Abstract
OBJECTIVE
We explore differences in the prevalence of asthma and other respiratory diseases at the neighborhood level. In addition to traditional metrics of neighborhood structure (e.g., concentrated disadvantage, residential stability), we incorporate residents’ evaluations of neighborhood context. We examine the extent to which indicators such as disorder (observable signs of physical and social decay) and collective efficacy (trust and shared expectations for beneficial community action) account for differences in the prevalence of asthma and other respiratory diseases.
METHODS
We examine 338 Chicago neighborhoods, combining 3 data sources from the 1990s: 1) the Metropolitan Chicago Information Center Metro Survey; 2) the Decennial Census; and 3) the Project on Human Development in Chicago Neighborhoods Community Survey. We use a multilevel statistical approach to disentangle neighborhood- from individual-level effects.
MEASUREMENTS
A survey-based response to whether a physician has diagnosed asthma, bronchitis, emphysema, or other breathing problems.
RESULTS
Findings indicate that individual- and neighborhood-level factors are associated with asthma/breathing problems. At the individual level, female gender, smoking, and a weight problem are positively associated with asthma/breathing problems, while Latino ethnicity is protective. At the neighborhood level, collective efficacy is protective against asthma/breathing problems. Residential stability is positively associated only when levels of collective efficacy are controlled.
CONCLUSIONS
Neighborhood context, particularly collective efficacy, may be an underlying factor that reduces vulnerability to asthma and other respiratory diseases. Collective efficacy may enhance the ability to garner health-relevant resources, eliminate environmental hazards that trigger asthma, and promote communication among residents which, in turn, enables dissemination of information relevant to respiratory ailments.
Keywords: asthma, collective efficacy, disorder, community, neighborhood effects
Asthma and other respiratory diseases are associated with urban life, particularly circumstances of the impoverished.1, 2 Although asthma is one of the most common chronic diseases in the United States, affecting approximately 15 million people,3 it occurs disproportionately among low-income persons and those of African-American and, in some cases, Latino descent.4 On average, African Americans are 4 to 6 times more likely to die from asthma than their white counterparts.5
The prevalence of, hospitalizations for, and deaths due to asthma increased over the 1980s and 1990s (after showing a steady decline in the 1970s). The death rate for 1993–1995 was 17.9 per 100,000, over double the rate for the 1975–1979 period.5 Central plains states and large urban centers, particularly Chicago, New York, and Phoenix, contribute disproportionately to these higher rates.6
Concern over these alarming increases has led researchers to examine the prevalence, treatment, and long-term consequences of asthma, principally in urban centers. Recent research has emphasized substandard housing that heightens exposure to indoor allergens,7 health beliefs or practices that inhibit use of prescribed medication,8 and inadequate access to care and/or inconsistent use of the same provider.9,10 Individual-level poverty, which may contribute to or exacerbate each of these, has also been a focus of recent research.11 Although these factors may independently contribute to the increase in asthma prevalence, morbidity, and mortality, none incorporate aspects of the larger social circumstance in which patients live. Analyses of regions or metropolitan statistical areas alone might mask significant variation by community context,12 and it may be the community context itself that drives such factors as allergen exposure or knowledge of it.
What is it about life in a disadvantaged urban community that contributes to the prevalence of asthma? We examine one urban center, Chicago, to explore this question. Chicago has one of the highest asthma rates in the country, although there is significant variation in asthma rates across Chicago's communities.13 We employ a powerful new concept from sociology, collective efficacy, to explore the extent to which neighborhood context affects the prevalence of asthma.14,15 Collective efficacy captures the level of trust and attachment characterizing community residents and their capacity for mutually beneficial action. We suggest that collective efficacy may ameliorate asthma-inducing conditions in inner-city neighborhoods. Low levels of trust, for instance, may be associated with a tendency to remain indoors and to consistently secure doors and windows, increasing exposure to indoor allergens. High levels of collective efficacy, on the other hand, may encourage the dissemination of health-enhancing information throughout communities and promote trust of both neighbors and local health care providers. A second community-level factor potentially relevant to the prevalence of asthma is the degree of social and physical disorder. Salient indicators of crime, gang activity, boarded-up housing, graffiti, and other cues that the local social order has broken down may also encourage residents to secure themselves and their children within their homes, concentrating exposure to allergens. We test whether these factors are associated with the prevalence of asthma and other respiratory diseases. Specifically, we hypothesize that communities with high collective efficacy and low disorder will experience a lower prevalence.
METHODS
To address our hypotheses, we need 1) data sources that provide individual-level outcomes nested in neighborhoods; 2) measures that capture both individual- and neighborhood-level phenomena; and 3) analytic methods that allow us to tease apart, to the extent possible, the separate contributions of individual- and neighborhood-level factors. This study combines 3 data sources from the 1990s to examine the extent to which neighborhood social context is associated with the prevalence of asthma and other respiratory diseases: 1) the Metropolitan Chicago Information Center Metro Survey (MCIC-MS); 2) the Decennial Census; and 3) the Project on Human Development in Chicago Neighborhoods Community Survey (PHDCN-CS). We describe each data source and its measures, then discuss the challenges inherent with analyses in a multilevel context and the tools we employ to address these challenges.
Data and Measures
MCIC-MS
The MCIC-MS is a serial cross-section of adults ages 18 and older who reside in the 6-county metropolitan Chicago area (on average, 3,000 respondents per wave). It focuses on an array of individual-level measures of health and well being. The response rate for the MCIC-MS was approximately 55% across the 10 cross-sectional samples available at the time of this study (1991–2000). Because the MCIC-MS did not achieve as high a response rate as the PHCDN-CS (described below), we compare the latter with combined 1993–1996 MCIC-MS samples. The distributions across demographic characteristics such as gender, age, and race in these MCIC-MS waves were similar to the PHDCN-CS, indicating that the sampling strategy of the former captures a reasonably representative sample of the city of Chicago. To create the individual-level component of our final analytic data set, we pooled the 1995, 1997, and 1999 waves of the MCIC-MS (N = 3,268).
Measures
The outcome measure and individual-level covariates come from the MCIC-MS. The outcome is a dichotomous measure derived from the question “Has a doctor ever told you that you have asthma, bronchitis, emphysema, or other breathing problems?” (hereafter referred to as asthma/breathing problems). While this question does not measure the presence of asthma alone, the high prevalence of asthma in Chicago suggests that the vast majority of these cases are asthma.13 This form of self-reported health status question has been found to be both reliable and valid.16 The individual-level covariates include gender, age, race/ethnicity, education, income, home ownership, years resident in neighborhood, marital status, current smoking behavior, physician-indicated weight problem, insurance status, and a regular source of care indicator.
Decennial Census
Census data allow us to construct measures of neighborhood socioeconomic structure. We use publicly available data obtained from the 1990 U.S. Census Summary Tape File STF 3B.
Measures
Two of the 4 neighborhood-level measures come from the Census. Factor analysis with oblique rotation was used to construct these measures. The first is a concentrated disadvantage factor score that includes percent below the poverty line, receiving public assistance, unemployed, in female-headed households, under age 18 (concentration of children), and African American. Factor loadings exceeded 0.85 for all measures of disadvantage (the factor loading for percent African American was 0.60). Ideally, the racial composition of the neighborhood clusters would be considered independently of concentrated disadvantage. Unfortunately, the extremely high correlation between these conceptually distinct dimensions renders investigation of their unique effects statistically problematic. Because we are primarily interested in disadvantage and racial composition as controls at this stage of the analysis, we combine them in a single factor. The second is a residential stability factor score that includes the percentage living in the same house since 1985 and the percentage of owner-occupied dwellings. Factor loadings exceeded 0.70. Disadvantage and stability are included as controls in the analysis to capture key aspects of neighborhood environment with which collective efficacy may be confounded.
PHDCN-CS
The sampling design of the PHDCN-CS relied on 1990 U.S. Census data for Chicago to identify 343 neighborhood clusters (NCs)—groups of 2 to 3 census tracts that contain approximately 8,000 people. Major geographic boundaries (e.g., railroad tracks, parks, freeways), knowledge of Chicago's local neighborhoods, and cluster analyses of Census data guided the construction of NCs so that they are relatively homogeneous with respect to racial/ethnic mix, socioeconomic status, housing density, and family structure.14 The study had 3 stages. At stage 1, city blocks were sampled within each NC; at stage 2, dwelling units were sampled within blocks; at stage 3, 1 adult resident (18 or older) was sampled within each selected dwelling unit. In total, 8,782 individuals 18 years of age or older were interviewed in their homes in 1995, with an average of 25 individuals per NC. The plan was designed to yield a representative probability sample of Chicago residents and large enough within-cluster samples to create reliable between-neighborhood measures. The final response rate was 75%. The samples within NCs were designed to be approximately self-weighting, and thus, between-neighborhood analyses are based on unweighted data.14 Participants rated their neighborhoods on a number of dimensions including social and physical disorder, violence and victimization, social cohesion, informal social control, danger, and availability of resources. By “neighborhood,” the survey protocol stated: “…we mean the area around where you live and around your house. It may include places you shop, religious or public institutions, or a local business district. It is the general area around your house where you might perform routine tasks, such as shopping, going to the park, or visiting with neighbors.”17
Measures
The 2 main covariates we use to test our hypothesis—collective efficacy and disorder—come from these data. Collective efficacy was operationalized through combining measures of social cohesion and informal social control. Social cohesion was constructed from a cluster of conceptually related items from the PHDCN-CS measuring the respondent's level of agreement (on a 5-point scale) with the following statements: 1) “People around here are willing to help their neighbors”; 2) “This is a close-knit neighborhood”; 3) “People in this neighborhood can be trusted”; and 4) “People in this neighborhood generally don’t get along with each other” (reverse coded). Health-related informal social control was tapped through items measuring the respondent's level of agreement with the following: 1) “If I were sick I could count on my neighbors to shop for groceries for me”; and 2) “You can count on adults in this neighborhood to watch out that children are safe and don’t get in trouble.” An additional informal social control item asked respondents how likely it is that people in their neighborhood would intervene if a fight broke out in front of their house. The informal social control items tap expectations for beneficial health-related action as well as neighborhood supervision of potentially hazardous conditions or violent situations. The 7 items were combined to form a single scale of health-related collective efficacy. The multilevel reliability of the collective efficacy scale is 0.73 (multilevel reliability is a function of the sample size of each neighborhood and the proportion of total variance between groups relative to the amount within groups).18 Disorder measures the level of social and physical disorder, with 4 items asking respondents to assess the prevalence of public drinking, abandoned buildings, litter and trash, and graffiti. The multilevel reliability of the disorder scale is 0.88.
Analysis
The clustering of respondents within Chicago's neighborhoods renders standard ordinary least squares techniques inappropriate due to the likely underestimation of standard errors. Our analysis strategy employs a random effects logit model—using hierarchical modeling (HM) techniques—to investigate the prevalence of asthma/breathing problems across neighborhoods.18 This approach has several advantages. Primarily, the technique adjusts standard errors for the effects of clustering within neighborhoods. In addition, HM provides a method for estimating the percentage of the total variance in any given outcome that can be attributed to neighborhood-level factors. In order to correct independent neighborhood-level measures of collective efficacy and disorder for missing data and measurement error, we use empirical Bayes residuals from a 3-level item-response model of the component items of these scales.18
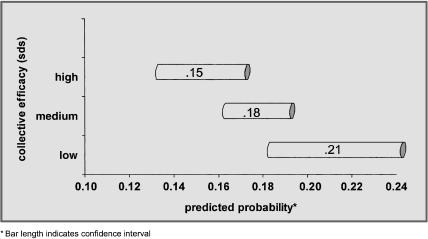
We begin with means and standard deviations (SD) that describe our study population, the individual-level component of our analysis (Table 1). We then construct a correlation matrix for the neighborhood-level variables (Table 2). The main feature of our analysis is a series of 6 nested hierarchical logit models (Table 3) that combine individual- and neighborhood-level covariates. A “yes” response to the asthma/breathing problems question forms the outcome. The 2-level HM logit coefficients in Table 3 are log odds ratios. Positive coefficients are associated with having asthma/breathing problems. We sequentially introduce individual-level demographic and socioeconomic background factors, health background factors, insurance status, and a regular source of care indicator. We then incorporate concentrated disadvantage and residential stability. The last 2 models introduce collective efficacy and disorder, respectively. Interview year is included as a control variable across models. Finally, we show a graphical representation of the predicted probability of asthma/breathing problems at selected levels of collective efficacy (Fig. 1).
Table 1.
Descriptive Statistics for Individual-level Variables
| Variables | Mean | Standard Deviation |
|---|---|---|
| Outcome | ||
| Asthma/breathing problems Control variables | 0.19 | 0.39 |
| Female | 0.59 | 0.49 |
| Age | 42.76 | 15.99 |
| Race/ethnicity | ||
| White | 0.40 | 0.49 |
| Black | 0.35 | 0.48 |
| Latino | 0.19 | 0.39 |
| Other | 0.06 | 0.23 |
| Education | ||
| 4th grade or less | 0.01 | 0.12 |
| 5th to 8th grade | 0.05 | 0.22 |
| 9th to 12th grade, no diploma | 0.11 | 0.31 |
| High school graduate | 0.16 | 0.37 |
| Trade or vaocational school | 0.08 | 0.26 |
| Some college | 0.26 | 0.44 |
| College graduate | 0.17 | 0.37 |
| Some graduate study | 0.03 | 0.18 |
| Graduate degree | 0.12 | 0.33 |
| Income, $ | ||
| ≤10,000 | 0.09 | 0.29 |
| >10,000 to 15,000 | 0.07 | 0.26 |
| >15,000 to 20,000 | 0.07 | 0.25 |
| >20,000 to 25,000 | 0.07 | 0.25 |
| >25,000 to 30,000 | 0.09 | 0.29 |
| >30,000 to 40,000 | 0.15 | 0.35 |
| >40,000 to 50,000 | 0.13 | 0.33 |
| >50,000 to 70,000 | 0.15 | 0.36 |
| >70,000 to 90,000 | 0.10 | 0.30 |
| >90,000 | 0.08 | 0.27 |
| Home ownership | 0.43 | 0.49 |
| Years resident in neighborhood | 11.55 | 9.73 |
| Married | 0.39 | 0.49 |
| Smoking | 0.29 | 0.45 |
| Weight problem | 0.20 | 0.40 |
| Insurance | ||
| Private insurance | 0.67 | 0.47 |
| Medicare | 0.08 | 0.27 |
| Medicaid | 0.08 | 0.28 |
| No insurance | 0.17 | 0.37 |
| Regular source of care | ||
| None | 0.04 | 0.19 |
| Doctor's office | 0.48 | 0.50 |
| HMO office | 0.15 | 0.36 |
| Hospital ER | 0.08 | 0.27 |
| Hospital clinic | 0.12 | 0.33 |
| Public clinic | 0.08 | 0.27 |
| Other clinic | 0.05 | 0.21 |
N= 3,268.
Table 2.
Correlations Among Neighborhood-level Variables
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Concentrated disadvantage | 1.000 | |||
| Residential stability | −0.048 | 1.000 | ||
| Collective efficacy | −0.393 | 0.311 | 1.000 | |
| Disorder | 0.766 | −0.294 | −0.580 | 1.000 |
N= 338.
Table 3.
Hierarchical Ordered Logit Models of Asthma/Breathing Problems*
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Individual-level | ||||||
| Interview year | 0.025 (.029) | 0.026 (.030) | 0.023 (.030) | 0.023 (.030) | 0.024 (.030) | 0.023 (.030) |
| Female | 0.387# (.095) | 0.363# (.095) | 0.354# (.096) | 0.352¶ (.096) | 0.353# (.096) | 0.352# (.096) |
| Age | −0.003 (.004) | −0.006 (.004) | −0.005 (.005) | −0.005 (.005) | −0.005 (.005) | −0.005 (.005) |
| Race/ethnicity† | ||||||
| Black | 0.196§ (.105) | 0.125 (.107) | 0.105 (.105) | 0.098 (.131) | 0.090 (.130) | 0.097 (.131) |
| Latino | −0.383|| (.164) | −0.360|| (.162) | −0.378|| (.162) | −0.376|| (.162) | −0.429¶ (.161) | −0.363|| (.163) |
| Education | −0.006 (.026) | −0.001 (.026) | −0.006 (.023) | 0.008 (.028) | 0.011 (.028) | 0.008 (.028) |
| Income | −0.002 (.019) | 0.000 (.019) | 0.006 (.020) | 0.005 (.020) | 0.008 (.020) | 0.005 (.020) |
| Home ownership | −0.017 (.018) | −0.007 (.119) | −0.006 (.119) | −0.039 (.126) | −0.055 (.126) | −0.039 (.126) |
| Years resident in neighborhood | ||||||
| 0.001 (.008) | 0.000 (.008) | 0.000 (.008) | 0.000 (.007) | 0.000 (.008) | 0.000 (.008) | |
| Married | −0.045 (.097) | −0.052 (.098) | −0.058 (.099) | −0.066 (.100) | −0.064 (.100) | −0.066 (.100) |
| Smoking | — | 0.229|| (.094) | 0.221|| (.095) | 0.222|| (.094) | 0.222|| (.094) | 0.223|| (.094) |
| Weight problem | — | 0.599# (.104) | 0.595# (.105) | 0.591# (.105) | 0.587# (.105) | 0.590# (.105) |
| Insurance‡ | ||||||
| Medicare | — | — | 0.183 (.174) | 0.189 (.177) | 0.190 (.178) | 0.187 (.178) |
| Medicaid | — | — | −0.092 (.209) | −0.089 (.208) | −0.067 (.207) | −0.092 (.208) |
| No insurance | — | — | 0.177 (.121) | 0.178 (.121) | 0.168 (.121) | 0.179 (.121) |
| No regular source of care | — | — | −0.374 (.274) | −0.372 (.275) | −0.386 (.275) | −0.373 (.275) |
| Neighborhood-level | ||||||
| Concentrated disadvantage | ||||||
| — | — | — | −0.011 (.062) | −0.059 (.064) | 0.016 (.095) | |
| Residential stability | — | — | — | 0.049 (.053) | 0.089§ (.053) | 0.039 (.057) |
| Collective efficacy | — | — | — | — | −0.132|| (.052) | — |
| Disorder | — | — | — | — | — | −0.037 (.100) |
| Intercept | −1.704# (.103) | −1.877# (.108) | −1.882# (.011) | −1.858# (.129) | −1.836# (.128) | −1.862# (.130) |
| Intercept variance component | 0.116|| | 0.103|| | 0.102|| | 0.104|| | 0.084§ | 0.104|| |
Neighborhood level N = 338; individual level N = 3,268.
Models estimated with robust standard errors.
Reference group is white/other.
Reference group is private insurance.
P < .10.
P < .05.
P < .01.
P < .001 (2-tailed tests).
Standard errors are in parentheses.
FIGURE 1.
Predicted probability of asthma/breathing problems at selected levels of neighborhood collective efficacy.
RESULTS
Table 1 describes our outcome and covariates of interest. Across neighborhoods, approximately 19% of the MCIC-MS respondents report that a physician has told them that they have asthma/breathing problems. The sample is 40% white, 35% African American, and 19% Latino, with the remainder falling in the “other” race/ethnicity group. Education, income, insurance, and access to care measures are relatively representative of the Chicago population. Of note, approximately 29% of the sample currently smokes and nearly 20% have been told by a physician that they have a weight problem (both of which potentially exacerbate asthma/breathing problems). The correlations presented in Table 2 show the extent to which the neighborhood-level variables in our analyses are interrelated. Disorder and concentrated disadvantage are the 2 variables with the highest positive association (r = .766), suggesting that concentrated disadvantage might manifest itself in disorder. As expected, disorder and collective efficacy are negatively associated (r = −.580), indicating that collective efficacy might inhibit visible signs of disorder. To a lesser extent, concentrated disadvantage is also negatively associated with collective efficacy (r = −.393). With the possible exception of disorder and concentrated disadvantage, the correlations illustrate that these variables are all tapping relatively unique components of neighborhood social context.
Table 3 shows a series of models that introduce, sequentially, individual- and neighborhood-level covariates (for ease of discussion, we will discuss selected coefficients in terms of odds ratios). In model 1, we see that women are nearly 1.5 times more likely to report asthma/breathing problems than men. While there is a positive relationship between African-American race and asthma/breathing problems, there is a negative relationship for Latino respondents. Contrary to expectations, we find no individual-level poverty effect. This may indicate that it is not income itself, but another variable correlated with income, that influences asthma/breathing problems prevalence. Model 2 introduces smoking and a weight problem (physician-reported). Current smokers are 1.25 times more likely to report asthma/breathing problems. Those with a physician-indicated weight problem are 1.82 times more likely to report such a diagnosis. Adjusting for these 2 health-related variables renders the African-American race coefficient insignificant. Insurance status and a dichotomous indictor for regular source of care, introduced in model 3, are not significant and do little to change the other covariates in the model.
The remaining 3 columns of Table 3 incorporate neighborhood-level variables with the individual-level models we have discussed previously. Measures of concentrated disadvantage and residential stability are not significant predictors in model 4. Female gender, Latino ethnicity, smoking, and weight all remain significantly associated with asthma/breathing problems (Latino ethnicity protective). Model 5 adds collective efficacy. Collective efficacy is significant and protective against asthma/breathing problems. A 2-SD increase on the collective efficacy scale results in a 22% reduction in the odds of reporting asthma/breathing problems. This means that the social cohesion and informal social control components that comprise collective efficacy have some potentially health-promoting attributes. The individual-level variables remain nearly the same, with the exception of Latino ethnicity (the protective effect increases modestly in magnitude). The introduction of collective efficacy results in a negligible change in the coefficient for concentrated disadvantage, but the coefficient for residential stability is now nominally significant (P < .10) and predictive of asthma/breathing problems. Model 6 substitutes disorder for collective efficacy. Disorder is not predictive of asthma/breathing problems and residential stability is no longer marginally significant. The individual-level variables remain unchanged with the introduction of the disorder measure.
The intercept variance component indicates the extent to which the prevalence of asthma/breathing problems varies across neighborhoods. Even after controlling for demographic background, individual-level socioeconomic status, and health-related variables, we continue to find significant variation in prevalence across neighborhood context (i.e., likelihood ratio χ2 tests on the intercept variance achieve significance at the conventional level). When we include collective efficacy, it accounts for approximately 18% of the residual neighborhood-level variance in asthma/breathing problems.
Figure 1 illustrates the predicted probability of asthma/breathing problems at selected levels of collective efficacy (where a −1.5 SD is low, 0 medium, and 1.5 high). The graded impact of collective efficacy on the likelihood of asthma/breathing problems is evident. When collective efficacy in a neighborhood is high, respondents have a 15% probability of reporting asthma/breathing problems as compared with 21% in the low–collective efficacy context. Note also that our estimates of the effect of collective efficacy are conservative—collective efficacy may exert influence on individual-level factors (e.g., health behaviors) that, in turn, affect asthma/breathing problems.
DISCUSSION
The aim of this paper was to understand the role of neighborhood social context in asthma. We focused on 2 key measures—collective efficacy and disorder (both social and physical). We hypothesized that neighborhood social context would affect asthma prevalence in the community. We postulated that characteristics of the community, not reducible to the individual level, contribute to the likelihood of such factors as allergen exposure.9 We employed a multilevel modeling approach so that we could sufficiently separate individual- from neighborhood-level effects. To our knowledge, this is the first instance where multilevel models have been employed to understand the link between neighborhood context and asthma.
Results indicate that individual-level variables such as female gender, current smoking, and a physician-indicated weight problem are all associated with a report of asthma/breathing problems. The finding on gender, although striking, is relatively consistent with published reports on gender differences in asthma attack rates, emergency department visits, and hospitalizations.3 Smoking often has been identified as aggravating asthma/breathing problems, and smoking cessation continues to be an area of high priority for the treatment of asthmatics.19 Although weight has been identified as a correlate to asthma,20 its role and its differential impact across groups remain under investigation. For instance, Guerra et al.21 found that preobese and obese women, in particular, are at increased risk of acquiring asthma. Chen et al.22 also found that obesity was salient for women. In this research, weight has a more powerful impact than smoking. That the coefficient for African-American race was rendered insignificant when smoking and a weight problem were introduced into the model highlights the need for future research on the relationship between health behavior and asthma.
The protective effect of Latino ethnicity might seem contrary to published research that typically shows Latino residents at a health disadvantage with respect to asthma.4 However, recent work by Homa et al. has shown that asthma prevalence varies considerably across Latino groups.23 Puerto Ricans have an asthma mortality rate of approximately 40.9 per million, Cuban Americans 15.8 million, and Mexican Americans 9.2 million. Because Chicago's Latino population is disproportionately of Mexican descent, our results are in keeping with Homa et al.'s work—this further illustrates the importance of incorporating national origin into research that includes Latino populations. Our results also may be reflective of the “Latino paradox” with respect to health outcomes.24
Contrary to expectations, individual-level income and education were not predictive of asthma/breathing problems. Insurance status and regular source of care also were not predictive. It may be, for instance, that income, education, insurance, and regular source of care are associated with asthma attacks or death from asthma, rather than the presence of asthma alone. The presence of asthma may be driven more readily by environmental context, to which we now turn.
At the neighborhood level, collective efficacy, as hypothesized, was protective. The higher the level of collective efficacy in the community, the lower the asthma/breathing problems prevalence. Neither concentrated disadvantage nor disorder was predictive. Residential stability was nominally predictive when entered in the presence of collective efficacy. This variable may capture older housing stock or reflect the negative consequences of residential stability described by Wilson25; social isolation and its associated limitations may impede opportunities to garner and sustain a healthful environment.
How might collective efficacy affect asthma specifically? As applied to health, the sociological theory of collective efficacy suggests that neighborhoods vary in the density and prevalence of community social networks and their associated levels of social cohesion and informal social control. The latter taps the community's capacity to mobilize existing social resources (network ties and community attachments) toward beneficial ends—this includes a healthful environment. The general mechanisms through which collective efficacy may protect against respiratory ailments such as asthma include: 1) the social control of health-compromising behaviors that could affect the onset of asthma (e.g., smoking); 2) the ability to secure high-quality and accessible health services that may encourage health-enhancing practices (e.g., breastfeeding), or aggressive treatment of conditions such as Respiratory Syncytial Virus, so residents are less likely to develop asthma or chronic broncospasm later in life; 3) the management of neighborhood physical hazards and potentially noxious conditions (e.g., an abandoned building may exacerbate exposure to cockroaches and mold)26; and 4) psychosocial processes (e.g., fear and stress that lead one to stay inside).
Allergen exposure,7 or susceptibility to exposure, may be the key element that collective efficacy can ameliorate. If residents feel uncomfortable walking outside or leaving windows open to fresh air, they may be continually exposed to high levels of indoor allergens such as dust mites or cockroaches. Similar to the older people who did not leave their homes during Chicago's heat wave,27 residents may be more apt to stay inside, even if health is potentially in jeopardy, to avoid perceived risks on the outside. In lower-income households where air conditioning is at a premium, air circulation may be further compromised. Air conditioning could reduce the presence of both indoor and outdoor triggers.28 Further, neighborhoods with low collective efficacy may not have parks perceived to be safe or other municipal features that encourage people to leave their homes; if residents are “out and about,” they not only get a reprieve from indoor allergens but also are contributing to network building and collective efficacy in their neighborhoods. In addition, communities with high collective efficacy are likely better equipped to provide forums, however informal, to discuss triggers to asthma and methods to avoid them. Or, they may have health resources in place that encourage activities, such as breastfeeding, which may have protective effects for the later emergence of allergies.
The study is not without limitations. First, our sample is restricted to the city of Chicago. While the data provide an unprecedented opportunity to examine community-based measures of intervening social processes at the neighborhood level on health, our capacity to generalize from the analyses is limited. Second, our individual-level data are cross-sectional. Despite relatively extensive health controls, we are unable to rule out selection effects as a confounding process in the association between neighborhood factors and asthma/breathing problems. Third, the survey question soliciting asthma/breathing problems is a self-report and is broad in nature. Although we realize that this type of question does not indicate a definitive diagnosis of any of the breathing problems mentioned, this type of question has been found to be reliable and valid in its ascertainment of health status. Further, the inclusion of respiratory conditions other than asthma may mute the effects of neighborhood context on the outcome measure, particularly if they do not share a common etiology (thus a more conservative test of our hypotheses). Finally, addressing asthma specifically, we are not able to examine quality of care, nor the rate of asthma attacks, emergency department visits, or hospitalizations. We believe, however, that the relationship between neighborhood context and potential triggers for asthma may provide insight into further analyses on these aspects of asthma and asthma care.
Previous research indicated a link between poverty and asthma, but we had little knowledge of the mechanism. The prevalence of asthma may not be affected by poverty, but rather by the social organization of the neighborhood. Although we have observed heightened asthma rates in poor neighborhoods, it might rather be poorly organized neighborhoods that we are observing. Findings such as these may encourage us to think differently about the role of socioeconomic status and its implications for health.29
Acknowledgments
Thanks to David Meltzer, JGIM reviewers, and participants in the University of Chicago Population Research Center Demography Workshop and the University of Chicago Department of Health Studies Seminar for their helpful comments. We wish to thank Robert Sampson, Felton Earls, and members of the Project on Human Development in Chicago Neighborhoods for generously providing access to the Community Survey. We also thank D. Garth Taylor and the Metropolitan Chicago Information Center for providing access to the Metro Survey.
REFERENCES
- 1.Steigman DM. Is it “urban” or is it “asthma”? Lancet. 1996;348:143–4. doi: 10.1016/s0140-6736(05)66107-7. [DOI] [PubMed] [Google Scholar]
- 2.Weiss KB, Grant EN, Li T. The effects of asthma experience and social demographic characteristics on responses to the Chicago Community Asthma Survey-32. Chicago Asthma Surveillance Initiative Project Team. Chest. 1999;116(4 suppl 1):183S–89S. doi: 10.1378/chest.116.suppl_2.183s. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. New estimates for asthma tracked. Atlanta, Ga: Centers for Disease Control; 2001. [Google Scholar]
- 4.Carr W, Zeitel L, Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am J Public Health. 1992;82:59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute of Allergy and Infectious Diseases. Asthma: a concern for minority populations. Bethesda, Md: National Institutes of Health; 2001. [Google Scholar]
- 6.Weiss KB, Wagener DK. Geographic variations in US asthma mortality: small-area analyses of excess mortality, 1981–85. Am J Epidemiol. 1990;132(1 suppl):S107–S15. doi: 10.1093/oxfordjournals.aje.a115771. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein JA, Fuhlbrigge A, Lozano P, et al. Parent-reported environmental exposures and environmental control measures for children with asthma. Arch Pediatr Adolesc Med. 2002;156:258–64. doi: 10.1001/archpedi.156.3.258. [DOI] [PubMed] [Google Scholar]
- 8.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: parent perspectives. Pediatrics. 2000;106:512–9. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 9.Adams RJ, Fuhlbrigge A, Guilbert T, Lozano P, Martinez F. Inadequate use of asthma medication in the United States: results of the asthma in America national population survey. J Allergy Clin Immunol. 2002;110:58–64. doi: 10.1067/mai.2002.125489. [DOI] [PubMed] [Google Scholar]
- 10.Hartert TV, Windom HH, Peebles RS, Jr, Freidhoff LR, Togias A. Inadequate outpatient medical therapy for patients with asthma admitted to two urban hospitals. Am J Med. 1996;100:386–94. doi: 10.1016/s0002-9343(97)89513-7. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz J, Gold D, Dockery DW, Weiss ST, Speizer FE. Predictors of asthma and persistent wheeze in a national sample of children in the United States. Association with social class, perinatal events, and race. Am Rev Respir Dis. 1990;142:555–62. doi: 10.1164/ajrccm/142.3.555. [DOI] [PubMed] [Google Scholar]
- 12.Almeida JP, Lwebuga-Mukasa JS. Geographic variations in asthma mortality in Erie and Niagara counties, western New York, 1991–96. Am J Public Health. 2001;91:1394–5. doi: 10.2105/ajph.91.9.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naureckas ET, Wolf RL, Trubitt MJ, et al. The Chicago Asthma Consortium: a community coalition targeting reductions in asthma morbidity. Chest. 1999;116(4 suppl 1):190S–93S. doi: 10.1378/chest.116.suppl_2.190s. [DOI] [PubMed] [Google Scholar]
- 14.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;227:918–23. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 15.Browning CR, Cagney KA. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. J Health Soc Behav. 2002;43(December):383–99. [PubMed] [Google Scholar]
- 16.Patrick DL, Erickson P. Health Status and Health Policy: Allocating Resources to Health Care. New York, NY: Oxford University Press; 1993. [Google Scholar]
- 17.Earls F. Connecting Social Science to the world. Cambridge, Mass: Harvard University; 2001. World Available at: http://www.hms.harvard.edu/chase/projects/chicago/about/connect.html. Accessed Jannuary 22, 2004. [Google Scholar]
- 18.Raudenbush SW, Bryk AS. Hierarchical Linear Models Applications and Data Analysis Methods. Thousand Oaks, Calif: Sage; 2002. [Google Scholar]
- 19.Eisner MD, Yelin EH, Trupin L, Blanc PD. Asthma and smoking status in a population-based study of California adults. Public Health Rep. 2001;116:148–57. doi: 10.1016/S0033-3549(04)50006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Litonjua AA, Sparrow D, Celedon JC, DeMolles D, Weiss ST. Association of body mass index with the development of methacholine airway hyperresponsiveness in men: the Normative Aging Study. Thorax. 2002;57:581–5. doi: 10.1136/thorax.57.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guerra S, Sherrill DL, Bobadilla A, Martinez FD, Barbee RA. The relation of body mass index to asthma, chronic bronchitis, and emphysema. Chest. 2002;122:1256–63. doi: 10.1378/chest.122.4.1256. [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, Dales R, Tang M, Krewski D. Obesity may increase the incidence of asthma in women but not in men: longitudinal observations from the Canadian National Population Health Surveys. Am J Epidemiol. 2002;155:191–7. doi: 10.1093/aje/155.3.191. [DOI] [PubMed] [Google Scholar]
- 23.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990–95. Am J Respir Crit Care Med. 2000;161:504–9. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 24.Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann NY Acad Sci. 2001;954:140–74. doi: 10.1111/j.1749-6632.2001.tb02751.x. [DOI] [PubMed] [Google Scholar]
- 25.Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago, Ill: The University of Chicago Press; 1987. [Google Scholar]
- 26.Litonjua AA, Carey VJ, Burge HA, Weiss ST, Gold DR. Exposure to cockroach allergen in the home is associated with incident doctor-diagnosed asthma and recurrent wheezing. J Allergy Clin Immunol. 2001;107:41–7. doi: 10.1067/mai.2001.111143. [DOI] [PubMed] [Google Scholar]
- 27.Klinenberg E. Heat Wave: A Social Autopsy of Disaster in Chicago. Chicago, Ill: The University of Chicago Press; 2002. [DOI] [PubMed] [Google Scholar]
- 28.Tartasky D. Asthma in the inner city: a growing public health problem. Holist Nurs Pract. 1999;14:37–46. doi: 10.1097/00004650-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Williams DR. Socioeconomic differentials in health: a review and redirection. Social Psychol Q. 1990;53:81–99. [Google Scholar]