Abstract
OBJECTIVE
To identify sociodemographic characteristics, numeracy level, and breast cancer risk factors that are independently associated with the accuracy of lifetime and 5-year breast cancer risk perceptions.
DESIGN
Cross-sectional survey. A probability scale was used to measure lifetime and 5-year risk perceptions. The absolute difference between perceived risk and the Gail model risk of breast cancer was calculated. Linear regression models were built to predict lifetime and 5-year breast cancer risk estimation error.
SETTING
Primary care internal medicine practices (N = 2).
PARTICIPANTS
Two hundred fifty-four women 40 to 85 years of age.
RESULTS
The mean lifetime and 5-year calculated breast cancer risk was 8.4% (SD [standard deviation] 6.1) and 1.5% (SD 1.3), respectively. Subjects had a mean estimation error for lifetime and 5-year risk of 29.5% (SD 22.9) and 24.8% (SD 23.9), respectively. In multivariate analyses, lower numeracy scores (0.005), higher number of previous breast biopsies (0.016), and a higher number of first-degree relatives (0.054) were predictive of larger estimation error for lifetime breast cancer risk. White race (0.014), lower educational levels (0.009), higher number of previous breast biopsies (0.008), and higher number of first-degree relatives (0.014) were predictive of larger estimation error for 5-year risk.
CONCLUSION
Among a primary care population, breast cancer risk factors may be more consistently associated with pessimistic perceptions of breast cancer risk than other factors studied during a lifetime and 5-year time span. Primary care physicians should consider counseling patients about individual breast cancer risk factors and risk over time.
Keywords: breast neoplasm, risk perception, pessimism, numeracy
It is human nature to demonstrate an optimistic bias (thereby underestimating risk) when considering personal risk.1 In contrast to this general finding, research has consistently found pessimism (overestimation) among women when estimating their risk of developing breast cancer.2–6 The reasons for this pessimism are not fully understood. Research in the field of breast cancer risk perception lacks standard methods with regard to the populations studied, variables evaluated, and statistical analyses employed. Prior studies have primarily evaluated populations at high risk and of limited diversity, and have not consistently incorporated breast cancer risk factors into the analyses.2–6 The primary purpose of our study is to better understand the effects of sociodemographic characteristics, numeracy, and breast cancer risk factors on breast cancer risk perception in a diverse average-risk population. A better understanding of predictors of pessimism will enhance our ability to counsel women effectively regarding their breast cancer risk.
METHODS
Conflict of Interest Notification
This work was supported by a grant from the American Cancer Society. The funding agency approved the original research design in the form of a grant application. The funding agency had no further role in the research design and collection of data, data analysis, data interpretation, reporting of the data, or conclusions drawn from the data. The funding agency had no role in the manuscript preparation. Investigators had full access to the data. The investigators accept full responsibility for the integrity of the data and the accuracy of the data analysis.
Subjects and Setting
Subjects were recruited from 2 primary clinic sites associated with faculty practices at the Medical College of Wisconsin. Inclusion criteria were female gender, ages 40 through 85 years, and the ability to speak English. Potential subjects were excluded if they had a personal history of breast cancer, dementia, or a comorbid condition leading to a life expectancy of less than 2 years as judged by their primary care provider. Invitation letters were mailed out to all eligible subjects between June 15, 1999 and June 19, 2000. The last entry date was July 26, 2000. The letter conveyed that the investigators were attempting to improve knowledge regarding preventive health care and did not specifically refer to breast cancer. Each letter was followed up with a telephone call to assess interest in the study. Approval from the Human Subjects Review Committee for the participating institutions was obtained.
Recruitment letters were mailed to 1,409 women (about 25% of our sampling frame). The sampling frame consisted of women over 40 years of age who were enrolled in one of the primary care clinic sites. Of the 1,409 eligible subjects, 967 were successfully contacted by telephone, and 254 women were enrolled. The final recruitment rate was 18% (254/1,409). Over 80% of those that declined stated the reason as lack of interest in participating in the study. Enrolled subjects were compensated $20 for their time.
Procedures
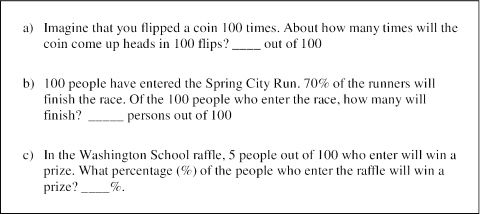
Subjects completed a breast cancer risk perception survey. The survey was self-administered with a research assistant available to answer questions. The survey was completed in an office in the same building as the participating clinics. The survey ascertained sociodemographic factors, breast cancer risk factors, and numeracy. Numeracy was assessed with a 3-item scale, adapted from a previously validated numeracy scale (Fig. 1).5,7 The final numeracy scale had adequate internal consistency in our study population (Cronbach's α = 0.63).
FIGURE 1.
Numeracy assessment. This figure displays the numeracy assessment used in study. Answers: a. 50, b. 70, and c. 5. The number of correct responses comprised the numeracy score (range 0 to 3). The Cronbach's α of the scale for our population was 0.63.
Measurement of Calculated Risk.
The Gail et al. (1989) model for breast cancer risk, modified to incorporate information on race, was used to estimate the risk of breast cancer over a 5-year period and for a lifetime.8–10 This model includes information on age, race, number of first-degree relatives with breast cancer, age at menarche, age at first live birth, number of breast biopsies, and history of atypical hyperplasia. All data entered into the model were obtained by patient history. The history of atypical hyperplasia was not confirmed by pathologic report.
Measurement of Perceived Breast Cancer Risk.
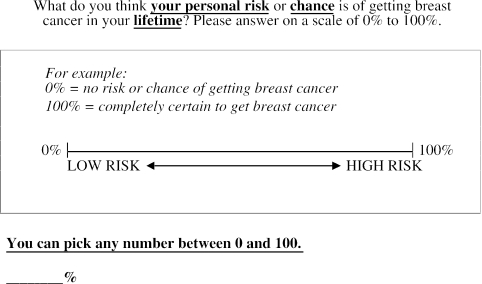
Perceived lifetime breast cancer risk was measured on a percent scale, ranging from 0% to 100%. To elicit an individual's perception of their lifetime risk of breast cancer, the following question was asked.
What do you think your personal risk or chance is of getting breast cancer in your lifetime? Please answer on a scale of 0% to 100%.
A graphic was included to illustrate 0% as low risk and 100% as high risk (Fig. 2). A similar question was asked to measure perceived risk over a 5-year time frame.
FIGURE 2.
Lifetime risk assessment. This figure displays the risk assessment scale and graphic used to measure lifetime risk. A similar scale and graphic was used to assess 5-year risk.
Analysis
Estimation error was defined as the absolute difference of the perceived risk and the Gail model risk as portrayed below.
Univariate association of subject characteristics with lifetime and 5-year estimation error were evaluated using the appropriate nonparametric statistics. Multivariate linear regression models were developed to predict lifetime and 5-year estimation error, using backward-stepwise linear regression on Stata version 7.0 (Stata Corp., College Station, Tex). The dependent variable of estimation error was transformed using a log transformation (Log [1 + estimation error]) to improve the normality of the distribution. The variables considered for the model included those that were significant by univariate analysis and those that were predictive of risk perceptions in previous studies.3,6 The following variables were considered for the model: age, race, years of education, income level, numeracy score, family history of breast cancer, age at menses, age at first live birth, and number of prior breast biopsies. Income was dichotomized as follows: 1) annual family income less than $20,000 and 2) annual family income equal to or greater than $20,000. Age at first live birth was analyzed combining nulliparous and ages 25 to 29 per the equal risk estimate as determined by the Gail model.11 Potential interactions were evaluated between race and income, and race and education.
RESULTS
Study Population
The mean age of subjects was 57.6 years (SD [standard deviation] 10.10.6), with a range of 40 to 84 years. The majority of the participants had graduated from high school (81%) and reported a household income of less than $20,000 (50%). Sixty-eight percent were of white race, 30% were black, 4 subjects (1.6%) were Hispanic, and 2 subjects (0.7%) were Native American. Less than 50% answered all 3 numeracy questions correctly. The majority of the women had no family history of breast cancer (82%), and had no prior breast biopsies (77%) (Tables 1a and 1b).
Table 1a.
Univariate Association of Sociodemographic and Numeracy Characteristics with Estimation Error for Lifetime and Five-year Risk Estimates
| n | Lifetime Estimation Error % (mean, SD) | P Value* | Five-year Estimation Error % (mean, SD) | P Value* | |
|---|---|---|---|---|---|
| Total subjects | 254 | ||||
| Age quartiles, years | |||||
| 1st (40–50) | 71 | 30.7 (21.4) | 24.8 (21.9) | ||
| 2nd (51–56) | 58 | 31.4 (25.7) | 27.1 (27.4) | ||
| 3rd (57–65) | 64 | 28.7 (21.9) | 25.6 (24.8) | ||
| 4th (66–84) | 61 | 27.0 (22.8) | .33 | 21.9 (21.6) | .56 |
| Race | |||||
| White | 178 | 27.4 (21.4) | 25.5 (23.6) | ||
| Other | 81 | 33.9 (25.3) | .02 | 23.4 (24.4) | .37 |
| Education, years | |||||
| <12 | 49 | 37.9 (25.6) | 29.8 (28.9) | ||
| 12 | 81 | 29.9 (22.4) | 25.3 (24.9) | ||
| 12–16 | 97 | 26.9 (22.3) | 25.6 (21.7) | ||
| ≥17 | 27 | 22.0 (16.4) | .0005 | 11.8 (10.9) | .04 |
| Annual family income, $ | |||||
| <10,000 | 87 | 34.8 (24.9) | 27.9 (26.2) | ||
| 10,000–19,999 | 37 | 26.8 (18.9) | 25.5 (21.4) | ||
| 20,000–34,999 | 36 | 34.0 (24.5) | 29.9 (26.1) | ||
| 35,000–49,999 | 23 | 34.1 (22.1) | 32.1 (24.0) | ||
| 50,000–74,999 | 30 | 19.5 (19.7) | 15.0 (19.7) | ||
| >75,000 | 34 | 21.0 (19.1) | .002 | 16.8 (17.9) | .03 |
| Numeracy, number of correct responses | |||||
| 0 | 38 | 40.1 (25.3) | 32.2 (28.6) | ||
| 1 | 42 | 28.3 (24.2) | 24.0 (26.7) | ||
| 2 | 69 | 30.1 (21.1) | 27.8 (22.7) | ||
| 3 | 105 | 25.8 (21.7) | .006 | 20.5 (20.8) | .10 |
Spearman's correlation was used for continuous variables and ordinal. Kruskal–Wallis was used for categorical variables. Age and education were analyzed as a continuous variable.
Table 1b.
Univariate Association of Breast Cancer Risk Factors with Estimation Error for Lifetime and Five-year Risk Estimates
| Breast Cancer Risk Factor | n | Lifetime Estimation Error (mean, SD) | P Value* | Five-year Estimation Error (mean, SD) | P Value* |
|---|---|---|---|---|---|
| Total subjects | 254 | ||||
| Family history of breast cancer, number of first degree relatives | |||||
| 0 | 208 | 27.9 (22.8) | 22.2 (22.0) | ||
| 1 | 29 | 36.2 (23.0) | 31.0 (27.5) | ||
| ≥2 | 17 | 38.0 (20.0) | .005 | 45.7 (27.6) | .001 |
| Age at menarche, years | |||||
| ≤11 | 54 | 34.3 (24.6) | 25.0 (21.3) | ||
| 12–13 | 136 | 28.9 (22.4) | 24.2 (24.5) | ||
| ≥14 | 60 | 24.8 (20.3) | .04 | 24.1 (22.8) | .75 |
| Age at first live birth, years | |||||
| 13–19 | 8 | 35.1 (24.1) | 27.6 (25.1) | ||
| 20–24 | 73 | 24.6 (21.0) | 23.9 (23.8) | ||
| 25–29 | 37 | 25.3 (22.2) | 24.6 (24.4) | ||
| 30–39 | 12 | 33.0 (21.6) | 32.6 (24.5) | ||
| Nulliparous† | 43 | 28.9 (22.3) | .21 | 18.7 (19.9) | .28 |
| Number of breast biopsies | |||||
| 0 | 195 | 27.9 (23.3) | 22.2 (22.9) | ||
| 1 | 38 | 31.3 (20.8) | 32.3 (23.9) | ||
| 2 | 14 | 39.8 (20.4) | 34.5 (29.5) | ||
| ≥3 | 7 | 42.8 (18.9) | .006 | 37.9 (23.7) | .004 |
| Abnormal breast biopsy “history of atypical hyperplasia” | |||||
| Yes | 6 | 21.3 (17.5) | 18.3 (12.1) | ||
| No | 223 | 28.5 (22.9) | 23.9 (24.0) | ||
| Unknown | 24 | 41 (20.9) | .16 | 35.2 (23.2) | .10 |
Spearman's correlation was used for continuous variables and ordinal variables. Kruskal–Wallis was used for categorical variables.
In the multivariate analysis, the nulliparous and 25- to 29-year-old groups were combined (see results section).
Perceived Risk of Breast Cancer and Estimation Error
Subjects greatly overestimated their personal breast cancer risk (Table 2). The study population had a mean lifetime expected risk of 8.4% (SD 6.1) and a mean 5-year expected risk of 1.5% (SD 1.3) as calculated by the Gail model. The mean absolute estimation error (defined as the |perceived − Gail model risk|) was 29.5% (22.9 SD) for lifetime risk and 24.8% (23.9 SD) for 5-year risk. The majority of subjects overestimated risk, with only 10.7% and 17.7% underestimating their lifetime and 5-year risk, respectively. For those who did underestimate risk, the magnitude of underestimation was low, with a mean difference in perceived and calculated risk of −5.2% and −1.3% for lifetime and 5-year risk, respectively.
Table 2.
Gail Model Risk, Perceived Risk, and Estimation Error Among the Study Population
| Mean % (SD) | |
|---|---|
| Gail model breast cancer risk | |
| Lifetime, | 8.4 (6.1) |
| Five-year, | 1.5 (1.3) |
| Perceived breast cancer risk | |
| Lifetime, | 36.7 (25.3) |
| Five-year, | 25.9 (24.6) |
| Estimation error | |
| Lifetime, | 29.5 (22.9) |
| Five-year, | 24.8 (23.9) |
Estimation error was defined as the absolute difference of the perceived risk and the Gail mode risk.
SD, standard deviation.
Patient Characteristics Associated with Perceived Risk and Estimation Error
The association of sociodemographic and numeracy variables with estimation error was evaluated. Women of nonwhite race, lower levels of education, lower income, and lower numeracy levels were more likely to have an increased estimation error of lifetime breast cancer risk (Table 1a). With regard to breast cancer risk factors, women with a higher number of first-degree relatives with breast cancer, younger age of menarche, and higher numbers of previous breast biopsies were also more likely to have a larger estimation error of lifetime breast cancer risk (Table 1b). Women with lower levels of education, moderate to low income (< 50,000), a higher number of first-degree relatives with breast cancer, and a higher number of breast biopsies had a larger estimation error for 5-year breast cancer risk (Tables 1a and 1b).
Correlations Among Sociodemographic Variables
Positive correlations were found between the following sociodemographic and numeracy variables in our population (Spearman's correlation): 1) education and numeracy (0.53), 2) education and income (0.53), 3) education and white race (0.38), 4) income and numeracy (0.49), 5) income and white race (0.46), and 6) numeracy and white race (0.47).
Multivariate Analysis
A multivariate model was constructed to evaluate the independent effect of sociodemographic characteristics, numeracy scores, and breast cancer risk factors on estimation error of breast cancer risk. The final model predicting estimation error for lifetime risk included the variables of numeracy score, number of first-degree relatives with breast cancer, and number of prior breast biopsies. The following variables were associated with a larger estimation error: 1) lower numeracy scores, 2) higher number of first-degree relatives with breast cancer, and 3) higher number of breast biopsies. For 5-year risk, the final model included race, years of education, family history, and number of breast biopsies. A larger estimation error for 5-year risk was seen with: 1) white race, 2) less education, 3) higher number of first-degree relatives with breast cancer, and 4) higher number of breast biopsies (Table 3). No interaction between race and education was found.
Table 3.
Multivariate Linear Regression Model Predicting Lifetime and Five-year Breast Cancer Risk Estimation Error
| Lifetime | Five-year | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Coeff | SE | P Value | 95% CI | Coeff | SE | P Value | 95% CI |
| Race (other vs white) | — | — | — | — | −0.438 | 0.177 | .014 | −0.786 to −0.089 |
| Years of education | — | — | — | — | −0.08 | 0.031 | .009 | −0.141 to −0.020 |
| Numeracy | −0.18 | 0.063 | .005 | −0.303 to −0.056 | — | — | — | — |
| Family history | 0.238 | 0.123 | .054 | −0.004 to 0.479 | 0.339 | 0.138 | .014 | 0.068 to 0.611 |
| No. of breast biopsies | 0.234 | 0.096 | .016 | 0.045 to 0.424 | 0.294 | 0.110 | .008 | 0.078 to 0.511 |
| Constant | 2.97 | 0.211 | <.001 | 2.55 to 3.83 | 3.32 | 0.479 | <.001 | 2.38 to 4.27 |
Variables considered in the multivariate analysis include age, race, years of education, income, numeracy, family history of breast cancer, age of first live birth, and number of previous breast biopsies. Potential interactions between race and education were evaluated.
SE, standard error; CI, confidence interval.
DISCUSSION
We report a significant overestimation of breast cancer risk among a diverse group of women from a primary care practice. The mean difference between calculated and estimated risk was almost 30% for lifetime risk and 25% for 5-year risk, and consisted predominantly of overestimation. This finding reflects significant pessimism in breast cancer risk perceptions. Breast cancer risk factors, including a family history of breast cancer and previous breast biopsies, were more consistently associated with error in breast cancer risk perceptions than sociodemographic factors.
Few studies have evaluated and compared risk perceptions over different time frames.12 In our study, women conveyed lower risk estimates over the short-term versus lifetime time frame. However, the magnitude of the difference was not reflective of the true difference in risk over these respective periods. The models for lifetime and 5-year risk perceptions were similar; both included family history of breast cancer and a history of previous breast biopsies. However, they differed in terms of the contribution of sociodemographic factors and numeracy. The model for lifetime risk included numeracy but no sociodemographic factors. The model for 5-year risk included education and race but did not include numeracy. Education and numeracy are highly correlated and measure-related constructs. This may explain why only 1 of the 2 measures was in each model. Numeracy is a more specific measure of how people understand and use quantitative information and therefore may better reflect how well people retain widely publicized risk information (such as 12% lifetime risk). Given the correlation between numeracy and sociodemographic factors, further studies are needed to clarify the relationship of these characteristics to breast cancer risk perceptions. The finding that race was a factor in the 5-year but not lifetime model suggests that race might affect how people view risk over different time periods, an area that also warrants further study.
The direction of effect of sociodemographic factors in our 5-year model was consistent with previous literature. 2,3,6,13 Subjects with lower levels of education or white race were more pessimistic in their risk perceptions. The reasons for the race effect are not clear, although one study reports that black women are less aware of the importance of family history as a risk factor for breast cancer compared to white women.13 In contrast to previous studies, we did not find that younger age was associated with overestimation of breast cancer risk.3,6
The importance of numeracy in our lifetime risk perceptions model is an important finding and consistent with prior literature. In a study of women age 40 to 50 in New Hampshire, both numerate and innumerate women greatly overestimated their risk of breast cancer; however, less numerate women overestimated risk to a greater degree.2 Numeracy, or how comfortable people are with the use and interpretation of numbers, is likely to reflect how well people retain and process risk information.
Breast cancer risk factors were important predictors of risk perception in both our lifetime and 5-year risk models. Women with a family history of breast cancer or a history of previous breast biopsies were more likely to overestimate their risk than women without these risk factors. This finding is similar to that reported by Alexander et al., who found greater overestimation of breast cancer risk in women who had a mother with breast cancer.4 Other studies did not find this association, but differed from this study in using only univariate analysis14 or a dichotomous outcome variable.6
This study has important clinical implications. We found significant overestimation of breast cancer risk in an average-risk clinical population. Women who overestimate their risk of breast cancer have increased scores on measures of depression and anxiety, as well as less coping abilities compared to underestimators.15 In a higher risk population, breast cancer worries were found to be a barrier to breast cancer screening mammography, especially among women with less formal education.16 In another group of higher risk women, anxiety and emotional distress were found to interfere with screening and quality of life.17 It is therefore important for physicians to correct pessimistic breast cancer risk perceptions among primary care patients. Our study suggests that this is especially true among women at higher risk of breast cancer due to their family and clinical history. In addition, innumerate patients may need help with the interpretation of quantitative risk estimates.
This study has some limitations. We used a numeric scale to assess perceived risk. Results may differ with the use of a verbal (such as low, medium, high, or very high) or a comparative scale (such as lower, the same, or higher than others). Prior work has found underestimation of breast cancer risk when using verbal comparative scales, but overestimation when using numeric scales.12,18 Subjects may misinterpret numeric scales. A woman who considers herself average risk may report a number of 50%. For example, one subject stated that her risk was 50%, because she was “as likely as the next person” to get breast cancer. Comparative scales may be more intuitive to understand but are also subject to error. A woman may correctly respond that she is “the same” risk as most women, but significantly overestimate the magnitude of average risk. No gold standard exists for measuring risk perceptions. The study of reliability and validity of risk perception scales has been limited and needs further study.19,20 A second study limitation is the possible role of volunteer bias. Our study had a recruitment rate of 18% and may have preferentially enrolled subjects with an interest in preventive care. It is unclear in what direction this bias would affect the accuracy of risk perceptions.
We analyzed the data as an absolute difference rather than as ratios as some investigators have done.2,14 The use of ratios can inflate lower levels of difference when a woman is near accuracy (estimation error of zero). For example, if a woman's calculated risk is 5% and her risk estimate is 10%, she would have overestimated by a ratio of 2:1 or 100%. However, her absolute risk difference would be only 5%. A woman who had a calculated risk of 45% and a risk estimate of 50% would have overestimated by a ratio of 1.1:1, or 10%. Her absolute risk difference would also be 5%. By calculating error as an absolute difference, a 5% difference is of equal magnitude along the scale of 0% to 100%. We chose to analyze the absolute value of the difference because we were primarily interested in the magnitude (rather than direction) of error.
In conclusion, we find that women of average breast cancer risk in a primary care population overestimate their risk of developing breast cancer over a lifetime and 5-year time frame. The most consistent findings associated with overestimation were the presence of breast cancer risk factors, specifically, a higher number of first-degree relatives with a history of breast cancer and higher number of previous breast biopsies. In our study, innumeracy was an important predictor of pessimism regarding lifetime risk. However, further work is needed to fully to clarify the influence of numeracy and sociodemographic factors on patients’ perceptions of health risk. Physicians should consider counseling patients about individual risk factors and providing accurate information about breast cancer risk over time, especially for women with a family history of breast cancer and/or a history of previous breast biopsies.
Acknowledgments
This work was supported by an American Cancer Society Cancer Control Career Development Award to Dr. Schapira.
REFERENCES
- 1.Eiser JR. Communication and interpretation of risk. Br Med Bull. 1998;54:779–90. doi: 10.1093/oxfordjournals.bmb.a011729. [DOI] [PubMed] [Google Scholar]
- 2.Black WC, Nease RF, Tosteson AN. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. J Natl Cancer Inst. 1995;87:720–30. doi: 10.1093/jnci/87.10.720. [DOI] [PubMed] [Google Scholar]
- 3.Harris RP, Fletcher SW, Gonzalez JJ, et al. Mammography and age: are we targeting the wrong women? A community survey of women and physicians. Cancer. 1991;67:2010–4. doi: 10.1002/1097-0142(19910401)67:7<2010::aid-cncr2820670730>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 4.Alexander NE, Ross J, Sumner W, Nease RF, Littenberg B. The effect of an educational intervention on the perceived risk of breast cancer. J Gen Intern Med. 1996;11:92–7. doi: 10.1007/BF02599584. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:72. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 6.Daly MB, Lerman CL, Ross E, Schwartz MD, Sands CB, Masny A. Gail model breast cancer risk components are poor predictors of risk perception and screening behavior. Breast Can Res Treat. 1996;41:59–70. doi: 10.1007/BF01807037. [DOI] [PubMed] [Google Scholar]
- 7.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 8.Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–86. doi: 10.1093/jnci/81.24.1879. [DOI] [PubMed] [Google Scholar]
- 9.Fisher B, Constantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371–88. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- 10.Costantino JP, Gail MH, Pee D, et al. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst. 1999;91:1541–8. doi: 10.1093/jnci/91.18.1541. [DOI] [PubMed] [Google Scholar]
- 11.Benichou J, Gail MH, Mulvihill JJ. Graphs to estimate an individualized risk of breast cancer. J Clin Oncol. 1996;14:103–10. doi: 10.1200/JCO.1996.14.1.103. [DOI] [PubMed] [Google Scholar]
- 12.Lipkus IM, Kuchibhatla M, McBride CM, et al. Relationships among breast cancer perceived absolute risk, comparative risk, comparative risk, and worries. Cancer Epidemiol Biomarkers Prev. 2000;9:973–5. [PubMed] [Google Scholar]
- 13.Hughes C, Lerman C, Lustbader E. Ethnic differences in risk perception among women at increased risk for breast cancer. Breast Cancer Res Treat. 1996;40:25–35. doi: 10.1007/BF01806000. [DOI] [PubMed] [Google Scholar]
- 14.Smith BL, Gadd MA, Lawler C, et al. Perception of breast cancer risk among women in breast center and primary care settings: correlations with age and family history of breast cancer. Surgery. 1996;120:297–303. doi: 10.1016/s0039-6060(96)80301-1. [DOI] [PubMed] [Google Scholar]
- 15.Bowen D, Hickman KM, Powers D. Importance of psychological variables in understanding risk perceptions and breast cancer screening of African American women. Women's Health. 1997;3:227–42. [PubMed] [Google Scholar]
- 16.Lerman C, Daly M, Sands C, et al. Mammography adherence and psychological distress among women at risk for breast cancer. J Natl Cancer Inst. 1993;85:1074–80. doi: 10.1093/jnci/85.13.1074. [DOI] [PubMed] [Google Scholar]
- 17.Kash KM, Holland JC, Osborne MP, Miller DG. Psychological counseling strategies for women at risk of breast cancer. J Natl Cancer Inst Monogr. 1995;17:73–9. [PubMed] [Google Scholar]
- 18.Woloshin S, Schwartz LM, Black WC, Welch HG. Women's perception of breast cancer risk: how you ask matters. Med Decis Making. 1999;19:221–9. doi: 10.1177/0272989X9901900301. [DOI] [PubMed] [Google Scholar]
- 19.Woloshin S, Schwartz LM, Byram S, Fischhoff B, Welch HG. A new scale for assessing perceptions of chance. Med Decis Making. 2000;20:298–307. doi: 10.1177/0272989X0002000306. [DOI] [PubMed] [Google Scholar]
- 20.Diefenbach MA, Weinstein ND, O'Reilly J. Scales for assessing perceptions of health hazard susceptibility. Heath Educ Res. 1993;8:181–92. doi: 10.1093/her/8.2.181. [DOI] [PubMed] [Google Scholar]