Abstract
OBJECTIVE
This paper describes trends in screening mammography utilization over the past decade and assesses the remaining disparities in mammography use among medically underserved women. We also describe the barriers to mammography and report effective interventions to enhance utilization.
DESIGN
We reviewed medline and other databases as well as relevant bibliographies.
MAIN RESULTS
The United States has dramatically improved its use of screening mammography over the past decade, with increased rates observed in every demographic group. Disparities in screening mammography are decreasing among medically underserved populations but still persist among racial/ethnic minorities and low-income women. Additionally, uninsured women and those with no usual care have the lowest rates of reported mammogram use. However, despite apparent increases in mammogram utilization, there is growing evidence that limitations in the national survey databases lead to overestimations of mammogram use, particularly among low-income racial and ethnic minorities.
CONCLUSIONS
The United States may be farther from its national goals of screening mammography, particularly among underserved women, than current data suggests. We should continue to support those interventions that increase mammography use among the medically underserved by addressing the barriers such as cost, language and acculturation limitations, deficits in knowledge and cultural beliefs, literacy and health system barriers such as insurance and having a source regular of medical care. Addressing disparities in the diagnostic and cancer treatment process should also be a priority in order to affect significant change in health outcomes among the underserved.
Keywords: mammography, health disparities, breast cancer, cancer screening
In 2002, approximately 205,000 women in the United States were diagnosed with breast cancer and 40,000 died of their disease.1 Vulnerable populations such as racial/ethnic minorities, the elderly, and the poor continue to bear a disproportionate burden of breast cancer mortality.1–3 For example, despite an overall lower incidence of disease compared to white women, African-American women suffer higher breast cancer mortality1,2 (Fig. 1) owing to a higher proportion of advanced breast cancer stage.3 A similar pattern of excess late-stage disease is observed in some groups of Hispanic, Native-American, Asian, and low-income women, particularly those who are immigrants or less acculturated, presumably due to less access to screening.4–6
FIGURE 1.
Breast cancer incidence and mortality by race and ethnicity—United States, 1992 to 1998. Data sources: American Cancer Society Surveillance Research 2001, National Cancer Institute SEER Program 2001, National Center for Health Statistics 2001.
To date, women such as Native Americans/Alaskan Natives, Hispanics, women of lower socioeconomic backgrounds and in rural areas, the uninsured and those without a usual source of care, women over age 70, and recent immigrants have not achieved the Healthy People 2010 (HP2010) objective of 70% participation in mammography within the prior 2 years. This HP2010 goal is for all women age 40 and over, regardless of race/ethnicity or social class. Although disparities in screening mammography have improved overall since the early 1990s, significant differences in screening persist among many medically underserved communities.
This paper examines trends in breast cancer screening over the past decade and reports on the remaining disparities in mammography. We discuss the methodological limitations of national databases which have likely overestimated our progress toward the elimination of screening disparities and HP2010 goals. For example, the under-sampling of ethnic minorities (particularly those at high risk for under-screening), collapsing heterogeneous ethnicities into single groups, and the overestimation of preventive services use by minorities have limited the accurate assessment of screening mammography utilization in the U.S.
This paper explores the various barriers to mammography, with special attention to the unique needs of different populations. Despite the heterogeneity of medically underserved women, many of the barriers are common to different populations and reflect limited access to health information and services. We also address interventions to enhance mammography utilization and conclude with a discussion of areas of further research necessary to address disparities in screening mammography.
POPULATIONS WITH DISPARITIES IN SCREENING MAMMOGRAPHY
Low Socioeconomic Status
Low socioeconomic status (SES) is a consistent marker for mammography underuse; women with lower SES are more likely to be uninsured and lack a usual source of care.7–9 Compared to their middle-class and wealthy counterparts, low-income women have the lowest rates of breast cancer screening, even when adjusted for race, ethnicity, and insurance status.9 Although disparities in screening mammography are improving, this group is the furthest from the HP2010 goal of having 70% of women with recent mammogram use; only 50% of uninsured women reported having a mammogram within the prior 2 years, a rate 23.7% lower than that of insured women.10 Women without a usual source of care may be the most at risk for underscreening; only 34.6% of these women reported having a mammogram within the prior 2 years, in comparison to 73.0% of women who had a medical home.11 In 1997, women who did not complete high school had 17.1% lower mammography utilization than those who had some degree of postsecondary education.10 Low-income women had 20.7% lower reports of recent mammography use than those of women living in households with higher incomes.10 The reasons underlying the screening disadvantage associated with low SES are multifactorial and include inadequate cancer prevention knowledge and behaviors, lower educational attainment, and suboptimal health care access.12
Racial/Ethnic Minorities
All racial/ethnic minorities in the U.S. have documented underutilization of preventive health services that reflect sociodemographic variables, cultural barriers, and health systems obstacles. Recent data from the 2000 National Health Interview Survey (NHIS) describes new immigrants as the latest subpopulation of women with low rates of mammography use. Only 39.3% of women living in the U.S. for less than 10 years reported having a mammogram within the prior 2 years, in comparison to 64.7% of women living in the U.S. for 10 years or more and 71.3% of women born in the U.S.11 Immigrants are disproportionately members of racial/ethnic minorities, making these women at particularly high risk for underuse of mammography.
African Americans
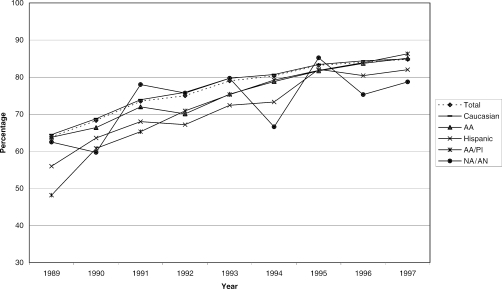
Although earlier studies reported lower breast cancer screening rates among African-American women, recent data from the Behavioral Risk Factor Surveillance Survey (BRFSS) and other databases suggest that mammography use is now comparable to that of white women (Fig. 2).10,13,14 In 1997, 85.1% of surveyed African Americans reported having recent mammograms compared to 84.9% of white women.10 In fact, mammography use is more prevalent among low-income African-American women than low-income white women, even after adjusting for health access and geographic factors. Pooled 1993 to 1994 data from the NHIS reported mammography rates of 60.2% for low-income blacks in comparison to 43.8% for low-income white women.15 However, recent data from the 2000 NHIS does show some residual differential use of mammography, with 67.6% of African-American women reporting mammograms within the prior 2 years compared to 71.2% of white women.11 Additionally, disparities among African Americans are still documented in Medicare and fee-for-service insurance plans, indicating some heterogeneity within this population.15,16
FIGURE 2.
Percentage of women aged > 40 years who reported ever having a mammogram, 38 states—Behavioral Risk Factor Surveillance System, 1989 to 1997.
Hispanics
Hispanic women have narrowed their screening disparity over the past decade from 9.7% to 4.7%, with 67.0% of Hispanic women reporting having had a mammogram within the prior 2 years.10 Not all Hispanic subpopulations have such a high rate of mammography; one recent study reported mammography use among Mexican women to be 10% to 15% lower than that in non-Hispanic whites.17 Other studies have documented the variability within Hispanic subgroups; pooled 1990 and 1992 NHIS data reported mammography rates of 35% among Mexicans, 43% among Puerto Ricans, 41% among Cubans, and 47% among Other Hispanics.18 Regional variations also exist within subpopulations; one study of Mexican Americans reported rates of recent mammography that ranged from nearly 45% among women in Texas to 60% among women living in California.19 Health care access factors, such as insurance status and a usual source of care, account for the bulk of the differences among Hispanic subgroups, but cultural and ethnic factors, such as acculturation and English fluency are also important variables.18–20
Asian Americans/Pacific Islanders
National BRFSS data indicate that Asian Americans/Pacific Islanders (AA/PIs) have closed the screening gap in mammography, with 72.5% of AA/PI women reporting recent mammography compared with 71.4% of white women (Fig. 2).10,21 However, samples of AA/PI women in national surveys are small and frequently aggregated, making conclusions difficult and masking important subgroup differences. State-level and community surveys of AA/PI subpopulations have demonstrated variable mammography utilization, ranging from 30% to 68% of AA/PI women reporting no prior mammogram compared with 10% to 21% of white women.22–25 Among the general AA/PI population, Japanese women appear to have the highest rates of mammography; similar to white women, only 21% have never had a mammogram.25 Particularly low rates of mammography utilization have been documented among groups such as Chinese, Vietnamese, Korean, and Filipino women. For example, among multiethnic women in San Francisco, 73% of Chinese and 46% of Vietnamese women reported prior mammography, compared to 93% of white women.26 The California BRFSS and Korean Health Survey show that subgroups such as Koreans are underscreened, with 45% to 52% of Korean women reporting no previous lifetime mammogram, compared with 10% of the state's general female population.23,27 Low rates of recent mammography use have been demonstrated among Cambodian women (12% to 40%) and Filipino women (55%).28–30 Less is known about Asian-Indian women's screening rates and available data are conflicting; aggregated NHIS data suggest significant underscreening, with 68% of Asian-Indian women reporting no prior mammogram, in contrast to a small study showing that 70% of women had received a mammogram within the past year, a rate higher than those of other Asian subgroups.25,31
Native Americans/Alaskan Natives
Of all racial/ethnic minorities described, American Indians/Alaskan Natives (NA/ANs) have the lowest breast cancer screening and are the only group to increase their screening disparity over the past decade.10,32 In 1997, only 59.9% of these women over age 40 had received a mammogram in the past 2 years, compared to 71.4% of white women,10 and pooled BRFSS data (1992 to 1997) indicate that only 65.1% of those aged 50 and older have had recent mammography.32 According to computerized mammography data from New Mexico, a state with a large NA/AN population, only 37% of Native-American women aged 50 to 74 years received annual mammography, compared to 49% of non-Hispanic white women.17 Despite their heterogeneity, Native-American and Alaskan-Native women are frequently classified into one category when breast cancer and screening data are reported, masking wide variations in outcomes and screening.33 Smaller studies of NA/AN subgroups have found that screening rates vary substantially with tribal affiliation, living situation (reservation vs nonreservation), and geographic location. For example, Hopi women residing on a reservation in Arizona demonstrated recent mammography rates as low as 26.4%, while 67.7% of rural NA/AN women in New Mexico reported a mammogram within the past year.34,35 Audits of Indian Health Service patients and national surveys reinforce this variability, showing lifetime mammography rates ranging from 35% to 81.2% among NA/AN women.34–36
Women Living in Rural Areas
Women residing in rural areas of the US are screened for breast cancer at a significantly lower rate than women in urban areas (66.7% vs 75.4%).37 Many rural regions are characterized by longer distances between medical facilities and less availability of health services, subsequently limiting access to breast cancer screening.38 Since women living in rural areas are more likely to be uninsured, have a low household income, and be less educated, they are at particular risk of preventive care underutilization compared to women in nonrural regions.37 In addition, studies suggest that screening disparities between rural and nonrural populations are more pronounced among minorities. For example, rural ethnic subgroups such as African-American and Native-American women have been found to receive less cancer screening than their nonrural counterparts.39,40
Elderly Women
Although comprising only 13% of the adult US population, women over 65 constitute 44% of new breast cancer diagnoses and 56% of the resultant deaths.41 Despite increased risk and evidence suggesting that mammography's mortality benefits can extend to elderly populations, older women are less likely to be screened.42,43 This is due, in part, to competing risks of death and limited life expectancy; although elderly women have the highest risk of breast cancer, they are actually more likely to die of cardiovascular disease than malignancy.44 Most medical organizations recommend continued screening for women with few comorbid illnesses, yet there is still some controversy within the medical community about screening older women for breast cancer.45
Numerous studies verify that women age 70 and older have lower rates of mammography compared to those between 50 and 69 years of age.10,46 According to the 1997 BRFSS, the percentage of women aged 70 and older who reported having a mammogram within the prior 2 years was 66.7%, compared to 77.1% for women aged 60 to 69 and 78.0% for women aged 50 to 59.10
ASSESSMENT OF SCREENING MAMMOGRAPHY: METHODOLOGIC ISSUES
National estimates of health behaviors among the US adult population are primarily obtained through surveys such as the BRFSS and the NHIS. The BRFSS is a state-based health survey coordinated by the Centers for Disease Control (CDC) and conducted through random telephone interviews of community-dwelling adults aged 18 years and older. The NHIS, also conducted by the CDC, consists of in-person household health surveys. These instruments assess preventive services utilization and monitor progress toward national cancer screening goals.10,11Table 1 presents BRFSS data on reported mammography use within the prior 2 years by various sociodemographic groups;10 because 12 states did not participate in each year of the BRFSS from 1989 to 1997, current trend data includes information from only 38 states.
Table 1.
Percentage*† of Women Aged ≥40 Years Who Reported Having a Mammogram Within the Past 2 Years, 38 States—Behavioral Risk Factor Surveillance Survey (BRFSS), 1989, 1993, 1997
| Characteristic | 1989 % (SD ± 95% CI) | 1993 % (SD ± 95% CI) | 1997 % (SD ± 95% CI) |
|---|---|---|---|
| Annual household | |||
| Income, $ | |||
| <10,000 | 42.1 (3.1) | 51.3 (2.4) | 58.4 (3.2) |
| 10 000 to <25,000 | 50.8 (2.1) | 60.5 (1.6) | 64.1 (1.5) |
| 25 000 to 50,000 | 61.0 (2.7) | 73.3 (1.7) | 74.6 (1.3) |
| >50,000 | 68.0 (4.6) | 80.0 (2.4) | 79.1 (2.2) |
| Education, y | |||
| <12 | 44.1 (2.5) | 53.3 (2.2) | 58.8 (2.2) |
| 12 | 53.0 (1.8) | 65.7 (1.4) | 71.0 (1.1) |
| >12 | 61.5 (1.7) | 73.2 (1.2) | 75.9 (0.9) |
| Health insurance | |||
| Yes | ‡ | 69.4 (0.8) | 73.7 (0.7) |
| No | ‡ | 36.7 (4.2) | 50.0 (3.9) |
| Race | |||
| White | 54.7 (1.1) | 67.0 (0.9) | 71.4 (0.7) |
| African American | 55.7 (3.7) | 65.5 (2.7) | 72.9 (2.2) |
| Asian American or Pacific Islander | 38.8 (7.1) | 66.0 (7.1) | 72.5 (7.2) |
| Native American or Alaska Native | 45.4 (10.9) | 66.7 (8.6) | 59.9 (8.9) |
| Other | 43.3 (10.8) | 60.2 (6.7) | 59.7 (7.6) |
| Ethnicity | |||
| Hispanic | 45.2 (6.2) | 61.4 (4.3) | 67.0 (3.7) |
| Non-Hispanic | 54.9 (1.1) | 67.1 (0.8) | 71.7 (0.7) |
| Mean age, y | |||
| 40–49 | 54.3 (2.1) | 65.9 (1.4) | 65.0 (1.3) |
| 50–59 | 61.3 (2.3) | 71.5 (1.8) | 78.0 (1.4) |
| 60–69 | 55.1 (2.2) | 69.2 (1.7) | 77.1 (1.4) |
| ≥70 | 46.3 (2.1) | 60.2 (1.5) | 66.7 (1.3) |
| Total | 54.3 (1.1) | 66.7 (0.8) | 71.3 (0.7) |
Adjusted to the 1989 BRFSS age distribution for women.
Reflects respondents who answered positively to the question: “A mammogram is an X-ray of each breast to look for breast cancer. Have you ever had a mammogram?” and subsequently answered “Within past 2 years” or “Within the past year” to the question: “How long has it been since you had your last mammogram?”.
Question not asked in 1989.
Despite their widespread use, methodological and sampling limitations may make these instruments unsuited to accurately detect disparities within underserved communities.47–49 For example, these surveys undersample ethnic minorities, particularly those at risk for underscreening. Since persons living in the southern United States, minorities (particularly African Americans, Hispanics, and Native Americans), and those in lower socioeconomic groups are less likely to have telephone coverage, the BRFSS may undersample low-income racial/ethnic minorities who are more likely to have foregone mammography.10,50,51 In addition, the survey questions are generally administered in English and potential respondents who are not English proficient are ineligible for survey completion.52 Recently, some states have utilized bilingual interviewers with translated surveys but this is not standard practice.22,24
Although the BRFSS has surveyed respondents in all US states and 3 territories since 1997, it remains difficult to sample minority and underserved groups. In the 1997 BRFSS, only 11.2% of women surveyed were uninsured. Whites comprised 75.4% of the respondent group in comparison to 9.7% African Americans, 11.1% Hispanics, 1.0% NA/AN, and 2.8% AA/PIs.53 The number of respondents was sufficient (i.e., ≥ 50 respondents) in 51 states for whites, 35 states for African Americans, 36 states for Hispanics, 11 states for NA/ANs, and 10 states for AA/PIs. In addition, the single category of AA/PI or NA/AN masks important differences among ethnic subgroups. When available, targeted BRFSS surveys conducted among Chinese, Korean, and Vietnamese populations in California have demonstrated that each group has distinct sociodemographic characteristics, health behaviors, and preventive services use.22–24 Even when subgroup data are collected, caution must be used in interpreting and generalizing the data. The prevalence reported in a small number of states with larger proportions of certain ethnic minorities may not be representative of the nation for these groups.
Both the BRFSS and NHIS rely on self-reported health behavior, which may not accurately reflect the actual receipt of health services.53–55 BRFSS- and NHIS-reported mammography rates are at least 8.7% higher than claims-based and medical chart-derived rates.54–56 Additionally, there is evidence that low-income ethnic minorities are more likely than whites to over-report rates of screening mammography. In a medical record validation study of women's self-reported mammography, white women had higher accuracy rates (89.3%) compared to those of African Americans, Hispanics, and Asians (66.7% to 75.9%), even after adjustment for source of care and amount of time since the mammogram.57 Thus, self-reported mammography rates may need to be adjusted downward by 25% to 30% for some populations.
BARRIERS TO MAMMOGRAPHY
Attempts to understand disparities in mammography utilization have revealed multiple barriers to equitable health care access and use. Conceptually, patient, provider, health care system, and financial factors must be considered.
Access: Financial & Health System Barriers
Receipt of breast cancer screening is contingent upon gaining adequate access to the health care system. Access factors, such as insurance status, income, and usual source of care, are the largest contributors to racial/ethnic screening differences in mammography rates.20 Women without a usual source of care are half as likely to report having had a mammogram, and low-income women report cost as a significant barrier to obtaining a mammogram.58,59 Despite the availability of free mammograms to the uninsured, women without insurance remain one of the most underscreened groups, indicating that expanding insurance coverage to this population may be a more effective strategy than targeted mammography interventions.
Once women gain access to the health care system, the clinical encounter also affects subsequent mammography utilization. Physician recommendation is one of the strongest predictors of breast cancer screening and is particularly influential for women with continuity care providers.60–62 Older women who perceived provider enthusiasm in their discussion of mammography were 4 times more likely to have had recent mammography.63 Unfortunately, individual provider's prescription of health services is not uniform; racial/ethnic minorities, the elderly, and low-income women are less likely to receive physician recommendations for mammography.64,65 Further work needs to elucidate the causes of this variability in physician recommendation, but potential factors include poor communication, provider assumptions about patient age and financial resources, and discrimination.66,67
Patient Knowledge, Attitudes, Cultural Beliefs
Patient-associated barriers to screening mammography include inadequate cancer knowledge, attitudes, and cultural beliefs. Studies demonstrate that these barriers vary by race/ethnicity, age, and socioeconomic status.68 Vulnerable groups such as the poor, elderly, and minorities often lack awareness of mammography, have misconceptions regarding cancer, and view mammography negatively.68–70 Cultural norms of modesty, fatalistic attitudes about cancer, and fear of finding malignancy are reported barriers among racial/ethnic populations.71–73 Historical discrimination has led to cultural guidelines among some racial/ethnic populations that emphasize caution, mistrust, and avoidance when interacting with health care institutions.74
Language and Acculturation
Within immigrant populations, inadequate English proficiency poses a tremendous barrier to preventive services, as individuals may be unable to navigate the health care system or communicate effectively with providers.75,76 Several studies report lower rates of screening mammography among Spanish-speaking Hispanic patients as compared to English-proficient Hispanics and non-Hispanics.76,77 Some investigators have concluded that although English fluency is a component of acculturation, its strong association with preventive service use independent of cultural attitudes and values indicates that it is a proxy for health care access.78,79 Acculturation can be measured by English proficiency, country of birth, education, and the number of years in the US, and is linked to lower preventive and primary care services utilization.80,81
Literacy
Literacy is a barrier to mammography distinct from language proficiency that affects all racial/ethnic and age groups.82 Low literacy impacts a woman's ability to access written cancer screening materials, benefit from instruction during the clinical encounter, and apply for health insurance to obtain preventive screening.82–84 Lower reading ability is associated with inadequate breast cancer screening knowledge and correlates with negative attitudes toward mammography; low-literate women are more likely to view the process as embarrassing, harmful, or painful.82 Recent research highlights illiteracy as an independent contributor to cancer disparities, as it is more prevalent among low-income, elderly, and racial/ethnic minority women.81,83,84
INTERVENTIONS TO IMPROVE MAMMOGRAPHY UTILIZATION
Over the past decade, the federal government has launched several initiatives to decrease disparities in breast cancer screening among medically underserved women. In 1987, the National Cancer Institute created the Special Populations Studies Branch of the Division of Cancer Prevention and Control to support cancer control activities in racial and ethnic communities.85 In 1990, the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) was instituted to improve medically underserved populations’ access to screening mammography.86 Enacted at the state and local levels, these initiatives have been largely responsible for increasing mammography use among vulnerable populations.87 In addition, numerous health care facilities and communities have implemented programs designed to improve mammography utilization for minority and disadvantaged women.
Although systematic evaluation of mammography-enhancing interventions is difficult due to the diversity of populations in different studies and heterogeneity of interventions and study designs, available meta-analyses have reported significant increases in screening from targeted interventions. The estimated intervention effect was greatest for older women (17.9%), followed by groups consisting of > 40% low income women (12.7%), and groups consisting of > 40% nonwhites (12.0%).88
Patient-Targeted Interventions
Individual-directed Interventions.
A recent meta-analysis of interventions that targeted patients through tailored and untailored letters/reminders, in-person counseling, and telephone counseling concluded that individual-directed interventions in health care settings were successful in increasing mammography use by 17.6% while those in community settings were somewhat less effective (6.8%).88 For underserved populations, programs that used tailored, theory-based messages in an interactive format such as individualized letters, in-person, or telephone counseling were significantly more effective at increasing mammography rates (10.7% to 19.9%) compared to nontailored interventions such as pamphlets and generic letters (2.7% to 3.5%).89,90
Access-enhancing Interventions.
The most effective patient-targeted strategies to increase mammography use are access-enhancing interventions, which have been shown to increase rates by 19%.88 The success of interventions that address the structural, economic, and geographic barriers to mammography, such as mobile vans, transportation services, and reduced cost mammograms, underscores the importance of health care access in addressing health disparities. For example, mobile mammography can reduce the geographic barriers for rural women, migrant farm workers, Native Americans, and underserved urban women.91,92 They provide mammography in nonthreatening settings such as churches and community centers, and can reach women who may be reluctant to navigate complex health care systems.91,92 Similarly, translation services, facilitated scheduling, and patient navigators assist women with the logistical barriers to mammography.93 Providing free or low-cost mammography is a particularly effective strategy and has been shown to increase mammography use by 45% in low-income populations.86,94
Community Education/Mass Media.
Although attempts to increase mammography uptake through community education and mass media campaigns have variable penetrance into their intended audience, they have the potential to reach substantial numbers of women and are cost-effective if the community has a significant proportion of women at risk for underscreening.95–97 Public education efforts may be particularly instrumental in low-income ethnic communities because women of low socioeconomic status, with low literacy levels or limited English proficiency are more likely to receive their health information from television or radio than from print media or traditional health sources.98 Effect sizes for community education and media interventions range from 5.9% to 9.7%.88
Social Networks.
Sociological interventions that rely on social networks to mediate behavioral change have also successfully increased mammography rates from 9.7% to 22.0%.90,93 Social ties have been shown to influence health behaviors in African-American and Latino women99–101 and to be predictors for older African-American women accepting physician recommendations, making appointments, and obtaining mammograms.102,103 In a context where racial/ethnic minorities interact less frequently with formal health services and often distrust the health care system, community health educators can overcome the social, cultural, and linguistic barriers to mammography.104,105 They have been effective in African-American, Latino, Native-American, and Asian communities, as well as among older women and those living in rural areas.106–109
System/Provider-Directed Interventions
Researchers have identified structural flaws in our health care delivery system that may account for many of the observed health disparities.110 Currently, the largest discrepancy in breast cancer screening remains among the uninsured and those without a usual source of care.10,12 Targeted programs such as the NBCCEDP have successfully opened access for uninsured and underserved women by providing free breast cancer screening and follow-up diagnostic procedures.86 Studies have also documented that mammography screening is influenced by the type of health care delivery; health plans that emphasize preventive services, such as health maintenance organizations, have higher screening mammography rates and fewer racial/ethnic disparities.111–115 A national health plan with a coordinated system of preventive and primary health care services could potentially eliminate the current disparity based on health insurance, which disproportionately affects racial and ethnic minorities.
Physician recommendation is one of the strongest predictors of mammography use; efforts to change mammography prescribing behaviors have increased screening among underserved populations. Interventions include strategies to change provider behavior (reminder systems/office prompts), cognitive interventions to influence provider attitudes toward screening (chart audits with feedback, educational sessions/materials), and indirect methods that create screening opportunities independent of provider behavior (clinic reorganization, nurse-instituted protocols).116,117 A meta-analysis of provider-targeted strategies determined that all these types of interventions to change provider behavior were effective and increased mammography use from 6% to 21%.116 In addition, office system prompts were the most successful strategy to change provider behavior; recent research shows computer-based reminders to be more effective prompts than chart-based checklists or nurse-initiated reminders.117–119
Multiple Strategies
Because underserved communities frequently have numerous barriers to breast cancer screening, the most effective programs have incorporated multiple strategies, such as those that combine access-enhancing interventions with individual-directed interventions (26.9%), or programs that combine access-enhancing interventions with system-directed interventions (19.4%).88 Caution should be used in interpreting these results, however, because the number of available studies was small.
CONCLUSIONS
Although disparities in screening mammography have improved over the past decade, documented differences persist among women of lower socioeconomic backgrounds, the uninsured, women without a usual source of care, the elderly, recent immigrants, women in rural areas, and some racial/ethnic minorities such as NA/ANs and Hispanics. There is evidence that the actual magnitude of these disparities, particularly among low-income racial/ethnic minorities, is underestimated and that disparities persist for some subpopulations of AA/PIs and African Americans. While current population-based surveys may not accurately assess disparities in screening mammography, there are also limitations to claims-based and chart review methods of data collection. Claims-based data does not capture the experience of uninsured women, and chart reviews are subject to manual documentation errors. New methodologies are needed to more precisely determine preventive care utilization in the US, particularly within medically underserved populations.
The most significant disparities in screening mammography are based on insurance status, usual source of care, and socioeconomic status. Consequently, access-enhancing strategies, which are the most effective type of patient-targeted intervention, will continue to be important complements to programs that mediate individual change. Health care systems change, such as the implementation of a national health plan, will be vital to eliminating disparities among the uninsured and those with limited access to health care.
While meta-analyses have reported increased mammography utilization from a wide range of interventions, the overall effectiveness of such strategies may be overestimated because negative studies are less likely to be published. Although generally viewed as successful, these interventions have not reached full penetrance within all underserved communities. Continuing national and local initiatives to reach at-risk women must continue to be funded and systematically evaluated for effectiveness. We should not, however, endeavor to reach 100% utilization of screening mammography among the elderly, as a substantial number of these women will have significant comorbid illnesses that make the risks of screening outweigh the benefits. Additionally, initiatives should emphasize the importance of rescreening medically underserved women, as data indicate that more women report having been screened in the past than report recent mammogram use.10
Future research in breast cancer screening disparities is warranted in several key areas. First, more work is needed to collect accurate national screening estimates of NA/AN, AA/PI, and Hispanic subpopulations and to understand the heterogeneity within these groups that affects mammography use, such as regional variation, cultural differences, English proficiency, and sociodemographic factors. Second, there is little current data examining the long-term effectiveness of mammography-enhancing interventions. Finally, the effectiveness of different types and/or combinations of interventions in specific patient subpopulations is not well known, hampering our ability to assess cost effectiveness and make health policy decisions.
Efforts to decrease disparities in screening mammography are successful only if they result in reduced breast cancer morbidity and mortality. Despite improvements in screening rates, it is concerning that disparities in breast cancer mortality persist among underserved populations such as African Americans, Hispanics, Native Americans, Vietnamese, and Native Hawaiians.120,121 Because changes in disease outcomes lag behind public health interventions, it is possible that we have yet to witness the benefits of enhanced screening in specific underserved groups. More likely, however, screening mammography is only one of several factors impacting disparities in breast cancer mortality. Decreasing disparities in the diagnostic and cancer treatment process must also become a priority if we are to reduce mortality differentials in breast cancer.
Acknowledgments
We gratefully acknowledge Dr. Avery Hart for his generous assistance in preparing and revising this manuscript.
REFERENCES
- 1.SEER Cancer Statistics. Available at: http://seer.cancer.gov. Accessed January 10, 2003.
- 2.Chevarley F, White E. Recent trends in breast cancer mortality among white and black US women. Am J Public Health. 1997;87:775–81. doi: 10.2105/ajph.87.5.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eley JW, Hill HA, Chen VW, et al. Racial differences in survival from breast cancer: results of the National Cancer Institute Black/White cancer survival study. JAMA. 1994;272:947–54. doi: 10.1001/jama.272.12.947. [DOI] [PubMed] [Google Scholar]
- 4.Hedeen AN, White E. Breast cancer size and stage in Hispanic American women, by birthplace: 1992–95. Am J Public Health. 2001;91:122–5. doi: 10.2105/ajph.91.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA. 1998;279:1801–7. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- 6.Randolph WM, Goodwin JS, Mahnken JD, Freeman JL. Regular mammography use is associated with elimination of age-related disparities in size and stage of breast cancer at diagnosis. Ann Intern Med. 2002;137:783–90. doi: 10.7326/0003-4819-137-10-200211190-00006. [DOI] [PubMed] [Google Scholar]
- 7.Anonymous. Self-reported use of mammography and insurance status among women aged greater than or equal to 40 years—United States, 1991–92 and 1996–97. Morb Mortal Wkly Rep. 1998;47:825–30. [PubMed] [Google Scholar]
- 8.Robert Wood Johnson Foundation Special Report. Access to health care in the United States: results of a 1986 survey. 1987. pp. 1–11.
- 9.Katz SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite universal coverage: breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272:530–4. [PubMed] [Google Scholar]
- 10.Blackman DK, Bennett EM, Miller DS. Trends in self-reported use of mammograms (1989–97) and papanicolaou tests 1991–97—Behavioral Risk Factor Surveillance System. Morb Mortal Wkly Rep. 1999;48:1–22. [PubMed] [Google Scholar]
- 11.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States. Results from the 2000 National Health Interview Study. Cancer. 2003;97:1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 12.Hedegaard HB, Davidson AJ, Wright RA. Factors associated with screening mammography in low-income women. Am J Prev Med. 1996;12:51–6. [PubMed] [Google Scholar]
- 13.Blustein J. Medicare coverage, supplemental insurance, and the use of mammography by older women. N Engl J Med. 1995;332:1138–43. doi: 10.1056/NEJM199504273321706. [DOI] [PubMed] [Google Scholar]
- 14.Burns RB, McCarthy EP, Freund KM, et al. Black women receive less mammography even with similar use of primary care. Ann Intern Med. 1996;125:173–82. doi: 10.7326/0003-4819-125-3-199608010-00002. [DOI] [PubMed] [Google Scholar]
- 15.Makuc DM, Breen N, Freid V. Low income, race, and the use of mammography. Health Serv Res. 1999;34:229–39. [PMC free article] [PubMed] [Google Scholar]
- 16.Corbie-Smith G, Flagg EW, Doyle JP, O'Brien MA. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002;17:458–64. doi: 10.1046/j.1525-1497.2002.10733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilliland FD, Rosenberg RD, Hunt WC, et al. Patterns of mammography use among Hispanic, American Indian, and Non-Hispanic white women in New Mexico, 1994–97. Am J Epidemiol. 2000;152:432–7. doi: 10.1093/aje/152.5.432. [DOI] [PubMed] [Google Scholar]
- 18.Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed ML. Use of cancer screening practices by Hispanic women: analyses by subgroup. Prev Med. 1999;29:466–77. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- 19.Ramirez AG, Talavera GA, Villareal R, et al. Breast cancer screening in regional Hispanic populations. Health Educ Res. 2000;15:559–68. doi: 10.1093/her/15.5.559. [DOI] [PubMed] [Google Scholar]
- 20.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Coughlin SS, Uhler RJ. Breast and cervical cancer screening practices among Asian and Pacific Islander women in the United States, 1994–97. Cancer Epidemiol Biomarkers Prev. 2000;9:597–603. [PubMed] [Google Scholar]
- 22.Anonymous. Behavioral Risk Factor Survey of Chinese— California, 1989. Morb Mortal Wkly Rep. 1992;41:266–70. [PubMed] [Google Scholar]
- 23.Anonymous. Behavioral Risk Factor Survey of Korean Americans—Alameda County California, 1994. Morb Mortal Wkly Rep. 1997;46:774–7. [PubMed] [Google Scholar]
- 24.Anonymous. Behavioral Risk Factor Survey of Vietnamese—California, 1991. Morb Mortal Wkly Rep. 1992;41:69–72. [PubMed] [Google Scholar]
- 25.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and Healthy People 2000 Objectives. Cancer. 2000;89:696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 26.Hiatt R, Pasick R, Perez-Stable E, et al. Pathways to early cancer detection in the multiethnic population of the San Francisco Bay Area. Health Educ Q. 1996;23(suppl):S10–S27. [Google Scholar]
- 27.Wismer BA, Moskowitz JM, Chen AM, et al. Mammography and clinical breast examination among Korean American women in two California counties. Prev Med. 1998;27:144–51. doi: 10.1006/pmed.1997.0259. [DOI] [PubMed] [Google Scholar]
- 28.Kelly AW, Chacori MD, Wollan PC, et al. A program to increase breast and cervical cancer screening for Cambodian women in a Midwestern community. Mayo Clin Proc. 1996;71:437–44. doi: 10.4065/71.5.437. [DOI] [PubMed] [Google Scholar]
- 29.Tu SP, Yasui Y, Kuniyuki A, et al. Breast cancer screening among Cambodian American women. Cancer Detect Prev. 2000;24:549–63. [PubMed] [Google Scholar]
- 30.Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000;18:62–8. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- 31.Sadler GR, Dhanjal SK, Shah NB, et al. Asian Indian women: knowledge, attitudes and behaviors toward breast cancer early detection. Public Health Nurs. 2001;18:357–63. doi: 10.1046/j.1525-1446.2001.00357.x. [DOI] [PubMed] [Google Scholar]
- 32.Coughlin SS, Uhler RJ, Blackman DK. Breast and cervical cancer screening practices among American Indian and Alaska Native women in the United States, 1992–97. Prev Med. 1999;29:287–95. doi: 10.1006/pmed.1999.0537. [DOI] [PubMed] [Google Scholar]
- 33.Cobb N, Paisano RE. Patterns of cancer mortality among Native Americans. Cancer. 1998;83:2377–83. doi: 10.1002/(sici)1097-0142(19981201)83:11<2377::aid-cncr18>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 34.Gilliland FD, Mahler R, Hunt WC, Davis SM. Preventive health care among rural American Indians in New Mexico. Prev Med. 1999;28:194–202. doi: 10.1006/pmed.1998.0401. [DOI] [PubMed] [Google Scholar]
- 35.Giuliano A, Papenfuss M, Guernsey de Zapien J, Tilousi S, Nuvayestewa L. Breast cancer screening among Southwest American Indian women living on-reservation. Prev Med. 1998;27:135–43. doi: 10.1006/pmed.1997.0258. [DOI] [PubMed] [Google Scholar]
- 36.Strauss KF, Mokdad A, Ballew C, et al. The health of Navajo women: findings from the Navajo Health and Nutrition Survey, 1991–92. J Nutr. 1997;127(suppl):2128S–2133S. doi: 10.1093/jn/127.10.2128S. [DOI] [PubMed] [Google Scholar]
- 37.Coughlin SS, Thompson TD, Hall HI, Logan P, Uhler RJ. Breast and cervical carcinoma screening practices among women in rural and nonrural areas of the United States, 1998–99. Cancer. 2002;94:2801–12. doi: 10.1002/cncr.10577. [DOI] [PubMed] [Google Scholar]
- 38.Kreher NE, Hinkner JM, Rufin MT, Lin CH. Effect of distance and travel time on rural women's compliance with screening mammography: the UPRNet study. J Fam Pract. 1995;40:143–7. [PubMed] [Google Scholar]
- 39.O'Malley MS, Earp JL, Harris RP. Race and mammography use in two North Carolina counties. Am J Public Health. 1997;87:782–6. doi: 10.2105/ajph.87.5.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hall HI, Uhler RJ, Coughlin SS, Miller DS. Breast and cervical cancer screening among Appalachian women. Cancer Epidemiol Biomarkers Prev. 2002;11:137–42. [PubMed] [Google Scholar]
- 41.Cancer Statistics Review 1973–1987. SEER Program. Bethesda, Md: US Dept. of Health and Human Services, PHS, NIH, NCI; NIH Publication no. 90–2789. [Google Scholar]
- 42.Smith-Bindman R, Kerlikowske K, Gebretsadik T, Newman J. Is screening mammography effective in elderly women? Am J Med. 2000;108:112–9. doi: 10.1016/s0002-9343(99)00406-4. [DOI] [PubMed] [Google Scholar]
- 43.Randolph WM, Goodwin JS, Mahnken JD, Freeman JL. Regular mammography use is associated with elimination of age-related disparities in size and stage of breast cancer at diagnosis. Ann Intern Med. 2002;137:783–90. doi: 10.7326/0003-4819-137-10-200211190-00006. [DOI] [PubMed] [Google Scholar]
- 44.Satariano WA, Ragland DR. The effect of comorbidity on 3-year survival of women with primary breast cancer. Ann Intern Med. 1994;120:104–10. doi: 10.7326/0003-4819-120-2-199401150-00002. [DOI] [PubMed] [Google Scholar]
- 45.Walter LC, Eng C, Covinsky KE. Screening mammography for frail older women. What are the burdens? J Gen Intern Med. 2001;16:779–84. doi: 10.1111/j.1525-1497.2001.10113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith RA, D’Orsi CJ. Broast imaging and image-guided biopsy techniques. In: Harris JR, editor. Screening for Breast Cancer. Diseases of the Breast. 2nd edn. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 47.Hiatt RA, Perez-Stable EJ, Quesenberry C, Jr, Sabogal F, Otero-Sabogal R, McPhee SJ. Agreement between self-reported early cancer detection practices and medical audits among Hispanic and non-Hispanic white health plan members in Northern California. Prev Med. 1995;24:278–85. doi: 10.1006/pmed.1995.1045. [DOI] [PubMed] [Google Scholar]
- 48.Johnson CS, Archer J, Campos-Outcalt D. Accuracy of Pap smear and mammogram self-reports in a Southwestern Native American tribe. Am J Prev Med. 1995;11:360–3. [PubMed] [Google Scholar]
- 49.Champion VL, Menon U, McQuillen DH, Scott C. Validity of self-reported mammography in low-income African American women. Am J Prev Med. 1998;14:111–7. doi: 10.1016/s0749-3797(97)00021-4. [DOI] [PubMed] [Google Scholar]
- 50.Bureau of the Census. Phoneless in America. Statistical Brief 94–16, July 1994. US Department of Commerce, Bureau of the Census.
- 51.BRFSS Survey Protocol Site. Available at: http://www2.cdc.gov/nccdphp/brfss2/training_gu/dispositions.asp. Accessed September 8, 2003.
- 52.Baquet CR. Native Americans’ cancer rates in comparison with other peoples of color. Cancer. 1996;78:1538–44. [PubMed] [Google Scholar]
- 53.Bolen JC, Rhodes L, Powell-Griner EE, et al. State-specific prevalence of selected health behaviors, by race and ethnicity—Behavioral Risk Factor Surveillance System, 1997. CDC Surveillance Summaries, Morb Mortal Wkly Rep. 2000;49:1–60. [PubMed] [Google Scholar]
- 54.Thompson BL, O'Connor P, Boyle R, et al. Measuring clinical performance: comparison and validity of telephone survey and administrative data. Health Serv Res. 2001;36:813–25. [PMC free article] [PubMed] [Google Scholar]
- 55.Lawrence VA, De Moor C, Glenn ME. Systematic differences in validity of self-reported mammography behavior: a problem for intergroup comparisons? Prev Med. 1999;29:575–80. doi: 10.1006/pmed.1999.0575. [DOI] [PubMed] [Google Scholar]
- 56.Bloom SA, Harris JR, Thompson BL, Ahmed F, Thompson J. Tracking clinical preventive service use: a comparison of the Health Plan Employer Data and Information Set with the Behavioral Risk Factor Surveillance System. Med Care. 2000;3:187–94. doi: 10.1097/00005650-200002000-00008. [DOI] [PubMed] [Google Scholar]
- 57.McPhee SJ, Nguyen TT, Shema SJ, et al. Validation of recall of breast and cervical cancer screening by women in an ethnically diverse population. Prev Med. 2002;35:463–73. doi: 10.1006/pmed.2002.1096. [DOI] [PubMed] [Google Scholar]
- 58.O'Malley AS, Mandelblatt J, Gold K, Cagney KA, Kerner J. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997;157:1462–70. [PubMed] [Google Scholar]
- 59.Kiefe CI, McKay SV, Halevy A, Brody BA. Is cost a barrier to screening mammography for low-income women receiving Medicare benefits? A randomized trial. Arch Intern Med. 1994;154:1217–24. [PubMed] [Google Scholar]
- 60.O'Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations: the roles of primary care, health insurance, and HMOs. J Gen Intern Med. 2002;17:144–54. doi: 10.1046/j.1525-1497.2002.10431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996;86:1748–54. doi: 10.2105/ajph.86.12.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O'Malley AS, Mandelblatt J, Gold K, Cagney KA, Kerner J. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997;157:1462–70. [PubMed] [Google Scholar]
- 63.Fox SA, Siu AL, Stein JA. The importance of physician communication on breast cancer screening of older women. Arch Intern Med. 1994;154:2058–68. [PubMed] [Google Scholar]
- 64.Schulman K, Berlin J, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 65.Grady KE, Lemkau JP, McVay JM, et al. Clinical decision-making and mammography referral. Prev Med. 1996;25:327–38. doi: 10.1006/pmed.1996.0063. [DOI] [PubMed] [Google Scholar]
- 66.Williams RL, Flocke SA, Stange KC. Race and preventive services delivery among black patients and white patients seen in primary care. Med Care. 2001;39:1260–7. doi: 10.1097/00005650-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 67.Smith RA, Haynes S. Barriers to screening for breast cancer. Cancer. 1992;69:1968–78. doi: 10.1002/1097-0142(19920401)69:7+<1968::aid-cncr2820691718>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 68.Loehrer PJ, Greger HA, Weinberger M, et al. Knowledge and beliefs about cancer in a socioeconomically disadvantaged population. Cancer. 1991;68:1665–71. doi: 10.1002/1097-0142(19911001)68:7<1665::aid-cncr2820680734>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 69.Pham CT, McPhee SJ. Knowledge, attitudes, and practices of breast and cervical cancer screening among Vietnamese women. J Cancer Educ. 1992;7:305–10. doi: 10.1080/08858199209528187. [DOI] [PubMed] [Google Scholar]
- 70.Perez-Stable EJ, Sabogal F, Otero-Sabogal R, et al. Misconceptions about cancer among Latinos and Anglos. JAMA. 1992;268:3219–23. doi: 10.1001/jama.1992.03490220063029. [DOI] [PubMed] [Google Scholar]
- 71.Kagawa-Singer M. Addressing issues for early detection and screening in ethnic populations. Oncol Nurs Forum. 1997;24:1705–11. [PubMed] [Google Scholar]
- 72.Lawson EJ. A narrative analysis: a Black woman's perceptions of breast cancer risks and early breast cancer detection. Cancer Nursing. 1998;21:421–9. doi: 10.1097/00002820-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 73.Phillips JM, Cohen MZ, Moses G. Breast cancer screening and African American women: fear, fatalism, and silence. Oncol Nurs Forum. 1999;26:561–71. [PubMed] [Google Scholar]
- 74.Glanz K. Cancer in Women of Color Monograph. Cancer in African American Women. DHHS, NCI; January 2003. Available at: http://cancercontrol.cancer.gov/womenofcolor/. Accessed September 10, 2003. [Google Scholar]
- 75.Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language a barrier to the use of preventive services? J Gen Intern Med. 1997;12:472–7. doi: 10.1046/j.1525-1497.1997.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 77.Perez-Stable EJ, Sabogal F, Otero-Sabogal R. Use of cancer-screening tests in the San Francisco bay area: comparison of Latinos and Anglos. J Natl Cancer Inst. 1995;18:147–53. [PubMed] [Google Scholar]
- 78.Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. Am J Public Health. 1990;80(suppl):11–9. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Suarez L. Pap smear and mammogram screening in Mexican-American women. The effects of acculturation. Am J Public Health. 1994;84:742–6. doi: 10.2105/ajph.84.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Coe K, Harmon MP, Castro FG, et al. Breast self-examination: knowledge and practices of Hispanic women in two southwestern metropolitan areas. J Community Health. 1994;19:433–8. doi: 10.1007/BF02260325. [DOI] [PubMed] [Google Scholar]
- 81.Williams MV, Parker RM, Baker DW, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–82. [PubMed] [Google Scholar]
- 82.Davis TC, Arnold C, Berkel HJ, Nandy I, Jackson RH, Glass J. Knowledge and attitude on screening mammography among low-literate, low-income women. Cancer. 1996;78:1677–82. doi: 10.1002/(sici)1097-0142(19961101)78:9<1912::aid-cncr11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 83.Davis TC, Williams MV, Marin E, Parker R, Glass J. Health literacy and cancer communication. CA Cancer J Clin. 2002;52:134–49. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- 84.Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health literacy: report of the Council on Scientific Affairs. JAMA. 1999;281:552–7. [PubMed] [Google Scholar]
- 85.Burhansstipanov L. National Cancer Institute's Native American Cancer Research Projects. Alaska Med. 1993;35:248–54. [PubMed] [Google Scholar]
- 86.May DS, Lee NC, Nadel MR, Henson RM, Miller DS. The National Breast and Cervical Cancer Early Detection Program: report on the first 4 years of mammography provided to medically underserved women. Am J Roentgenol. 1998;170:97–104. doi: 10.2214/ajr.170.1.9423608. [DOI] [PubMed] [Google Scholar]
- 87.Henson RM, Wyatt SW, Lee NC. The National Breast and Cervical Early Detection Program: a comprehensive public health response to two major health issues for women. J Public Health Manag Pract. 1996;2:36–47. [PubMed] [Google Scholar]
- 88.Legler J, Meissner HI, Coyne C, et al. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11:59–71. [PubMed] [Google Scholar]
- 89.Skinner CS, Strecher VJ, Hospers H. Physicians’ recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–9. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yarbroff KR, O'Malley A, Mangan P, Mandelblatt J. Inreach and outreach interventions to improve mammography use. JAMA. 2001;56:166–73. [PubMed] [Google Scholar]
- 91.Zavertnik JJ, McCoy CB, Robinson DS, Love N. Cost-effective management of breast cancer. Cancer. 1992;69:1979–84. doi: 10.1002/1097-0142(19920401)69:7+<1979::aid-cncr2820691719>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 92.Flynn BS, Gavin P, Worden JK, Ashikaga T, Gautam S, Carpenter J. Community education programs to promote mammography participation in rural New York state. Prev Med. 1997;26:102–8. doi: 10.1006/pmed.1997.0110. [DOI] [PubMed] [Google Scholar]
- 93.Yabroff KR, Mandelblatt JS. Interventions targeted toward patients to increase mammography use. Cancer Epidemiol Biomarkers Prev. 1999;8:749–57. [PubMed] [Google Scholar]
- 94.Skaer TL, Robison LM, Sclar DA, Harding GH. Financial incentive and the use of mammography among Hispanic migrants to the United States. Health Care Women Int. 1996;17:281–91. doi: 10.1080/07399339609516245. [DOI] [PubMed] [Google Scholar]
- 95.Suarez L, Nichols DC, Brady CA. Use of peer role models to increase Pap smear and mammogram screening in Mexican-American and black women. Am J Prev Med. 1993;9:290–6. [PubMed] [Google Scholar]
- 96.Mayer JA, Kossman MK, Miller LC, Crooks CE, Slymen DJ, Lee CD. Evaluation of a media-based mammography program. Am J Prev Med. 1992;8:23–9. [PubMed] [Google Scholar]
- 97.Anonymous. Dramatic print ads raise awareness. NorthEast Medical Center's breast health campaign. Profiles Healthc Mark. 2002;18:15–9. [PubMed] [Google Scholar]
- 98.Breen N, Kessler LG, Brown ML. Breast cancer control among the underserved—an overview. Breast Cancer Res Treat. 1996;40:105–15. doi: 10.1007/BF01806006. [DOI] [PubMed] [Google Scholar]
- 99.Husaini B, Castor R, Linn J, Moore S, Warren H, Whitten-Stovall R. Social support and depression among the black and white elderly. J Community Psychol. 1990;18:12–8. [Google Scholar]
- 100.Husaini B, Moor S, Castor R, et al. Social density, stressors, and depression: gender differences among the black elderly. J Gerontol. 1991;46:236–42. doi: 10.1093/geronj/46.5.p236. [DOI] [PubMed] [Google Scholar]
- 101.Gibson RC, Jackson JS. The health, physical functioning, and informal supports of the black elderly. Milbank Q. 1987;65:421–55. [PubMed] [Google Scholar]
- 102.Kang SH, Bloom JR, Romano PS. Cancer screening among African-American women: their use of tests and social support. Am J Public Health. 1994;84:101–3. doi: 10.2105/ajph.84.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kang SH, Bloom JR. Social support and cancer screening among older Black Americans. J Natl Cancer Inst. 1993;85:737–42. doi: 10.1093/jnci/85.9.737. [DOI] [PubMed] [Google Scholar]
- 104.Weber BE, Reilly BM. Enhancing mammography use in the inner city. Arch Intern Med. 1997;157:2345–9. [PubMed] [Google Scholar]
- 105.Brownstein JN, Cheal N, Ackerman SP, Bassford TL, Campos-Outcalt D. Breast and cervical cancer screening in minority populations: a model for using lay health educators. J Cancer Educ. 1992;7:321–6. doi: 10.1080/08858199209528189. [DOI] [PubMed] [Google Scholar]
- 106.Gotay CC, Banner RO, Matsunaga DS, et al. Impact of a culturally appropriate intervention on breast and cervical screening among Native Hawaiian women. Prev Med. 2000;31:529–37. doi: 10.1006/pmed.2000.0732. [DOI] [PubMed] [Google Scholar]
- 107.Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por la vida model intervention enhances use of cancer screening tests among Latinas. Am J Prev Med. 1998;15:32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- 108.Skinner CS, Sykes RK, Monsees BS, Adriole DA, Arfken CL, Fisher EB. Learn, share and live: breast cancer education for older, urban minority women. Health Educ Behav. 1998;25:60–78. doi: 10.1177/109019819802500106. [DOI] [PubMed] [Google Scholar]
- 109.Anderson MR, Yasui Y, Meischke H, Kuniyuki A, Etzioni R, Urban N. The effectiveness of mammography promotion by volunteers in rural communities. Am J Prev Med. 2000;18:199–207. doi: 10.1016/s0749-3797(99)00161-0. [DOI] [PubMed] [Google Scholar]
- 110.Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Available at: http://www.nap.edu. Accessed January 15, 2003.
- 111.Gordon NP, Rundall TG, Parker L. Type of health care coverage and the likelihood of being screened for cancer. Med Care. 1998;36:636–45. doi: 10.1097/00005650-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 112.Makuc DM, Fried VM, Parsons PE. Health insurance and cancer screening among women. Adv Data. 1994;254:1–12. [PubMed] [Google Scholar]
- 113.Reisch LM, Barton MB, Fletcher SW, Kreuter W, Elmore JG. Breast cancer screening use by African Americans and whites in an HMO. J Gen Intern Med. 2000;15:229–34. doi: 10.1111/j.1525-1497.2000.01339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.DeLaet DE, Shea S, Olveen C. Receipt of preventive services among privately insured minorities in managed care versus fee-for-service insurance plans. J Gen Intern Med. 2002;17:451–7. doi: 10.1046/j.1525-1497.2002.10512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Haas JS, Phillips KA, Sonneborn DMA, McCulloch CE, Liang S. Effect of managed care insurance on the use of preventive care for specific ethnic groups in the United States. Med Care. 2002;40:743–51. doi: 10.1097/00005650-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 116.Mandelblatt JS, Yabroff KR. Effectiveness of interventions designed to increase mammography use: a meta-analysis of provider-targeted strategies. Cancer Epidemiol Biomarkers Prev. 1999;8:759–67. [PubMed] [Google Scholar]
- 117.Tierney WM, Hui SL, McDonald CJ. Delayed feedback of physician performance versus immediate reminders to perform preventive care. Med Care. 1986;24:659–66. doi: 10.1097/00005650-198608000-00001. [DOI] [PubMed] [Google Scholar]
- 118.Cheney C, Ramsdell JW. Effect of medical records’ checklists on implementation of periodic health measures. Am J Med. 1987;83:129–36. doi: 10.1016/0002-9343(87)90507-9. [DOI] [PubMed] [Google Scholar]
- 119.Davidson RA, Fletcher SW, Retchin S, Duh S. A nurse-initiated reminder system for the periodic health examination. Implementation and evaluation. Arch Intern Med. 1984;144:2167–70. [PubMed] [Google Scholar]
- 120.Clegg LX, Li FP, Hankey BF, Chu K, Edwards BK. Cancer survival among US whites and minorities. Arch Intern Med. 2002;162:1985–93. doi: 10.1001/archinte.162.17.1985. [DOI] [PubMed] [Google Scholar]
- 121.Li CI, Malone KE, Daling JR. Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med. 2002;163:49–56. doi: 10.1001/archinte.163.1.49. [DOI] [PubMed] [Google Scholar]