Abstract
OBJECTIVE
To investigate the effects of exclusively physical presentation of depression on 1) depression management and outcomes under usual care conditions, and 2) the impact of an intervention to improve management and outcomes.
DESIGN AND SETTING
Secondary analysis of a depression intervention trial in 12 community-based primary care practices.
PARTICIPANTS
Two hundred adults beginning a new treatment episode for depression.
MEASUREMENTS
Presenting complaint and physician depression query at index visit; antidepressant use, completion of adequate antidepressant trial, change in depressive symptoms, and physical and emotional role functioning at 6 months.
MAIN RESULTS
Sixty-six percent of depressed patients presented exclusively with physical symptoms. Under usual care conditions, psychological presenters were more likely than physical presenters to complete an adequate trial of antidepressant treatment but experienced equivalent improvements in depressive severity and role functioning. In patients presenting exclusively with physical symptoms, the intervention significantly improved physician query (40.8% vs 18.0%;P = .06), receipt of any antidepressant (63.0% vs 20.1%; P = .001), and an adequate antidepressant trial (34.9% vs 5.9%; P = .004), but did not significantly improve depression severity or role functioning. In patients presenting with psychological symptoms, the intervention significantly improved receipt of any antidepressant (79.9% vs 38.0%; P = .01) and an adequate anti(40.8% vs 18.0%;P = .06), receipt of any antidepressant and an adequate antidepressant trial (34.9% vs 5.9%; P = .004), and also improved depression severity and emotional role functioning.
CONCLUSIONS
Our results suggest that there is a differential intervention effect by presentation style at the index visit. Thus, current interventions should be targeted at psychological presenters and new approaches should be developed for physical presenters.
Keywords: depressive disorder, affective symptoms, moderator variables, somatoform disorders
Investigators have long recognized that the majority of depressed primary care patients across different cultures and socioeconomic strata present exclusively with physical symptoms, 1–11 which they do not attribute to psychological etiologies. Previous research provides some evidence that presentation with physical symptoms creates barriers to depression recognition 12–15 and treatment initiation.16 Little is known about the degree to which quality improvement interventions for depression reduce the risk for poor management and outcomes when depressed patients present with physical symptoms. In this study, we use prospective trial data 17 to explore the effect of physical presentation on depression management and outcomes in usual care, as well as evaluate the differential effect of a quality improvement intervention for patients presenting with physical versus psychological symptoms at their index visit.
We hypothesized that exclusive presentation with physical symptoms at the index visit would be associated with lower quality management and less clinical improvement over 6 months in usual care. Further, we hypothesized that an intervention to systematically improve the management of depression would differentially benefit patients presenting exclusively with physical symptoms compared to patients presenting with psychological symptoms at the index visit.
METHODS
Design, Setting, and Participants
We conducted a secondary analysis of data from the Quality Enhancement by Strategic Teaming (QuEST) project, described previously 17,18 and summarized here. The study was conducted in 12 geographically diverse community primary care practices located across 10 U.S. states. The practices served patients with a variety of managed care and fee-for-service health plans, as well as uninsured patients, and none employed onsite mental health professionals to treat depression. The study used a stratified blocking procedure 18 to match the participating practices into 6 pairs according to their baseline depression treatment patterns, and then the 2 matched practices were randomly assigned to usual care or to the enhanced care intervention.18 Two physicians from each enhanced and usual care practice participated in the study (N= 24 physicians); 23 (96%) were family medicine physicians and the other was trained in internal medicine and pediatrics. Human subjects approval was obtained from the Human Research Advisory Committee of the University of Arkansas for Medical Sciences and the Colorado Multi-institutional Review Board prior to the study.
Patient Eligibility Criteria
Patients presenting for routine care at the participating practices between April 1996 and September 1997 completed a two-stage screening questionnaire, which identified patients reporting at least 5 of the 9 criteria for major depression listed in the Diagnostic and Statistical Manual of Mental Disorders—Third Edition Revised(DSM-III-R) in the previous 2 weeks, as measured by the Inventory to Diagnose Depression (IDD).19 We excluded patients who met criteria for bereavement, mania, alcohol dependence, pregnancy or the postpartum period, life-threatening physical illness, patients who did not intend to use the clinic as their usual source of care during the year after the index visit, patients without telephone access, patients who were illiterate in English, and patients who were cognitively impaired.18 In order to examine the effects of presentation style at the index visit on acute phase depression management, we selected patients beginning a new treatment episode for depression for our analysis. Patients were characterized as beginning a new depression treatment episode if they reported that they had not taken antidepressant medication in the past month or made one or more specialty care visits in the past 6 months.17 Administrative staff from enhanced and usual care practices screened and recruited 211 subjects meeting study criteria before patients saw the doctor at the index visit.17,18 Complete medical records with documentation of presenting complaint at the index visit were obtained for 200 patients (95%); 22 patients (11.1% of the study sample) were lost to 6-month follow-up, leaving 178 patients for longitudinal analysis of depression treatment and outcomes over 6 months. No significant differences in 6-month attrition were observed between depressed patients presenting exclusively with physical symptoms at the index visit compared to those presenting with psychological symptoms (12.9% vs 7.4%, respectively; P = .24).
Intervention
Physicians in enhanced care practices received a notice on the patient's chart that the patient had screened positive for depression, and physicians agreeing with the diagnosis asked patients to schedule a return visit within 1 week to meet with the physician and a nurse care manager. Nurse care managers reassessed each patient's depression, explained treatment options and asked about treatment preferences, asked patients to complete exercises to increase/maintain their readiness to engage in active treatment, and arranged weekly follow-up contacts with the patient over the course of 6 to 8 weeks. Usual care physicians were not informed of patients’ screening results or which patients were participating in the study, nor did usual care nurses meet with depressed patients.18
Data Collection
Each enrolled patient participated in structured telephone interviews administered by a trained research interviewer during the week following the index visit (baseline), and again at 6 months following the index visit.18 Medical records were reviewed and abstracted by a trained abstractor who was blinded to patient intervention status.
Operational Definition of Major Study Variables
Physical and Psychological Presentation at Index Visit.
Psychological or exclusive physical presentation at the index visit was determined from review of the medical record. Notations of presenting complaints were coded as physical or psychological, and patients were characterized as presenting with physical complaints exclusively or with psychological (with or without physical) complaints, as shown in the Appendix.8 We classified depression symptoms as “psychological” or “physical” according to the Composite International Diagnostic Interview (CIDI) depression module convention.20,21 Problems with appetite, weight gain/loss, muscle tension, palpitations, pounding/accelerated heart rate, sweating, trembling/shaking, shortness of breath/smothering sensations, choking sensation, chest pain/discomfort, nausea/abdominal distress, dizziness/unsteadiness/lightheadedness/faintness, numbness/tingling sensations, and chills/hot flashes were considered physical symptoms unless the medical record clearly reflected that the patient considered the symptom to be psychological in nature. For instance, a participant whose presenting complaints were “headache” and “dizziness” was categorized as presenting with physical symptoms. A patient whose presenting complaints were “fatigue” or “low energy” and “dizziness” was categorized as presenting with psychological complaints, because fatigue was considered a psychological complaint.
A single individual reviewed and abstracted all medical records, using the distinctions described in the Appendix. Twenty percent of medical records were selected at random and were reviewed independently by a second abstractor. Interrater agreement on dichotomized patient presentation was 95% and the κ was 0.89.
Process of Care.
Patient recall of the doctor asking about depression at the index visit was measured by patient report in the baseline interview following the index visit. Completion of an adequate trial of antidepressant medication was measured by patient report at 6-month follow-up that they had taken an antidepressant medication at minimum therapeutic 22 daily doses for a duration of at least 3 months between baseline and 6 months.17 Use of mental health specialists for counseling over the 6-month follow-up period by patients in this sample was too low to accommodate stable analyses (data available from authors on request); thus, process of care analysis for mental health specialty counseling is not presented.
Clinical Outcomes.
Depression symptom severity was measured by a modified 23-item Center for Epidemiologic Studies—Depression scale (mCES-D).23,24 The mCES-D was constructed by removing 7 original CES-D items that did not directly parallel DSM-IV criteria for major depression and adding an additional 10 items to measure DSM-IV criteria not assessed in the original CES-D. The mCES-D scores were standardized to a 100-point scale, with higher scores reflecting greater depression symptom severity. Emotional and physical role functioning were measured with 100-point subscales from the Short Form-36,25 where lower scores indicated greater perceived limitations with usual daily activities in the previous month due to emotional or physical problems.
Covariates.
To control for potential confounding factors, sociodemographic and clinical covariates were collected for each subject at baseline. Baseline covariates included age, gender, minority status (minority vs nonminority) education (high school educated vs not), paid employment (full-/part-time vs not), and marital status (married vs not). Clinical covariates included physical comorbidity (sum of 14 patient-reported comorbidities assessed), bodily pain,25 dysthymia during the past year,26 and acceptability of treatment with antidepressants and/or mental health counseling (4-point Likert scales).18 In addition, baseline emotional role functioning score was added as a clinical covariate in analyses examining depression severity at 6 months, and baseline mCES-D score was added as a clinical covariate in analyses examining emotional role functioning and physical role functioning at 6 months. Due to relatively small sample size for some analyses, covariates were tested in preliminary models and all those with P < .25 were retained in the final model.
Data Analysis
Chi-squares and t tests were used to assess differences in baseline characteristics between patients presenting with physical or psychological symptoms. To assess the effects of presentation style on dichotomous process of care variables, we included all 200 patients in multilevel logistic regression models 27,28 controlling for covariates listed above, which were used to assess and account for potential practice- or physician-level intraclass correlation on the outcome variables we measured. To assess the effects of presentation style on continuous clinical outcomes, we used general linear mixed models 27,29 treating time as a random effect in which repeated measures were nested within patients, and patients were nested within physicians as needed. To determine whether presentation style moderated the effects of the enhanced care intervention for the process of care or clinical outcomes noted above,29 we added an ERDN intervention*presentation style*time interaction term to these models.
RESULTS
Patient Characteristics
At baseline, the 200 subjects from usual and enhanced care had a mean age of 43.4 years, 168 (84.0%) were women, 168 (84.0%) were non-Hispanic white, 94 (47.0%) were currently married, 41 (20.5%) had received less than a high school education, and 127 (63.5%) were employed full- or part-time. Subjects reported 6.4 (SD [standard deviation], 1.3) of the 9 depressive criteria at baseline. Twenty patients (10.0%) met criteria for dysthymia in the previous year, and patients averaged 2.1 (SD, 1.9) baseline physical comorbidities.
Medical record abstraction indicated that 66.0% of participants (132/200) presented exclusively with physical symptoms at the index visit, with no significant differences between enhanced and usual care patients (62.7% vs 70.0%, respectively; P = .28). As Table 1 shows, the 68 psychological presenters were statistically similar to the 132 physical presenters in all sociodemographic and clinical characteristics except that patients presenting with psychological symptoms more often reported that antidepressants were an acceptable treatment for depression (72.1% vs 40.2%, respectively; P= .001). Of particular note, patients presenting with psychological or physical symptoms reported similar pain scores, diminishing the likelihood that severity of pain differentially influenced depression management or outcomes in usual or enhanced care.30,31
Table 1.
Baseline Characteristics of Study Participants, by Presentation Style at Index Visit
| Presentation | |||
|---|---|---|---|
| Characteristics | Physical (N= 132) | Psychological (N= 68) | P Value |
| Mean age, y (SD) | 42.9 (14.4) | 44.4 (15.4) | .51 |
| Women, n(%) | 112 (84.9) | 56 (82.4) | .65 |
| White non-Hispanic, n(%) | 109 (82.6) | 59 (86.8) | .44 |
| Currently married, n(%) | 59 (44.7) | 35 (51.5) | .36 |
| Less than high school education, n(%) | 23 (17.4) | 18 (26.5) | .13 |
| Employed full- or part-time, n(%) | 84 (66.1) | 48 (65.8) | .96 |
| Number of physical comorbidities, mean (SD) | 1.8 (1.9) | 2.2 (1.9) | .22 |
| Number of depression symptoms identified at screening, mean (SD) | 6.6 (1.4) | 6.4 (1.3) | .31 |
| Dysthymia in past year, n(%) | 15 (11.4) | 5 (7.4) | .37 |
| Considers antidepressants an acceptable treatment,n(%) | 53 (40.2) | 49 (72.1) | .001 |
| Considers mental health counseling an acceptable treatment, n(%) | 93 (70.5) | 41 (60.3) | .20 |
| Received intervention, n(%) | 69 (52.3) | 41 (60.3) | .28 |
| Bodily pain, mean (SD) | 48.7 (26.2) | 52.5 (26.6) | .33 |
SD, standard deviation.
Process of Depression Care
Physician Query About Depression at Index Visit.
Under usual care conditions, patients who presented exclusively with physical symptoms were less likely to report that the physician had asked them about depression than those presenting with psychological symptoms (18.0% vs 80.2%; P < .001). The interaction terms indicated that the enhanced care intervention differentially affected physician query in patients presenting with physical versus psychological symptoms (P = .012). The intervention tended to increase physician query about depression in physically presenting patients (40.8% vs 18.0%; P = .06), but had no effect in psychologically presenting patients (61.0% vs 80.2%; P = .23) (see Fig. 1).
FIGURE 1.
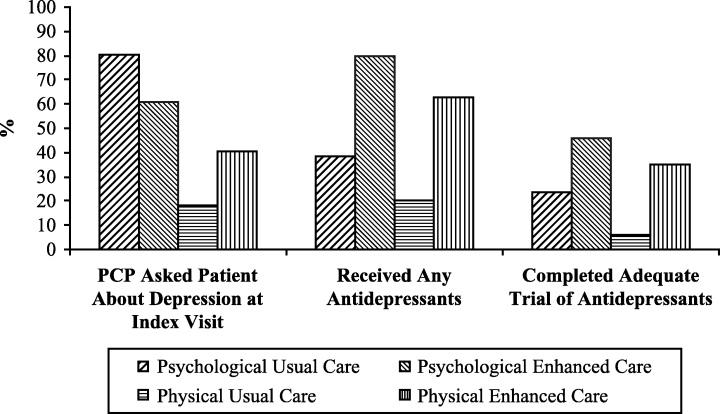
Depression treatment by presentation style at index visit and intervention status.
Any Antidepressant.
Under usual care conditions, patients presenting with physical symptoms were not significantly less likely than patients presenting with psychological symptoms to use antidepressants in the 6 months following the index visit (20.0% vs 38.0%; P= .11). Overall, the intervention significantly improved antidepressant use (P < .01) and the interaction term indicated that the intervention effect on any antidepressant use was similar for physically presenting and psychologically presenting patients (P = .93). Among physically presenting patients, 63.0% of enhanced care patients reported use of any antidepressant between baseline and 6 months, compared to only 20.0% of usual care patients (P = .001). Among psychologically presenting patients, 79.9% of enhanced care patients reported taking an antidepressant between baseline and 6 months, compared to 38.0% of their usual care counterparts (P = .01) (see Fig. 1).
Adequate Trial of Antidepressants.
Under usual care conditions, patients presenting with physical symptoms were significantly less likely to complete an adequate antidepressant trial over 6 months than those presenting with psychological symptoms (5.9% vs 23.8%; P = .04). Overall, the intervention increased the likelihood that patients would complete an adequate trial of antidepressants (P < .01) and the interaction term indicated that the intervention had a similar effect on adequate trial of antidepressants for patients presenting with physical versus psychological symptoms (P = .17) (see Fig. 1).
Among patients presenting with physical symptoms, 34.8% of enhanced care patients reported completing an adequate antidepressant trial between baseline and 6 months, compared to only 5.9% of usual care patients (P = .04). Among patients presenting with psychological symptoms, 46.0% of enhanced care patients reported completing an adequate antidepressant trial between baseline and 6 months, compared to 23.8% of their usual care counterparts (P = .14).
Clinical Outcomes
Depression Symptom Severity.
The model indicated that under usual care, patients presenting with physical symptoms experienced similar improvement in depression severity over 6 months to patients presenting with psychological symptoms (12.7- vs 15.5-point decline; P = .63). The three-way interaction term indicated that the intervention had a differential effect on depression severity in patients presenting with physical versus psychological symptoms (P < .001). Among physically presenting patients, enhanced care patients reported comparable improvement in severity compared to usual care patients (16.0- vs 12.9-point decline; P = .48). Among psychologically presenting patients, enhanced care patients reported a significantly greater improvement in severity compared to usual care patients (28.2- vs 15.4-point decline; P = .04) (see Fig. 2).
FIGURE 2.
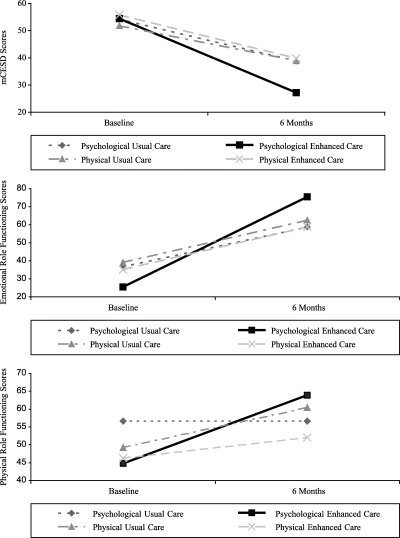
Depression symptom severity and emotional and physical role functioning outcomes at 6 months, by presentation style at index visit and intervention status.
Emotional Role Functioning.
The model indicated that under usual care, patients presenting with physical symptoms experienced comparable improvement in emotional role functioning over 6 months compared to those presenting with psychological symptoms (23.8- vs 22.2-point increase; P = .89). The three-way interaction term indicated that the intervention had differential effects on emotional role functioning in patients presenting with physical compared to psychological symptoms (P < .01). Among physically presenting patients, enhanced care patients reported comparable change in emotional role functioning compared to usual care patients (23.8- vs 23.6-point increase; P = .97). Among psychologically presenting patients, enhanced care patients reported a significantly greater improvement in emotional role functioning compared to usual care patients (48.0- vs 22.2-point increase; P = .03) (see Fig. 2).
Physical Role Functioning.
The model indicated that under usual care, patients presenting with physical and psychological symptoms experienced similar change in physical role functioning over 6 months (11.2- vs 0.0-point increase; P = .20). The three-way interaction term indicated that the intervention had differential effects on physical role functioning in patients presenting with physical compared to psychological symptoms (P < .01). Among physically presenting patients, enhanced care patients reported comparable change in physical role functioning compared to usual care patients (5.9- vs 11.2-point increase; P = .43). Among psychologically presenting patients, enhanced care patients reported a significantly greater improvement in physical role functioning compared to usual care patients (19.0- vs 0.0-point increase; P = .04) (see Fig. 2).
DISCUSSION
Sixty-six percent of depressed patients presented exclusively physical symptoms at the index visit. Under usual care conditions, psychological presenters were more likely than physical presenters to be asked about depression at the index visit and to complete an adequate trial of antidepressant treatment, but physical and psychological presenters experienced equivalent improvements in depressive severity and role functioning. In patients presenting with exclusively physical symptoms, the intervention improved physician query and antidepressant medication management but did not improve symptoms or functioning. In patients presenting with psychological symptoms, the intervention did not improve physician query but did improve antidepressant medication management comparably to physical presenters, and also improved symptoms and functioning.
These results are consistent with previous findings that most patients present with physical symptoms.32,33 Somatic presentation has been shown to be associated with lower rates of depression recognition and treatment,32,34,35 although many patients with depression will acknowledge psychological symptoms if asked about them.36,37 Consistent with this study's usual care findings, recognition of depression in patients presenting with physical symptoms often suffers because treating physicians misattribute multiple, ill-defined, somatic complaints accompanying depression 3,11,13,38,39 to nonpsychological etiologies.32 Thus, it is important to note that the intervention was successful in encouraging primary care physicians to inquire about depression in almost half of depressed patients presenting with physical symptoms.18
However, the intervention's failure to improve outcomes in depressed patients presenting with physical symptoms, even while increasing their likelihood of completing an adequate antidepressant trial, appears to contradict previous studies demonstrating a positive relationship between antidepressant adequacy and clinical outcomes.40,41 To achieve acceptable outcomes,42 patients with physical presentations may require increased pharmacotherapy doses, duration, and/or different drugs,43 or specific psychotherapy.42,44–46
In our analysis, physical presenters did not have more physical comorbidities than psychological presenters,13 but may have greater health concerns about their comorbidities,47 which may negatively affect depression management.47,48 Physical presentation may reflect underlying somatoform syndromes, and evidence suggests that antidepressant treatment has only moderate success with somatoform syndromes.16,49–52 Somatizing is common among depressed primary care patients, with up to 50% of patients characterized by significantly elevated levels of unexplained symptoms.32,53,54 A limited number of studies following both depression and physical symptoms have noted minimal correlation between physical symptom and depression responses.52,55,56
Similar to depressed primary care patients’ general preference for counseling,5770% of the depressed primary care patients with physical presentation in our study were receptive to mental health counseling. Because matching treatment to patient preferences may improve outcomes 58 in general, modalities such as problem-solving therapy 45 and cognitive-behavioral therapy 44 may have similar effectiveness in these patients as the effectiveness they have demonstrated in somatizing patients.49,59,60
There is an emerging suggestion that among patients with physical complaints, pain is particularly important in predicting both the presence and the severity of depression.30,61 While elevated baseline pain negatively impacts clinical improvement 30 in usual care, it is not known whether quality improvement interventions counteract this effect. In our study baseline pain was equivalent for physical and psychological presenters, and did not account for the differentially improved symptom improvement that the enhanced care intervention had on patients presenting with psychological versus physical symptoms.
The internal validity of the study's findings is potentially limited by the possibility that enhanced care physicians may have elicited or recorded different chief complaints than usual care physicians; however, the likelihood of this threat is diminished because there was no statistical difference in the probability that depressed patients presented with psychological or physical symptoms within the enhanced or usual care groups. Enhanced and usual care patients screening positive for depression were informed of the results, possibly altering their initial presentation at the index visit in comparable but unknown ways; however, most quality improvement interventions share screening results with patients, increasing our findings’ generalizability. Although strict rules were established for reliably classifying patients as presenting with physical or psychological symptoms in the medical record abstraction process (see Appendix), it is possible that some patients may have been classified inaccurately; however, such measurement error would make it more difficult to demonstrate statistically significant differences between the two groups.
External validity of our results is enhanced by the clinically and socioeconomically diverse study population targeted by the Agency for Healthcare Research and Quality depression guidelines.22 The intervention was tested in 12 geographically diverse, mixed model practices caring for patients insured through multiple health plans or not at all. Future investigators are encouraged to explore these findings in other depressed patient cohorts, before interventions are targeted exclusively to depressed patients with psychological complaints.
This study shows that depressed primary care patients’ presentation style at the index visit is an important moderator of treatment effect during acute treatment phase. For patients presenting with psychological symptoms, state-of-the-art primary care depression interventions significantly improve depression treatment, symptom severity, and physical/emotional role functioning over 6 months. For patients presenting with physical symptoms only, quality improvement interventions improve antidepressant use but do not translate to symptomatic or functional improvement. Given that the majority of depressed patients in primary care present with physical symptoms, this moderator should be considered as a stratification variable in future randomized clinical trials.62 Current depression quality improvement interventions should be modified, or new interventions designed, to improve outcomes for depressed patients who present with physical symptoms.
Appendix.
Coding of “Presenting Complaint” at Index Visit
| The medical record abstractor considered the below Diagnostic and Statistical Manual—Version IV (DSM-IV) symptoms as psychological complaints, EXCEPT in the case of shaded symptoms,which were considered physical complaints UNLESS the medical record clearly reflected that the symptom was considered by the patient to be psychological or related to mental health problems. |
| Depression Symptoms |
| * Depressed mood |
| * Lack of interest or pleasure in usual activities |
| * Hypersomnia (sleeping too much) or insomnia (sleeping too little) |
| * Appetite/weight gain/loss |
| * Fidgety/restless or slow speech/movement |
| * Low energy or fatigue |
| * Worthlessness, guilt, lack of self-confidence, or low self-esteem |
| * Trouble with thinking or concentration |
| * Thoughts of death or suicide |
| Generalized Anxiety Disorder (GAD) Symptoms |
| * Anxiety or worry |
| * Irritability |
| * Muscle tension |
| Panic Disorder Symptoms |
| * Periods of intense fear or discomfort |
| * Palpitations, pounding heart, or accelerated heart rate |
| * Sweating |
| * Trembling or shaking |
| * Shortness of breath or smothering sensations |
| * Feeling of choking |
| * Chest pain or discomfort |
| * Nausea or abdominal distress |
| * Feeling dizzy, unsteady, lightheaded, or faint |
| * Feelings of unreality (derealization) or of being detached from oneself (depersonalization) |
| * Fear of losing control or going crazy |
| * Fear of dying |
| * Numbness or tingling sensations (paresthesias) |
| * Chills or hot flashes |
| Substance Use/Abuse |
| * Alcohol use |
| * Sedatives or tranquilizers (barbiturates, sleeping pills, Seconal, Valium, Librium, Quaaludes, or Xanax) |
| * Marijuana (cannabis, THC) or hashish |
| * Stimulants (amphetamines, speed, or uppers) |
| * Opiates (heroin, codeine, Demerol, morphine, Percodan, methadone, Darvon, opium, or Dilaudid) |
| * Cocaine, crack, or coca leaves |
| * Hallucinogens (PCP, LSD, mescaline, peyote, psilocybin, or DMT) |
| * Inhalants (glue, toluene, or gasoline) |
| * Other drug use not listed |
Acknowledgments
The authors wish to acknowledge and thank Marcia Blake, Nancy Burris, Byron Burton, Beth Gallovic, Robert Gibbons, Stephanie Mitchell, Barbara Howard, Joylyn Humphrey, Oliver Lin, Kathryn Magruder, Susan Moore, and James Werner for their substantial contributions to this study. The authors also express gratitude to the physicians, nurses, office staff, and patients from the participating primary care practices, and to the practice-based research networks (Ambulatory Sentinel Practice Network, Minnesota Academy of Family Physicians Research Network, and the Wisconsin Research Network) from which participating practices were recruited. Finally, the authors thank anonymous reviewers of earlier drafts of this manuscript for their helpful comments.
This research was supported by National Institute of Mental Health grant R01 MH54444, Health Resources and Services Administration National Research Service Award 5T32 HP10006-10, and by a grant from the John D. and Catherine T. MacArthur Foundation. Dr. Rost is also supported by NIMH K02 Independent Scientist Award MH63651.
REFERENCES
- 1.Jackson JL, Houston JS, Hanling SR, Terhaar KA, Yun JS. Clinical predictors of mental disorders among medical outpatients. Arch Intern Med. 2001;161:875–9. doi: 10.1001/archinte.161.6.875. [DOI] [PubMed] [Google Scholar]
- 2.Kirmayer LJ, Robbins JM. Patients who somatize in primary care: a longitudinal study of cognitive and social characteristics. Psychol Med. 1996;26:937–51. doi: 10.1017/s0033291700035273. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg DP, Bridges K. Somatic presentations of psychiatric illness in primary care setting. J Psychosom Res. 1988;32:137–45. doi: 10.1016/0022-3999(88)90048-7. [DOI] [PubMed] [Google Scholar]
- 4.Wilson DR, Widmer RB, Cadoret RJ, Judiesch K. Somatic symptoms. A major feature of depression in a family practice. J Affect Disorders. 1983;5:199–207. doi: 10.1016/0165-0327(83)90042-3. [DOI] [PubMed] [Google Scholar]
- 5.Watts CAH. The mild endogenous depression. BMJ. 1957;I:4–8. doi: 10.1136/bmj.1.5009.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clarke RL. The treatment of depression in general practice. South African Med J. 1969;1:724–5. [PubMed] [Google Scholar]
- 7.Kleinman A. Culture and patient care—psychiatry among the Chinese. Drug Ther. 1981;11:134–40. [Google Scholar]
- 8.APA. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1995. [Google Scholar]
- 9.Escobar JI, Gomez J, Tuason VB. Depressive phenomenology in North and South American patients. Am J Psychiatry. 1983;140:47–51. doi: 10.1176/ajp.140.1.47. [DOI] [PubMed] [Google Scholar]
- 10.Kleinman A. Neurasthenia and depression: a study of somatization and culture in China. Cult Med Psychiatry. 1982;6:117–90. doi: 10.1007/BF00051427. [DOI] [PubMed] [Google Scholar]
- 11.Katon W, Kleinman A, Rosen G. Depression and somatization: a review. Part I. Am J Med. 1982;72:127–35. doi: 10.1016/0002-9343(82)90599-x. [DOI] [PubMed] [Google Scholar]
- 12.Zung WW, Magill M, Moore JT, George DT. Recognition and treatment of depression in a family medicine practice. J Clin Psychiatry. 1983;44:3–8. [PubMed] [Google Scholar]
- 13.Williamson PS, Yates WR. The initial presentation of depression in family practice and psychiatric outpatients. Gen Hosp Psychiatry. 1989;11:189–93. doi: 10.1016/0163-8343(89)90040-6. [DOI] [PubMed] [Google Scholar]
- 14.Magruder-Habib K, Zung WW, Feussner JR. Improving physicians’ recognition and treatment of depression in general medical care. Results from a randomized clinical trial. Med Care. 1990;28:239–50. doi: 10.1097/00005650-199003000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med. 1997;103:339–47. doi: 10.1016/s0002-9343(97)00241-6. [DOI] [PubMed] [Google Scholar]
- 16.Maier W. The epidemiology of comorbidity between depression, anxiety disorders and somatic diseases. Int Clin Psychopharmacol. 1999;14(suppl 2):S1–S6. [PubMed] [Google Scholar]
- 17.Rost K, Nutting P, Smith JS, Werner J, Duan N. Improving depression outcomes in community primary care practice: a randomized trial of the QuEST intervention. Quality enhancement by strategic teaming. J Gen Intern Med. 2001;16:143–9. doi: 10.1111/j.1525-1497.2001.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rost K, Nutting PA, Smith J, Werner JJ. Designing and implementing a primary care intervention trial to improve the quality and outcome of care for major depression. Gen Hosp Psychiatry. 2000;22:66–77. doi: 10.1016/s0163-8343(00)00059-1. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerman M, Coryell W, Wilson S, Corenthal C. Evaluation of symptoms of major depressive disorder: self-report vs. clinician ratings. J Nerv Ment Dis. 1986;174:150–3. doi: 10.1097/00005053-198603000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33:80–8. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- 21.Tacchini G, Coppola MT, Musazzi A, Altamura AC, Invernizzi G. Multinational validation of the Composite International Diagnostic Interview (CIDI) Minerva Psichiatr. 1994;35:63–80. [PubMed] [Google Scholar]
- 22.AHCPR . Depression Guideline Panel: Depression in Primary Care. Detection and Diagnosis. Clinical Practice Guideline. No. 5. Vol. 1. Rockville, Md: U.S. Department of Health and Human Services, Public Health Agency, Agency for Health Care Policy and Research; 1993. [Google Scholar]
- 23.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 24.Orlando M, Sherbourne CD, Thissen D. Summed-score linking using item response theory: application to depression measurement. Psychol Assess. 2000;12:354–9. doi: 10.1037//1040-3590.12.3.354. [DOI] [PubMed] [Google Scholar]
- 25.Ware JEJ, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston, Mass: Health Institute, New England Medical Center; 1993. [Google Scholar]
- 26.WHO . Composite International Diagnostic Interview for Primary Care. Version 2.0. Geneva, Switzerland: World Health Organization; 1996. [Google Scholar]
- 27.Byrk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis Methods. 1st ed. Newbury Park, Calif: Sage Publications; 1992. [Google Scholar]
- 28.Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS System for Mixed Models. Cary, NC: SAS Institute, Inc.; 1999. [Google Scholar]
- 29.Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychol Methods. 1997;2:64–78. [Google Scholar]
- 30.Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66:17–22. doi: 10.1097/01.psy.0000106883.94059.c5. [DOI] [PubMed] [Google Scholar]
- 31.Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry. 2003;60:39–47. doi: 10.1001/archpsyc.60.1.39. [DOI] [PubMed] [Google Scholar]
- 32.Bridges KW, Goldberg DP. Somatic presentations of DSM-III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–9. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- 33.Simon GE, Heiligenstein J, Revicki D, et al. Long-term outcomes of initial antidepressant drug choice in a ‘real world’ randomized trial. Arch Fam Med. 1999;8:319–25. doi: 10.1001/archfami.8.4.319. [DOI] [PubMed] [Google Scholar]
- 34.Susman JL, Crabtree BF, Essink G. Depression in rural family practice: easy to recognize, difficult to diagnose. Arch Fam Med. 1995;4:427–31. doi: 10.1001/archfami.4.5.427. [DOI] [PubMed] [Google Scholar]
- 35.Freeling P, Rao BM, Paykel ES, Sireling LI, Burton RH. Unrecognized depression in general practice. Br Med J. 1985;290:1880–3. [PMC free article] [PubMed] [Google Scholar]
- 36.Williams JWJ, Mulrow CD, Kroenke K, et al. Case-finding for depression in primary care: a randomized trial. Am J Med. 1999;106:36–43. doi: 10.1016/s0002-9343(98)00371-4. [DOI] [PubMed] [Google Scholar]
- 37.Simon GE, Von Korff, Picinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–35. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 38.Von Korff M, Goldberg D. Improving outcomes for depression. BMJ. 2001;323:948–9. doi: 10.1136/bmj.323.7319.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klinkman MS. Competing demands in psychosocial care: a model for the identification and treatment of depressive disorders in primary care. Gen Hosp Psychiatry. 1997;19:98–111. doi: 10.1016/s0163-8343(96)00145-4. [DOI] [PubMed] [Google Scholar]
- 40.Fortney J, Rost K, Zhang M, Pyne J. The relationship between quality and outcomes in routine depression care. Psychiatr Serv. 2001;52:56–62. doi: 10.1176/appi.ps.52.1.56. [DOI] [PubMed] [Google Scholar]
- 41.Koike AK, Unutzer J, Wells KB. Improving the care for depression in patients with comorbid medical illness. Am J Psychiatry. 2002;159:1738–45. doi: 10.1176/appi.ajp.159.10.1738. [DOI] [PubMed] [Google Scholar]
- 42.Manning JS. Difficult-to-treat depressions: a primary care perspective. J Clin Psychiatry. 2003;64(suppl 1):24–31. [PubMed] [Google Scholar]
- 43.Goldstein DJ, Mallinckrodt C, Lu Y, Demitrack MA. Duloxetine in the treatment of major depressive disorder: a double-blind clinical trial. J Clin Psychiatry. 2002;63:225–31. doi: 10.4088/jcp.v63n0309. [DOI] [PubMed] [Google Scholar]
- 44.Hamilton KE, Dobson KS. Cognitive therapy of depression: pretreatment patient predictors of outcome. Clin Psychol Rev. 2002;22:875–93. doi: 10.1016/s0272-7358(02)00106-x. [DOI] [PubMed] [Google Scholar]
- 45.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 46.Dowrick C, Dunn G, Ayuso-Mateos JL, et al. Problem solving treatment and group psychoeducation for depression: multicentre randomised controlled trial. Outcomes of Depression International Network (ODIN) Group. BMJ. 2000;9:1450–4. doi: 10.1136/bmj.321.7274.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barsky AJ. Clinical practice: the patient with hypochondriasis. N Engl J Med. 2001;345:1395–9. doi: 10.1056/NEJMcp002896. [DOI] [PubMed] [Google Scholar]
- 48.Keeley R, Smith M, Miller J. Somatoform symptoms and treatment nonadherence in depressed family medicine outpatients. Arch Fam Med. 2000;9:46–54. doi: 10.1001/archfami.9.1.46. [DOI] [PubMed] [Google Scholar]
- 49.Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes: a critical review of controlled clinical trials. Psycho Psychosom. 2000;69:205–15. doi: 10.1159/000012395. [DOI] [PubMed] [Google Scholar]
- 50.Bass C, May S. ABC's of psychological medicine: chronic multiple functional somatic symptoms. BMJ. 2002;325:323–6. doi: 10.1136/bmj.325.7359.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mayou R, Farmer A. ABC's of psychological medicine: functional somatic symptoms and syndromes. BMJ. 2002;325:265–8. doi: 10.1136/bmj.325.7358.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.O'Malley PG, Jackson JL, Santoro J, et al. Antidepressant therapy for unexplained symptoms and symptom syndromes. J Fam Pract. 1999;48:980–90. [PubMed] [Google Scholar]
- 53.Dickinson WP, Dickinson LM, deGruy FV, et al. The somatization in primary care study: a tale of three diagnoses. Gen Hosp Psychiatry. 2003;25:1–7. doi: 10.1016/s0163-8343(02)00247-5. [DOI] [PubMed] [Google Scholar]
- 54.Dickinson WP, Dickinson LM, deGruy FV, Main DS, Candib LM, Rost KM. A randomized clinical trial of a care recommendation letter intervention for somatization in primary care. Ann Fam Med. 2003;1:228–35. doi: 10.1370/afm.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Loldrup D, Langemarck M, Hansen H, Olesen J, Bech P. Clomipramine and mianserin in chronic idiopathic pain syndrome: a placebo controlled study. Psychopharmacology. 1989;99:1–7. doi: 10.1007/BF00634443. [DOI] [PubMed] [Google Scholar]
- 56.Couch JR, Hassanein RS. Amitriptyline in migraine prophylaxis. Arch Neurol. 1979;36:695–9. doi: 10.1001/archneur.1979.00500470065013. [DOI] [PubMed] [Google Scholar]
- 57.Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2000;15:527–34. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine. 2001;26:1418–24. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 59.Linton SJ, Andersson T. Can chronic disability be prevented? Spine. 2000;25:2825–31. doi: 10.1097/00007632-200011010-00017. [DOI] [PubMed] [Google Scholar]
- 60.Allen LA, Woolfolk RL, Leher PM, Gara MA, Escobar JI. Cognitive behavior therapy for somatization disorder: a preliminary investigation. J Behav Ther Exp Psychiatry. 2001;32:53–62. doi: 10.1016/s0005-7916(01)00020-9. [DOI] [PubMed] [Google Scholar]
- 61.Kroenke K. The interface between physical and psychological symptoms. Prim Care Companion J Clin Psychiatry. 2003;5(suppl 7):11–8. [Google Scholar]
- 62.Kraemer HC, Wilson T, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]


