Abstract
BACKGROUND
Symptoms are common and often remain medically unexplained.
OBJECTIVE
To assess 5-year symptom outcomes, determine how often symptoms remain unexplained and assess their relationship with mental disorders.
DESIGN
Prospective cohort study.
PARTICIPANTS
Five hundred consecutive patients presenting to a medicine clinic with physical symptoms.
MEASUREMENTS PREVISIT
Mental disorders, symptom characteristics, stress, expectations, illness worry, and functional status. Postvisit (immediately, 2 weeks, 3 months, 5 years): unmet expectations, satisfaction, symptom outcome, functional status, and stress.
RESULTS
While most subjects (81%) experienced symptom improvement by 5 years, resolution rates were lower (56%), with 35% of symptoms remained medically unexplained. Most patients with medically unexplained symptoms (MUS) did not have a mental disorder. Mood or anxiety disorders were not associated with MUS (relative risks [RR]: 0.94, 95% confidence interval [CI]: 0.79 to 1.13), or with lower rates of symptom improvement (RR: 1.14, 95% CI: 0.60 to 2.2). In contrast, most patients with somatoform disorders had MUS and were unlikely to improve. Worse functioning (RR: 0.95, 95% CI: 0.91 to 0.99), longer duration of symptom at presentation (RR: 0.5, 95% CI: 0.28 to 0.87), illness worry at presentation (RR: 0.56, 95% CI: 0.35 to 0.89), or lack of resolution by 3 months (RR: 0.47, 95% CI: 0.26 to 0.86) reduced the likelihood of symptom improvement at 5 years.
CONCLUSIONS
More than half of patients presenting with a physical symptom resolve by 5 years, while a third remain medically unexplained. Most patients whose symptom remained unexplained had no mental disorder. While mood and anxiety disorders were not associated with MUS or worse outcomes, most patients with somatoform disorders had MUS and were unlikely to improve.
Keywords: outcomes, symptoms, unexplained symptom
Physical symptoms are common, accounting for over half of all outpatient visits.1 Research on the natural history of symptoms is limited. Most studies focus on specific symptoms such as back pain,2 fatigue,3 dizziness,4 palpitations,5 abdominal pain,6,7 or chest pain.8 Few prospective primary care studies have provided data on a spectrum of symptoms, and none have followed patients more than a few months.9,10
Previous studies suggest that up to a third of physical symptoms remain unexplained,11 even after extensive evaluation,12,13 Clinicians often assume that psychiatric problems underlie medically unexplained symptoms (MUS).11 For many, the term “MUS” has become a euphemism for patients with somatization or other mental disorders.14 This has occurred for several reasons. First, part of the criteria for somatization disorder is the presence of a multitude of unexplained physical symptoms. Second, patients with anxiety or depressive disorders usually present with physical rather than emotional complaints,15,16 and an increasing number of symptoms predict the presence of mood or anxiety disorders.16,17 In addition, many studies of patients with MUS use entry criteria that result in high rates of mental disorders. Some focus on high utilizers18 others on patients with multiple MUS.19 As utilization rates20,21 and multiple symptoms are markers for mood, anxiety, and somatoform disorders,15–17 this results in a concentration of patients with such disorders. A recent systematic review of MUS found an association with mental disorders and fibromyalgia, chronic fatigue, nonulcerative dyspepsia, and irritable bowel syndrome, but concluded, “there is only limited meta-analytic evidence for the same sort of association for medically unexplained physical symptoms in general.”22 This is similar to other studies in which the relationship between MUS and emotional disorders was found to be unclear. 12,23
Our study purposes were to determine symptom outcomes over 5 years of follow-up, assess how often these symptoms remain unexplained and to elucidate the relationship between mental disorders, symptoms and MUS in a prospective primary care cohort.
Patients
Consecutive adults presenting to the primary care walk-in clinic at Walter Reed Army Medical Center with a chief complaint of a physical complaint (excluding upper respiratory infection complaints such as cough, coryza, or sore throat) were eligible to participate. Upper respiratory infections were excluded because 90% resolve within 2 weeks.10 We have previously shown that patient age, gender, and case mix is similar in this military treatment facility to that seen in nonmilitary U.S. Internal Medicine office practices.24,25 Of 528 patients approached, 500 agreed to participate. Participants were similar to nonparticipants in terms of age, race, sex, and type of complaint. We achieved 93% (n=463) 2 week, 83% 3 month (n=413) and 75% (338/441) 5 year follow-up rates (Figure 1). We obtained informed consent from all patients and our Institutional Review Board approved this study.
FIGURE 1.
Study timeline and participation rates.
Previsit Assessment
Immediately before their visit, subjects completed surveys that asked what problem brought them to the clinic, symptom duration and severity (0 to 10), whether or not they were worried this problem could be because of a serious illness (yes/no), what their expectations were for the visit from a checklist that included receiving: an explanation of the problem's cause (diagnosis), an estimate of how long the problem is likely to last (prognosis), a prescription, a diagnostic test, a referral or other.26 Patients were asked whether they had been under stress in the past week (yes/no), completed a 6-item functional status assessment (Medical Outcomes Study SF-6),27 and completed the Patient Health Questionnaire (PHQ-15), an instrument that assesses whether the patient has been bothered, in the past month, by up to 15 common physical symptoms.28 Patients were also were screened for mental disorders with the PRIME-MD. Screen positive patients for depression, anxiety, or somatization disorders underwent structured psychiatric PRIME-MD interviews to make Diagnostic and Statistical Manual of Mental Disorders, 4th edition diagnoses of mood, anxiety, and somatoform disorder not otherwise specified (NOS).29 Because the PRIME-MD has acceptable specificity, but low sensitivity for somatoform disorders,30 we expanded our diagnoses of somatoform disorders to include multisomatoform disorder. This diagnosis was made, based on the presence of more than 3 symptoms of more than 2 years duration using the PHQ-15, an instrument that has been shown valid and reliable for this diagnosis.28,31
Postvisit Assessment
Immediate postvisit satisfaction with the clinician in 5 domains (overall, technical competence, bedside manner, time spent with clinician, and explanation of what was performed) was assessed with the Medical Outcomes 9-item instrument.32 Patients were also asked whether or not they had been given a diagnosis for their symptom(s), whether they were still worried their symptom could be because of something serious (yes/no), and whether or not they had any postvisit unmet expectations from a checklist (for a diagnosis, prognostic information, prescription, diagnostic test, referral or other). Two weeks, 3 months, and 5 years after the visit, patients completed a mailed follow-up questionnaire that assessed symptom outcome (completely resolved, better, same, or worse), symptom severity (0 to 10), and were again asked about stress, worry, functional status (MOS SF6), satisfaction, and unmet expectations, using the same questions asked on the pre- and immediately postvisit surveys. At 5 years, patients additionally completed the PHQ-15, a self-report version of the PRIME-MD,33 as well as other symptom related outcomes including: symptom frequency (more than half the days, 10 to 15, 5 to 9, 1 to 4 days per month, less than monthly), how disabling the symptom was (not difficult, a little, somewhat difficult, moderately difficult, extremely difficult), and whether they had received a diagnosis for their symptom. In order to minimize recall bias, our follow-up questionnaires about symptom outcome at 2 weeks, 3 months, and 5 years specified the date of the index appointment, the name of the clinician they saw and the complaint(s), if more than 1 was listed by the patient, using the same words the patients wrote on the initial survey.
Patient deaths were taken from the national death index. Patients not responding to 2 mailed surveys were contacted telephonically. Overall, 65% responded to the first mailing, another 28% to the second mailing. We had to contact 7% by telephone.
Our study instruments have been previously demonstrated to be valid and reliable including the PRIME-MD,29,30,33 our satisfaction instrument,32 the PHQ-15,28 the MOS SF-6,27 and our measures of expectations.10,11
Analysis and Sample Size Calculations
All analyses were performed using Stata (Version 8.2). The primary outcome was symptom resolution at each of the 3 time points. Whether or not the patient's symptom was medically unexplained was based on the patient surveys immediately postvisit and at 5 years. Other symptoms outcomes were based on the PHQ-15. Independent variables were compared using Students t-tests or the Kruskal–Wallis signed rank test for continuous variables and χ2 for categorical ones. ANOVA was used to compare functional status among the categories of symptom outcome. Logistic regression assessed predictors of symptom resolution and illness worry. Based on a 2-tailed test, α=0.05, β=0.8, and a rate of mental disorders of 30%, we calculated a need to enroll 496 patients to demonstrate a 15% difference in the likelihood of having a medically unexplained symptom.
RESULTS
Patient Characteristics
Patients averaged 55 years in age, half were women, 49% were white, 45% African American, and 6% other. Patients presented with a variety of symptoms, which we collapsed into 14 categories (Table 1). Ninety-seven (19%) recorded 2 symptoms and 5% listed 3 symptoms as their reasons for seeking medical attention. Pain of some type was present in 65%. Musculoskeletal complaints were the largest symptom category. Twenty-one percent had experienced their symptom less than 3 days, 55% less than 2 weeks and 68% less than a month. Sixty-four percent were worried that their symptom could represent a serious illness. In addition to the chief complaint, patients endorsed an average of 2.9 (range: 0 to 14) “other bothersome” symptoms on the PHQ-15.
Table 1.
Symptom Types and Outcomes
| Symptom Type | Symptom Resolution | |||
|---|---|---|---|---|
| n | 2 wk, % | 3 mo, % | 5 y, % | |
| Ear/Nose/Throat problems | 23 | 35 | 38 | 65 |
| Gastrointestinal problems | 40 | 30 | 35 | 68 |
| Chest pain | 17 | 18 | 53 | 59 |
| Dizziness | 26 | 4 | 20 | 54 |
| Numbness | 12 | 0 | 33 | 60 |
| Genitourinary problems | 24 | 33 | 52 | 73 |
| Pain, other | 20 | 0 | 25 | 44 |
| Dermatological | 53 | 21 | 43 | 46 |
| Musculoskeletal | 150 | 12 | 35 | 56 |
| Headache | 19 | 5 | 29 | 50 |
| Back pain | 37 | 8 | 29 | 46 |
| Fatigue | 15 | 33 | 25 | 50 |
| Eye problems | 15 | 45 | 47 | 53 |
| Miscellaneous | 16 | 23 | 31 | 52 |
A depressive or anxiety disorder was present in 146 patients (29%); 11% had more than 1 disorder. Specific disorders included: major depression (8.4%), dysthymia (1.4%), minor depression (10.4%), panic disorder (1.4%), generalized anxiety disorder (2%), anxiety NOS (11.4%), somatoform disorder (12%), and multisomatoform disorder (5%). Patients with mood, anxiety or somatoform disorders had a greater number of symptoms on the PHQ-15 (6.2 vs 4.7, P<.0001), greater symptom severity (6.6 vs 5.0, 0 to 10 scale, P<.001), were more likely to report stress (69% vs 30%, P<.001) and had greater functional impairment (P<.001).
Immediately postvisit, patients reported receiving a diagnosis in 52% of encounters (n=260). The majority of the 48% of patients without a medical explanation for their symptom after their initial visit had no mental disorder (relative risks [RR]: 0.94%, 95% confidence interval [CI]: 0.79 to 1.13). Among the specific mental disorder diagnoses, there was no relationship between MUS and mood (RR: 0.87, 95% CI: 0.73 to 1.04) or anxiety disorders (RR: 0.81, 95% CI: 0.57 to 1.15), although patients with somatoform or multisomatoform disorders were more likely to report not receiving a medical explanation (somatoform: RR: 1.58%; 95% CI: 1.18 to 1.92, multisomatoform: RR: 1.21; 95% CI: 1.09 to 1.37). After the visit 32% of patients were still worried their symptom could be because of something serious. While the presence of a mood or anxiety disorders was not associated with persistent worry, those with somatoform disorders were more likely to be worried (RR: 1.8, 95% CI: 1.4 to 2.3).
2-Week Outcomes
By 2 weeks, 18% of the subjects experienced symptom resolution; 52% were better, 21% unchanged, and 8% were worse. In each successive category of symptom outcome (worse, same, better, resolved) patients had better functional status scores (P<.001). Patients experiencing symptom resolution were more satisfied (RR: 1.6, 95% CI: 1.4 to 1.9), less likely to be worried their symptom could be serious (RR: 0.60, 95% CI: 0.54 to 0.67) and had fewer unmet expectations (RR: 0.76, 95% CI: 0.68 to 0.86).
Predictors of symptom resolution included shorter duration of the symptom at the index visit (median 4 vs 21 days, P<.001), less symptom severity (4.9 vs 5.7, P=.01), fewer PHQ-15 symptoms (3.4 vs 4.1, P=.05), better functioning (P=.002) and no serious illness worry either at baseline (RR: 2.2, 95% CI: 1.5 to 3.5) or immediately postvisit (RR: 2.3, 95% CI: 1.3 to 4.2). Anxiety or mood disorders had no impact on the rate of symptom improvement, although subjects with somatoform disorders were less likely to improve (RR: 0.69, 95% CI: 0.49 to 0.96).
3-Month Outcomes
By 3 months, 37% experienced symptom resolution, 43% were better, 12% unchanged, and 8% were worse. Almost half (47%) of patients with symptoms at 2 weeks had resolution by 3 months. Conversely, 27% of those with 2-week symptom resolution had recurrence by 3 months. As with 2-week outcomes, each category of better symptom category (worse, same, better, resolved) was associated with better functioning (P<.001).
Predictors of 3-month symptom resolution included shorter duration prior to presentation (median 4 vs 28 days, P<.0001), no immediate postvisit illness worry (RR: 1.41, 95% CI: 1.02 to 1.92), and better baseline functional status (P=.002). While there was no effect of anxiety or depressive disorders on symptom outcome, those with somatoform or multisomatoform disorders were less likely to improve (RR: 0.70, 95% CI: 0.51 to 0.96). There was no relationship between the whether or not the symptom was explained on the initial visit and symptom improvement (RR: 1.09%, 95% CI: 0.97 to 1.22). The strongest predictor of symptom resolution at 3 months was resolution of the symptom at 2 weeks (RR: 2.6%, 95% CI: 2.1 to 3.3).
Outcomes at 5 Years
Forty-nine (9%) patients died during the 5 years of follow-up. Among survivors, 56% experienced symptom resolution, 25% were improved, 10% unchanged and 9% were worse. Among those with persistent symptoms, symptom frequency varied: 37% experienced symptoms daily, 10% more than half the month, 15% more than 1 week per month, 15% a few days each month, and 24% less than monthly. The impact of persistent symptoms also varied, 49% experienced “no difficulty” in their daily life from their symptom, 38%“some,” 14%“considerable,” and 7%“extreme difficulty.”
At 5 years, patients averaged 2.4 other bothersome symptoms on the PHQ-15. Among patients reporting 1 or fewer PHQ symptom at baseline, 38% had no PHQ symptoms at 5 years and the remaining 62% averaged only 1 PHQ symptom (range 1 to 4). Among patients reporting 2 or more “other bothersome” symptoms during the baseline visit, a greater number of symptoms was associated with less likelihood of having no symptoms on the PHQ 15 at 5 years. For example, among those with 2 “other bothersome” symptoms at the baseline visit, 33% had no “other bothersome” symptoms at 5 years, while among those with 5 or more baseline symptoms, only 6% reported no “other bothersome” symptoms at 5 years (P<.001 for trend).
At 5 years, 14% of subjects had mood, anxiety or somatoform disorders (mood: 8%, anxiety: 6%, somatoform: 4%). Mental disorders were associated with a greater number of symptoms on the PHQ-15 (RR: 1.44, 95% CI: 1.21 to 1.72), worse functioning (RR: 0.82, 95% CI: 0.78 to 0.88), and greater symptom severity (RR: 1.20%, 95% CI: 1.05 to 1.38).
Over the 5 years of follow-up, 34% of the symptoms for which the patient originally presented remained medically unexplained. Most patients (69%) with a medically unexplained symptom did not have a mental disorder (RR: 0.89%, 95% CI: 0.62 to 1.27). While there was no relationship between the presence of a mood or anxiety disorder either at baseline or at 5 years and having a medically unexplained symptom, most patients (64%) with somatoform or multisomatoform disorders symptoms remained medically unexplained. When patients with somatoform or multisomatoform disorders were excluded, 28% of patients reported that their symptom remained medically unexplained at 5 years. Whether or not the symptom remained medically unexplained had no impact on 5-year symptom outcomes (P=.85), symptom severity (P=.61), serious illness worry (P=.75), or functional status (P=.82).
There was also no relationship between mood and anxiety disorders and symptom outcome (RR: 0.96, 95% CI: 0.87 to 1.07), although those with somatoform (RR: 0.64, 95% CI: 0.42 to 0.96) or multisomatoform disorders were less likely to improve (RR: 0.43%, 95% CI: 0.20 to 0.95) and more likely to be worried (somatoform: RR: 2.9, 95% CI: 1.7 to 4.9, multisomatoform: RR: 2.2, 95% CI: 1.1 to 4.6) about their symptom at 5 years.
Over the 5 years, there was gradual increase in the proportion of patients experiencing complete symptom resolution (2 weeks: 18%, 3 months: 36%, 5 years: 56%), and most subjects (60 to 70%) experienced 1 to 2 categories of symptom improvement by 5 years. Overall, 8% reported worsening of their symptom at any time point, although patients with somatoform or multisomatoform disorders were more than 3 times likely to reports worsening of their symptom than those without these disorders (3 months: RR: 3.14, 95% CI: 1.37 to 7.20; 5 years: RR: 3.03, 95% CI: 1.32 to 6.94).
Predictors of 5-year symptom resolution included: shorter symptom duration at presentation (median: 14 vs 21 days, P=.009), better baseline functional status (P=.02), younger age (50 vs 57 years, P<.001) and resolution by 3 months (RR: 4.6, 95% CI: 2.3 to 9.4). As with 2-week and 3-month outcomes, patients with symptom resolution were more satisfied (RR: 2.1, 95% CI: 1.8 to 2.5) and less worried (RR: 0.14, 95% CI: 0.61 to 0.33). Predictors of illness worry at 5 years included lack of improvement (RR: 5.5, 95% CI: 2.9 to 10.3), somatoform disorders (RR: 2.3, 95% CI: 1.0 to 5.4), and worse functioning (RR: 1.1, 95% CI: 1.0 to 1.2), but not mood or anxiety disorders or MUS.
DISCUSSION
Previous studies have focused on symptom improvement rather than symptom resolution and found that most patients (70% to 78%) improve by 2 weeks, improvement that is sustained through 3 months and 1 year.5,10,11 In this study, we found similar high rates improvement, although lower rates of symptom resolution (2 weeks: 18%, 3 months: 36% and 5 years: 56%). This was true across all categories of symptoms (Table 1). As with previous studies, we found that about a third of symptoms remain unexplained, even after 5 years of follow-up. The presence of a medically unexplained symptom did not affect the likelihood of symptom improvement or resolution for most patients. The majority of patients whose symptom remained unexplained did not have underlying mood, anxiety, or somatoform disorders, although patients with somatoform disorders were particularly likely to have MUS. Consistent with previous reports, we found a relationship between the number and severity of symptoms and mood, anxiety, and somatoform disorders.15,16,34 While mood or anxiety disorders did not affect symptom outcomes, somatoform disorders were particularly unlikely to improve.
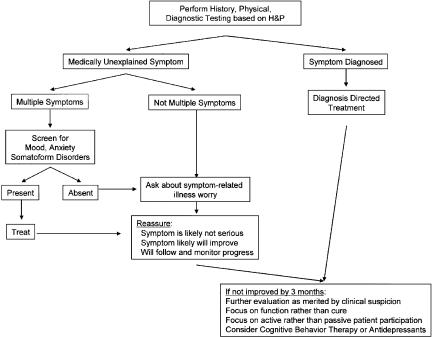
This study has implications regarding managing patients presenting with physical symptoms in primary care (Figure 2). In the majority of patients who receive a diagnosis, appropriate and specific therapy should be provided. For those with no clear diagnosis after the initial visit, symptomatic treatment with follow-up is indicated and patients should be counseled that most of them will experience symptom improvement within a couple of weeks, although resolution may take longer. As most patients with symptoms at 3 months have persistent symptoms at 5 years, clinicians should consider shifting their emphasis from diagnosis and cure to maximizing function for patients whose symptoms persist at 3 months. This should include trying to keep patients actively rather than passively engaged in their health care.14 Cognitive behavior therapy 35,36 and antidepressants may help with managing patients with persistent, troubling MUS,37 independent of any effect they may have on mood or anxiety. Patients with multiple symptoms, with greater symptom severity, stress, or poor functional status should be screened for mood or anxiety disorders. Medically unexplained symptoms, in the absence of a somatoform disorder, is not a harbinger of bad outcomes because they are equally likely to resolve. Patients with somatoform disorders are likely to have MUS and are particularly unlikely to improve.
FIGURE 2.
Symptom treatment algorithm.
Patient illness worry also has implications for symptom resolution. Postvisit illness worry correlated with symptom outcomes at all 3 time points. Our measure of worry should be distinguished from pathologic worry or hypochondriasis. Hypochondriasis is commonly associated with mood, somatoform and anxiety disorders38,39 and is relatively fixed over time.40 Most of our baseline worry was not hypochondriasis. While 68% of our patients were initially worried that their symptom could be serious, this fell to 32% immediately postvisit. Over 5 years the most important predictor of worry was lack of symptom improvement. Other predictors included worse functioning and the presence of a somatoform disorder. As postvisit worry is associated with symptom outcome, directly asking patients about their symptom-related worry may be beneficial. Statements such as “after my careful physical examination and after hearing your story, I'm sure that this isn't cancer or some other serious medical problem” can serve to help reassure patients. Such a patient-centered approach to understanding patients' symptom related concerns,26,41 improves satisfaction,42–44 trust, and simple reassurance may even be therapeutic.26 Providing reassurance that the clinician will continue to work with and follow the symptom over time can also help.
Our study has several limitations. First, this was a walk-in clinic, with most patients seeing the provider for the first time. Our findings may not generalize to established relationships. Second, while this was a consecutive sample of patients, they were not all presenting with their first-ever episode of the symptom. While this mirrors clinical reality, it also decreases the proportion of patients experiencing resolution, as duration predicts symptom outcome. Third, our study was conducted in a health system that provides free care, so our patient's threshold for seeking care may be lower than in other systems. Fourth, our study may be subject to recall bias as we relied on patient reports for whether a physical symptom was explained both immediately postvisit and at 5 years as well as whether or not the symptom improved at the 3 time points (2 weeks, 3 months, 5 years). There is ample data that shows that patients with somatoform disorders are resistant to accepting diagnoses and hence are less likely to report receiving 1. Fortunately, somatoform patients were a small segment of our study population. In these patients, we found what one would expect, a large portion of reporting receiving no explanation and low likelihood of symptom improvement. In the majority of patients without such disorders, there is previous data suggesting a discrepancy between patient reports of receiving a diagnosis and clinician reports of providing diagnostic information. One study using audiotapes found that, among patients without somatoform disorders, patient reports of receiving diagnostic information was more accurate than clinician reports.45 In addition, patients sometimes wrote in more than 1 symptom in response to our initial survey question about what problem was bringing them to the clinic. In those instances, on follow-up surveys, we listed all the symptoms, using the same wording that the patient provided, but only asked an overall question about whether the symptom(s) had improved and whether they had received a medical explanation. It is possible that 1 or more of the symptom either was explained or remained medically unexplained and the patient response would not capture this subtlety. It is likely that the patient responses focused on persistently bothersome symptoms and thus may have over estimated the overall proportion of symptoms that remained medically unexplained. However, our finding that 34% of symptoms remained medically unexplained is consistent with the results from studies that used other methods for determining whether or not a symptom was medically unexplained and there was no differential bias in which patients reporting MUS had worse outcomes.
A fifth limitation is that our study may have been underpowered to show clinically significant differences in the relationship between depression or anxiety disorders and having a medically unexplained symptom. For both mood and anxiety disorders, our study was sufficiently powered to show a 9% difference in the rate of having MUS compared with patients with no mental disorders, for mood and anxiety disorders alone, we could have shown an 11% and 13% difference, respectively, as statistically significant. Sixth, our instrument for assessing the presence of somatoform disorders has good specificity but is relatively insensitive. In order to reduce this possibility, we also included a diagnosis of multisomatoform disorder, a diagnosis that only requires 3 symptoms of 2-year duration. Overall, we found that 17% of patients had either somatoform or multisomatoform disorders, very close to the prevalence of somatoform disorders reported in most primary care cohorts. It seems unlikely that the few miscategorized somatoform patients would significantly change our conclusions.
In summary, while most patients will experience symptom improvement, only about half have symptom resolution by 5 years. About a third of patients' symptoms will remain medically unexplained. Most patients with MUS do not have a mental disorder and for them, the lack of explanation does not affect symptom outcome. The number and severity of symptoms correlates with mood and anxiety disorders, although not with MUS. Most patients with somatoform disorders will have MUS and few will improve. Poor baseline functional status, serious illness worry, and longer symptom duration at presentation predicts lack of resolution. Among patients without symptom resolution by 3 months, clinician's should focus on maximizing function rather than on cure.
Table 2.
Medical Explanation of Symptom by Mental Disorder
| Symptom Was | ||
|---|---|---|
| Medically Explained, n (%) | Medically Unexplained, n (%) | |
| No mental disorder (n=347) | 235 (68) | 112 (32) |
| Depressive disorder (n=106) | 62 (59) | 44 (42) |
| Anxiety disorder (n=74) | 45 (61) | 29 (39) |
| Somatoform disorder (n=85) | 14 (16) | 71 (84) |
References
- 1.Schappert SM, Nelson C. National Ambulatory Medical Care Survey 1995–96 summary. Vital Health Stat. 1999;13:1–122. [PubMed] [Google Scholar]
- 2.Von Korff M, Deyo RA, Cherkin D, Barlow W. Back pain in primary care: outcomes at one year. Spine. 1993;18:855–62. doi: 10.1097/00007632-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Valdini AF, Steinhardt S, Valicenti J, Jaffe A. One-year follow up of fatigued patients. J Fam Pract. 1998;26:33–8. [PubMed] [Google Scholar]
- 4.Kroenke K, Lucas CA, Rosenberg ML, Scherokman BJ, Herbers JE. One-year outcome in patients with a chief complaint of dizziness. J Gen Intern Med. 1994;9:684–9. doi: 10.1007/BF02599010. [DOI] [PubMed] [Google Scholar]
- 5.Weber BE, Kapoor WN. Evaluation and outcomes of patients with palpitations. Am J Med. 1996;100:138–48. doi: 10.1016/s0002-9343(97)89451-x. [DOI] [PubMed] [Google Scholar]
- 6.Wasson JH, Sox HC, Sox CH. The diagnosis of abdominal pain in ambulatory male patients. Med Decis Making. 1981;1:215–24. doi: 10.1177/0272989X8100100302. [DOI] [PubMed] [Google Scholar]
- 7.Arndorff DK, Knottnerus JA, Hujjnen LG, Sarmans R. How well do general practitioners manage dyspepsia? J R Coll Gen Pract. 1989;39:499–502. [PMC free article] [PubMed] [Google Scholar]
- 8.Martina B, Buchell C, Strotz M, Battega E, Gyr N. First clinical judgement by primary care physicians distinguishes well between nonorganic and organic causes of abdominal or chest pain. J Gen Intern Med. 1997;12:459–65. doi: 10.1046/j.1525-1497.1997.00083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kroenke K, Jackson JL. Outcome in general medical patients presenting with common symptoms: a prospective study with a 2-week and a 3-month follow-up. Fam Pract. 1998;15:398–403. doi: 10.1093/fampra/15.5.398. [DOI] [PubMed] [Google Scholar]
- 10.Marple RL, Kroenke K, Lucey CR, Wilder J, Lucas CA. Concerns and expectations in patients presenting with physical complaints frequency, physician perceptions and actions, and two-week outcome. Arch Intern Med. 1997;157:1482–8. [PubMed] [Google Scholar]
- 11.Kirmayer LJ, Groleau D, Looper KJ, Dao MD. Explaining medically unexplained symptoms. Can J Psychiatr. 2004;49:663–72. doi: 10.1177/070674370404901003. [DOI] [PubMed] [Google Scholar]
- 12.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86:262–6. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K, Arrington ME, Mangelsdorff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med. 1990;150:1685–9. doi: 10.1001/archinte.150.8.1685. [DOI] [PubMed] [Google Scholar]
- 14.Richardson RD, Engel CC., Jr Evaluation and management of medically unexplained physical symptoms. Neurologist. 2004;10:18–30. doi: 10.1097/01.nrl.0000106921.76055.24. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med. 1997;103:339–47. doi: 10.1016/s0002-9343(97)00241-6. [DOI] [PubMed] [Google Scholar]
- 16.Jackson JL, O'Malley PG, Kroenke K. Clinical predictors of mental disorders among medical outpatients. Validation of the “S4” model. Psychosomatics. 1998;39:431–6. doi: 10.1016/S0033-3182(98)71302-7. [DOI] [PubMed] [Google Scholar]
- 17.Jackson JL, Houston JS, Hanling SR, Terhaar KA, Yun JS. Clinical predictors of mental disorders among medical outpatients. Arch Intern Med. 2001;161:875–9. doi: 10.1001/archinte.161.6.875. [DOI] [PubMed] [Google Scholar]
- 18.Smith RC, Gardiner JC, Lyles JS, et al. Exploration of DSM-IV criteria in primary care patients with medically unexplained symptoms. Psychosom Med. 2005;67:123–9. doi: 10.1097/01.psy.0000149279.10978.3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feder A, Olfson M, Gameroff M, et al. Medically unexplained symptoms in an urban general medicine practice. Psychosomatics. 2001;42:261–8. doi: 10.1176/appi.psy.42.3.261. [DOI] [PubMed] [Google Scholar]
- 20.Nease DE, Jr, Volk RJ, Cass AR. Does the severity of mood and anxiety symptoms predict health care utilization? J Fam Pract. 1999;48:769–77. [PubMed] [Google Scholar]
- 21.Creed F, Barsky A. A systematic review of the epidemiology of somatisation disorder and hypochondriasis. J Psychosom Res. 2004;56:391–408. doi: 10.1016/S0022-3999(03)00622-6. [DOI] [PubMed] [Google Scholar]
- 22.Henningsen P, Zimmermann T, Sattel H. Medically unexplained physical symptoms, anxiety, and depression a meta-analytic review. Psychosom Med. 2003;65:528–33. doi: 10.1097/01.psy.0000075977.90337.e7. [DOI] [PubMed] [Google Scholar]
- 23.Maiden NL, Hurst NP, Lochhead A, Carson AJ, Sharpe M. Medically unexplained symptoms in patients referred to a specialist rheumatology service prevalence and associations. Rheumatology (Oxford) 2003;42:108–12. doi: 10.1093/rheumatology/keg043. [DOI] [PubMed] [Google Scholar]
- 24.Jackson JL, Strong J, Cheng E, Meyer G. Patients, diagnoses, and procedures in a military internal medicine clinic, comparison with civilian practices. Military Med. 1999;164:194–7. [PubMed] [Google Scholar]
- 25.Jackson JL, O'Malley PG, Kroenke K. A psychometric comparison of military and civilian medical practices. Military Med. 1999;164:112–5. [PubMed] [Google Scholar]
- 26.Jackson JL, Kroenke K. The effect of unmet expectations among adults presenting with physical symptoms. Ann Intern Med. 2001;134:889–97. doi: 10.7326/0003-4819-134-9_part_2-200105011-00013. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Nelson EC, Sjerbpirme CD, Stewart A. Preliminary tests of a 6-item general health survey: a patient application. In: Ware JE, Stewart AL, editors. Measuring Functioning and Well Being: The Medical Outcomes Study Approach. 1st ed. Durham: Duke University Press; 1997. pp. 199–308. eds. In. [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-15 validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care the PRIME-MD 1000 study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 30.Loerch B, Szegedi A, Kohnen R, Benkert O. The primary care evaluation of mental disorders (PRIME-MD), German version: a comparison with the CIDI. J Psychiatr Res. 2000;34:211–20. doi: 10.1016/s0022-3956(00)00005-4. [DOI] [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, deGruy FV, III, et al. Multisomatoform disorder. An alternative to undifferentiated somatoform disorder for the somatizing patient in primary care. Arch Gen Psychiatr. 1997;54:352–8. doi: 10.1001/archpsyc.1997.01830160080011. [DOI] [PubMed] [Google Scholar]
- 32.Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE. Patients' ratings of outpatient visits in different practice settings results from the Medical Outcomes Study. JAMA. 1993;270:1449–53. [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JB, Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 34.O'Malley PG, Jackson JL, Kroenke K, Yoon IK, Hornstein E, Dennis GJ. The value of screening for psychiatric disorders in rheumatology referrals. Arch Intern Med. 1998;153:2357–62. doi: 10.1001/archinte.158.21.2357. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes a critical review of controlled clinical trials. Psychother Psychosom. 2000;69:205–15. doi: 10.1159/000012395. [DOI] [PubMed] [Google Scholar]
- 36.Speckens AE, van Hemert AM, Spinhoven P, Hawton KE, Bolk JH, Rooijmans HG. Cognitive behavioural therapy for medically unexplained physical symptoms a randomised controlled trial. BMJ. 1995;311:1328–32. doi: 10.1136/bmj.311.7016.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Malley PG, Jackson JL, Santoro J, Tomkins G, Balden E, Kroenke K. Antidepressant therapy for unexplained symptoms and symptom syndromes. J Fam Pract. 1999;48:980–90. [PubMed] [Google Scholar]
- 38.Noyes R, Jr, Kathol RG, Fisher MM, Phillips BM, Suelzer MT, Woodman CL. Psychiatric comorbidity among patients with hypochondriasis. Gen Hosp Psychiatr. 1994;16:78–87. doi: 10.1016/0163-8343(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 39.Noyes R., Jr The relationship of hypochondriasis to anxiety disorders. Gen Hosp Psychiatr. 1999;21:8–17. doi: 10.1016/s0163-8343(98)00063-2. [DOI] [PubMed] [Google Scholar]
- 40.Noyes R, Jr, Kathol RG, Fisher MM, Phillips BM, Suelzer MT, Woodman CL. One-year follow-up of medical outpatients with hypochondriasis. Psychosomatics. 1994;35:533–45. doi: 10.1016/S0033-3182(94)71722-9. [DOI] [PubMed] [Google Scholar]
- 41.Hernbest RJ, Stewart M. Patient-centeredness in the consultation. Does it really make a difference? Fam Pract. 1990;7:28–33. doi: 10.1093/fampra/7.1.28. [DOI] [PubMed] [Google Scholar]
- 42.Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001;50:1057–62. [PubMed] [Google Scholar]
- 43.Roter DL, Hall JA, Katz NR. Relations between physicians' behaviors and analogue patients' satisfaction, recall, and impressions. Med Care. 1987;25:437–51. doi: 10.1097/00005650-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Satisfaction, gender, and communication in medical visits. Med Care. 1994;32:1216–31. doi: 10.1097/00005650-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 45.Jackson JL. Communication about symptoms in walk-in clinics. J Gen Intern Med. 2005;20(suppl 1):69–70. [Google Scholar]