Abstract
Background
Mindfulness-based stress reduction (MBSR) and massage may be useful adjunctive therapies for chronic musculoskeletal pain.
Objective
To evaluate the feasibility of studying MBSR and massage for the management of chronic pain and estimate their effects on pain and mood.
Design
Randomized trial comparing MBSR or massage with standard care.
Participants
Thirty patients with chronic musculoskeletal pain.
Measurements
Pain was assessed with 0 to 10 numeric rating scales. Physical and mental health status was measured with the SF-12.
Results
The study completion rate was 76.7%. At week 8, the massage group had average difference scores for pain unpleasantness of 2.9 and mental health status of 13.6 compared with 0.13 (P<.05) and 3.9 (P<.04), respectively, for the standard care group. These differences were no longer significant at week 12. There were no significant differences in the pain outcomes for the MBSR group. At week 12, the mean change in mental health status for the MBSR group was 10.2 compared with −1.7 in the standard care group (P<.04).
Conclusions
It is feasible to study MBSR and massage in patients with chronic musculoskeletal pain. Mindfulness-based stress reduction may be more effective and longer-lasting for mood improvement while massage may be more effective for reducing pain.
Keywords: mindfulness-based stress reduction, massage, chronic pain, mental health, integrative medicine
Chronic pain is a challenging problem affecting 75 to 85 million people in the U.S., with 50 million being partially or totally disabled.1 Comorbidity with depression and the influence of psychosocial factors 2 make chronic pain a particularly difficult problem for conventional medicine. An estimated 20% of those affected seek help through complementary and alternative medicine.3
There is growing evidence supporting the efficacy of mind-body therapies for chronic pain. Mindfulness-based stress reduction (MBSR) is an intervention that may be effective in reducing pain and emotional distress, and improving function in patients with chronic pain.4–7 However, as there have been few randomized controlled studies, the true value of this therapy remains uncertain.8 Evidence for the effectiveness of massage in chronic musculoskeletal pain is growing,9 as 3 randomized trials 10–12 have shown positive effects of massage on pain and functional status.
The purpose of this study was to determine the feasibility of evaluating MBSR and massage for the treatment of chronic musculoskeletal pain and to estimate treatment effects in a challenging patient population.
METHODS
This study was a 3-arm randomized unblinded trial comparing MBSR or massage with standard care among 30 adults with musculoskeletal pain for greater than 3 months recruited from 2 general internal medicine practices at the University of Virginia. Exclusion criteria included: prisoner status, cognitive impairment, lack of reliable transportation, or being pregnant. The sample size of 10 per group was established arbitrarily as a reasonable number to estimate the feasibility of a larger trial. All participants continued their use of prescribed pain medication.
Patients were recruited with a flyer distributed during clinic visits. A computer-generated random number sequence was used to assign patients to groups. Assessment of pain sensation and unpleasantness was performed with 0 to 10 numeric rating scales 13–16 obtained at baseline, 4, 8, and 12 weeks. A radio analogy was used to distinguish between pain sensation and unpleasantness with pain sensation the volume of the pain and unpleasantness how annoying the pain is. Participants reported average pain ratings over the previous week with 0=“none” and 10=“worst imaginable.” Global physical and mental health status was measured with the SF-12.17 The SF-12 scores are weighted averages of item responses, normed so that 50 represents the average with a standard deviation of 10. Participants' medication lists were obtained by chart review.
Mindfulness-based stress reduction is a mind-body intervention described by Kabat-Zinn.18 The participants met weekly for eight 2½ hour sessions. Meditation and yoga techniques were practiced to foster mindfulness (present moment, nonjudgmental awareness). Audiotaped meditation exercises were assigned as daily home practice. Participants were encouraged to use these skills in moments of stress and/or pain.
One-hour massage sessions were given once per week for 8 weeks by 3 licensed massage therapists. Massage techniques were at the discretion of the therapists and included Swedish, deep-tissue, neuromuscular, and pressure-point techniques. We specifically excluded music, scented oils, and energy techniques such as Reiki or therapeutic touch.
Standard care at the 2 practices was to be seen by a primary care physician at least every 3 months with medication adjustments made as indicated.
Participants were given $30 upon completion of the study.
Difference scores were computed by subtracting the pain report and SF-12 scores at weeks 8 and 12 from those at baseline. Differences were compared using T-tests.
RESULTS
Twenty-three of the participants were female and 7 were male. The average age was 46.5 and the mean education level was 12 years. Half the participants reported incomes less than $14,000 with an average income of $23,500. There were no significant differences among the groups in gender, age, education, or income.
Sixty percent of the recruited participants were taking at least 1 narcotic medication and 40% were taking only nonnarcotic medications.
Overall, the completion rate was 76.7%. In the MBSR arm, 3 participants dropped out of the study before attending any classes, 1 stopped coming because of transportation issues, and 1 attended only 3 classes but completed all the assessments. The remaining 5 attended 7 of 8 sessions. Two of the standard care participants dropped out and 1 of the massage participants dropped out soon after consent.
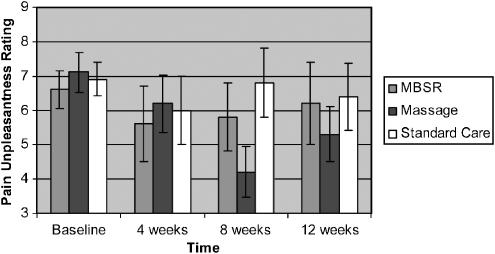
There were no significant differences among the groups in pain reports at baseline. Among trial completers, at week 8 the massage group had an average difference score in pain unpleasantness of 2.9 (SD=2.9) compared with the standard care group difference score of 0.13 (SD=2.4), P <.05 (t=2.1, df=15). The differences in pain unpleasantness scores were no longer significant at week 12. Differences in pain sensation scores showed a similar trend at Week 8 but this difference was not statistically significant. There were no significant differences in pain outcomes for the MBSR group (Figure 1).
FIGURE 1.
Average pain unpleasantness scores with standard errors for mindfulness-based stress reduction, massage and standard care groups from baseline through 12 weeks for participants who completed the study (n=23).
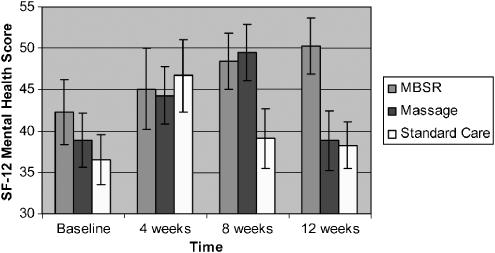
Changes in the global mental health SF-12 scores were observed while there were no significant changes in the global physical health SF-12 scores. At week 8, the massage group had an average difference score in mental health status of 13.6 (SD=8.9) compared with the standard care group with a difference score of 3.9 (SD=28.0), P <.04 (t=2.2, df=14). By week 12, the improvement in mental health status for the massage group had returned to baseline levels.
In contrast, the MBSR difference scores in mental health status at week 8 were nonsignificant, compared with the standard care group, but by week 12 the improvement in mental health status for the MBSR group achieved statistical significance with an average improvement of 10.2 (SD=8.7) compared with a decrease in mental health scores of −1.7 in the standard care group (t=2.3, df=10, P <.04) (Figure 2).
FIGURE 2.
Average SF-12 mental health scores with standard errors for mindfulness-based stress reduction, massage and standard care groups from baseline through 12 weeks for participants who completed the study (n=23).
DISCUSSION
The primary purpose of this study was to determine whether patients with chronic musculoskeletal pain who were of largely lower socioeconomic status would participate in a randomized trial that includes 2 alternative therapies. We specifically targeted patients who were likely to have the most barriers to participation. Even with this “worst-case scenario” the completion rate was 76%. We conclude that it is feasible to study these therapies in this patient group. There were 32 patients who were eligible for the study who decided not to participate and future studies should address issues such as distance, transportation, and timing of the MBSR classes to improve the participation rate. Although the completion rate differences in treatment group was not significant, there was a trend for more participants in the massage group to complete the study (90%) compared with the MBSR group (60%). This may be because of differences in the commitment required by the different modalities, or it may be merely chance.
The secondary aim of the study was to provide estimates of the treatment effects of the 2 therapies studied, in comparison with standard care. There were statistically significant differences noted between the treatment groups which have important implications for clinical care and future research. First, the massage group had statistically significant improvements in pain unpleasantness and mental health ratings on the SF-12 at week 8 compared with the standard care group. Pain sensation ratings showed a similar trend but did not reach statistical significance. Interestingly, this benefit was attenuated at week 12. It appears that massage was effective in improving pain but that benefit was lost when the massage sessions were ended.
Second, among the MBSR completers, there was a statistically significant improvement in mental health ratings on the SF-12 at week 12 compared with baseline, indicating this effect may be more durable than the pain effects seen with massage. With MBSR, patients learn a life skill, and the beneficial effects of this can conceivably grow rather than diminish over time.
The 2 interventions had different effects on the complex components of chronic pain. Understanding which modalities are most effective at improving which component will help us design treatment programs with the highest likelihood of success.
There were several limitations of this study, including the small sample size and that more patients dropped out of the MBSR arm. Other limitations include a limited duration follow-up and that the massage therapists used no music or massage oils which may not mimic actual practice. Finally, differences in contact time between the therapies may be a confounder.
In conclusion, MBSR and massage appear promising for the treatment of chronic musculoskeletal pain and even socioeconomically disadvantaged patients will participate in trials of these modalities. In addition, massage therapy can have a positive impact on pain unpleasantness, but this impact attenuates over time. Mindfulness-based stress reduction may have a positive impact on mental health in these patients, an effect that seems to persist after the classes are completed. Together, these findings provide support for conducting larger studies to more definitively establish the optimal role of massage and MBSR in the treatment of chronic musculoskeletal pain. In the meantime, it is both feasible and promising to offer these therapies to chronic pain patients in the ambulatory setting.
Acknowledgments
This study was supported in part by Grant 1D12HP00040-03: Academic Administrative Units in Primary Care, Department of Health and Human Services and in part by the John W. Kluge Foundation.
REFERENCES
- 1.Berman BM, Swyers JP. Complementary and alternative therapies for chronic pain establishing a research agenda for investigating alternative medial interventions for chronic pain. Primary Care: Clin Office Pract. 1997;24:743–58. doi: 10.1016/s0095-4543(05)70308-0. [DOI] [PubMed] [Google Scholar]
- 2.Broderick JE. Mind-body medicine in rheumatologic disease. [review] [68 refs] Rheum Dis Clin N Am. 2000;26:161–76. doi: 10.1016/s0889-857x(05)70129-0. [DOI] [PubMed] [Google Scholar]
- 3.Wolsko PM, Eisenberg DM, Davis RB, Phillips RS. Use of mind-body medical therapies. J Gen Intern Med. 2004;19:43–50. doi: 10.1111/j.1525-1497.2004.21019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caudill M, Schnable R, Suttermeister P, et al. Decreased clinic utilization by chronic pain patients: response to behavioral medicine intervention. Clin J Pain. 1995;7:305–10. doi: 10.1097/00002508-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8:163–90. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 6.Kabat-Zinn J, Lipworth L, Burney R, Sellers W. Four year follow-up of a meditation-based program for the self-regulation of chronic pain treatment outcomes and compliance. Clin J Pain. 1986;2:159–73. [Google Scholar]
- 7.Kaplan KH, Goldenberg DL, Galvin-Nadeau M. The impact of a meditation-based stress reduction program on fibromyalgia. Gen Hosp Psychiatr. 1993;15:284–9. doi: 10.1016/0163-8343(93)90020-o. [DOI] [PubMed] [Google Scholar]
- 8.Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosom Med. 2002;64:71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Cherkin D, Sherman K, Deyo R, Shekelle P. A review of the evidence for the effectiveness, safety and cost of acupuncture, massage therapy and spinal manipulation for back pain. Ann Intern Med. 2003;138:898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 10.Cherkin DC, Eisenberg D, Sherman K, Barlow W, Kaptchuk T, Street J, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001;161:1081–8. doi: 10.1001/archinte.161.8.1081. [DOI] [PubMed] [Google Scholar]
- 11.Preyde M. Effectiveness of massage therapy for subacute low back pain a randomized controlled trial. CMAJ. 2000;162:1815–20. [PMC free article] [PubMed] [Google Scholar]
- 12.Hernandez-Reir M, Field T, Krasnegor J, Theakston H. Lower back pain is reduced and range of motion increased after massage therapy. I J Nurs. 2001;1061:131–45. doi: 10.3109/00207450109149744. [DOI] [PubMed] [Google Scholar]
- 13.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–81. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kremer E, Atkinson JH, Ignelzi RJ. Measurement of pain patient preference does not confound pain measurement. Pain. 1981;10:241–8. doi: 10.1016/0304-3959(81)90199-8. [DOI] [PubMed] [Google Scholar]
- 15.Seymour RA. The use of pain scales in assessing the efficacy of analgesics in post-operative dental pain. Eur J Clin Pharmacol. 1982;23:441–4. doi: 10.1007/BF00605995. [DOI] [PubMed] [Google Scholar]
- 16.Wallenstein SL, Heidrich GI, Kaiko R, RWH Clinical evaluation of mild analgesics the measurement of clinical pain. Br J Clin Pharmacol. 1980;10:319S–27S. doi: 10.1111/j.1365-2125.1980.tb01816.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation theoretical considerations and preliminary results. Gen Hosp Psychiatr. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]