients were simply confused, if they referred mistakenly to past events, or if they interpreted the term “operated on” loosely, including for instance repeated attempts at inserting a central intravenous line, or an unproductive needle biopsy. Nevertheless, such instances were rare (<1% of respondents). It is possible that in any large-scale self-completed survey, a small percentage of responses—perhaps in the 0.5% to 2% range—are just plain wrong. This would be no different than most measures in medicine—laboratory tests, imaging procedures, etc.
Variables Associated with Undesirable Events
Not all undesirable events were equally associated with patient dissatisfaction, as reflected by ratings of care on a scale between excellent and poor. Low ratings were most notable for patients who reported interpersonal problems. Patients who felt rejected or disrespected by the health care team were particularly unhappy with the care they received. These results underscore the importance of patient-centered care for patients' assessment of quality. Most problems related to the process of care were also associated with lower patient ratings. In contrast, the impact of medical complications on patient satisfaction was minimal. Patients may consider complications as unavoidable, or as consequences of their disease. The pattern of these associations is comparable to associations between problem scores and patient satisfaction reported by Jenkinson et al.35: overall assessment of care was most strongly associated with emotional support and respect for patient preferences.
Several patient characteristics were associated with more frequent reporting of undesirable events. In particular, patients who felt depressed reported strikingly more interpersonal problems. Depressed patients may interpret more human interactions in an unfavorable light. Alternatively, the health care team may behave differently towards depressed patients than towards patients who are in better spirits. Limited evidence suggests that cheerful and outgoing patients may be treated differently by hospital staff.36
Quite logically, the frequency of undesirable events was associated with length of stay. The cumulative incidence of problems can only increase over time. That this association was strongest for medical complications also makes sense, as several complications may extend the length of stay. From these cross-sectional data, we cannot distinguish whether the complication arose because of longer exposure to hospital care, or whether its occurrence extended the hospital stay.
How do Event Reports Relate to Other Types of Patient Surveys?
From a methodologic standpoint, asking patients about the occurrence of undesirable events lies squarely in the tradition of “reports”—as opposed to “ratings”—of health care.37,38 By asking patients about discrete undesirable events, our approach differs somewhat from questionnaires such as the Picker instrument,29,30 which enquire about the usual pattern of care during the hospital stay. To link the various forms of patient queries, we propose the following model: at the most elementary level, the patient experiences discrete events, good or bad, during the hospital stay. This is the level we explored with reports of undesirable events (however, we did not ask about positive events). Summarizing this experience over the hospital stay, the patient can then report on the general patterns of care. This is the level explored by most Picker survey items. Further still, the patient forms a global impression, or rating, of care, which is based in part on the average pattern of care, but also on other elements, such as the patient's expectations, previous experiences, or tendency to be lenient or severe in his or her assessments.39
Each type of patient query has its own merits and weaknesses. Event reports are the most factual and concrete, but may misrepresent the bigger picture. Ratings are effective summaries, but may not be easy to translate into corrective actions. Reports of usual patterns of care are inbetween these 2 extremes. We believe that all 3 types of questions—ratings, reports of usual patterns of care, and reports of discrete events—are potentially useful for quality management. For instance, all 9 interpersonal problems were associated with the more global Picker item on respect and dignity (Table 3), but the strength of the association varied considerably between events. Whether the summary item should be used or the more detailed event reports will depend on the desired level of detail of the information to be collected. Furthermore, the categorization as event-summary report rating is a convenient oversimplification, as the distinction between the types of questions may be blurry. For instance, “feeling rejected by the health care team” can be either a time-limited experience akin to an event, or a characterization of the whole hospitalization.
Limitations and Strengths
The main limitation of the study is the lack of independent verification of reported events. To protect the respondents' privacy, we did not have access to their medical records, and in any case, a record-based validation procedure is difficult to imagine for interpersonal problems. On balance, as discussed above, we believe that reports by most patients were globally trustworthy, with few exceptions. Another concern is that hospital stays are longer in Switzerland than in many other countries, so the external validity of our findings is uncertain. Participation in the survey was good, and a separate analysis suggested that selection bias was likely modest.27 The main strength of this study is that patients were consulted regarding undesirable events.
Conclusion
The study suggests that incident reporting, a method traditionally used by professionals to identify medical errors and other threats to patient safety, may be effectively used by patients to identify problems related to patient-centeredness and to the delivery of care. Contrary to incident reports by professionals, which are influenced by local regulations and the culture of safety, reports of undesirable events by patients may have value as a quantitative indicator of quality and safety.
Acknowledgments
The authors thank Véronique Kolly, RN, for assistance with data collection. The study was funded by the Quality of Care Program, Geneva University Hospitals.
References
- 1.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–6. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 2.Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–84. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- 3.Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38:261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ. 2001;322:517–9. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leape LL, Berwick BM, Bates DW. What practices will most improve safety? Evidence-based medicine meets patient safety. JAMA. 2002;288:501–7. doi: 10.1001/jama.288.4.501. [DOI] [PubMed] [Google Scholar]
- 6.Scott HD, Thacher-Renshaw A, Rosenbaum SE, et al. Physician reporting of adverse drug reactions. Results of the Rhode Island adverse drug reaction reporting project. JAMA. 1990;263:1785–8. [PubMed] [Google Scholar]
- 7.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 8.Runciman WB, Roughhead EE, Semple SJ, Adams RJ. Adverse drug events and medication errors in Australia. Int J Qual Health Care. 2003;15(suppl 1):i49–59. doi: 10.1093/intqhc/mzg085. [DOI] [PubMed] [Google Scholar]
- 9.Vincent JL, Bihari DJ, Suter PM, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European prevalence of infection in intensive care (EPIC) Study. JAMA. 1995;274:639–44. [PubMed] [Google Scholar]
- 10.Sax H, Hugonnet S, Harbarth S, Herrault P, Pittet D. Variation in nosocomial infection prevalence according to patient care setting: a hospital-wide survey. J Hosp Infect. 2001;48:27–32. doi: 10.1053/jhin.2001.0961. [DOI] [PubMed] [Google Scholar]
- 11.Perneger TV, Héliot C, Raë AC, Borst F, Gaspoz JM. Hospital-acquired pressure ulcers: risk factors and use of preventive devices. Arch Intern Med. 1998;158:1940–5. doi: 10.1001/archinte.158.17.1940. [DOI] [PubMed] [Google Scholar]
- 12.Bours GJ, Halfens RJ, Candel MJ, Grol RT, Abu-Saad HH. Pressure ulcer audit and feedback project across multi-hospital settings in the Netherlands. Int J Qual Health Care. 2004;16:211–8. doi: 10.1093/intqhc/mzh034. [DOI] [PubMed] [Google Scholar]
- 13.Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229–35. doi: 10.1056/NEJMsa021721. [DOI] [PubMed] [Google Scholar]
- 14.Runciman WB, Sellen A, Webb RK, et al. The Australian incident monitoring study. Errors, incidents and accidents in anaesthetic practice. Anaesth Intens Care. 1993;21:506–19. doi: 10.1177/0310057X9302100506. [DOI] [PubMed] [Google Scholar]
- 15.Witham MD, Kendall PA. A prospective, physician self-reported adverse incident audit on a general medical unit. J Qual Clin Pract. 2001;21:61–5. doi: 10.1046/j.1440-1762.2001.00413.x. [DOI] [PubMed] [Google Scholar]
- 16.Welsh CH, Pedot R, Anderson RJ. Use of morning report to enhance adverse event detection. J Gen Intern Med. 1996;11:454–60. doi: 10.1007/BF02599039. [DOI] [PubMed] [Google Scholar]
- 17.Weingart SN, Callanan LD, Ship AN, Aronson MD. A physician-based voluntary reporting system for adverse events and medical errors. J Gen Intern Med. 2001;16:809–14. doi: 10.1111/j.1525-1497.2001.10231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas EJ, Petersen LA. Measuring errors and adverse events in health care. J Gen Intern Med. 2003;18:61–7. doi: 10.1046/j.1525-1497.2003.20147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murff HJ, Patel VL, Hripcsak G, Bates DW. Detecting adverse events for patient safety research: a review of current methodologies. J Biomed Inform. 2003;36:131–43. doi: 10.1016/j.jbi.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Michel P, Quenon JL, de Sarasqueta AM, Scemama O. Comparison of three methods for estimating rates of adverse events and rates of preventable adverse events in acute care hospitals. BMJ. 2004;328:199–202. doi: 10.1136/bmj.328.7433.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waring JJ. A qualitative study of the intra-hospital variations in incident reporting. Int J Qual Health Care. 2004;16:347–52. doi: 10.1093/intqhc/mzh068. [DOI] [PubMed] [Google Scholar]
- 22.Cleary PD, Edgman-Levitan S. Health care quality. Incorporating consumer perspectives. JAMA. 1997;278:1608–12. [PubMed] [Google Scholar]
- 23.Vincent CA, Coulter A. Patient safety: what about the patient? Qual Saf Health Care. 2002;11:76–80. doi: 10.1136/qhc.11.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van den Bemt PM, Egberts AC, Lenderink AW, et al. Adverse drug events in hospitalized patients. A comparison of doctors, nurses and patients as sources of reports. Eur J Clin Pharmacol. 1999;55:155–8. doi: 10.1007/s002280050611. [DOI] [PubMed] [Google Scholar]
- 25.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–7. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 26.Bovier PA, Charvet A, Cleopas A, Vogt N, Perneger TV. Self-reported management of pain in hospitalized patients: link between process and outcome. Am J Med. 2004;117:569–74. doi: 10.1016/j.amjmed.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 27.Perneger TV, Chamot A, Bovier PA. Non-response bias in a survey of patient perceptions of hospital care. Med Care. 2005;43:374–80. doi: 10.1097/01.mlr.0000156856.36901.40. [DOI] [PubMed] [Google Scholar]
- 28.Cleary PD, Edgman-Levitan S, Roberts M, et al. Patients evaluate their hospital care: a national survey. Health Aff (Milwood) 1991;10:254–67. doi: 10.1377/hlthaff.10.4.254. [DOI] [PubMed] [Google Scholar]
- 29.Jenkinson C, Coulter A, Bruster S. The picker patient experience questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14:353–8. doi: 10.1093/intqhc/14.5.353. [DOI] [PubMed] [Google Scholar]
- 30.Perneger TV, Kossovsky MP, Cathieni F, di Florio V, Burnand B. A randomized trial of four patient satisfaction questionnaires. Med Care. 2003;41:1343–52. doi: 10.1097/01.MLR.0000100580.94559.AD. [DOI] [PubMed] [Google Scholar]
- 31.Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53:46–50. doi: 10.1136/jech.53.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leplège A, Ecosse E, Verdier A, Perneger TV. The French SF-36 health survey: translation, cultural adaptation, and preliminary psychometric evaluation. J Clin Epidemiol. 1998;51:1013–23. doi: 10.1016/s0895-4356(98)00093-6. [DOI] [PubMed] [Google Scholar]
- 33.Andrews LB, Stocking C, Krizek T, et al. An alternative strategy for studying adverse events in medical care. Lancet. 1997;349:309–13. doi: 10.1016/S0140-6736(96)08268-2. [DOI] [PubMed] [Google Scholar]
- 34.Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279:1200–5. doi: 10.1001/jama.279.15.1200. [DOI] [PubMed] [Google Scholar]
- 35.Jenkinson C, Coulter A, Bruster S, Richards N, Chandola T. Patients' experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care. 2002;11:335–9. doi: 10.1136/qhc.11.4.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Escher M, Perneger TV, Chevrolet JC. National questionnaire survey on what influences doctors' decisions about admission to intensive care. BMJ. 2004;329:425–9. doi: 10.1136/bmj.329.7463.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cleary PD, Lubalin J, Hays RD, Short PF, Edgman-Levitan S, Sheridan S. Debating survey approaches (letter) Health Aff (Milwood) 1998;17:265–6. doi: 10.1377/hlthaff.17.1.265. [DOI] [PubMed] [Google Scholar]
- 38.Allen HM, Rogers WH. Debating survey approaches: the authors respond (letter) Health Aff (Milwood) 1998;17:266–8. [Google Scholar]
- 39.Perneger TV. Adjustment for patient characteristics in satisfaction surveys. Int J Qual Health Care. 2004;16:433–5. doi: 10.1093/intqhc/mzh090. [DOI] [PubMed] [Google Scholar]