Abstract
Background
Whether there is an association between depression at the time of acute myocardial infarction and subsequent risk of cardiac complications and death remains controversial. Most studies of this risk factor have been limited to patients of single institutions, and this might account for the varying results. We prospectively evaluated patients admitted to 5 tertiary care and 5 community hospitals and followed them for 1 year to measure the prevalence and prognostic impact of depressive symptoms after acute myocardial infarction.
Methods
Patients were recruited for the study by trained nurse interviewers who had documented acute myocardial infarction within 2–3 days of admission. The nurses collected information from the medical records and asked study subjects to complete the Beck Depression Inventory questionnaire during their stay in hospital and using a mailed questionnaire 30 days, 6 months and 1 year later. We obtained information on vital status for patients lost to follow-up from a central death registry.
Results
Of the 587 study subjects, 550 (94%) completed the Beck Depression Inventory at baseline and 191 (35%) had a score of 10 or more, indicating at least mild depression. Rates of depression did not vary over the follow-up period and were similar among patients admitted to tertiary care or community hospitals. Depressed patients were more likely to undergo catheterization (57% v. 47%, 95% confidence interval [CI] around the difference 0.1%–19.6%) and were more likely to undergo percutaneous coronary intervention (32% v. 24%, 95% CI around the difference 0.1%–16.2%) within 30 days of first admission to hospital. Patients with depression on admission had higher rates of a composite of cardiac complications, including recurrent ischemia, infarction or congestive heart failure during their first stay in hospital or readmission for angina, recurrent acute myocardial infarction, congestive heart failure or arrhythmia (adjusted hazard ratio 1.4, 95% CI 1.05–1.86), compared with patients who were not depressed on admission. After 1 year, death rates were higher among patients who were depressed at admission (30 patients, 16%) compared with nondepressed patients (28 patients, 8%), although the difference was not statistically significant (hazard ratio 1.3, 95% CI 0.59–3.05).
Interpretation
Depressive symptoms are common after acute myocardial infarction and are associated with a slight increase in risk of in-hospital catheterization and angiography and readmission because of cardiac complications. Death was infrequent, with no statistically significant difference between the 2 groups.
Several studies have reported that there is a high prevalence of depressive symptoms among patients after acute myocardial infarction (AMI), ranging from 15% to 32%.1,2,3,4,5 Depression has also been found in some studies to be an independent predictor of increased mortality after AMI,4,6,7,8,9,10 with the association between depression and mortality being as strong as that between mortality and important clinical predictors such as Killip class, ejection fraction or peak creatine kinase.6,9 After these results were published, it was recommended in the 1995 Canadian Cardiovascular Society guidelines on the management of acute myocardial infarction that all patients with AMI be screened with the Beck Depression Inventory (BDI) questionnaire.11
However, recent studies have challenged these findings.12,13,14,15 Mayou and colleagues found that symptoms of depression did not predict mortality up to 1 year after AMI among 347 patients.14 Similarly, Lane and colleagues found that symptoms of depression did not predict 1-year mortality among 288 patients.12,13 These and the other studies were limited because for the most part they were performed in a single tertiary care centre. The management of AMI varies markedly across regions and practice settings,16,17 as do patient characteristics that influence onset and recovery from depression, such as level of education and social support.18,19,20,21,22 Thus, the generalizability of these studies to other centres and practice settings remains questionable.
We conducted a prospective cohort study to measure the prevalence of depressive symptoms after AMI, as well as the prognostic impact of depression after AMI, among 550 patients admitted to 5 tertiary care and 5 community hospital settings.
Methods
This is an ancillary study to a prospective cohort study of quality of life after AMI.16 Patients enrolled in the study were treated in a coronary care unit for AMI at 1 of 10 hospitals in Quebec between Dec. 28, 1996, and Nov. 1, 1998. The study hospitals included 5 tertiary care and 5 community hospitals, which are listed at the end of the article. It has previously been shown that the participating hospitals were similar to hospitals of the same practice setting across Quebec in terms of characteristics such as total number of admissions for AMI and total numbers of cardiac procedures performed.23 Any patient admitted to one of the study hospitals was deemed eligible for the study if he or she had sustained a Q-wave or non-Q-wave AMI and had survived up to 24 hours after hospital admission. As the design of the original study involved the grouping of patients based on the practice setting of the initial hospital of admission, eligible patients had to be admitted through the emergency department and could not have been transferred from another hospital. In order to ensure complete follow-up, patients also had to be able to read and understand French or English, and they were excluded if they were physically incapable of responding to a questionnaire (e.g., they were intubated) or unable to give informed consent. This study received ethical approval from the Montreal General Hospital Ethics Review Board.
The procedures for the collection of data for this study have been described previously.16 Briefly, research nurses approached eligible patients for enrolment within 2–3 days after the date of admission. The research nurses conducted chart reviews for each study subject in order to record data on demographic and clinical characteristics at the time of enrolment (baseline) and information on the course of treatment up to the time of discharge. Study subjects completed a self-administered questionnaire at baseline and were mailed questionnaires at 30 days, 6 months and 1 year after baseline. These questionnaires measured subjects' symptoms of depression using the previously validated BDI questionnaire.24,25 For each BDI questionnaire, patients were asked to relate their responses to their perception of their health status during the preceding 2 weeks. For the questionnaires delivered at 30 days, 6 months and 1 year, patients were also asked to report details about all admissions to hospital that had occurred since the date of last contact. A chart review was performed for any patients who reported an emergency department visit, readmission to hospital or a cardiac procedure. Patients who did not respond to the mail survey were contacted by telephone for an interview. Vital status 1 year post AMI was obtained from a central death registry for all patients who were lost to follow-up.
The BDI was designed to assess the intensity of 21 depressive symptoms and attitudes.24,25 Each item of the questionnaire ranks 1 of the 21 symptoms and attitudes on a scale of 0–3, with a higher score representing a higher intensity. The 21 symptoms and attitudes are as follows: (1) mood, (2) pessimism, (3) sense of failure, (4) lack of satisfaction, (5) guilt feelings, (6) sense of punishment, (7) self-dislike, (8) self-accusation, (9) suicidal wishes, (10) crying, (11) irritability, (12) social withdrawal, (13) indecisiveness, (14) distortion of body image, (15) work inhibition, (16) sleep disturbance, (17) fatiguability, (18) loss of appetite, (19) weight loss, (20) somatic preoccupation and (21) loss of libido. When scoring the questionnaire, the ranks for each item are added, resulting in a continuous scale from 0 to 63, with a higher score representing a higher level of depression. Steer and Beck26 have set guidelines for cut-off scores used to classify the extent of a patient's depressive symptoms: a score of < 10 means no or minimal depression; 10–17 is mild-to-moderate depression; 18–29 is moderate-to-severe depression; and severe depression is 30–63. Previous studies of depression after AMI have classified patients with a BDI score of ≥ 10 as having at least mild-to-moderate depression.1,4,5,6,8,9,12,13,27,28,29 For comparability with these previous studies, we used the same classification scheme in this study.
After determining the prevalence of depression at baseline, 30 days, 6 months and 1 year, we compared summary statistics for all demographic and clinical variables for patients who were depressed with those who were not depressed at baseline. Aspects of care potentially associated with psychosomatic disorders and clinical outcomes were also compared for patients who were depressed with those who were not depressed at baseline. The aspects of care compared were the cumulative incidence of invasive cardiac procedures at 30 days and 1 year, the proportions of patients taking cardiac and psychotropic medications at 1 year and the mean number of outpatient physician visits between 6 months and 1 year. Data on use of medications and physician visits were reported by the patients in the 1-year questionnaire. The outcomes compared were the cumulative incidence of cardiac complications during the initial admission to hospital, as well as the cumulative incidence of readmissions for cardiac complications and mortality over the course of follow-up.
We used Cox proportional hazards models to examine the association between depression at baseline and mortality within 1 year after AMI. We also created models to examine the association between depression at baseline and the incidence of a cardiac complication within 1 year after AMI. To define the variable describing incidence of cardiac complications, we determined whether patients experienced a cardiac complication in-hospital (recurrent ischemia, recurrent infarction or congestive heart failure) or if they were readmitted for a cardiac complication post discharge (angina, recurrent AMI, congestive heart failure or arrhythmia). All models were adjusted for baseline clinical and demographic characteristics shown in previous studies to predict mortality after AMI30 (age at admission, history of a previous AMI, anterior location of infarct, diabetes, hypertension and current smoking at baseline), as well as variables identified a priori as potential confounders (sex, history of previous angina).
Finally, we also examined whether the impact of depression after AMI on the incidence of mortality and cardiac complications was similar for patients treated at tertiary care and community hospitals. To do so, the interaction between depression at baseline and admission to a tertiary care hospital was examined by including an interaction term in the full models.
Results
Of the 587 study patients, 550 (94%) completed the BDI questionnaire at baseline, whereas 466, 464 and 486 completed the BDI at 30 days, 6 months and at 1 year post AMI respectively. When compared with baseline (35%), the overall prevalence of depressive symptoms increased slightly at 30 days (39%) and 6 months (39%), but decreased by 1 year (30%). However, on average, patients' BDI scores did not change substantially over the follow-up period. Of the patients who were depressed at baseline, 70% were also depressed at 30 days. Of the patients who were not depressed at baseline, only 24% became depressed at 30 days. The prevalence of depressive symptoms over the follow-up period did not vary according to the practice setting of admission.
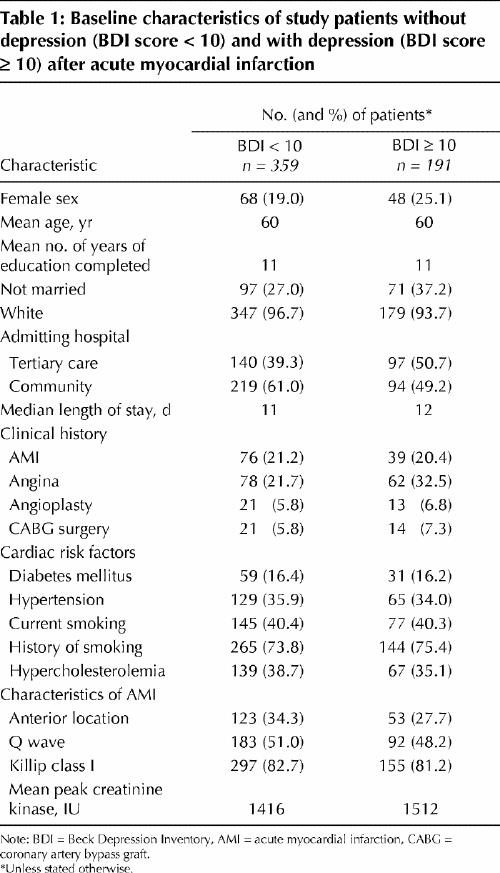
Overall, the baseline demographic and clinical characteristics were similar for patients who were depressed and those who were not depressed at baseline (Table 1). The only notable difference in demographic characteristics was that a greater proportion of patients who were depressed were female (25% v. 19%, 95% confidence interval [CI] around the difference –0.9% to 13.8%) or were not married or living as married (37% v. 27%, 95% CI around the difference 1.9%–18.3%). Notable differences in clinical characteristics were that a greater proportion of patients who were depressed had a history of angina (32% v. 22%, 95% CI around the difference 2.7%–18.9%). However, other indicators of AMI severity did not differ between the 2 groups.
Table 1
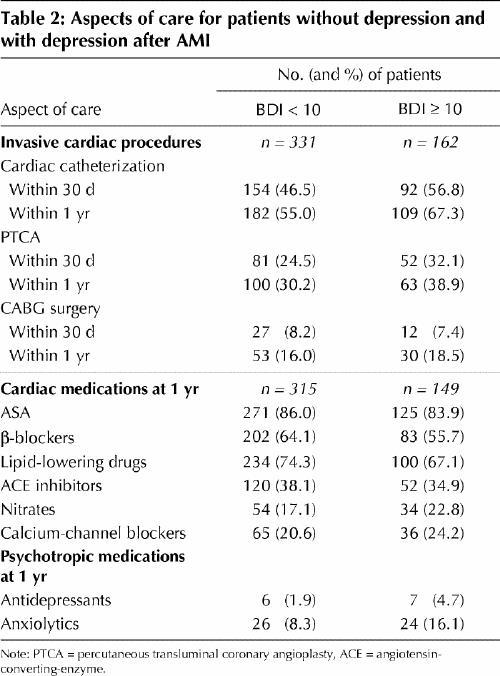
There were differences in aspects of care between patients who were depressed and those who were not depressed at baseline in terms of invasive cardiac procedures, cardiac and psychotropic medications received and physician visits (Table 2). For example, patients who were depressed at baseline received more cardiac catheterization (57% v. 47%, 95% CI around the difference 0.1%–19.6%) and percutaneous transluminal coronary angioplasty (32% v. 24%, 95% CI around the difference 0.1%–16.2%) within 30 days of admission. These trends also held at 1 year. Patients who were depressed at baseline were also less likely to be taking β-blockers (56% v. 64%, 95% CI around the difference –18.0% to 1.2%) or lipid-lowering drugs (67% v. 74%, 95% CI around the difference –16.1% to 1.8%) and were more likely to be taking a psychotropic medication (antidepressant: 5% v. 2%, 95% CI around the difference –0.9% to 6.5%; anxiolytic: 16% v. 8%, 95% CI around the difference 1.2%–14.5%) at 1 year. In addition, patients who were depressed at baseline had a slightly higher frequency of visits to internists (average of 0.4 v. 0.3 visits) and psychiatrists or psychologists (average of 0.4 v. 0.1 visits) between 6 months and 1 year. This difference was not significant.
Table 2
During the initial stay in hospital, a slightly greater proportion of patients who were depressed had an episode of recurrent ischemia (25% v. 20%, 95% CI around the difference –2% to 13%) and/or congestive heart failure (13% v. 8%, 95% CI around the difference –1% to 10%) (Table 3). However, there were no differences between the 2 groups in terms of other cardiac complications, such as recurrent AMI (3% v. 2%, 95% CI around the difference –2% to 4%). Patients who were depressed at baseline also had higher rates of readmission because of angina (22% v. 13%, 95% CI around the difference 2%–17%) and a higher composite index of readmission because of cardiac complications (31% v. 18%, 95% CI around the difference 5%–22%) over the follow-up period. After adjusted analyses, depression remained associated with higher rates of cardiac complications over the 1-year follow-up period (hazard ratio 1.4, 95% CI 1.05–1.86). Fig. 1 shows Kaplan–Meier curves for incidence of complications for patients who were depressed and those who were not depressed at baseline.
Table 3
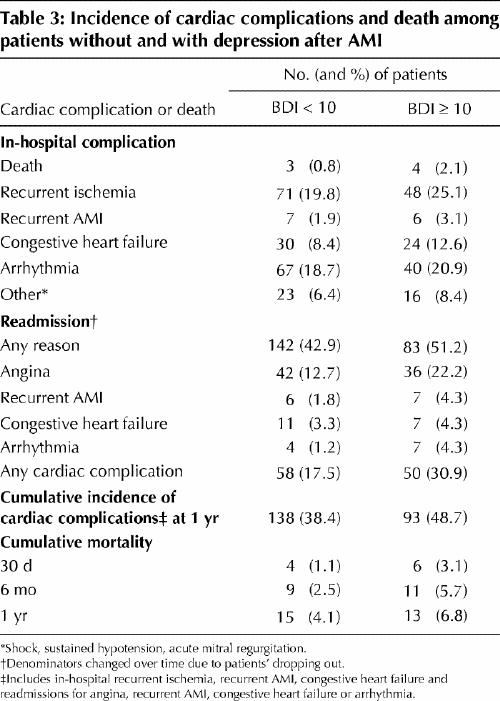
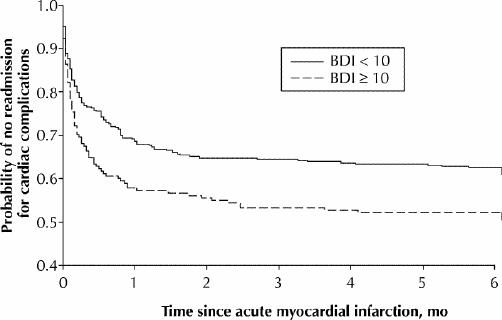
Fig. 1: Kaplan–Meier survival curves showing probability of no readmission to hospital because of unstable angina, recurrent acute myocardial infarction, pulmonary edema, arrhythmia or congestive heart failure for patients who were either depressed (Beck Depression Inventory [BDI] ≥ 10) or not depressed (BDI < 10). Log-rank statistic for differences between curves p = 0.01. Note that the differences persisted to 12 months.
Although we found an association between depression at baseline and cardiac complications, we did not find an association between depression at baseline and mortality. The unadjusted incidence of mortality was slightly, but not significantly, higher for patients who were depressed at baseline, both at 6 months (6% v. 3%, 95% CI around the difference –0.4% to 7%) and at 1 year (7% v. 4%, 95% CI around the difference –2% to 7%) (Table 3). Similarly, in adjusted analyses, depression was not associated with mortality over the 1-year follow-up period (hazard ratio 1.3, 95% CI 0.59–3.05). Fig. 2 shows Kaplan–Meier survival curves for patients who were depressed and those who were not depressed at baseline.
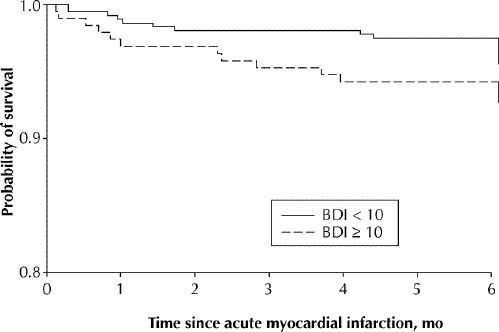
Fig. 2: Kaplan–Meier survival curves for patients who were either depressed (BDI ≥ 10) or not depressed (BDI < 10). Log-rank statistic for differences between curves p = 0.15. Note that the differences persisted to 12 months.
Finally, there was also no evidence of an interaction between depression at baseline and admission to tertiary care hospitals, nor was any association found with the incidence of cardiac complications or mortality.
Interpretation
We did not find an association between symptoms of depression measured shortly after admission because of AMI and mortality within 1 year. Previous studies found that post-AMI depressive symptoms were associated with increased mortality after adjusting for known prognostic variables such as Killip class and severity of AMI, with odds ratios as high as 3.6 (95% CI 1.68–6.70)5 or a relative risk of 2.6 (p = 0.06).9 Our data do not support these conclusions, and it should be noted that the prevalence of depressive symptoms in our study was comparable to those of previous studies, while our study population was larger.
However, we did find a higher incidence of readmission because of cardiac complications among patients who reported depressive symptoms. These readmissions appeared to be attributable to angina for the most part and did not appear to be attributable to recurrent AMI. As suggested in previous studies, this association could represent some direct effect of depressive symptoms on the cardiovascular system, mediated by endogenous neurohormonal activation, endothelium dysfunction, decreased heart rate variability or other unknown mechanisms.3,31 More likely, and as reported recently by Mayou and colleagues,14 it could just be a reflection of a more severe anxious state, with patients post AMI having an increased propensity to experience and report different kinds of symptoms akin to angina.
Interestingly, we found a high prevalence of depressive symptoms at baseline and little change in depressive symptoms over the 1-year follow-up period. These results suggest that most patients' post-AMI depressive symptoms were probably present before the AMI admission and were not a direct consequence of the AMI event. It should also be noted that rates of use of psychotropic medications, and especially antidepressants, were low overall despite the overall high prevalence of depressive symptoms. Consistent with previous studies,32,33 this finding suggests potential underdiagnosis and undertreatment of depression before and after AMI.
Finally, the practice setting of the hospital of admission does not appear to play a role in the prevalence or prognostic impact of post-AMI depressive symptoms. Patients with AMI admitted to community hospitals are more likely to be treated by general practitioners than patients admitted to tertiary care hospitals. We had hypothesized that because general practitioners are more familiar with the screening and treatment of depression compared with cardiologists, such familiarity might lead to better behavioural and pharmacological intervention at community hospitals. In turn, this treatment might lead to better prognosis. The findings of this study refute this hypothesis.
Several potential limitations to the study must be considered. First, patients who died shortly after admission were not enrolled in this study and post-AMI mortality rates were low. Thus, the study may have been underpowered to detect differences in mortality, despite the fact that our study enrolled over 500 patients. However, in comparison with previous studies showing a relation between depression and post-AMI mortality, our study had the same design, more than twice the number of patients and about the same prevalence of depressive symptoms. If depressive symptoms were of a substantially prognostic importance, we would expect to have found as strong an impact of depression on mortality as in the previous studies. Thus, it is unlikely that depression has a strong impact on mortality after AMI. A second limitation is that the exclusion criteria resulted in the exclusion of the sickest patients with AMI, who could be expected to be the most depressed and to have the highest death and complication rates. These exclusions restrict the generalizability of our results to healthier patients but probably do not affect the internal validity of the study. Moreover, we found a prevalence of depression to a degree similar to that of previous studies. One final limitation is that this study relied upon the BDI as a measure of depressive symptoms. Structured clinical interviews, such as the “Diagnosis Interview Schedule,”34 could have been useful to confirm the diagnosis of minor or major depression obtained by the BDI. However, previous studies have demonstrated that the BDI is sensitive and specific1 and also a better measure of the prognostic impact of depression.6
In conclusion, there is a high prevalence of depressive symptoms post AMI. Patients with depressive symptoms tend to have a higher incidence of cardiac complications, as they present with more chest pain. However, they do not appear to have a higher incidence of mortality. Nevertheless, although depressive symptoms are not clearly associated with mortality after AMI, because of their high prevalence and impact on the heath care system, as well as a potential negative impact on quality of life, screening for in-hospital identification and treatment of depression is recommended. The results of this study and other recent publications also warrant a larger, multicentre study to determine more precisely the prognostic impact of post-AMI depressive symptoms.
β See related article page 570
Participating study hospitals and investigators: Tertiary care hospitals: Montreal General Hospital, Montréal, Que. (Dr. Thao Huynh, Dr. Louise Pilote); Sir Mortimer B. Davis Jewish General Hospital, Montréal, Que. (Dr. Jean G. Diodati, Dr. Mark J. Eisenberg); Hôpital Notre-Dame, Montréal, Que. (Dr. Normand Racine); Royal Victoria Hospital, Montréal, Que. (Dr. François Charbonneau); Complexe hospitalier de la Sagamie, Chicoutimi, Que. (Dr. Claude Levesque); Community hospitals: Centre hospitalier de la région de l'Amiante, Thetford Mines, Que. (Dr. Claude Lauzon); Centre hospitalier régional du Grand Portage, Rivière-du-Loup, Que. (Dr. Susanne Carignan); Centre hospitalier Beauce Etchemin, Saint-Georges, Que. (Dr. Danielle Dion); Hôpital Sainte-Croix de Drummondville, Drummondville, Que. (Dr. René Roux); Centre hospitalier de Val d'Or, Val d'Or, Que. (Dr. Joël Pouliot).
Acknowledgments
Dr. Pilote is an Investigator of the Canadian Institutes of Health Research (CIHR).
Footnotes
This article has been peer reviewed.
Contributors: All authors contributed substantially to the conception and design of the study; data acquisition, analysis and interpretation; and to writing the manuscript. All authors approved the final version to be published.
The study was supported by a grant from the Fonds de la Recherche en Santé du Québec (grant no. 961305-104).
Competing interests: None declared.
Correspondence to: Dr. Louise Pilote, Division of Clinical Epidemiology, Montreal General Hospital, 1650 Cedar Ave., Montréal QC H3G 1A4; fax 514 934-8293; louise.pilote@mcgill.ca
References
- 1.Carney RM, Rich MW, Tevelde AJ, Saini J, Clark K, Jaffe AS. Major depressive disorders in coronary artery disease. Am J Cardiol 1987;60:1273-5. [DOI] [PubMed]
- 2.Schleifer SJ, Macari-Hinson NM, Coyle DA, Slater WR, Kahn M, Gorlin R, et al. The nature and course of depression following myocardial infarction. Arch Intern Med 1989;149:1785-9. [PubMed]
- 3.Fielding R. Depression and acute myocardial infarction: a review and reinterpretation. Soc Sci Med 1991;32:1017-27. [DOI] [PubMed]
- 4.Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6 month survival. JAMA 1993;270:1819-25. [PubMed]
- 5.Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, Talajic M, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation 2000;101:1919-24. [DOI] [PubMed]
- 6.Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation 1995;91:999-1005. [DOI] [PubMed]
- 7.Ahern DK, Gorkin L, Anderson JL, Tierney C, Hallstrom A, Ewart C, et al. Biobehavioral variables and mortality or cardiac arrest in the Cardiac Arrhythmia Pilot Study (CAPS). Am J Cardiol 1990;66:59-62. [DOI] [PubMed]
- 8.Lespérance F, Frasure-Smith N, Talajic M. Major depression before and after myocardial infarction: its nature and consequences. Psychosom Med 1996; 58 : 99-110. [DOI] [PubMed]
- 9.Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens S, Zahalsky H, et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol 2001;88:337-41. [DOI] [PubMed]
- 10.Moser DK, Dracup K. Is anxiety early after myocardial infarction associated with subsequent ischaemic and arrhythmic events? Psychosom Med 1996; 58:395-401. [DOI] [PubMed]
- 11.Fallen EL, Cairns J, Dafoe W, Frasure-Smith N, Genest J Jr, Massel D, et al. Treatment of patients with myocardial infarct: a consensus report — revision of the 1991 guidelines issued by the Canadian Society of Cardiology. Can J Cardiol 1995;11:477-86. [PubMed]
- 12.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Mortality and quality of life 12 months after myocardial infarction: effects of depression and anxiety. Psychosom Med 2001;63:221-30. [DOI] [PubMed]
- 13.Lane D, Carroll C, Ring C, Beevers DG, Lip GY. Do depression and anxiety predict recurrent coronary events 12 months after myocardial infarction? Q J Med 2000;93:739-44. [DOI] [PubMed]
- 14.Mayou RA, Gill D, Thomson DR, Day A, Hicks N, Volmink J, et al. Depression and anxiety as predictors of outcomes after myocardial infarction. Psychosom Med 2000;62:212-9. [DOI] [PubMed]
- 15.Berkman LF, Leo-Summers L, Horwitz RL. Emotional support and survival after myocardial infarction: a prospective, population-based study of the elderly. Ann Intern Med 1992;117:1003-9. [DOI] [PubMed]
- 16.Pilote L, Lauzon C, Huynh T, Dion D, Roux R, Racine N, et al. Quality of life after acute myocardial infarction among patients treated at sites with and without on-site availability of angiography. Arch Intern Med 2002;162(5):553-9. [DOI] [PubMed]
- 17.Cox JL, Chen E, Naylor CD. Revascularization after acute myocardial infarction: impact of hospital teaching status and on-site invasive facilities. J Gen Intern Med 1994;9:674-8. [DOI] [PubMed]
- 18.Lebovits BZ, Swhekelle RB, Otsfeld AM, Paul O. Prospective and retrospective psychological studies of coronary heart disease. Psychosomatic Med 1967; 29(3):265-72. [DOI] [PubMed]
- 19.Brackett CD, Powell LH. Psychosocial and physiological predictors of cardiac death after healing of acute myocardial infarction. Am J Cardiol 1988;61:979-83. [DOI] [PubMed]
- 20.Ragland DR, Brand RJ. Type A behavior and mortality from coronary heart disease. N Engl J Med 1988;318:65-9. [DOI] [PubMed]
- 21.Ruberman W, Weinblatt E, Goldberg JD, Chaudhary BS. Psychosocial influences on mortality after myocardial infarction. NEngl J Med 1984;311:522-9. [DOI] [PubMed]
- 22.Case RB, Moss AJ, Case N, McDermott M, Eberly S. Living alone after myocardial infarction. Impact on prognosis. JAMA 1992;267:515-9. [PubMed]
- 23.Beck CA, Lauzon C, Eisenberg MJ, Huynh T, Dion D, Roux R, et al. Discharge prescriptions following admission for acute myocardial infarction at tertiary care and community hospitals in Quebec. Can J Cardiol 2001;17:33-40. [PubMed]
- 24.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561-71. [DOI] [PubMed]
- 25.Beck AT, Steer RA. Beck depression inventory manual. San Antonio (TX): The Psychological Corporation, Harcourt-Brace-Jovanovich; 1987.
- 26.Steer RA, Beck AT. Beck depression inventory. Dictionary of behavioural assessment techniques. New York: Pergamon Press; 1988.
- 27.Lespérance F, Frasure-Smith N, Juneau M, Theroux P. Depression and 1-year prognosis in unstable angina. Arch Intern Med 2000;160:1354-60. [DOI] [PubMed]
- 28.Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161: 1849-56. [DOI] [PubMed]
- 29.Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, et al. Depression and health-care costs during the first year following myocardial infarction. J Psychosom Res 2000;48:317-20. [DOI] [PubMed]
- 30.Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, et al. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. Circulation 1995;91:1659-68. [DOI] [PubMed]
- 31.Carney RM, Rich MW, te Velde A, Saini J, Clark K, Freedland KE. The relationship between heart rate, heart rate variability and depression in patients with coronary artery disease. J Psychosom Res 1988;32:159-64. [DOI] [PubMed]
- 32.Reedland KE, Lustman PJ, Carney RM, Hong BA. Underdiagnosis of depression in patients with coronary artery disease: the role of non-specific symptoms. Int J Psychiatry Med 1992;22:221-9. [DOI] [PubMed]
- 33.Lavoie KL, Fleet RP. The impact of depression on the course and outcome of coronary artery disease: review for cardiologists. Can J Cardiol 2000;16:653-62. [PubMed]
- 34.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry 1981;38:381-9. [DOI] [PubMed]


