Abstract
Our mutagenesis study has investigated all amino acid mutations in the penicillin-binding domain of PBP 1A from Hungarian pneumococcal isolate 3191 to determine the importance of every mutation in the development of penicillin and cefotaxime resistance. Our data reveal that mutations at amino acid positions 574 to 577 and position 539 cause penicillin and cefotaxime resistance.
β-Lactam antibiotics inhibit the growth of pneumococci by inactivation of cell-wall-synthesizing penicillin-binding proteins (PBPs). Pneumococcal resistance to β-lactams is essentially due to a complex production of altered PBPs with decreased affinities for the antibiotic (5, 6, 18). Transformation studies have shown that high-level penicillin resistance requires altered PBPs 2X, 2B, and 1A (1), while only altered PBPs 2X and 1A are required to confer high-level cefotaxime resistance (9). A functional murMN operon is required for expression of PBP-mediated β-lactam resistance in the pneumococcus (4, 17). We have recently shown that in conjunction with altered PBPs, alteration in MurM may assist in the development of β-lactam resistance (13). Altered PBP 1A is particularly essential for high-level resistance (11, 14, 16), and the identification of resistance-causing alterations in PBP 1A has a number of benefits. Firstly, it could assist in the design of improved β-lactam antibiotics to counter bacterial resistance to the presently available antibiotics. Secondly, it could assist in the development of genetic tests (multiplex PCRs and microarrays) for the rapid diagnosis of high-level penicillin and cephalosporin resistance in the pneumococcus. With this in mind, we have analyzed the altered PBP 1A from β-lactam-resistant pneumococcal isolate 3191 (penicillin MIC, 16 μg/ml; cefotaxime MIC, 4 μg/ml), a representative of a Hungarian serotype 19A clone isolated during the period 1997 to 1998. Site-directed mutagenesis (SDM) was used to investigate all 43 amino acid mutations located in the penicillin-binding domain (PBD) of PBP 1A, and we report on their importance in the development of penicillin and cefotaxime resistance.
Pneumococcal strains were routinely cultured at 37°C in 5% CO2 on Mueller-Hinton agar supplemented with 5% horse blood. Antibiotic susceptibility testing was performed with the agar dilution method as specified by the National Committee for Clinical Laboratory Standards (10). Chromosomal DNAs were extracted from bacterial cells, and pbp genes were amplified from the chromosomal DNAs by PCR with methods that have been described previously (16). For pbp2X, pbp2B, and pbp1A PCR, primers have been described previously (15). PCR products were sequenced by using the BigDye Terminator Cycle Sequencing kit (Applied Biosystems, Foster City, Calif.) and an Applied Biosystems Model 310 automated DNA sequencer. Genes were cloned into plasmid pGEM-3Zf (Promega Corp., Madison, Wis.), and recombinant plasmid DNA was extracted from transformed Escherichia coli by using standard techniques (12). The QuickChange Site-Directed Mutagenesis kit (Stratagene, La Jolla, Calif.) was used to create specific mutations in the resistant pbp1A gene from isolate 3191. Unencapsulated, β-lactam-susceptible (penicillin and cefotaxime MICs, 0.015 μg/ml) laboratory strain R6 was used as the recipient in transformation studies. Cloned pbp genes were used as transforming DNA. Pneumococcal transformation and selection for transformants were performed by using previously described methods (14).
We present a mutagenesis study in which we investigated all amino acid mutations in the PBD of an altered PBP 1A from β-lactam-resistant isolate 3191 to determine the importance of every mutation in the development of penicillin and cefotaxime resistance. The PBD-encoding region of PBP 1A was sequenced from isolate 3191 and was compared to that of susceptible laboratory strain R6. This region of PBP 1A revealed 22% nucleotide sequence divergence, resulting in 43 amino acid mutations in the protein (Fig. 1). Before SDM of PBP 1A from isolate 3191 could commence, we first needed to obtain the correct genetic background with respect to PBPs 2X, 2B, and 1A. This was accomplished by using strain R6 as a recipient in transformation experiments. Strain R6 was first transformed with pbp2X and 2B resistance genes from isolate 3191, resulting in R63191/2X/2B strains showing penicillin and cefotaxime MICs of 0.25 μg/ml. When strain R63191/2X/2B was further transformed with the pbp1A resistance gene, R63191/2X/2B/1A transformants could be cultured on plates containing up to 1 μg of penicillin per ml. These R63191/2X/2B/1A strains revealed penicillin and cefotaxime MICs of 4 and 2 μg/ml, respectively. DNA sequencing confirmed the introduction of altered genes into transformed R6 strains.
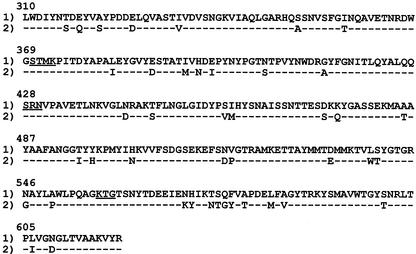
FIG. 1.
Amino acid sequences of the PBD of PBP 1A from susceptible strain R6 (line 1) and isolate 3191 (line 2). Only those positions that differ from strain R6 are shown in line 2. The conserved amino acid sequence motifs (STMK, SRN, KTG) are underlined. Sequences are numbered according to the published sequence of Martin and coworkers (7).
For SDM analysis of PBP 1A, we chose to inactivate amino acid mutations (substitutions were reversed) in altered PBP 1A from isolate 3191, followed by performing an assay for decreased resistance. The reason for choosing this approach is explained below. If we went the alternate route and assayed for increased resistance after introducing mutations into an unaltered pbp1A gene and transforming strain R6, the Hex mismatch repair system of pneumococci would have resulted in a high-frequency cancellation of this mutation at the donor-recipient heteroduplex DNA stage, resulting in very few mutant transformants. Our approach to SDM introduces an extensively altered pbp1A gene into strain R6, which saturates and inhibits the mismatch repair system as a result of excess mismatches, resulting in high-frequency transformation and recombination of the altered pbp1A gene into the genome of strain R6 (2). SDM experiments on the pbp1A gene from isolate 3191 were used to reverse the 43 amino acid substitutions located in the PBD of PBP 1A (the substitutions were reversed to the amino acid residues of the susceptible R6 strain). This was followed by transformation of R63191/2X/2B with the mutagenized pbp1A DNA, followed by an analysis of whether the reversal of an amino acid change resulted in R63191/2X/2B/1A transformants with decreased penicillin and cefotaxime resistance. For each mutagenesis, five transformants were picked and analyzed. DNA sequencing of transformants confirmed the presence of mutagenized PBP 1A. A total of 25 mutagenic primers were used to analyze the 43 mutations in the PBD of PBP 1A from isolate 3191. Some mutations were individually reversed with mutagenic primers and were investigated. Where several mutations were located very close together, they were all reversed by using a single mutagenic primer. Table 1 shows the mutagenic primers used and the effect amino acid reversals had on the level of resistance in mutagenized R63191/2X/2B/1A strains compared to those of strain R63191/2X/2B/1A (penicillin MIC, 4 μg/ml; cefotaxime MIC, 2 μg/ml). Mutant 574−575−576−577− was created by reversing four consecutive amino acid substitutions (Thr-574 by Asn, Ser-575 by Thr, Gln-576 by Gly, and Phe-577 by Tyr), which resulted in maximum penicillin and cefotaxime MICs of 0.25 μg/ml. Mutant 539− was created by the reversal of Leu-539 by Trp, which resulted in maximum penicillin and cefotaxime MICs of 0.5 μg/ml. The above mutant strains only grew on plates containing a maximum concentration of 0.25 μg of penicillin per ml. Inactivation of the other remaining 38 mutations in the PBD of PBP 1A had no effect on resistance levels. The four consecutive substitutions at positions 574 to 577 are present in all published PBP 1A sequences from pneumococcal isolates with penicillin or cefotaxime MICs of ≥0.25 μg/ml. These four substitutions always occur together as a cluster and never appear as individual substitutions. Data therefore suggests that mutations at positions 574 to 577 are vital in the development of penicillin and cefotaxime resistance. The substitution of Leu-539 by Trp does not appear in previously published PBP 1A data and is a novel resistance mutation associated with isolate 3191. Interestingly, altered PBP 1A from isolate 3191 does not have a substitution at position 371, adjacent to the active-site Ser-370. All published PBP 1A sequences from high-level resistant pneumococcal isolates have shown a replacement of Thr-371 by Ser or Ala, and the importance of this position has previously been confirmed (15). However, in isolate 3191, position 371 in PBP 1A appears to play no role in the development of penicillin and cefotaxime resistance. Hungarian isolate 3191 is therefore unique with respect to its mechanism for development of penicillin and cefotaxime resistance. In addition to its novel involvement of altered MurM in the development of resistance (13), its altered PBP 1A is deficient of the characteristic substitution at position 371 and contains a novel resistance-causing replacement of Leu-539 by Trp. Our data further show that resistance-causing mutations in PBP 1A carry equal weight with respect to penicillin and cefotaxime resistance in the pneumococcus. This is in contrast to some mutations in PBP 2X, which show different (sometimes opposite) influence on penicillin and cefotaxime resistance (3, 8). Therefore, although altered PBP 1A is an essential component in the step to high-level penicillin and cefotaxime resistance, we hypothesize that the mutational composition of altered PBP 2X is the vital component which dictates the final level of penicillin and cefotaxime resistance reached through the collective participation of altered PBP 2X, 2B, and 1A. This hypothesis is reached by excluding PBP 1A, leaving us with PBP 2X, which is the only remaining PBP resistance determinant that is common to both penicillin and cefotaxime.
TABLE 1.
Reversal of substitutions at amino acid positions in PBP 1A from isolate 3191 and the resulting effect of this mutagenesis on resistance levels in mutagenized R63191/2X/2B/1A strains compared to those for R63191/2X/2B/1A (penicillin MIC, 4 μg/ml; cefotaxime MIC, 2 μg/ml)
| Mutagenic primer | Position of amino acids where reversal of substitutions occurred | Drug MIC (μg/ml) for mutagenized R63191/2X/2B/1A
|
|
|---|---|---|---|
| Penicillin | Cefotaxime | ||
| 1 | 316, 318, 321 | 4 | 2 |
| 2 | 326 | 4 | 2 |
| 3 | 333 | 4 | 2 |
| 4 | 351, 358 | 4 | 2 |
| 5 | 382, 388 | 4 | 2 |
| 6 | 393, 395, 397 | 4 | 2 |
| 7 | 405 | 4 | 2 |
| 8 | 414 | 4 | 2 |
| 9 | 443, 447 | 4 | 2 |
| 10 | 458, 459 | 4 | 2 |
| 11 | 473, 475 | 4 | 2 |
| 12 | 485 | 4 | 2 |
| 13 | 495, 497 | 4 | 2 |
| 14 | 503 | 4 | 2 |
| 15 | 517, 518 | 4 | 2 |
| 16 | 533 | 4 | 2 |
| 17 | 539 | 0.5 | 0.5 |
| 18 | 540 | 4 | 2 |
| 19 | 546, 550 | 4 | 2 |
| 20 | 570, 571 | 4 | 2 |
| 21 | 574, 575, 576, 577 | 0.25 | 0.25 |
| 22 | 579 | 4 | 2 |
| 23 | 583, 585 | 4 | 2 |
| 24 | 600 | 4 | 2 |
| 25 | 606, 609 | 4 | 2 |
In conclusion, we have shown that amino acid residues 574 to 577 and residue 539 are important positions in PBP 1A with respect to the interaction with penicillin and cefotaxime in the pneumococcus. In Hungarian isolate 3191, mutation at these positions cause penicillin and cefotaxime resistance.
Nucleotide sequence accession numbers.
PBP 1A sequence data appear in the EMBL, GenBank, and DDBJ nucleotide sequence data libraries under the following accession numbers: isolate 3191, AY072702; strain R6, M90527.
REFERENCES
- 1.Barcus, V. A., K. Ghanckar, M. Yeo, T. J. Coffey, and C. G. Dowson. 1995. Genetics of high level penicillin resistance in clinical isolates of Streptococcus pneumoniae. FEMS. Microbiol. Lett. 126:299-303. [DOI] [PubMed] [Google Scholar]
- 2.Claverys, J.-P., M. Prudhomme, I. Mortier-Barriére, and B. Martin. 2000. Adaptation to the environment: Streptococcus pneumoniae, a paradigm for recombination-mediated genetic plasticity? Mol. Microbiol. 35:251-259. [DOI] [PubMed] [Google Scholar]
- 3.Coffey, T. J., M. Daniels, L. K. McDougal, C. G. Dowson, F. C. Tenover, and B. G. Spratt. 1995. Genetic analysis of clinical isolates of Streptococcus pneumoniae with high-level resistance to expanded-spectrum cephalosporins. Antimicrob. Agents Chemother. 39:1306-1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Filipe, S. R., and A. Tomasz. 2000. Inhibition of the expression of penicillin resistance in Streptococcus pneumoniae by inactivation of cell wall muropeptide branching genes. Proc. Natl. Acad. Sci. USA 97:4891-4896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hakenbeck, R., H. Ellerbrok, T. Briese, S. Handwerger, and A. Tomasz. 1986. Penicillin-binding proteins of penicillin-susceptible and resistant pneumococci: immunological relatedness of altered proteins and changes in peptides carrying the β-lactam binding site. Antimicrob. Agents Chemother. 30:553-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hakenbeck, R., M. Tarpay, and A. Tomasz. 1980. Multiple changes of penicillin-binding proteins in penicillin-resistant clinical isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 17:364-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin, C., T. Briese, and R. Hakenbeck. 1992. Nucleotide sequences of genes encoding penicillin binding proteins from Streptococcus pneumoniae and Streptococcus oralis with high homology to Escherichia coli penicillin binding proteins 1A and 1B. J. Bacteriol. 174:4517-4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mouz, N., A.-M. Di Guilmi, E. Gordon, R. Hakenbeck, O. Dideberg, and T. Vernet. 1999. Mutations in the active site of penicillin-binding protein PBP 2X from Streptococcus pneumoniae. J. Biol. Chem. 274:19175-19180. [DOI] [PubMed] [Google Scholar]
- 9.Muñoz, R., C. G. Dowson, M. Daniels, T. J. Coffey, C. Martin, R. Hakenbeck, and B. G. Spratt. 1992. Genetics of resistance to third-generation cephalosporins in clinical isolates of Streptococcus pneumoniae. Mol. Microbiol. 6:2461-2465. [DOI] [PubMed] [Google Scholar]
- 10.National Committee for Clinical Laboratory Standards. 2000. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A5, 5th ed., National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 11.Reichmann, P., A. König, A. Marton, and R. Hakenbeck. 1996. Penicillin-binding proteins as resistance determinants in clinical isolates of Streptococcus pneumoniae. Microbial Drug Resist. 2:177-181. [DOI] [PubMed] [Google Scholar]
- 12.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 13.Smith, A. M., and K. P. Klugman. 2001. Alterations in MurM, a cell wall muropeptide branching enzyme, increase high-level penicillin and cephalosporin resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 45:2393-2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith, A. M., and K. P. Klugman. 2000. Non-penicillin-binding protein mediated high-level penicillin and cephalosporin resistance in a Hungarian clone of Streptococcus pneumoniae. Microbial Drug Resist. 6:105-110. [DOI] [PubMed] [Google Scholar]
- 15.Smith, A. M., and K. P. Klugman. 1998. Alterations in PBP 1A essential for high-level penicillin resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 42:1329-1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith, A. M., K. P. Klugman, T. J. Coffey, and B. G. Spratt. 1993. Genetic diversity of penicillin-binding protein 2B and 2X genes from Streptococcus pneumoniae in South Africa. Antimicrob. Agents Chemother. 37:1938-1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weber, B., K. Ehlert, A. Diehl, P. Reichmann, H. Labischinski, and R. Hakenbeck. 2000. The fib locus in Streptococcus pneumoniae is required for peptidoglycan crosslinking and PBP-mediated β-lactam resistance. FEMS Microbiol. Lett. 188:81-85. [DOI] [PubMed] [Google Scholar]
- 18.Zighelboim, S., and A. Tomasz. 1980. Penicillin-binding proteins of multiply antibiotic-resistant South African strains of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 17:434-442. [DOI] [PMC free article] [PubMed] [Google Scholar]