Abstract
OBJECTIVE
To explore colorectal cancer (CRC) screening knowledge, attitudes, barriers, and preferences among urban African Americans as a prelude to the development of culturally appropriate interventions to improve screening for this group.
DESIGN
Qualitative focus group study with assessment of CRC screening preferences.
SETTING
Community health center serving low-income African Americans.
PARTICIPANTS
Fifty-five self-identified African Americans over 40 years of age.
MEASUREMENTS AND MAIN RESULTS
Transcripts were analyzed using an iterative coding process with consensus and triangulation on final thematic findings. Six major themes were identified: (1) Hope—a positive attitude toward screening, (2) Mistrust—distrust that the system or providers put patients first, (3) Fear—fear of cancer, the system, and of CRC screening procedures, (4) Fatalism—the belief that screening and treatment may be futile and surgery causes spread of cancer, (5) Accuracy—a preference for the most thorough and accurate test for CRC, and (6) Knowledge—lack of CRC knowledge and a desire for more information. The Fear and Knowledge themes were most frequently noted in transcript theme counts. The Hope and Accuracy themes were crucial moderators of the influence of all barriers. The largest number of participants preferred either colonoscopy (33%) or home fecal occult blood testing (26%).
CONCLUSIONS
Low-income African Americans are optimistic and hopeful about early CRC detection and believe that thorough and accurate CRC screening is valuable. Lack of CRC knowledge and fear are major barriers to screening for this population along with mistrust, and fatalism.
Keywords: colorectal cancer, screening, African American, minority, qualitative
Colorectal cancer (CRC) is the second leading cause of cancer death in the U.S.1,2 Research shows that clinical screening methodologies can reduce both the incidence of new cases and deaths from this disease.3–12 Despite guidelines for CRC screening,13,14 the prevalence of CRC screening remains low. The 2001 Behavioral Risk Factor Surveillance System showed that 53.1% of the population ≥50 years had received fecal occult blood testing (FOBT) within the past 12 months or a sigmoidoscopy or colonoscopy within the last 10 years.
Studies show CRC screening disparities between whites and African Americans,15–18 especially for sigmoidoscopy.19–22 African Americans have exhibited higher rates of late-stage CRC diagnosis and less overall decline in colorectal deaths than whites over the past decade.23–25
Barriers to CRC screening include the inconvenient or impractical nature of the tests,26–29 the embarrassing or unpleasant nature of the tests,28,29 fatalistic cancer beliefs,30,31 and participants not wanting to know that something is wrong.28,32,33 Studies of African Americans have shown that these barriers and others, such as lack of physician recommendation, limited CRC knowledge, and the uncomfortable nature of tests, may contribute to inadequate screening16,34–36 Although prior qualitative studies have explored how knowledge, socio-culturally mediated attitudes and perceptions, and testing preferences influence screening for breast and prostate cancer among African Americans,37–40 few qualitative studies have been conducted with African Americans on CRC screening.20,41,42 These qualitative studies had enrolled from multiethnic populations and had not specifically focused on the attitudes, opinions, and preferences of African Americans. The purpose of our focus group study was to explore CRC screening knowledge, attitudes, barriers, and preferences among urban African Americans as a prelude to the development of culturally appropriate interventions to improve CRC screening rates.
METHODS
Study Design
We used focus groups to obtain in-depth information regarding beliefs, opinions, and perceptions of cancer, CRC, cancer screening in general, and CRC screening specifically.43–46
Setting
All focus group participants were recruited from a large, urban community health center in a Mid-Western City.
Participants
Study staff approached individuals in the health center's main lobby to ask about participation. All individuals (primary care patients and visitors) ≥50 years who self-identified as African American and were without obvious mental or cognitive impairment were considered eligible. During recruitment, potential participants were informed of the date, place, and time of the next focus group scheduled and were asked whether they might be able to attend. Participants were not referred to study recruiters by health care providers or others. No attempt was made to divide or stratify focus groups by gender or other factors. This decision was based on our need to collect general data on the socio-culturally mediated opinions and perceptions of African Americans toward CRC screening. Focus group participants did not know each other prior to participating in groups. They were told that they would receive a $20 gift card as reimbursement for their time spent in getting to and participating in the focus group. Fifty-five participants attended 6 focus group sessions.
The entire study protocol was reviewed and approved by the University of Kansas Medical Center Human Subjects Committee and appropriate officials at Swope Parkway Health Center.
Instruments
Study staff used a short survey at the beginning of each session to assess CRC knowledge of focus group participants. The questions asked participants to identify the recommended age at which CRC screening should commence and to name or describe one or more CRC screening tests. At the end of the session, a longer, 18-question, anonymous survey assessed participant CRC knowledge and demographics.
A moderator's guide was based on previous studies of CRC and other cancer screening within African-American populations. The guide was designed to explicitly assess African-American's thoughts, feelings, and perceptions of cancer in general, CRC, early detection of cancer, and CRC screening. Because the guide was developed based on prior literature, its primary conceptual framework was the Health Belief Model (HBM).47 Many concepts within the guide were framed around HBM key elements (perceived severity, benefits, barriers, cues to action). The primary questions are shown in Table 1. The same focus group facilitator (W. B.) conducted all 6 groups. A co-facilitator (K.A.G.) kept notes.
Table 1.
Moderator's Guide Primary Questions
| 1. When I say the word cancer, what's the first thing that comes to mind? |
| 2. So what words or feelings or ideas come to mind when you think about colon cancer in specific? |
| 3. Do people you know talk about colon cancer much as compared with other cancers? |
| 4. Are some people or groups of people more likely to get colon cancer? |
| Prompts |
| What sorts of things do you think cause colon cancer? |
| 5. When it comes to preventing colon cancer, are there any ways that people can keep from getting colon cancer? |
| 6. What are your thoughts about finding colon cancer earlier vs. finding it later? Does timing make a difference? |
| 7. Let's go around and find out your initial reaction to the fecal occult blood testing, the sigmoidoscopy, and the colonoscopy test. What kind of things might make a person more likely to get screened for colon cancer? |
| 8. What kind of things might make a person less likely to get screened for colon cancer? |
| Prompts |
| How does cost figure in to the decision of whether or not to get screened? |
| How does the doctor/heath care provider figure in? |
| 9. Finally, if you could create an ideal situation where everyone would get screened for colon cancer, and no one would die from it, how would you do that? |
Following a short break toward the end of each focus group, the co-facilitator (K. A. G.) conducted a 10-minute educational lecture on CRC and screening options using props (FOBT cards and a sigmoidoscope). This session included a description of the natural history of colon cancer, use of, and descriptions of FOBT, sigmoidoscopy, and colonoscopy. Participants were then asked for their reactions to each of these three test forms. Group members were polled for a specific test preference and, when appropriate, were asked to explain why they preferred a particular method of CRC screening.
Data Analysis
Survey—descriptive statistics were calculated for all survey data using SAS version 8.1 for PC (SAS Institute, Inc., Cary, NC).
Qualitative—Focus groups were audiotaped and videotaped, and transcripts were produced by an experienced qualitative transcriptionist. These were then verified by several of the authors (K.A.G., W.B., and N.N.) watching each videotape. Corrections were made to each transcript by the focus group moderator (W.B.) and the primary author (K.A.G.), both of whom were present at each of the focus groups. The final corrected transcript copies were distributed to each member of the analysis team (K.A.G., W.B., and N.N.) in a bound project notebook.
Qualitative analysis was conducted using an iterative process and following standard techniques.43–46,48,49 Each analysis team member read through all transcripts and summarized the key findings. Memos of these key findings were saved and interviews were reread. First-level codes were assigned. At an initial analysis meeting, memos were shared and first-level codes were grouped into categories through a consensus process. Each category was named with an identifiable descriptive term and definitions were formulated. Team members then independently recoded transcripts using descriptive categories. New categories were identified and recorded in memos. These memos were shared at a second team meeting and original and new categories were clustered into themes. Each team member then reread the transcripts to assure thematic fit for all focus group content. Triangulation and consensus were used throughout the analysis phase to maximize the reliability of the findings. Team members evaluated themes in relation to each other to develop an assessment of the relative importance of each theme. Each investigator independently assessed the salience of the chosen themes by performing theme counts (total times participant comments reflected themes) and by judging the qualitative weight given to themes by participants. Team members met a final time to review theme counts and agree on relative theme importance. The entire coding and category decision-making process was documented and reviewed by all team members to maximize the reliability and validity of the process and results.
RESULTS
The mean age of focus group participants was of 56 years (SD=10 years), and 56% were female. Several participants <50 years attended focus groups. Only one group had a large percentage of individuals between the ages of 40 and 49 years (50% were <50 years in this group). The majority of participants had governmental (40%) or no (27%) health insurance. Twenty-seven percent had a family history of polyps or CRC. Thirty-five percent had ever had an FOBT test and 45% had ever had either a screening or diagnostic sigmoidoscopy or colonoscopy.
On the prefocus group survey, 15% correctly identified the recommended age at which CRC screening should commence and 58% could name or describe a CRC screening test. Following the focus group and the CRC educational lecture session conducted within the focus group, 29% correctly identified 50 years as the recommended age for initiating CRC screening.
At the end of each focus group, following the educational lecture session, one-third of the participants (33%) reported a preference for colonoscopy and 26% reported a preference for FOBT. The remaining participants reported that they would do whatever their physician recommended or that they were unsure of their test preference. Only 1 participant reported that he/she would choose not to be screened for CRC.
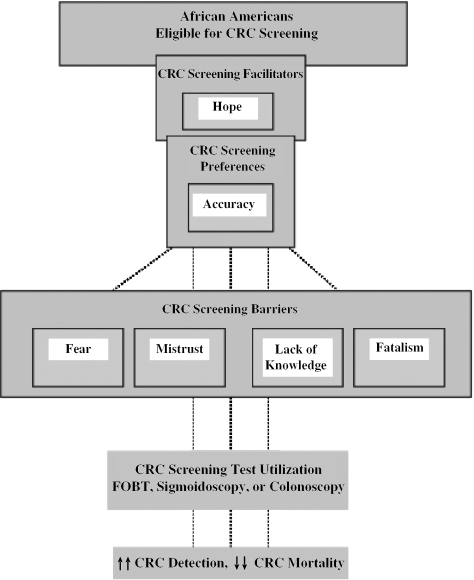
Six broad themes emerged from the focus group data. Each theme can be conceptualized as a screening barrier, facilitator, or a test preference that directly influences utilization (Figure 1). Each theme is described with illustrative quotes below and in Table 2.
FIGURE 1.
Influences on the Utilization of Colorectal Cancer Screening among African Americans.
Table 2.
Selected Focus Group Quotes Illustrating Major Data Themes
| Hope |
| With God, all things are possible. You see, I know people have reason to feel the way they feel, people have a reason that they believe the things that they believe, but it's amazing what a positive attitude will do. Ninety percent of success is attitude. Attitude is so important, and if you've got a positive one, it's so much better. I mean, the body will heal itself of just about most things, not all things, but most things. But it's your attitude that you take. Attitude is extremely important, and people don't seem to understand that. We're not born with fear, fear is something we develop, it's not something you born with. You're born with power and with love and a sound mind. Fear is something that is developed. |
| It's important to me because I had a triple bypass, and I hadn't had nobody cut me down to the bone or nothing, so I just left it up to the doctor, because I know he was God's instrument. And I didn't fear it at all, because I didn't even know what a triple bypass was. |
| So, as long as you live, and then there's always that higher priority … Miracles can happen, they'll think of some kind of way. A person would have to get in a good spiritual state of mind and to become above them. Cancer is something that you have to walk above. |
| Mistrust |
| … the doctors don't tell us … well, maybe the doctor should be as alarmed about colorectal cancer as he is about diabetes. Like she said, they don't tell us. They don't say, well, you know, this is your yearly check up, you need to suggest it more, and let them tell their husbands. |
| Fear |
| Fear of having cancer. Fear of the positive, yeah, I got it. I don't know and I don't want to know. |
| Now, as far as me going to the hospital, I don't like hospitals. I have had blood in my stools, but I have had bleeding ulcers—stress and stuff, but waiting for me to go to the hospital, forget it. |
| Now, to turn that around a little bit and ask myself, how come I haven't been checked for this? And I think it's because of fear, is what it would be. Fear of the procedure. |
| … it's not so much a denial, it's more so that this is a personal part of one's body, and this is a personal issue … it's not just a denial, just like, I don't want to know about it, it's more so, I don't even want to think about having a fatal death colon cancer. In thinking about a personal part of my body, infected with it. You don't want to deal with that. So, its more like I don't want to think about it, don't come this way with it, you know what I'm saying? |
| Fatalism |
| No such thing as recovery from cancer. This is where we see, when you say associate words, cancer automatically puts into the mind death. So even though they get it and you live 5 years longer, OK, there's always a possibility that it's going to spread later on somewhere else. |
| Accuracy |
| … I would rather pay the expense and go through it once and know that I have ten years control then to take that (fecal occult blood testing) every year and they still not finding cancer for that one year, and then I have to go through the test and everything else. I don't have to deal with me testing my own stool and possibly still having a question. |
| I'll take the long one. Cause what I've had before, so, like he said, they can see everything. |
| Well, like everybody else, that's the least comely portion of your body and it's very private. But in a case of whether or not you have something that could take your life, you want to avail yourself to whatever is going to prevent that. I guess my main thing is that anything that's preventive like that, I think that it's worth it and to go all the way in, because a scope like that (sigmoidoscope), it only go a portion of it, and the cancer may be higher up so you can miss that. You've tested, but you didn't test completely enough to rule it all the way out, so I would be for the longer one. |
| Knowledge |
| I think it is clear. I think the best thing for them is to learn about cancer. |
| Can I ask a question, does cancer spread. |
| Up until now, I never had a, I'm 58 years old and I've never had a colon check, just a prostate check |
| … this is the first time I ever just had a discussion on it, or ever talked about it with anyone. |
Hope
Participants had positive perceptions of early screening and agreed that detecting cancer early can lead to its cure and can save lives. They saw this as a positive feature of CRC and other cancer screening tests. They showed a great deal of hope about the achievement of positive outcomes. Hope was connected to personal religious or spiritual beliefs, with participants turning things over to God and being assured that things would turn out alright.*
I had a neighbor who had colon cancer, I lived there over 30 years, and she had 21 operations on colon cancer, she had hope, and any time the doctor said I need to go back in there. She let them go back in there. She lived way over I guess, 40 years with that colon cancer, so there is hope if you believe in what God said, he will heal your body and in the doctor.
Many described how God worked through doctors to achieve positive outcomes.
Discussions among the group often led to questions about why CRC screening is not recommended before the age of 50 years. Most participants felt that early detection should commence closer to the age of 35 years. These opinions reflected the positive stance of the groups with regard to CRC screening.
My question, why do they wait until you're like 50 to do this? Why can't they do it at an early age?
That was my question. Why not wouldn't you start it at age 35? Like put it on a card. Because I don't see any reason unless there's a lot of pain involved in it or something, I don't see any reason you wouldn't just start it.
Mistrust
Focus group participants described how the current health care system does not meet patient care needs. They described the system as a direct cause of poor utilization of cancer screening by African Americans. Costs contributed to mistrust. The organization of care and specifically managed care were blamed for a diminished focus on patient well-being. Doctors were described as being rushed by managed care and this led to omission of thorough testing for cancer. Participants explained that they often felt that the health care system had suspect motives and that it was up to patients to advocate for themselves. Some participants explained that it was important for patients to consider getting a second opinion on important medical issues.
… but I don't want them to use me as no guinea pig, you understand what I'm saying? I would want some tests to be done first, and then get a second opinion and we go from there. But I don't want you to use me as no experiment, know what I'm saying?
Fear
Many participants reported that their friends, neighbors, and relatives did not take proactive approaches toward early cancer detection. Some stated that members of the African-American community in general often adopt a passive role and avoid seeking medical care out of fear and denial that something might be wrong. Participants expressed the belief that if one looks and/or feels okay, one must be okay. Fear was described as a major factor influencing use of services and follow-up with physicians. Most participants reported that they had many fears with regard to cancer and that they could understand why many patients shy away from screening tests that might reveal a very grim prognosis.
I've had several friends die because they were just what you just said—fear. Fear of going to the hospital, fear of what they might find out. I'd rather go to that hospital and find out and possibly catch it in time than not go and when they do find it, it's too late. That's ignorance to me.
People repeatedly said that members of older generations typically did not even talk about cancer and that there was a culture of silence and avoidance around the issue.
Other participants reported fear of the embarrassing or uncomfortable nature of CRC tests. They described these fears as a significant influence on overall willingness to participate in screening, especially when they might have to follow up or initiate these embarrassing processes.
It's an embarrassing test. It goes against your beliefs to some degree, because if you read the Bible, we just don't let anything go in your rectum.
Older participants seemed less concerned with invasive procedures and stated that although these things bothered them when they were younger, they were willing to go through with them now.
When I was a younger person, I had a lot of fears and concerns to it. As I've gotten older and become a more spiritual person, my focus has changed. The advancement of technology and the way that it's come forth has really taken some of the sting of it out, the fear of it out.
Fatalism
A number of comments within focus groups represented fatalistic beliefs. They generally reflected the idea that once a person gets cancer, not much can be done about it.
If you find it early, you might can get treated for it, but I think that once the cancer is there, it's always gonna come back. I don't care how many years you go, that cancer's always gonna come right back.
Participants would sometimes describe fatalistic beliefs among their friends and community and attribute lack of CRC screening to such beliefs. The most common fatalistic topic discussed was that of cancer spread caused by surgical procedures. Virtually all focus group participants had heard people say that cancer spreads when a patient is opened up and “air hits the cancer.” Although the majority of our participants did not endorse this belief, they described it as a very common belief in their community.
Well, you know some older people that think that once you find cancer and start cutting on cancer, cancer will spread. At the first sign of cutting on it, the cancer will spread through your body.
But you also hear the rumors where people have been opened up and it seemed like when they were opened up, the cancer spread. And I think that's my biggest fear.
Accuracy
Most focus group participants expressed a strong preference for colon cancer screening tests that were thorough and accurate. After hearing descriptions of FOBT, sigmoidoscopy, and colonoscopy, the largest number of participants (33%) stated that they would want the test that could “see everything” (colonoscopy). Although a small subgroup of mostly males described reticence about having an invasive procedure such as a colonoscopy, many of these individuals said that in spite of this, they would probably choose this test because it was more thorough.
I would like the scope cause it's more accurate, knock me out, get it done, be done with it.
A number of participants stated that they would like to have both colonoscopy testing and yearly FOBT testing as an adjunct. This was described as another means to assure thorough assessment of cancer risk. A number of participants questioned the recommendation that screening should begin at age 50 for similar reasons. They described friends and acquaintances who had been diagnosed with CRC at ages much younger than 50. They felt that it would be most thorough and effective to screen individuals for CRC early and prevent all CRC deaths.
Knowledge
Participants uniformly described a lack of CRC knowledge and voiced a desire for more information on this. They asked many questions that clearly revealed their knowledge deficits and their strong interest in gaining information that could be used to assess their own risk for CRC and facilitate CRC screening. They stated that knowledge of CRC and CRC screening was very low among their friends, relatives, and self-defined communities. A large number of participants specifically described CRC knowledge and awareness as solutions to the problem of low CRC screening rates.
… when people are educated, then that takes away the fear because they have an understanding of things. Making education available, in the form of preventive medicine, things like that. And the more things are spoken to, people, I mean as long as it stays a mystery, then the fear factor is going to be real high …
Relative Thematic Importance
All three data coders (K.A.G., W.B., and N.N.) completed transcript theme counts and agreed that the Fear and Knowledge themes were the most frequently present them in participant comments. The Hope and Accuracy themes were often used as qualifiers that followed statements reflecting Fear, lack of Knowledge, and, less frequently, Fatalism and Mistrust. In other words, participants would often make a comment about Fear, Knowledge, etc., and then follow it up with a statement related to Hope or Accuracy.
We assessed each of the focus groups to determine whether focus group make-up affected the themes discussed. We found no significant variation by size of the group, or within the one focus group that was composed of 50% individuals <50 years.
DISCUSSION
Our results suggest that CRC screening in African Americans is influenced by Hope, Mistrust, Fear, Fatalism, Accuracy, and Knowledge (or lack of Knowledge). Although each of these themes had salience for the participants in our groups, the Fear and Knowledge themes were cited most often, suggesting key barriers to CRC screening. Participants in our groups suggested that enhanced CRC Knowledge would be most likely to raise screening rates among African Americans. They also placed qualitative emphasis on the Hope and Accuracy themes, and stated that if they remained positive and hopeful and received the highest standard and most accurate care, they would be able to overcome barriers and prevent CRC. The Hope, Accuracy, and Knowledge themes were offered as solutions to the barriers cited in this study (Fear, lack of Knowledge, Fatalism, and Mistrust). Prior work has shown that barriers contribute to inadequate CRC screening among African Americans.16,21,34–36,41,50 These studies have highlighted the influence of lack of physician recommendation and CRC knowledge, denial of the possibility that CRC might occur, not wanting to know whether it does occur, costs, and the embarrassing/uncomfortable/unpleasant nature of CRC tests. Additional studies have assessed barriers to breast and prostate cancer screening among African Americans.37–40,51–54 Many of these studies have relied on the HBM,47 a model within which barriers are often the most predictive construct for a given health behavior. Our results may be placed in the context of this model, and, in general, they confirm that CRC screening is influenced by many of the same factors influencing breast and prostate cancer screening in African Americans.
If CRC screening utilization is directly affected by barriers and facilitators facing patients as indicated by the HBM, our qualitative findings should assist with programs intended to raise utilization rates. We conceptualize lack of Knowledge, Mistrust, Fear, and Fatalism as barriers and Hope as a facilitator (Figure 1). Our Accuracy theme relates primarily to preference. Future initiatives can exploit these findings to provide a specifically tailored message to African Americans. Programs could advance CRC knowledge within the African-American community by improving health care provider and mass media transmission of information on CRC prevention. Our focus groups indicate that CRC factual information should be presented in simple terms. Interventions could capitalize on the qualitative importance of the Hope and Accuracy themes to raise awareness and give a positive spin to tailored educational messages. The Hope and Accuracy themes could also be used to craft interventions intended to overcome the barrier themes of Fear, Fatalism, Knowledge, and Mistrust. It will be important to acknowledge these barriers, especially the frequently noted Fear and Knowledge barriers. Once barriers have been acknowledged, the Hope and Accuracy themes could be offered as mechanisms for framing the issue of CRC screening for African Americans.
Our study has several limitations. Participants were recruited from a single site, and the findings may lack generalizability beyond the Mid-west and with non-urban-dwelling African Americans. In addition, our sample was exclusively low income. We did not stratify focus groups in any way. It is possible that this may have hindered open honest communication among participants. Another limitation was our failure to capture only participants over the age of 50 years. This may have artificially created a low CRC knowledge level among our participants. The consistency of low knowledge and thematic findings between groups with variable numbers of participants <50 years suggests that this was not a major problem.
CONCLUSIONS
Urban African Americans in this study described lack of CRC knowledge and fear as primary causes of low CRC screening rates within their community. Focus group comments also suggested that mistrust of the health care system and cancer fatalism are important barriers. Nevertheless, participants were strong advocates of early detection and saw thorough and accurate CRC screening as being valuable. Future interventions to improve screening should capitalize on the optimistic, engaged, and proactive attitudes prevalent in this population, and should craft programs that will directly address key barriers.
Acknowledgments
The authors would like to thank the administration, patients, and staff at Swope Parkway Health Center, Kansas City for making this project possible. Their insights and opinions have been invaluable. We would also like to thank Nichole Freeman for recruiting/focus group assistance, and Heather Hall for transcription services.
This study was supported by a Mentored-Clinician Scientist Career Development Award from the University of Kansas Medical Center Research Institute and an American Cancer Society Career Development Award for Primary Care Clinicians (CCCDA-02-223-01), K.A.G.
Footnotes
All quotes are verbatim statements with identifiers altered.
REFERENCES
- 1.Lag R, Eisner MP, Kosary CL, et al. SEER Cancer Statistics Review, 1973–1999. Bethesda, Md: National Cancer Institute; 2002. [Google Scholar]
- 2.Cancer Facts and Figures—2002. Atlanta: American Cancer Society; 2002. [Google Scholar]
- 3.Winawer SJ, Fletcher RH, Miller L, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology. 1997;112:594–642. doi: 10.1053/gast.1997.v112.agast970594. [DOI] [PubMed] [Google Scholar]
- 4.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota colon cancer control study. N Engl J Med. 1993;328:1365–71. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 5.Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91:434–7. doi: 10.1093/jnci/91.5.434. [DOI] [PubMed] [Google Scholar]
- 6.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343:1603–7. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 7.Selby JV, Friedman GD, Quesenberry CP, Jr, Weiss NS. A case–control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326:653–7. doi: 10.1056/NEJM199203053261001. [DOI] [PubMed] [Google Scholar]
- 8.Atkin WS, Hart A, Edwards R, et al. Uptake, yield of neoplasia, and adverse effects of flexible sigmoidoscopy screening. Gut. 1998;42:560–5. doi: 10.1136/gut.42.4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newcomb PA, Norfleet RG, Storer BE, Surawicz TS, Marcus PM. Screening sigmoidoscopy and colorectal cancer mortality. J Natl Cancer Inst. 1992;84:1572–5. doi: 10.1093/jnci/84.20.1572. [DOI] [PubMed] [Google Scholar]
- 10.Winawer SJ, Zauber AG. Colonoscopic polypectomy and the incidence of colorectal cancer. Gut. 2001;48:753–4. doi: 10.1136/gut.48.6.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–81. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 12.Muller AD, Sonnenberg A. Prevention of colorectal cancer by flexible endoscopy and polypectomy. A case–control study of 32,702 veterans. Ann Intern Med. 1995;123:904–10. doi: 10.7326/0003-4819-123-12-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 13.Smith RA, Cokkinides V, von Eschenbach AC, et al. American cancer society guidelines for the early detection of cancer. CA Cancer J Clin. 2002;52:8–22. doi: 10.3322/canjclin.52.1.8. [DOI] [PubMed] [Google Scholar]
- 14.Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN. Screening for colorectal cancer in adults at average risk: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:132–41. doi: 10.7326/0003-4819-137-2-200207160-00015. [DOI] [PubMed] [Google Scholar]
- 15.Coughlin SS, Thompson TD, Seeff L, Richards T, Stallings F. Breast, cervical, and colorectal carcinoma screening in a demographically defined region of the southern U.S. Cancer. 2002;95:2211–22. doi: 10.1002/cncr.10933. [DOI] [PubMed] [Google Scholar]
- 16.Holmes-Rovner M, Williams GA, Hoppough S, Quillan L, Butler R, Given CW. Colorectal cancer screening barriers in persons with low income. Cancer Pract. 2002;10:240–7. doi: 10.1046/j.1523-5394.2002.105003.x. [DOI] [PubMed] [Google Scholar]
- 17.Nadel MR, Blackman DK, Shapiro JA, Seeff LC. Are people being screened for colorectal cancer as recommended? Results from the National Health Interview Survey. Prev Med. 2002;35:199–206. doi: 10.1006/pmed.2002.1070. [DOI] [PubMed] [Google Scholar]
- 18.Breen N, Wagener DK, Brown ML, Davis WW, Ballard-Barbash R. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. J Natl Cancer Inst. 93:1704–13. doi: 10.1093/jnci/93.22.1704. Nov 21 2001. [DOI] [PubMed] [Google Scholar]
- 19.Behavioral Risk Factor Surveillance System, 1999. Survey Data. National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. Washington, DC: United States Department of Health and Human Services; 1999. [Google Scholar]
- 20.Beeker C, Kraft JM, Southwell BG, Jorgensen CM. Colorectal cancer screening in older men and women: qualitative research findings and implications for intervention. J Community Health. 2000;25:263–78. doi: 10.1023/a:1005104406934. [DOI] [PubMed] [Google Scholar]
- 21.Brenes GA, Paskett ED. Predictors of stage of adoption for colorectal cancer screening. Prev Med. 2000;31:410–6. doi: 10.1006/pmed.2000.0729. [DOI] [PubMed] [Google Scholar]
- 22.Paskett ED, Rushing J, D'Agostino R, Jr., Tatum C, Velez R. Cancer screening behaviors of low-income women: the impact of race. Womens Health. 1997;3:203–26. [PubMed] [Google Scholar]
- 23.Parker SL, Davis KJ, Wingo PA, Ries LA, Heath CW., Jr. Cancer statistics by race and ethnicity. CA Cancer J Clin. 1998;48:31–48. doi: 10.3322/canjclin.48.1.31. [DOI] [PubMed] [Google Scholar]
- 24.Freeman HP, Alshafie TA. Colorectal carcinoma in poor blacks. Cancer. 2002;94:2327–32. doi: 10.1002/cncr.10486. [DOI] [PubMed] [Google Scholar]
- 25.Mandelblatt J, Andrews H, Kao R, Wallace R, Kerner J. The late-stage diagnosis of colorectal cancer: demographic and socioeconomic factors. Am J Public Health. 1996;86:1794–7. doi: 10.2105/ajph.86.12.1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bejes C, Marvel MK. Attempting the improbable: offering colorectal cancer screening to all appropriate patients. Fam Pract Res J. 1992;12:83–90. [PubMed] [Google Scholar]
- 27.Myers RE, Ross EA, Wolf TA, Balshem A, Jepson C, Millner L. Behavioral interventions to increase adherence in colorectal cancer screening. Med Care. 1991;29:1039–50. doi: 10.1097/00005650-199110000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Arveux P, Durand G, Milan C, et al. Views of a general population on mass screening for colorectal cancer: the burgundy study. Prev Med. 1992;21:574–81. doi: 10.1016/0091-7435(92)90065-p. [DOI] [PubMed] [Google Scholar]
- 29.Hunter W, Farmer A, Mant D, Verne J, Northover J, Fitzpatrick R. The effect of self-administered faecal occult blood tests on compliance with screening for colorectal cancer: results of a survey of those invited. Fam Pract. 1991;8:367–72. doi: 10.1093/fampra/8.4.367. [DOI] [PubMed] [Google Scholar]
- 30.Powe BD. Fatalism among elderly African Americans. Effects on colorectal cancer screening. Cancer Nurs. 1995;18:385–92. [PubMed] [Google Scholar]
- 31.Hoogewerf PE, Hislop TG, Morrison BJ, Burns SD, Sizto R. Health belief and compliance with screening for fecal occult blood. Soc Sci Med. 1990;30:721–6. doi: 10.1016/0277-9536(88)90257-2. [DOI] [PubMed] [Google Scholar]
- 32.Vernon SW, Acquavella JF, Yarborough CM, Hughes JI, Thar WE. Reasons for participation and nonparticipation in a colorectal cancer screening program for a cohort of high risk polypropylene workers. J Occup Med. 1990;32:46–51. doi: 10.1097/00043764-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Vernon SW, Gilstrap EL, Jackson GL, Hughes JI. An intervention to increase participation in a work site cancer screening program. Health Values. 1992;16:3–9. [Google Scholar]
- 34.James AS, Campbell MK, Hudson MA. Perceived barriers and benefits to colon cancer screening among African Americans in North Carolina: how does perception relate to screening behavior? Cancer Epidemiol Biomarkers Prev. 2002;11:529–34. [PubMed] [Google Scholar]
- 35.Lipkus IM, Lyna PR, Rimer BK. Colorectal cancer risk perceptions and screening intentions in a minority population. J Natl Med Assoc. 2000;92:492–500. [PMC free article] [PubMed] [Google Scholar]
- 36.Lipkus IM, Rimer BK, Lyna PR, Pradhan AA, Conaway M, Woods-Powell CT. Colorectal screening patterns and perceptions of risk among African-American users of a community health center. J Community Health. 1996;21:409–27. doi: 10.1007/BF01702602. [DOI] [PubMed] [Google Scholar]
- 37.Doukas DJ, Fetters MD, Coyne JC, McCullough LB. How men view genetic testing for prostate cancer risk: findings from focus groups. Clin Genet. 2000;58:169–76. doi: 10.1034/j.1399-0004.2000.580303.x. [DOI] [PubMed] [Google Scholar]
- 38.McFall SL, Hamm RM. Interpretation of prostate cancer screening events and outcomes: a focus group study. Patient Educ Couns. 2003;49:207–18. doi: 10.1016/s0738-3991(02)00180-5. [DOI] [PubMed] [Google Scholar]
- 39.Phillips JM, Cohen MZ, Moses G. Breast cancer screening and African American women: fear, fatalism, and silence. Oncol Nurs Forum. 1999;26:561–71. [PubMed] [Google Scholar]
- 40.Bailey EJ, Erwin DO, Belin P. Using cultural beliefs and patterns to improve mammography utilization among African-American women: the witness project. J Natl Med Assoc. 2000;92:136–42. [PMC free article] [PubMed] [Google Scholar]
- 41.Brouse CH, Basch CE, Wolf RL, Shmukler C, Neugut AI, Shea S. Barriers to colorectal cancer screening with fecal occult blood testing in a predominantly minority urban population: a qualitative study. Am J Public Health. 2003;93:1268–71. doi: 10.2105/ajph.93.8.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Holmes-Rovner M, Williams GA, Hoppough S, Quillan L, Butler R, Given CW. Colorectal cancer screening barriers in persons with low income. Cancer Pract. 2002;10:240–7. doi: 10.1046/j.1523-5394.2002.105003.x. [DOI] [PubMed] [Google Scholar]
- 43.Willms DG, Best JA, Taylor DW, et al. A systematic approach for using qualitative methods in primary prevention research. Med Anthropol Q. 1990;4:391–411. [Google Scholar]
- 44.Pope C, Mays N. Qualitative methods in health and health services research. In: Mays N, Pope C, editors. Qualitative Research in Health Care. London: BMJ; 1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Basch CE. Focus group interview: an underutilized research technique for improving theory and practice in health education. Health Educ Q. 1987;14:411–48. doi: 10.1177/109019818701400404. [DOI] [PubMed] [Google Scholar]
- 46.Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320:50–2. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 48.Miles M, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, Calif: Sage Publications; 1994. [Google Scholar]
- 49.Miles MB, Huberman AM. Qualitative Data Analysis: A Source Book of New Methods. Thousand Oaks, Calif: Sage Books; 1984. [Google Scholar]
- 50.Price JH. Perceptions of colorectal cancer in a socioeconomically disadvantaged population. J Community Health. 1993;18:347–62. doi: 10.1007/BF01323966. [DOI] [PubMed] [Google Scholar]
- 51.Bowen D, Hickman KM, Powers D. Importance of psychological variables in understanding risk perceptions and breast cancer screening of African American women. Womens Health. 1997;3:227–42. [PubMed] [Google Scholar]
- 52.Crump SR, Mayberry RM, Taylor BD, Barefield KP, Thomas PE. Factors related to noncompliance with screening mammogram appointments among low-income African-American women. J Natl Med Assoc. 2000;92:237–46. [PMC free article] [PubMed] [Google Scholar]
- 53.Zhu S-H, Tedeschi GJ, Anderson CM, Pierce JP. Telephone counseling for smoking cessation: whats in a call? J Couns Dev. 1996;75:93–102. [Google Scholar]
- 54.Kinney AY, Emery G, Dudley WN, Croyle RT. Screening behaviors among African American women at high risk for breast cancer: do beliefs about god matter? Oncol Nurs Forum. 2002;29:835–43. doi: 10.1188/02.ONF.835-843. [DOI] [PubMed] [Google Scholar]