Abstract
OBJECTIVE
Understanding the roles and responsibilities of physicians who manage mutual patients is important for assuring good patient care. Among physicians expressing a preference to involve a neurologist in the care of a patient, we evaluated agreement between neurologists and primary care physicians for the extent of specialty involvement in the evaluation and management of the patient, and the factors influencing those preferences.
DESIGN AND SETTING
A self-administered survey containing 3 clinical scenarios was developed with the assistance of a multispecialty advisory board and mailed to a stratified probability sample of physicians.
PARTICIPANTS
Six hundred and eight family physicians, 624 general internists, and 492 neurologists in 9 U.S. states.
INTERVENTIONS
For each scenario, those respondents who preferred involvement of a specialist were asked about the preferred extent of that involvement: one-time consultation with and without test/medication ordering, consultation and limited follow-up, or taking over ongoing care of the specialty problem as long as it persists.
MAIN RESULTS
Survey response rate was 60%. For all 3 scenarios, neurologists preferred a greater extent of specialty involvement compared to primary care physicians (all P <.05). Other physician and practice characteristic factors, including financial incentives, had lesser or no influence on the extent of specialty involvement preferred.
CONCLUSIONS
The disagreement between primary care physicians and specialists regarding the preferred extent of specialist involvement in the care of patients with neurological conditions should raise serious concerns among health care providers, policy makers, and educators about whether mutual patient care is coordinated and appropriate.
Keywords: referral and consultation, physician's practice patterns
Perhaps because of the movement toward a generalistcentered health care system, physicians have been largely dichotomized into 2 physician groups with different patient care roles and responsibilities: generalists and specialists. While dichotomizing these physician groups is relatively easy when based on postgraduate education, understanding and defining their actual role in patient care is complicated by their overlapping responsibilities 1,2. Notwithstanding this limitation, the physician specialists’ role has developed out of the expansion of science and the technological advances inherent in this growth,3 and the physician specialist, particularly the internal medicine subspecialist and the medical specialist, is generally considered an expert in evaluating and managing organ- or disease-specific conditions. Not surprisingly, patients seen by specialists have been shown to have more specialty-specific complications than patients seen by primary care physicians.4 The role of the generalist is more complex. Primary care physician responsibilities have been shown to include patient care coordination, gatekeeping,5 preventative care,6 care for common conditions,7 care for a wide range of conditions, continuous care, and accessible care.8 Thus, it is not surprising that most patients with specialty conditions are frequently managed by more than one type of physician.9
Patients who are managed by more than one physician are transferred between physicians via the use of consultations and referrals. A consultation has been defined as the exchange of physician expertise with the patient responsibility remaining with the initial physician, and a referral has been defined as the transfer of some or all of the patient responsibility to the consulted physician.10 Primary care physicians may request a specialist consultation or referral for many reasons including advice or second opinion on diagnosis or management, needed skills or facilities, or patient request.11–13
The major concern when multiple physicians are involved in the care of a patient with a specialty condition is whether the appropriate physician is responsible for the patient and whether patient care is coordinated. The specialty of neurology is particularly relevant because neurologists are very dependent on physician referrals for their patients; however, primary care physicians manage many common neurological conditions.14–16 Even neurologists disagree as to whether primary care physicians or neurologists should coordinate the medical care for patients with neurological conditions.17 In addition, coordinated care may be further complicated by the use of utilization management techniques,18 financial incentives,19 and other organizational-based factors 20,21 used by health care organizations to influence physician referral behavior.22,23
In a previous study,24 we described primary care physicians’ and neurologists’ preferences for involving a specialist in the care of patients with neurological conditions and found that nearly all neurologists preferred to be involved in the care of a patient with a neurological condition, whereas only one quarter to two thirds of primary care physicians preferred to involve a neurologist, depending on the particular patient scenario. The study presented here focuses on the subset of physicians who preferred that a specialist be involved in a particular scenario, and is aimed at understanding the level of agreement between primary care physicians and neurologists on the extent of involvement of a neurologist.
METHODS
Overview
We mailed a questionnaire to a national sample of general internists, family physicians, and neurologists containing scenarios describing patients with common neurological conditions. Among those physicians who felt a neurologist should be involved, we compared neurologists and primary care physicians’ preferences for the preferred extent of specialist involvement, ranging from a one-time consultation with recommendations for tests, procedures, or medications to ongoing specialist involvement in the care of the patient for the duration of the neurological condition or problem. We also assessed factors that might influence these choices.
Survey Instrument
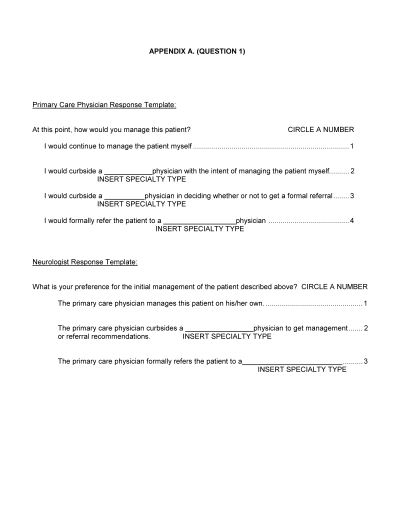
Clinical Scenarios and Referral/Consultation Preferences.
The questionnaire included 3 clinical scenarios developed with the assistance of an 8-member advisory board, with 2 members each nominated by the American Academy of Family Physicians, the American College of Physicians—American Society of Internal Medicine (ACP-ASIM), and the American Academy of Neurology. A health services researcher and a medical director of a health care trade association were also included. We modeled specialty preferences regarding care of elderly patients with neurological conditions. The 3 clinical scenarios described 1) a patient with a recent transient neurological event and carotid stenosis, 2) a Parkinson's disease patient on carbidopa-levodopa with dyskinesias, and 3) a patient presenting with dementia symptoms.24 The neurological conditions for the clinical scenarios were chosen based on the following criteria: the neurological condition is seen by both generalists and neurologists, the condition is prevalent, and the condition has treatment or management processes substantiated by generally accepted evidence-based literature.
Each of the 3 clinical scenarios was followed by 2 questions addressing physician referral preferences. Our model assumed that the primary care physician was the patient's first physician contact. The questions were framed to accommodate the different perspectives of the primary care physician making the referral and the neurologist receiving the referral. The first question measured physician preferences for the primary care physician managing the patient without specialty assistance, requesting a curbside consultation, or preferring to formally refer the patient to a specialist.
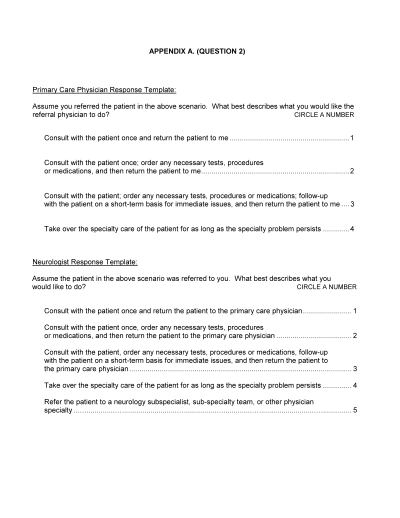
For physicians who indicated they would prefer to formally refer the patient presented in the scenario to a specialist—the subset of physicians’ responses presented here—we analyzed responses to a second question, which assessed the type of referral or consultation preferred. Response options for physicians for the second question, which reflected the extent of specialty involvement, included preferences for the specialist to 1) conduct a one-time consultation and return the patient to the primary care physician, 2) conduct a one-time consultation with the patient, order necessary tests, procedures, or medications, and return the patient to the primary care physician, 3) evaluate the patient, order necessary tests, procedures, or medications, and provide short-term follow-up for the immediate problem before returning the patient to the primary care physician, or 4) take over the specialty care of the patient for as long as the specialty problem persists. Response options for the neurologists’ survey also included a fifth choice: the option to refer the patient on to a subspecialist. We excluded responses to the fifth option in our analyses as it consisted of less than 4% of the neurologists’ responses.
Clinical and Nonclinical Factors.
Physicians reported their specialty designation, age, gender, practice setting (solo practice, single-specialty group practice, multispecialty group practice, university setting, staff-model HMO, government clinic, or hospital), number of patients seen per week, and their perception of time pressure to see patients. Physician knowledge relevant to each of the 3 clinical scenarios was also measured using 3 scenario-specific knowledge scales developed with the help of an advisory board.24 Physicians were also asked the percentage of personal income derived from salary, capitated payments, fee-for-service payments, withhold returns, and bonuses, the percentage of their Medicare patients in managed care Medicare contracts or plans, the percentage of their patients requiring preauthorization and referrals from primary care physicians, and the number of times they were profiled per year.
Sample and Data Collection
Six hundred twenty-four general internists were drawn from the ACP-ASIM membership database, 608 family physicians were drawn from the American Medical Association's Physician Masterfile, and 492 neurologists were drawn from the American Academy of Neurology's membership database. Physicians within each database were sampled using a stratified probability sample of the 9 states with the highest managed care Medicare penetration in 1998. Surveys were mailed during fall–winter 1998–1999 and included a $15 cash payment; 4% of all sampled physicians were later deemed ineligible because the physician was still in training, retired, spent <50% in clinical work, had subspecialty training (for internists), resided outside the United States, or had a survey returned undelivered. All variables were obtained from the survey instrument except for age and gender, which were obtained from the physician databases for neurologists and general internists. For the family physicians, these variables were obtained from physician directories and telephone calls to office staff.
Analyses
t tests were used to evaluate practice characteristic and demographic differences between physicians who preferred referral to a specialist and those who preferred to manage alone or curbside. All subsequent analyses refer to those respondents for each scenario who would refer to a specialist. For each scenario, χ2was used to compare primary care physicians and neurologists on the 4 types of referral-consultation options. Simple logistic regression was subsequently used to evaluate the effect size of physicians’ specialty on their choices for extent of specialist involvement. Simple and multivariate logistic regression and correlation analyses were used to explore the relationships of organizational and financial factors, physician knowledge, and demographic characteristics on preferences for extent of specialist involvement.
RESULTS
The overall survey response rate was 60.0%; response rates did not differ across general internists (60.1%; n= 367), family physicians (57.2%; n= 321), and neurologists (62.2%; n= 299) (P= .26). Respondent and nonrespondent neurologists and general internists did not differ in age, and there was no difference in the proportion of neurologist respondents and nonrespondents who were female. However, a larger proportion of nonrespondent general internists were female (31.5% females in nonrespondent group vs 23% females in respondent group; P= .02). Among respondents, general internists, family physicians, and neurologists differed on most characteristics including age (general internists slightly younger than other 2 groups), gender (higher proportion of women among general internists than other 2 groups), practice characteristics (smaller proportion of general internists in solo practice than other 2 groups), and utilization management (less profiling of neurologists than of other 2 groups), among others.24
For the transient neurological event scenario, the Parkinson's disease scenario, and the dementia scenario, 92%, 90%, and 95% of the neurologists, 37%, 47%, and 21% of the general internists, and 46%, 39%, and 29% of the family physicians surveyed, respectively, preferred to refer the patient in the scenario to a specialist and therefore were included in these analyses. Some differences in practice characteristics and demographics were found between physicians who preferred specialist involvement and those preferring to manage alone or curbside (Table 1)
Table 1.
Practice Characteristic and Demographic Differences Between Physicians Who Preferred to Refer to a Specialist Versus Manage Alone or Curbside
| Referral Preference | ||||
|---|---|---|---|---|
| Physician Group | Practice Characteristic/Demographic | Refer to Specialist * | Manage Alone or Curbside | P Value |
| Family physician | Number of respondents † | 139‡/120§/89|| | 164‡/184§/214|| | |
| Percent of respondents | 46‡/39§/29|| | 54‡/61§/71|| | ||
| Average age of physician | 51‡|| | 47‡|| | <.01‡|| | |
| Avg. number of patients seen per week | 90‡/88|| | 102‡/100|| | <.02‡/<.04|| | |
| Percent of patients requiring preauthorization | 40‡§/42|| | 37‡/37§/37|| | ns | |
| Percent of income from capitation | 11‡/13§|| | 11‡/10§|| | ns | |
| Internist | Number of respondents † | 135‡/166§/74|| | 227‡/195§/286|| | |
| Percent of respondents | 37‡/47§/21|| | 63‡/53§/79|| | ||
| Average age | 48‡|| | 45‡|| | <.01‡|| | |
| Avg. number of patients seen per week | 84‡||/86§ | 89‡§/88|| | ns | |
| Percent of patients requiring preauthorization | 36‡/41|| | 27‡|| | .01‡/.001|| | |
| Percent of income from capitation | 6§/5|| | 11§/10|| | <.01§/.04|| | |
| Neurologist | Number of respondents † | 273‡/266§/279|| | 23‡/28§/14|| | |
| Percent of respondents | 92‡/90§/95|| | 8‡/10§/5|| | ||
| Average age of physician | 49‡§|| | 48‡||/49§ | ns | |
| Avg. number of patients seen per week | 60§ | 50§ | .04§ | |
| Percent of patients requiring preauthorization | 42‡ | 22‡ | <.01‡ | |
| Percent of income from capitation | 2‡§|| | 0‡§/1|| | ns | |
No differences between groups in any scenarios were found for percent income from fee-for-service or salary, extra time to see patients, number of times profiled per year, or percent of patients self-referred.
Physicians included in the analyses of this manuscript.
Not all physicians completed all 3 vignettes. Results reported for scenarios with differences withP < .05; in cases where P <.05 for all comparisons, all results are reported.
Transient neurological event scenario.
Parkinson's disease scenario.
Dementia scenario.
ns, not significant.
For those physicians who preferred formal specialist involvement, more neurologists than internists and family physicians preferred the neurologist take over the care of the patient for as long as the neurological condition persisted: 29.7% versus 16.3% and 23%, respectively, for the transient neurological event scenario; 68.4% versus 36.1% and 24.2%, respectively, for the Parkinson's disease scenario; and 34.8% versus 18.9% and 13.5%, respectively, for the dementia scenario (all P < .001). While similar proportions of neurologists, general internists, and family physicians preferred the consult with limited follow-up for the transient neurological event and dementia scenarios, far fewer neurologists compared to primary care physicians preferred a one-time specialty consult or a one-time specialty consult with responsibility for initial tests or medications in the Parkinson's disease scenario (Table 2)
Table 2.
Type of Referral–Consultation Option Preferred by Neurologists and Primary Care Physicians
| Specialty Consult with Tests | Consult with Limited Follow-up | |||
|---|---|---|---|---|
| One-time Specialty Consult | Percentage of Respondents | Specialist Takes over Care “Ongoing Management” | ||
| Transient Neurological Event | ||||
| Neurologists (N= 273) | 1.5 | 7.7 | 60.0 | 29.7 |
| Internists (N= 135) | 4.4 | 19.2 | 60.0 | 16.3 |
| Family physicians (N= 139) | 5.7 | 14.4 | 56.8 | 23.0 |
| Parkinson's Disease | ||||
| Neurologists (N= 266) | 1.5 | 1.9 | 23.3 | 68.4 |
| Internists (N= 166) | 4.8 | 9.6 | 49.4 | 36.1 |
| Family physicians (N= 120) | 7.5 | 18.3 | 50.0 | 24.2 |
| Dementia Evaluation and Management | ||||
| Neurologists (N= 279) | 1.4 | 7.9 | 53.4 | 34.8 |
| Internists (N= 74) | 8.1 | 20.3 | 52.7 | 18.9 |
| Family physicians (N= 89) | 7.9 | 28.1 | 50.6 | 13.5 |
Rows add to 100%.
χ2P < .001 for each clinical scenario.
The odds of a neurologist versus a primary care physician preferring a referral or consultation that required more visits from the neurologist were significant for all scenarios. However, the odds of a neurologist versus a primary care physician preferring a single consult with responsibility for initial tests or medications versus just a single consult were not significant in any of the scenarios (Table 3), after controlling for a physician's knowledge specific to that clinical scenario and other physician and organizational factors, the respondent's specialty designation, that is, neurologist versus primary care physician, had the largest and most consistent association with the dichotomous outcome of preference for ongoing specialty management (reflecting a greater extent of specialist involvement) versus the collapsed category of the remainder of the 3 consultation options (reflecting a lesser extent of specialist involvement) (P < .05).
Table 3.
Neurologists’ Versus Primary Care Physicians’ Preferences for Extent of Specialty Involvement
| Odds Ratio (95% Confidence Interval) | |||
|---|---|---|---|
| Ongoing Management Versus Consultation with Limited Follow-up | Consultation with Limited Follow-up Versus One-time Consultation with Tests, Procedures, and Medications | One-time Consultation with Tests, Procedures, and Medications Versus One-time Consultation Only | |
| Transient neurological event scenario | 1.5 (>1.0 to 2.2) | 2.2 (1.3 to 3.9) | ns |
| Parkinson's disease scenario | 4.6 (3.2 to 6.9) | 3.3 (1.2 to 8.8) | ns |
| Dementia evaluation scenario | 2.1 (1.3 to 3.5) | 3.2 (1.8 to 5.8) | ns |
In multivariate logistic regression analyses (Table 4)after controlling for a physician's knowledge specific to that clinical scenario and other physician and organizational factors, the respondent's specialty designation, that is, neurologist versus primary care physician, had the largest and most consistent association with the dichotomous outcome of preference for ongoing specialty management (reflecting a greater extent of specialist involvement) versus the collapsed category of the remainder of the 3 consultation options (reflecting a lesser extent of specialist involvement)(P < .05).
Table 4.
Variables Explaining Referral Preferences for Ongoing Management Versus Consultation
| Transient Neurological Event Ongoing Management Versus Consultation *(N = 535) | Parkinson's Disease Ongoing Management Versus Consultation (N= 548) | Dementia Ongoing Management Versus Consultation (N= 422) | |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | |||
| Physician Characteristics | |||
| Neurologist versus primary care physician | 2.5 (1.6 to 3.9) | 6.5 (4.0 to 10.7) | 4.4 (2.5 to 7.7) |
| Decrease in physician's age by 10 years | 1.4 (1.1 to 1.7) | 0.8 (0.7 to 1.0) | ns |
| Scenario-specific Clinical Knowledge | |||
| 20% increase in knowledge on scenario-specific knowledge scale | 0.7 (0.6 to 0.9) | ns | ns |
| Practice Characteristics | |||
| 20% increase in patients who are self-referred | 1.3 (<1.0 to 1.4) | ns | 1.3 (<1.0 to 1.4) |
| Increase in patient load by 20 patients per week | 1.1 (<1.0 to 1.2) | ns | 1.2 (1.1 to 1.4) |
| Utilization Management | |||
| No profiling versus yearly or more | ns | 1.6 (1.2 to 2.4) | ns |
| Practice Setting | |||
| Staff-model HMO | ns | 2.3 (<1.0 to 4.5) | ns |
Model also controlling for physician gender, time availability, percent of patients requiring preauthorization, and reimbursement from fee-for-service, salary, and capitation, all of which were not significant in any model.
Ongoing management includes those physician respondents who indicated they preferred the specialist to take over the care of the patient for as long as the specialty problem persists. Consultation includes those physician respondents who preferred a consultation alone, either with tests and procedures or with limited follow-up.
ns = not significant at 95% confidence interval.
DISCUSSION
Among the neurologists and primary care physicians who agreed a specialist should be involved in the care of patients with neurological conditions, we observed important differences in the type of consult and referral they preferred and the extent of specialist involvement they preferred. For all scenarios, the specialist preferred a greater extent of involvement than did the primary care physician. The disagreement in how primary care physicians and neurologists should care for mutual patients underscores concerns about whether the care provided by both the primary care physician and specialist is coordinated and appropriate.
The most important difference in the primary care physicians’ and neurologists’ consultation and referral preferences was the proportion of physicians who preferred the neurologist provide ongoing management for the patient's specialty condition. More neurologists felt they should be responsible for the care of the patient as compared to primary care physicians preferring the neurologist take over the care of the patient. Some have argued that specialists should manage patients with specialty conditions because the care of some chronic conditions can be complex and specialists have more knowledge about these conditions.25 Others argue that the primary care physician is still better able to provide and coordinate all the varying medical needs and so the responsibility should still remain with the primary care physician.26
The pattern of more neurologists than primary care physicians preferring the neurologists take over the care of the patient was more pronounced for the Parkinson's disease scenario than for the other two scenarios. One possible explanation for this may be that Parkinson's disease is less common than dementia and stroke disorders. The prevalence of Parkinson's disease is 1.6% in patients aged 65 years and older,27 whereas the prevalence of dementia in patients over the age of 65 years has been estimated as high as 10%.28 Another possible explanation is that physician specialty groups make assumptions about the specific conditions they should manage, and information may be more readily available to neurologists for some conditions and to primary care physicians for others. Although scenario-specific knowledge was not a significant predictor of type of consultation in this study, we previously showed that the generalist's knowledge, relative to the neurologist's knowledge, of management of the Parkinson's disease scenario was much lower than for the other two scenarios.24
When health care providers are not in agreement about how work efforts should be differentiated, coordination is unlikely to exist. Coordination is the activity of consciously synchronizing differentiated work efforts,29 and coordinated care has been associated with better patient outcomes.30–32 The coordination of care may be disrupted because physicians are in competition for patient resources. Physicians might prefer consultations and/or referrals requiring increasing time and effort when the reimbursement for their services is linked to more patient visits, such as occurs in fee-for-service reimbursement. Thus, physicians with primarily fee-for-service reimbursement should prefer referrals and consultations requiring more patient visits compared to salaried physicians. After controlling for specialty designation, we found a null effect of all financial incentives in the multivariate analyses; therefore, our findings do not support this explanation. Other factors, such as experiences with profiling and working in a staff-model HMO, were only significant in one scenario. Other investigators found that neurologists in HMOs were less likely to provide extended care compared to consultative care; however, they did not measure the construct of “ongoing management.”33
Several other factors were found to predict a physician's preference for extent of specialty involvement besides the specialty designation. The fact that physicians with more self-referred patients were more likely to prefer ongoing management than those with fewer self-referred patients is not surprising, as self-referred patients are less likely to have an assigned primary care physician and therefore will have a stronger need for a physician to provide ongoing management. After controlling for several practice and provider characteristics, physicians who saw more patients preferred the neurologist to provide ongoing management. The magnitude of this association was not large and this may be because the effect is working in opposite directions for each physician specialty group, that is, a busy primary care physician might prefer the neurologist provide ongoing management, but the busy neurologist might prefer the primary care physician retain responsibility. Age has been found to predict physicians’ referral preferences;34,35 however, in our study, physician age was not a consistent predictor of extent of specialist involvement among those preferring some sort of referral.24 Physician knowledge was only significant in one scenario. Studies linking physician knowledge to referral behavior have shown conflicting results.36–40 Physician knowledge has been shown to consistently predict whether specialty involvement would be preferred (physicians with less knowledge specific to that clinical situation express a greater preference to refer to a specialist than physicians with greater knowledge), but it is plausible that among those preferring specialty involvement, knowledge is a less important factor in the extent of specialist involvement.24
The multivariate logistic regression analysis for the Parkinson's disease scenario revealed slightly different results than for the other two scenarios. For the Parkinson's disease scenario, physicians in a staff-model HMO and physicians who were not profiled were more likely to prefer the neurologist to provide ongoing management, and the physician's patient load and percent of self-referred patients were not significant. Thus, some of the factors that influence physician referral preferences appear to be dependent on the type of condition and the issues specific to the management of that condition.
The question remains as to what factor associated with the physicians’ specialty group is responsible for the major differences in the neurologists’ and primary care physicians’ referral- and consultation-type preferences. Perhaps physicians prefer and derive pleasure from referrals and consultations that are more likely to allow them to observe patients improving and responding to their management decisions. A recent study assessing physician satisfaction showed that clinical autonomy, that is, the physician's freedom to make clinical decisions, ability to form continuing relationships, and assessment of their ability to provide high-quality care, was the strongest and most consistent predictor of physician satisfaction, and managed care was a weak predictor of physician satisfaction.41 This study supports our findings that factors inherent to the physician's identity, not financial reimbursement or factors associated with managed care, influence referral decisions.
The influence of physician specialty group on the neurologists’ and primary care physicians’ referral- and consultation-type preferences might also be explained by their respective patient experience. Despite the fact that primary care physicians’ and specialists’ referral preferences were based on the same patient scenario, the type of patients they see in practice may still indirectly influence their preferences. Parkinson's disease patients seen by neurologists are younger 14 and patients with stroke admitted to neurology service versus medicine service are younger, have better prognostic profiles, more uncommon stroke mechanisms, and lower frequency of comorbidities.16,42 Therefore, primary care physicians, presented with the same clinical scenario as neurologists, may still presume that the patient will have comorbid issues and issues related to aging that require the attention of a primary care physician. Subsequently, they may hesitate to recommend the specialist take over the care of the patient. In contrast, the neurologist may presume that the patient is likely to have more complicated problems restricted to neurology and therefore not hesitate to take over the care of the patient.
Several strengths and limitations characterized our study. Our study measured physician referral and consultation preferences. Survey methods are felt to represent an excellent method for measuring physician knowledge, preferences, attitudes, and beliefs.43 Nevertheless, the generalizability of our findings to actual practice is not clear. While there are biases inherent in vignette methodology,44 a recent study evaluating the ability of written case simulations to represent actual physician behavior found that written case simulations were a good proxy for actual behavior when judged by a standardized patient.45 In addition, the use of vignettes has the advantage of naturally “controlling” for patient case mix,45 which has been implicated as a confounder in other studies comparing physicians.16,46,47
The physicians in these analyses are a subset of the respondent physicians who already expressed a preference for referring the patients presented in the scenarios to a specialist. Therefore, our findings may underestimate the disagreement in the community, where physicians who would not prefer a specialist to be involved might not have a choice about sharing care for some patients. Generalizations of study findings to physicians nationally must be made cautiously given that we sampled physicians in states with higher Medicare managed care penetration, and a larger proportion of nonrespondent than respondent general internists were female. Finally, there may be some limitations to the generalizability of these findings in the care of patients with uncommon neurological conditions or where there is no overlap in care between primary care physicians and neurologists.
The disagreement between the primary care physicians and specialists regarding how patients who are referred to a specialist are best managed should raise serious concerns among health care providers, policy makers, and educators about whether the care for mutual patients is coordinated and appropriate. We found no factor that consistently explained this disagreement except for the physician's specialty group designation. Thus, interventions designed to improve physician coordination of care and better define physician roles and responsibilities will need to address factors inherent to physician specialty groups such as changing group belief systems and enhancing interphysician group communication and understanding. The next steps in a research agenda to elucidate such factors should include qualitative research methods including focus groups and interviews with physicians.
Acknowledgments
This study was supported by the American Academy of Neurology, the Robert Wood Johnson Foundation, and the VA Office of Academic Affairs. The authors thank the members of the Advisory Board: Roman Hendrickson, Michael LaCombe, Steven Ringel, William Likosky, Daniel Lang, Theodore Ganiats, and Jose Escarce. We would like to thank the American Academy of Neurology and the American College of Physicians—American Society of Internal Medicine for their help. We are also grateful to colleagues Brian Mittman, Martin Lee, and Ron Hays for assistance and to Sehyun Kim and Chris Donald for staff support.
Appendix A
 |
Appendix B
 |
REFERENCES
- 1.Dietrich AJ, Goldberg H. Preventative content of adult primary care: do generalists and subspecialists differ? Am J Public Health. 1984;74:223–7. doi: 10.2105/ajph.74.3.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aiken LH, Lewis CE, Craig J, et al. The contribution of specialists to the delivery of primary care. N Engl J Med. 1979;300:1363–70. doi: 10.1056/NEJM197906143002404. [DOI] [PubMed] [Google Scholar]
- 3.Cooper RA. Seeking a balanced physician workforce for the 21st century. JAMA. 1994;272:680–7. [PubMed] [Google Scholar]
- 4.Chin MH, Zhang JX, Merrell K. Specialty differences in the care of older patients with diabetes. Med Care. 2000;38:131–40. doi: 10.1097/00005650-200002000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Grumbach K, Selby JV, Damberg C, et al. Resolving the gatekeeper conundrum. What patients value in primary care and referrals to specialists. JAMA. 1999;282:261–6. doi: 10.1001/jama.282.3.261. [DOI] [PubMed] [Google Scholar]
- 6.Bindman AB, Grumbach K, Osmond D, Vranizan K, Stewart AL. Primary care and receipt of preventative services. J Gen Intern Med. 1996;11:269–76. doi: 10.1007/BF02598266. [DOI] [PubMed] [Google Scholar]
- 7.Spiegel JS, Rubenstein LV, Scott B, Brook RH. Who is the primary physician? N Engl J Med. 1983;308:1208. doi: 10.1056/NEJM198305193082007. [DOI] [PubMed] [Google Scholar]
- 8.Franks P, Clancy C, Nutting PA. Defining primary care: empirical analysis of the National Ambulatory Medical Care Survey. Med Care. 1997;35:655–68. doi: 10.1097/00005650-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Schappert SM. Office visits to neurologists: United States, 1991–1992. Adv Data. 1995;267:1–20. [PubMed] [Google Scholar]
- 10.Ludke RL. An examination of the factors that influence patient referral decisions. Med Care. 1982;20:782–96. doi: 10.1097/00005650-198208000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Brock C. Consultation and referral patterns of family physicians. J Fam Pract. 1977;4:1129–34. [PubMed] [Google Scholar]
- 12.Coulter A, Noone A, Goldacre M. General practitioners’ referrals to specialist outpatient clinics. BMJ. 1989;299:304–6. doi: 10.1136/bmj.299.6694.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forrest CB, Glade GB, Baker AE, Bocian AB, Kang M, Starfield B. The pediatric primary-specialty care interface. How pediatricians refer children and adolescents to specialty care. Arch Pediatr Adolesc Med. 1999;153:705–14. doi: 10.1001/archpedi.153.7.705. [DOI] [PubMed] [Google Scholar]
- 14.Rybicki BA, Johnson CC, Gorell JM. Demographic differences in referral rates to neurologists of patients with suspected Parkinson's disease: implications for case-control study design. Neuroepidemiology. 1995;14:72–81. doi: 10.1159/000109781. [DOI] [PubMed] [Google Scholar]
- 15.Callahan CM, Hendrie HC, Tierney WM. Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann Intern Med. 1995;122:422–9. doi: 10.7326/0003-4819-122-6-199503150-00004. [DOI] [PubMed] [Google Scholar]
- 16.Horner RD, Matchar DB, Divine GW, Feussner JR. Relationship between physician specialty and the selection and outcome of ischemic stroke patients. Health Serv Res. 1995;30:275–87. [PMC free article] [PubMed] [Google Scholar]
- 17.Ringel SP, Vickrey BG, Rogstad TL. U.S. neurologists: attitudes on the U.S. health care system. Neurology. 1996;47:279–87. doi: 10.1212/wnl.47.1.279. [DOI] [PubMed] [Google Scholar]
- 18.Hurley RE, Freund DA, Gage BJ. Gatekeeper effects on patterns of physician use. J Fam Pract. 1991;32:167–74. [PubMed] [Google Scholar]
- 19.Hillman AL, Pauly MV, Kerstein JJ. How do financial incentives affect physicians’ clinical decisions and the financial performance of health maintenance organizations? N Engl J Med. 1989;321:86–92. doi: 10.1056/NEJM198907133210205. [DOI] [PubMed] [Google Scholar]
- 20.Greenfield S, Nelson EC, Zubkoff M, et al. Variations in resource utilization among medical specialties and systems of care. JAMA. 1992;267:1624–30. [PubMed] [Google Scholar]
- 21.Pauly MV, Hillman AL, Kerstein J. Managing physician incentives in managed care. Med Care. 1990;28:1013–24. doi: 10.1097/00005650-199011000-00004. [DOI] [PubMed] [Google Scholar]
- 22.St. Peter RF, Reed MC, Kemper P, Blumenthal D. Changes in the scope of care provided by primary care physicians. N Engl J Med. 1999;341:1980–5. doi: 10.1056/NEJM199912233412606. [DOI] [PubMed] [Google Scholar]
- 23.Grumbach K, Osmond D, Vranizan K, Jaffe D, Bindman AB. Primary care physicians’ experience of financial incentives in managed-care systems. N Engl J Med. 1998;339:1516–21. doi: 10.1056/NEJM199811193392106. [DOI] [PubMed] [Google Scholar]
- 24.Swarztrauber K, Mittman BS, Vickrey BG. Physicians’ preferences for specialty involvement in the care of patients with neurological conditions. Med Care. 2002;40:1196–209. doi: 10.1097/00005650-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Ayanian JZ, Hauptman PJ, Guadagnoli E, et al. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331:1136–42. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 26.Gerber PD, Smith DS, Ross JM. Generalist physicians and the new health care system. Am J Med. 1994;97:554–8. doi: 10.1016/0002-9343(94)90351-4. [DOI] [PubMed] [Google Scholar]
- 27.de Rijk MC, Tzourio C, Breteler MMB, et al. Prevalence of parkinsonism and Parkinson's disease in Europe: the EUROPARKINSON collaborative study. J Neurol Neurosurg Psychiatry. 1997;62:10–5. doi: 10.1136/jnnp.62.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans D, Funkenstein H, Albert M, et al. Prevalence of Alzheimer's disease in a community population of older persons. Higher than previously reported. JAMA. 1989;262:2551–6. [PubMed] [Google Scholar]
- 29.Haimann T, Scott WG, et al. Management of the Modern Organization. 2nd ed. Boston, Mass: Houghton-Mifflin; 1974. p. 126. [Google Scholar]
- 30.Young GJ, Charns MP, Desai K, et al. Patterns of coordination and clinical outcomes: a study of surgical services. Health Serv Res. 1998;33(5 pt 1):1211–36. [PMC free article] [PubMed] [Google Scholar]
- 31.Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay. A nine-hospital study of surgical patients. Med Care. 2000;38:807–19. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Shortell SM, Zimmerman JE, Rousseau DM, et al. The performance of intensive care units: does good management make a difference? Med Care. 1994;32:508–25. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Franklin GM, Ringel SP, Jones M, Baron A. A prospective study of principal care among Colorado neurologists. Neurology. 1990;40:701–4. doi: 10.1212/wnl.40.4.701. [DOI] [PubMed] [Google Scholar]
- 34.Keating NL, Zaslavsky AM, Ayanian JZ. Physicians’ experiences and beliefs regarding informal consultation. JAMA. 1998;280:900–4. doi: 10.1001/jama.280.10.900. [DOI] [PubMed] [Google Scholar]
- 35.Kuo D, Gifford DR, Stein MD. Curbside consultation practices and attitudes among primary care physicians and medical subspecialists. JAMA. 1998;280:905–9. doi: 10.1001/jama.280.10.905. [DOI] [PubMed] [Google Scholar]
- 36.Franks P, Williams GC, Zwanziger J, Mooney C, Sorbero M. Why do physicians vary so widely in their referral rates? J Gen Intern Med. 2000;15:163–8. doi: 10.1046/j.1525-1497.2000.04079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reynolds GA, Chitnis JG, Roland MO. General practitioner outpatient referrals: do good doctors refer more patients to hospital? BMJ. 1991;302:1250–2. doi: 10.1136/bmj.302.6787.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calman NS, Hyman RB, Licht W. Variability in consultation rates and practitioner level of diagnostic certainty. J Fam Pract. 1992;35:31–8. [PubMed] [Google Scholar]
- 39.Franks P, Clancy CM. Referrals of adult patients from primary care: demographic disparities and their relationship to HMO insurance. J Fam Pract. 1997;45:47–53. [PubMed] [Google Scholar]
- 40.Vehvilainen AT, Kumpusalo EA, Voutilainen SO, Takala JK. Does the doctors’ professional experience reduce referral rates? Evidence from the Finnish referral study. Scand J Prim Health Care. 1996;14:13–20. doi: 10.3109/02813439608997063. [DOI] [PubMed] [Google Scholar]
- 41.Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1997–2001. JAMA. 2003;289:442–9. doi: 10.1001/jama.289.4.442. [DOI] [PubMed] [Google Scholar]
- 42.Petty GW, Brown RD, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Ischemic stroke: outcomes, patient mix, and practice variation for neurologists and generalists in a community. Neurology. 1998;50:1669–78. doi: 10.1212/wnl.50.6.1669. [DOI] [PubMed] [Google Scholar]
- 43.Swanson DB, Barrow HS, Friedman CP. Issues in assessment of clinical competence. Prof Educ Res. 1982;4:2. [Google Scholar]
- 44.Jones TV, Gerrity MS, Earp J. Written case simulations: do they predict physicians’ behavior? J Clin Epidemiol. 1990;43:805–15. doi: 10.1016/0895-4356(90)90241-g. [DOI] [PubMed] [Google Scholar]
- 45.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283:1715–22. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 46.Salem-Schatz S, Moore G, Rucker M, Pearson SD. The case for case-mix adjustment in practice profiling. JAMA. 1994;272:871–4. [PubMed] [Google Scholar]
- 47.Cowen ME, Zodet MW. Methods for analyzing referral patterns. J Gen Intern Med. 1999;14:474–80. doi: 10.1046/j.1525-1497.1999.06368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


