Abstract
OBJECTIVE
Although hospitalists have been shown to improve both financial and educational outcomes, their ability to manage dual roles as clinicians and educators has been infrequently demonstrated, particularly in the community setting where large numbers of residents train. We evaluated the impact of hospitalists on financial and educational outcomes at a mid-sized community teaching hospital 1 year after implementation.
DESIGN
Two hospitalist clinician educators (HCEs) were hired to provide inpatient medical care while participating in resident education. Length of stay and cost per case data were calculated for all patients admitted to the hospitalist service during their first year and compared with patients admitted to private physicians. The hospitalists’ top 11 discharge diagnoses were individually assessed. For the same time period, categorical medicine residents (N = 36) were given an anonymous written survey to assess the HCEs’ impact on resident education and service.
RESULTS
Resource consumption: length of stay was reduced by 20.8% and total cost per case was reduced by 18.4% comparing the HCEs with community-based physicians. Reductions in both length of stay and cost per case were noted for 8 of the 11 most common discharge diagnoses. Resident survey: over 75% of residents responded, with all noting improvement in the quality of attending rounds, bedside teaching, and the overall inpatient experience. Residents’ roles as teachers and team leaders were largely unchanged.
CONCLUSION
Hospitalist clinician educators as inpatient teaching attendings effectively reduce length of stay and resource utilization while improving resident education at community-based teaching hospitals.
Keywords: hospitalist, clinician-educator, resident education, resource utilization
A driving force behind the expansion of the hospitalist movement is the potential to deliver high-quality medical care while decreasing inpatient costs and improving efficiency. Several institutions have demonstrated that both length of stay (LOS) and cost per case (C/C) have been reduced through the use of hospitalists.1–6 On average, hospitalists have been reported to reduce LOS by 16.6% and C/C by 13.4%.1 Such decreases have been shown in both academic2,3 and community-based institutions.4–6 Though economic forces ultimately drive the utilization of hospitalists, other outcomes, such as the benefit of hospitalists on the medical education of internal medicine residents and medical students, have been explored to a limited extent.7 In one large university medical center, residents expressed satisfaction with the teaching provided by hospitalists and reported that it was equivalent and often superior to that of traditional ward attendings.2 In fact, these residents requested that hospitalists be a part of all of their future inpatient ward rotations. Another university medical center found that the presence of hospitalists improved the quality of attending rounds, increased the emphasis on resident education during inpatient rotations, and enhanced residents’ overall learning experience.8
Despite the fact that hospitalists often serve in dual roles as clinicians and educators, there are few data on their ability to effectively manage these roles simultaneously. For academic community-based teaching hospitals, which educate the largest number of residents in internal medicine, there are no data. Structured evaluation of this model was performed when salaried, full-time hospitalist clinician educators (hereafter referred to as HCEs) were introduced at the Norwalk Hospital, an academic community hospital affiliated with Yale University.
METHODS
One year after implementation, the impact of the Norwalk HCEs on patient LOS and C/C was evaluated. Concurrently, internal medicine residents completed a written anonymous survey to assess the value of the HCEs on both inpatient resource utilization and residency education.
Setting
The Norwalk Hospital is a 250-bed, university-affiliated community teaching hospital in an urban center of southwest Connecticut. It is the only hospital in Norwalk and provides the great majority of inpatient care for the 200,000 regional inhabitants. Norwalk Hospital is a level II trauma center with a cardiac catheterization lab. There are over 3,000 medical admissions per year. Patients admitted are 77% white, 12% black, and 9% Hispanic with a wide social and economic spectrum.
Internal Medicine Residency
Medical house staff during 1999 to 2000 consisted of 36 categorical residents, 4 preliminary residents, and 2 chief residents. All residents rotated on the inpatient service over the course of a year (PGY1, 4.5 months; PGY2, 3 months; PGY3, 2 months). There were 4 resident teams who rotated call on a daily basis.
Resident Supervision and Teaching Before Implementation of the HCE System
Approximately 75% of admitted patients had a local primary care physician and 25% were either indigent or had a physician who did not admit to the Norwalk Hospital. Of patients with a physician associated with the Norwalk Hospital, two-thirds were admitted to the teaching service. Admission to the resident service was determined by the patient's complexity, educational value, and the availability of space on the house staff teams (dictated by predetermined admission caps). Residents were expected to perform a comprehensive history and physical examination on patients admitted under their care, develop a diagnostic and therapeutic plan, and participate in key patient management decisions with daily supervision provided by the patient's primary care physician. Residents were generally uninvolved with the one-third of patients admitted to the nonteaching service unless the patient became unstable, in which case they could be reevaluated for possible transfer to one of the resident teams.
Before implementation of the HCE program, inpatient care for indigent patients or those without a primary care physician with admitting privileges was divided among 150 community physicians who rotated call on a daily basis. Because these patients were usually unknown to the admitting attending and often complex, such patients were always admitted to the teaching service. Resident responsibilities were the same as described above. Supervision was provided by the admitting attending throughout the patient's hospital course. Pulmonary/critical care specialists and cardiologists generally provided attending level care and supervision for patients admitted to the intensive care unit and coronary care unit, respectively. Upon discharge, these patients would usually follow up at a hospital-based, resident clinic supervised by a small number of dedicated, full-time outpatient faculty.
In addition to their supervisory roles, community physicians also supplied the majority of inpatient teaching, both formal and informal, for the residency program. Community physicians, along with a small number of full-time faculty, served as instructors for formal resident-teaching rounds on a voluntary basis. Bedside teaching and physical examination skills were provided as time permitted. Over the past decade, however, economic and time constraints had limited the ability of the private physician to provide effective resident education on a consistent basis.
Resident Supervision and Teaching After Implementation of the HCE System
Patients with primary care physicians with privileges at Norwalk Hospital were handled in the same manner as before. For indigent patients and those without a physician affiliated with Norwalk, the HCEs assumed the role of inpatient attending physicians. Each HCE was assigned to and admitted with 2 of the 4 resident teams. Resident responsibilities for patients were unchanged. The system was established so as to give all resident teams equal exposure to the HCEs and still allow residents to interact with community physicians in a meaningful way. Intensive care unit and coronary care unit patients continued to be admitted by pulmonary/critical care specialists and cardiologists.
Discharge follow-up for indigent patients changed dramatically 5 months prior to the start of the HCE system. A new major ambulatory teaching site, the Norwalk Community Health Center, replaced the hospital-based resident clinics. This federally qualified community health center was created through a partnership among local community groups, the Norwalk Department of Public Health, and the Norwalk Hospital, which provides substantial ongoing fiscal support.9 The internal medicine residents and their supervising physicians provide all internal medicine care. Patients admitted to Norwalk Hospital on the HCE service were followed after discharge at the health center, usually with a resident who managed their inpatient care. When inpatient care was required, patients of the health center were admitted to the HCE service.
In addition to clinical responsibilities, the HCEs had a large educational role with internal medicine house officers and medical students. HCEs were to provide bedside teaching and physical examination skills for both their own patients and those of the community physicians. Each HCE was to act as the teaching attending for one resident team, while other full-time faculty and a reduced number of community physicians served as teaching attendings for the other two teams. A complete list of HCE roles is provided in Table 1.
Table 1.
Clinical and Educational Responsibilities of Hospitalist Clinician Educators
| Clinical |
| Average number of patients on service: 8 to 12 per attending |
| Average number of admissions per 24-hour period: 2 to 6 patients |
| Patient care population |
| Self-pay, Medicaid, Medicare, few with private insurance (many indigent patients followed at Norwalk Community Health Center) |
| Voluntary hospitalist service for private attendings (<3% chose to utilize) |
| Weekly supervision at Norwalk Community Health Center (Ambulatory Teaching Site) |
| Educational |
| Attending rounds/morning report/journal club |
| Weekly intern tutorials |
| Medical student tutorials |
| Monthly conferences |
| Medical jeopardy |
| Evidence-based medicine |
| Medical consultation curriculum |
| Medical informatics weekly sessions |
| Administrative committees |
| Residency mentoring |
| Residency recruitment |
Resource Utilization
Analysis of LOS/ C/C.
Data were analyzed retroactively by the Norwalk Hospital Finance Department using a hospital-based computer program. Neither HCEs nor community physicians were aware that it was being collected. The data did not become available to providers until the time of this analysis. All primary discharge diagnosis related groups (DRG) for which the HCEs had at least 10 admissions for fiscal year 2000 were included in the analysis. For each DRG, LOS and cost per case were calculated and compared to aggregate data from patients with the same discharge DRG who had been admitted by private, nonhospitalist physicians during the same fiscal year whether or not they had house staff coverage. Patients with primary care physicians who elected to have their patients admitted to the HCEs were included in the HCE data, though this number was relatively small (<3%).
For each patient admission, LOS, total C/C, and direct C/C were determined. Length of stay is the integer difference between date of patient admission and date of discharge. Total costs include all salary and nonsalary expenses accounted to the patient encounters under analysis. Direct costs represent total costs minus specific overhead and indirect costs allocated to patient encounters by the financial systems. Cost per case is calculated as the sum of the total (or direct) costs for each sample, divided by the number of patients in the sample. We excluded from analysis those patients for whom total LOS exceeded Medicare thresholds (extreme outliers were excluded from all analyses) and patients who had initially been admitted to either the Intensive Care Unit or Critical Care Unit. For both samples, we obtained overall total C/C, direct C/C, and average length of stay (ALOS), and used the Student's t test for distributions of unequal variance in order to gauge the statistical significance of the difference between the two samples. When, after the ninth most common diagnosis, there were two diagnoses with the exact same number of admissions, both of these were included in analysis. Thirty-day hospital readmission rates were also calculated for both the HCEs and community physicians.
Resident Survey
An 18-question written survey was developed by members of the full-time faculty and mailed to all categorical medicine residents (N = 36) at the end of the HCEs’ first year to be returned anonymously to the residency registrar. All second- and third-year residents had been extensively exposed to the inpatient service both before and after the implementation of the HCEs. Because the HCE system was not fully operational until their fourth month, the first-year residents also had enough perspective to complete the questionnaire. The survey elements were those previously noted to be most important for resident satisfaction.8 Specifically, the survey assessed HCEs’ impact on educational environment, quality of patient care, and patient interaction, as well as resident autonomy. Residents were also asked to assess changes in their own clinical behavior. Questions about the educational environment and quality of care were rated on a 5-point Likert scale. Questions relating to patient interactions, resident autonomy, and behaviors were rated as “increased,”“decreased,” or “unchanged” by the presence of HCEs. The questions used were derived from standardized attending evaluation forms such as those supplied by the American Board of Internal Medicine and are similar to those from other studies exploring the impact of hospitalists on resident education.2,8
RESULTS
One year after the initiation of an HCE system, substantial improvements in ALOS and C/C were achieved by HCEs when compared to performance by private, community-based physicians. Residents reported improved education with high degrees of satisfaction with the HCE system.
Resource Utilization
Length of Stay/Cost per Case
Thirty-two primary discharge DRGs for which the HCEs had at least 10 admissions during fiscal year 2000 were identified. These DRGs included a total of 2,707 admissions with 583 cases (21.5%) admitted to the hospitalist service. Compared to private physicians, the HCEs demonstrated an average 20.8% decrease in LOS and an average 18.4% decrease in C/C, or approximately $500 per admission. Based upon these 583 admissions for fiscal year 2000, a total cost savings of approximately $300,000 was achieved in the first year of the HCE program.
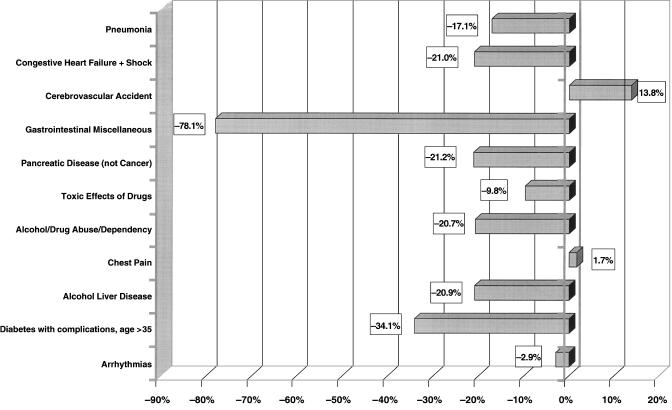
When the top 11 most common discharge DRGs were examined, substantial reductions in LOS and C/C were documented between HCEs and community-based attending physicians for most diagnoses (Table 2; Figs. 1 and 2). Reductions in LOS of 1 day or greater were achieved for the diagnoses of congestive heart failure (DRG 127), cardiac arrhythmias (138), alcohol/drug abuse or dependency or detoxification (434), diabetes with complications (294), cirrhosis and alcoholic hepatitis (202), and esophagitis, gastroenteritis, and miscellaneous diagnosis (182) (which includes esophagitis and gastroenteritis, to be subsequently referred to as GI Misc) (Fig. 1). In contrast, cerebrovascular accident (DRG 14) was the only discharge diagnosis of the 11 most common where community-based attendings had a statistically significant shorter LOS than HCEs.
Table 2.
Total Number of Patients Seen by HCEs Versus Private Physicians in Fiscal Year 2000 Grouped by the Top 11 DRGs
| Number of Patients | |||
|---|---|---|---|
| DRG | HCE | Community Internists | |
| 89 | Simple pneumonia & pleurisy age >17 with complications | 46 | 241 |
| 127 | Heart failure & shock | 44 | 374 |
| 14 | Specific cerebrovascular disorders except transient ischemic attack | 40 | 191 |
| 182 | Esophagitis, gastroenteritis, & misc digestive disorders age >17 with complications | 35 | 142 |
| 204 | Disorders of pancreas except malignancy | 33 | 62 |
| 449 | Poisoning & toxic effects of drugs age >17 with complications | 30 | 49 |
| 434 | Alcohol/drug abuse or depend, detox, or other symptoms treat with complications | 21 | 69 |
| 143 | Chest pain | 21 | 87 |
| 202 | Cirrhosis & alcoholic hepatitis | 20 | 25 |
| 138 | Cardiac arrhythmia & conduction disorders with complications | 19 | 129 |
| 294 | Diabetes age >35 with complications | 19 | 31 |
HCE, hospitalist clinician educator; DRG, diagnosis related group.
FIGURE 1.
Length of stay by diagnosis related group: hospitalist clinician educators versus private physicians for fiscal year 2000. In descending order of prevalence, the bars represent percentage increases or decreases in length of stay for HCEs as compared to private physicians (P = .002). Diagnosis related group for pneumonia = 89, congestive heart failure + shock = 127, cerebrovascular accident = 14, gastrointestinal miscellaneous = 182, pancreatic diseases (not cancer) = 204, toxic effects of drugs = 449, alcohol/drug abuse/dependency = 434, chest pain = 143, alcohol liver disease = 202, diabetes with complications (age >35), arrhythmias = 138.
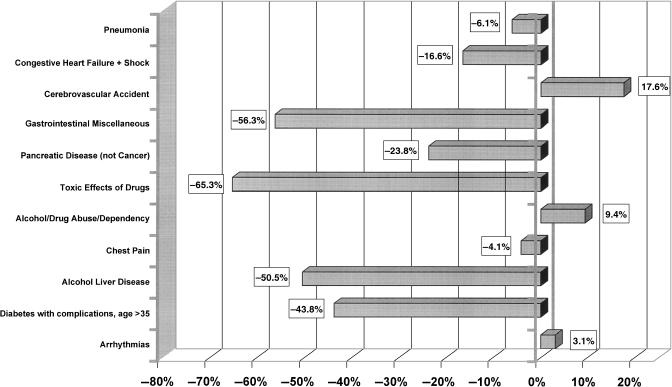
FIGURE 2.
Cost per case by diagnosis related group: hospitalist clinician educators versus all other MDs for fiscal year 2000. In descending order of prevalence, the bars represent the relative percentage increases or decreases in cost per case for the HCEs as compared to the private physicians (P = .01). Diagnosis related group for pneumonia = 89, congestive heart failure + shock = 127, cerebrovascular accident = 14, gastrointestinal miscellaneous = 182, pancreatic diseases (not cancer) = 204, toxic effects of drugs = 449, alcohol/drug abuse/dependency = 434, chest pain = 143, alcohol liver disease = 202, diabetes with complications (age >35), arrhythmias = 138.
Similar trends were noted when the individual top 11 most common discharge DRGs were analyzed for C/C. Reductions in C/C of $500 or more were noted for the diagnoses of congestive heart failure (DRG 127), GI Misc (182), pancreatic disorders except malignancy (204), and poisoning and toxic effects of drugs (449). Reductions of $1,000 or greater were demonstrated for the diagnoses of diabetes with complications age >35 (294) and cirrhosis and alcoholic hepatitis (202). The only DRGs where HCEs had a significantly higher C/C were cerebrovascular accident (14) and alcohol/drug abuse dependency, detoxification, or other (434) (Fig. 2).
Readmission rates were also assessed. For the HCEs, the 30-day readmission rate was 7.5%, while for community-based physicians the rate was 11.1% (P < .001).
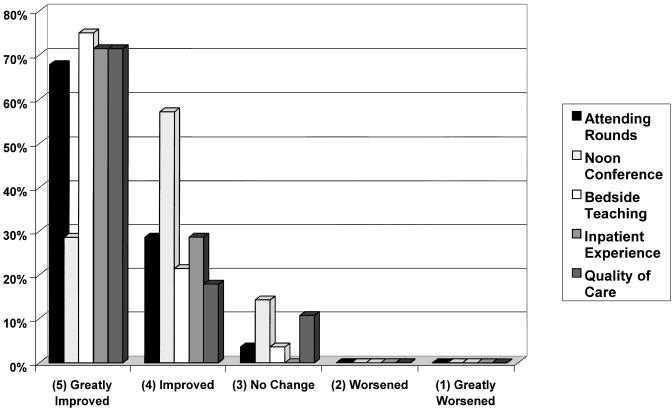
Resident Education
The return rate of the anonymous resident survey was 78%. Overall, the implementation of an HCE system had a positive impact on residents’ perception of their inpatient educational experience. Of the respondents, 97% reported that the presence of HCEs “improved” or “greatly improved” formal and informal teaching including bedside rounds, attending rounds, and didactic conferences. The majority also noted improved medical care for indigent and unassigned patients (Figs. 3 and 4).
FIGURE 3.
Resident perception of hospitalist clinician educators’ impact on educational activities. Residents were asked to assess the effect of HCEs on several parameters of their inpatient experience on a 5-point Likert scale.
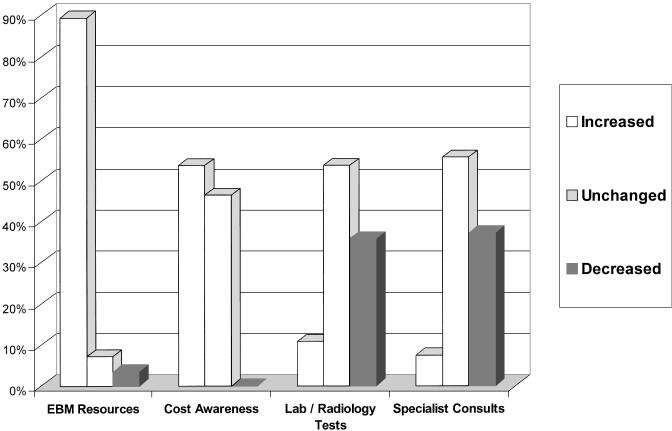
FIGURE 4.
Resident perception of hospitalist clinician educators’ impact on resource utilization. Residents were asked whether use of evidence-based medicine, cost awareness, ancillary studies (labs, X-rays), and subspecialty consults was “increased,”“unchanged,” or “decreased” by the presence of HCEs. Percentages of each response are shown above.
Medical house staff also perceived changes in their own behavior during the first year of the HCE program. Almost 90% of respondents agreed that the presence of HCEs encouraged their use of evidence-based medicine (EBM) resources and over half noted an increased awareness of hospitalization costs. Somewhat unexpectedly, despite the demonstrated difference in C/C, only a minority of residents reported that they were ordering fewer consults or ancillary tests on hospitalist versus nonhospitalist patients (Fig. 4).
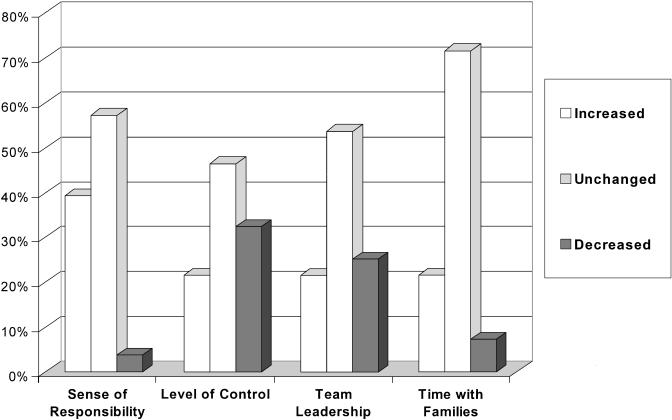
The influence of hospitalists on resident autonomy and patient interaction was also assessed. Before implementation, residents informally expressed concern that the addition of hospitalists might interfere with resident leadership and teaching responsibilities. However, after a year, 75% of respondents noted that their roles as team leaders were either increased or unchanged, and only 25% felt less independent since the advent of the hospitalist system (Fig. 5). As a whole, 100% of respondents preferred the new HCE system to the prior arrangement.
FIGURE 5.
Resident perception of hospitalist clinician educators’ impact on resident behavior. Residents were asked whether their sense of responsibility, level of control, team leadership, and time spent with families was “increased,”“unchanged,” or “decreased” by the presence of HCEs. Results are shown by percentage for each response.
DISCUSSION
In a recent review of hospitalist medicine, Wachter and Goldman suggested that the hospitalist model should be judged on cost, quality, education, and patient satisfaction.1 There is little published about hospitalists affecting financial outcomes while concurrently affecting resident education. This prompted an editorial regarding two recently published articles on hospitalists10,11 that stated that although “residents were an integral part of care for all patients in both studies, neither study tells us much about how attendings and house staff interacted.”12 In our study, we have demonstrated that HCEs have substantial positive impacts on both clinical efficiency and resident education in a mid-sized academic community teaching hospital.
Resource Utilization: Patient Outcomes Including Length of Stay and Cost per Case
Reductions in LOS and C/C were significant for several diagnoses and comparable to reductions seen in other studies.2,13 Because these conditions require reevaluation and active management, they may be especially responsive to hospitalist care. We hypothesize that HCEs were also more aggressive in ordering appropriate tests early and that they were more intimately involved in the case management process than community physicians. Though not formally studied, discussions with our case managers indicated that both hypotheses are probably true (personal correspondence with Anna Brooks, Director of Case Management). On the other hand, should patients deteriorate, the onsite presence of hospitalists allows patients to be evaluated by an attending physician more promptly and efficiently. This facilitates both the early implementation of necessary consultations and therapeutic interventions including transfer to the intensive care unit or coronary care unit.
In contrast with the majority of DRGs at Norwalk Hospital, the HCEs were significantly less effective compared with private physicians for cerebrovascular accident. This may be related to insurance coverage and discharge planning for extended care. Our faculty care for many indigent patients, who do not have the financial resources to move quickly into rehabilitation units or extended care facilities. Thus, even with the prompt evaluation and workup by HCEs, discharge planning was complicated by financial considerations.
Based on our data and almost 600 HCE admissions, we calculate a cost savings to the hospital of almost $300,000 in the year 2000, at least some of which was directed back into the residency and hospitalist programs. In fact, because of the financial benefits achieved by the HCE system, our residency and hospitalist programs have both expanded significantly.
Given the fact that thousands of residents and students are trained at community hospitals each year, demonstrating the educational value of hospitalists in these settings is vital. We have shown that HCEs greatly enhanced the inpatient experience for our internal medicine residents and had a positive effect on their behavior, particularly in influencing resident use of EBM resources and increasing their awareness of costs. As found in prior studies,2 hospitalists did not affect residents’ ordering of tests or consults.
These educational benefits did not come at the expense of an adverse effect on resident roles as teachers or leaders. Though concerns about declines in resident autonomy are commonly cited when discussing hospitalist models, most data show that this is not a major issue.2,8,14–16 At our program where interactions between hospitalists and residents occur at an intimate level, one could posit that the risk of residents losing their autonomy would be greater. We have shown, however, that this fear is not realized, as the majority of residents indicated that their roles as leaders and teachers were either increased or unchanged.
From an educational standpoint, the presence of HCEs has resulted in qualitative changes in our program as well. The hospitalists have developed several innovative educational programs including an EBM curriculum, a monthly medical jeopardy conference to enhance board preparation, a required month in consultative medicine, and most recently, a hospitalist elective. This latter elective provides residents with an opportunity to work with hospitalists on an individual basis with a focus on end-of-life discussions and care, quality measurement, cost containment, and hospital billing. These areas are generally underemphasized in resident training but considered important, particularly for those considering a career in hospitalist medicine.17,18
Hospitalist clinician educators have been instrumental in helping our residents fulfill the latest Accreditation Council for Graduate Medical Education requirements, particularly those that focus on “system-based learning.”19 Under the guidance of HCEs, our residents have become involved in a number of multidisciplinary committees focused on specific inpatient issues. One of these is a core measures improvement project committee, which creates systems to improve quality outcomes in specific diagnoses including congestive heart failure, myocardial infarction, and pneumonia.20 Residents have also actively participated in multidisciplinary hospital committees such as the patient care and evaluation committee, which focuses on inpatient quality of care, as well as the pain, ethics, and Institutional Review Board committees. Residents have presented aspects of these activities at regional meetings.21
There are several limitations to our study. The use of DRG data, though easiest to obtain, is subject to error by nonphysician coders, resulting in patients of hospitalists and nonhospitalists being misclassified in terms of their primary discharge diagnosis and/or comorbidities. However, given the large number of patients included in our study, and the strongly positive LOS and cost data favoring hospitalists, it is unlikely that such misclassifications would result in significant alterations of the data.
Another weakness of our study is that we did not make adjustments for patient complexity beyond the primary discharge DRG. Again, given that a large portion of the hospitalists’ patients in our study were indigent, a group that tends to present later and in more severe stages of disease processes, we can only assume that if adjustments for complexity were made, our data would favor the hospitalists even more. Discharge planning problems and their impact on LOS was not explored.
We also did not look specifically at quality of care issues. One might posit that though HCEs reduced LOS and costs, perhaps they did so at the expense of quality of care. This point is refuted somewhat by the fact that HCE 30-day readmission rates (7.5%) were actually better than those of community physicians (11.1%). This indicates that HCEs were probably not prematurely discharging patients in order to save hospital days and cut costs. Future investigations will focus on the quality of care delivered by our HCEs in more detail.
With respect to the resident survey, it was a retrospective questionnaire completed about 1 year after implementation of the HCE system. Thus, residents may have overestimated the impact of the HCEs due to recall bias.
A final weakness of our study was that it included a relatively small number of hospitalists (N = 2), who were trained at large, university-based medical centers where inpatient medicine is heavily emphasized. Whether similar success can be obtained with other hospitalists remains to be determined.
CONCLUSION
We have demonstrated that hospitalist clinician educators in an academic, community teaching hospital reduced length of stay and cost per case while improving the educational experience of internal medicine residents. These results support the use of hospitalist clinician educators in community-based teaching hospitals.
REFERENCES
- 1.Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487–94. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- 2.Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service. Impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–5. doi: 10.1001/jama.279.19.1560. [DOI] [PubMed] [Google Scholar]
- 3.Halpert AP, Pearson SD, LeWine HE, McLean SC. The impact of an inpatient physician program on quality, utilization and satisfaction. Am J Manag Care. 2000;6:549–55. [PubMed] [Google Scholar]
- 4.Feese RB. Clinical, logistical and political issues in creating a hospitalist system. Ann Intern Med. 1999;130:350–4. doi: 10.7326/0003-4819-130-4-199902161-00004. [DOI] [PubMed] [Google Scholar]
- 5.Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes and patient satisfaction in a rural health system. Am J Med. 2000;108:621–6. doi: 10.1016/s0002-9343(00)00362-4. [DOI] [PubMed] [Google Scholar]
- 6.Hackner D, Tu G, Braunstein GD, et al. The value of a hospitalist service: efficient care for the aging population? Chest. 2001;119:580–9. doi: 10.1378/chest.119.2.580. [DOI] [PubMed] [Google Scholar]
- 7.Whitcomb WF, Nelson JR. The role of hospitalists in medical education. Am J Med. 1999;107:305–9. doi: 10.1016/s0002-9343(99)00234-x. [DOI] [PubMed] [Google Scholar]
- 8.Chung P, Morrison JU, Jin Lei Levinson W, Humphrey H, Meltzer D. Resident satisfaction on an academic medical service: time to teach. Am J Med. 2002;112:597–601. doi: 10.1016/s0002-9343(02)01155-5. [DOI] [PubMed] [Google Scholar]
- 9.Mazur EM, Cleary JP, Pols KB, et al. Collaboration between an internal medicine residency program and a federally qualified health center. Norwalk Hospital and the Norwalk Community Health Center. Acad Med. 2000;76:1159–64. doi: 10.1097/00001888-200111000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Auerbach AD, Wachter RM, Katz P, et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859–65. doi: 10.7326/0003-4819-137-11-200212030-00006. [DOI] [PubMed] [Google Scholar]
- 11.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic medical service: results of a trial of hospitalists. Ann Intern Med. 2002;137:866–74. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 12.Editorial. The who, what, when, where, whom, and how of hospitalist care. Ann Intern Med. 2002;137:930–1. doi: 10.7326/0003-4819-137-11-200212030-00015. [DOI] [PubMed] [Google Scholar]
- 13.Davis KM, Koch KE, Harvey JK, Wilson R, Englert J, Gerard P. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med. 2000;108:621–6. doi: 10.1016/s0002-9343(00)00362-4. [DOI] [PubMed] [Google Scholar]
- 14.Goldman L. The impact of hospitalists on medical education and the academic health system. Ann Intern Med. 1999;130:364–7. doi: 10.7326/0003-4819-130-4-199902161-00007. [DOI] [PubMed] [Google Scholar]
- 15.Brown MD, Halpert A, McKean S, Sussman A, Dzau VJ. Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School. Am J Med. 1999;106:134–7. [PubMed] [Google Scholar]
- 16.Hauer KE, Wachter RM. Implication of the hospitalist model for medical students’ education. Acad Med. 2001;76:324–9. doi: 10.1097/00001888-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Wachter RM. An introduction to the hospitalist model. Ann Intern Med. 1999;130:338–42. doi: 10.7326/0003-4819-130-4-199902161-00002. [DOI] [PubMed] [Google Scholar]
- 18.Plauth WH, Pantilat SZ, Wachter RM, Fenton CL. Hospitalists’ perception of their residency training needs: results of a national survey. Am J Med. 111:60–6. doi: 10.1016/s0002-9343(01)00837-3. [DOI] [PubMed] [Google Scholar]
- 19.Accreditation Council for Graduate Medical Education. ACGME Outcome Project: General Competencies. ACGME website. Available at: http://www.acgme.org. Accessed January 2003.
- 20.Meehan TP, Weingarten SR, Holmboe ES, et al. A statewide initiative to improve the care of hospitalized pneumonia patients: The Connecticut Pneumonia Pathway Project. Am J Med. 2001;111:203–10. doi: 10.1016/s0002-9343(01)00803-8. [DOI] [PubMed] [Google Scholar]
- 21.Kasbari S, Bain M, Charney P. Resident Pain Assessment and Management on the Medicine Inpatient Service. Presented at Connecticut State ACP meeting, September, 2002.