Abstract
OBJECTIVE
The purpose of this study was to determine the predictors of referral and enrollment, including racial differences, in phase 2 cardiac rehabilitation programs among African-American and white women who are eligible for such programs.
DESIGN
Prospective longitudinal design.
SETTING
One large academic medical center and two large community hospitals.
PATIENTS
A total of 253 women (108 African American, 145 white) were surveyed within the first month of discharge from the hospital for a percutaneous coronary intervention, coronary artery bypass surgery, or myocardial infarction without revascularization. A total of 234 (99 African American, 135 white) completed the 6-month follow-up.
MAIN RESULTS
The rate of referral to outpatient phase 2 cardiac rehabilitation was significantly lower for African-American women compared with white women, 12 (12%) versus 33 (24%) (P = .03). Only 35 (15%) of women in the study reported enrollment in phase 2 cardiac rehabilitation programs, with fewer African-American women reporting enrollment compared with white women, 9 (9%) versus 26 (19%) (P = .03). Controlling for age, education, angina class, and comorbidities, women with annual incomes <$20,000 were 66% less likely to be referred to cardiac rehabilitation (P = .01) and 60% less likely to enroll compared to women with incomes >$20,000 (P = .01). Although borderline significant, African-American women were 55% less likely to be referred (P = .059) and 58% less likely to enroll (P = .059) than white women.
CONCLUSIONS
We found disparities in cardiac rehabilitation program participation, with women with lower incomes less likely to be referred and to have lower enrollment rates in cardiac rehabilitation and a strong trend for African-American women to be less likely to be referred and enroll. Because almost all patients who have had an acute coronary event, with or without revascularization procedures, will benefit from cardiac rehabilitation, automatic referral systems should be considered to increase utilization and reduce disparities.
Keywords: cardiac rehabilitation, women's health, health disparities
Coronary heart disease (CHD) affects more than 50% of women, and is their major cause of disability and death.1 Cardiovascular disease accounts for more hospitalizations and health care costs than any other illness. Cardiac rehabilitation programs have been shown to reduce mortality, improve functional capacity, improve quality of life, and decrease the incidence of rehospitalization for cardiac complications and overall medical costs in both men and women.2,3 Despite the preponderance of this evidence, less than 25% of patients eligible for cardiac rehabilitation services enroll in an early outpatient cardiac rehabilitation program.4,5 The few studies that have reported gender-specific data show that women have lower attendance and higher dropout rates from outpatient cardiac rehabilitation compared with men.4–9 Although the data are limited, the dropout rate is even higher for African-American women compared with white women (49% vs 36%, respectively),10 and a national survey revealed that only 9.3% of female participants in cardiac rehabilitation programs in 1990 were nonwhite.11 These findings are striking because African-American women have a greater incidence of CHD compared with white women and hence a greater proportion are presumably eligible for cardiac rehabilitation.
Physician referral patterns, program characteristics, and patient-related factors, such as demographic, economic, health, and psychosocial factors, contribute to whether patients are referred to and whether they enroll and continue to attend cardiac rehabilitation programs.8 However, there is a paucity of research that specifically addresses the facilitators for and barriers to cardiac rehabilitation in women and whether there are racial disparities in referral and attendance. Consistent with the Healthy People 2010 goal to eliminate health disparities among segments of the population, including differences that occur by gender, race, or ethnicity,12 the purpose of this study was to determine the predictors of referral and enrollment, including racial differences, in phase 2 cardiac rehabilitation programs in African-American and white women who are eligible for such programs.
METHODS
This study used a prospective longitudinal design. African-American and white women were identified at the time of hospitalization for a coronary event. They were interviewed by telephone within the first 4 weeks following their hospital discharge to collect baseline sociodemographic and clinical data. They were interviewed again 6 months later by telephone to obtain information on referral to and enrollment in cardiac rehabilitation programs, and information on psychosocial and behavioral factors that may be associated with rehabilitation utilization. Interviews were conducted by three trained research assistants who recorded responses directly onto questionnaire forms that were optically scanned directly into a database.
Study Population
The census records of three participating hospitals were reviewed daily to identify possible study candidates. Women were eligible if they were African American or white and were hospitalized with a diagnosis of myocardial infarction (MI) or had undergone coronary artery bypass graft surgery (CABG) or percutaneous coronary intervention, and qualified for cardiac rehabilitation according to the criteria of the American College of Sports Medicine13 and the American Association of Cardiovascular and Pulmonary Rehabilitation.14 Women were excluded if they had a major noncardiac comorbidity with a poor prognosis, recent history of uncontrolled psychiatric or substance abuse disorder, or no telephone. Consecutive, eligible patients were recruited between March 2001 and January 2002.
The participating hospitals were a large academic medical center and two large community hospitals that serve patients from Baltimore city and its surrounding counties. Each of these hospitals serves a large number of African-American and white women with CHD. One of the community hospitals has an outpatient cardiac rehabilitation center located on site, while the other two have cardiac rehabilitation centers located at nearby wellness centers.
Conceptual Framework
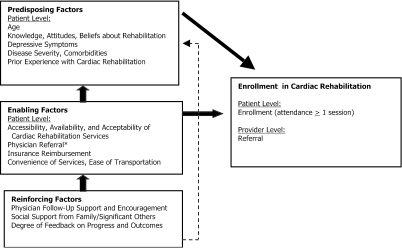
The selection of variables of interest was guided by the PRECEDE-PROCEED model,15 which is an ecological conceptual framework that integrates psychosocial, behavioral, and environmental factors relevant to women's enrollment in cardiac rehabilitation at multiple levels (patient provider, system). Predisposing factors are antecedents to behavior that provide the rationale or motivation; enabling factors are antecedents to behavior that facilitate a motivation to be realized; and reinforcing factors are subsequent to a behavior that provide continuing reward or incentive for the behavior and contribute to its persistence or repetition.15Figure 1 illustrates the conceptual framework to organize the three sets of factors influencing cardiac rehabilitation utilization. The factors selected for study were identified from a systematic review of relevant research.16
FIGURE 1.
Based on PRECEDE-PROCEED model. Provider referral is theorized as both a predictor of patient enrollment in cardiac rehabilitation as well as an outcome. (Adapted with permission from Health Promotion Planning: An Educational and Environmental Approach.15)
Measures
Predictor variables included predisposing, enabling, and reinforcing factors hypothesized as being related to the outcomes. Sociodemographics, disease severity, comorbidities, depression, and physical functioning were measured at baseline, approximately 1 month after discharge from the hospital. Sociodemographic variables included age in years, self-identified race (either white or African American), education in years, income, and marital status. Measures of disease severity included frequency and grade of angina and length of cardiac disability. Angina was classified according to the Canadian Cardiovascular Society Classification grading for angina [pectoris].17 Length of preoperative disability was assessed as a self-reported measure of the number of months the patient had experienced decreased functioning due to cardiac disease symptoms.
Comorbidity was assessed by the Charlson Comorbidity Index, a weighted comorbidity index that takes into account both the number and seriousness of comorbid diseases.18 The adjusted relative risks were employed as weights for the different comorbid diseases. The index is the summation of these weights and ranges from 0 (no comorbid disease) to 36 (severe comorbid disease).
Physical functioning was measured at baseline using the physical role function subscale of the Beth Israel Functional Status Questionnaire (FSQ).19 Questions on the physical function subscale measure the person's degree of difficulty in carrying out intermediate activities of daily living. The scores range from 0 to 100, with a higher score indicating higher functional ability. The psychometric properties have been assessed in cohorts of ambulatory patients reporting an internal consistency reliability of 0.82 and significant correlations with variables believed to be related to function.
Depression was measured at baseline by the Center for Epidemiologic Studies Depression Scale (CES-D), a short self-report scale designed to measure depressive symptomatology in the general population.20 Scores of 16 or more are commonly defined as indicative of depression.21 Radloff reported α coefficients of 0.85 for general population samples and of 0.90 for a patient sample.20
The primary dependent variables were referral to and enrollment in phase 2 outpatient cardiac rehabilitation. Referral was defined as the woman's self-report of a health care professional's recommendation for cardiac rehabilitation. Enrollment was defined as self-reported registration and attendance at a minimum of 1 session in an outpatient cardiac rehabilitation program. Data on each of these outcomes were collected at the time of the 6-month follow-up survey.
The 6-month follow-up telephone interview also included a series of questions to assess additional predisposing, reinforcing and enabling factors that may be associated with referral to and enrollment in cardiac rehabilitation. The questions were adapted from a prior study of women's preferences for cardiac rehabilitation program elements22 and questions designed by the investigators. An early draft of the telephone interview was reviewed for content, question format, and organization by a volunteer group of community advisors. The group included 1 African-American and 3 white women who had a prior cardiac event and were eligible for rehabilitation, a cardiologist, a cardiac rehabilitation nurse, and a Medicare reimbursement specialist. The final list of questions was based on this feedback and a pilot-test in a sample of 5 women.
The 6-month interview assessed the receipt of a referral from self-report of the patient, including the patient's recall of having received a verbal or written referral by a health professional at any time since being hospitalized. For those who reported receiving a referral, the reinforcing factors of the patient's perception of the strength of the health professional's and family/significant others’ encouragement to participate in cardiac rehabilitation was measured using a scale of 1 (little or no encouragement) to 10 (strongly encouraged). Enabling factors such as the accessibility, availability, and acceptability of cardiac rehabilitation services were assessed. Women who did not enroll were asked to respond whether a list of 33 factors, such as paying for the program, a doctor's advice, and transportation, were factors in their decision not to attend. Predisposing factors to participation such as knowledge/awareness of the benefits of cardiac rehabilitation programs and knowledge of insurance reimbursement and prior experience with cardiac rehabilitation also were assessed.
Statistical Analysis
Descriptive and univariate statistics were used to examine the distribution of all variables. Multivariate logistic regression analysis was used to develop models to determine the predictors of referral to and enrollment in cardiac rehabilitation. The relative odds of enrolling and 95% confidence intervals were calculated. Variables included in the regression models included income (<$20,000 vs ≥$20,000), race (African American vs white), education (≤ high school vs > high school), and angina class, age, and comorbidities as continuous variables. Interaction terms were examined to determine whether the effect of covariates remained constant over groups. These analyses were performed using SAS, Windows version 5.0 (SAS Institute, Cary, NC).
RESULTS
Sample Characteristics
A total of 253 women were enrolled at baseline. Their demographic characteristics and medical history are presented in Table 1. Forty-three percent were African American, 64% were high school graduates, and almost half had annual household incomes less than $20,000. The majority (59%) had undergone a percutaneous coronary intervention procedure for unstable angina or MI, 26% had undergone CABG, and only 15% had experienced an MI without revascularization. Almost two thirds of the women reported no angina prior to their hospitalization, while greater than one third reported class 3 or 4 angina. All of the 253 women (145 white and 108 African American) who consented to participate completed the baseline interviews (100% response rate) and 234 women (135 white and 99 African American) completed the 6-month follow-up (92% response rate). There were no statistically significant differences between the women who did and did not complete the 6-month interview. White women were older, had more years of education, reported higher income, fewer comorbidities, and less angina compared with African-American women. Depression was not significantly different by race. However, the mean depression scores for the total sample revealed that more than one third of women had symptoms of depression 1 month after discharge from the hospital.
Table 1.
Baseline Sample Characteristics
| Characteristic | Total (N = 253) | White (N = 145) | African American (N = 108) | >P Value |
|---|---|---|---|---|
| Mean age, y (SD) | 66 (12) | 69 (11) | 62 (12) | <.001 |
| Education ≥12 years, % | 64 | 73 | 51 | .001 |
| Married, % | 44 | 50 | 35 | .02 |
| Household income >$20,000, % | 51 | 57 | 36 | .002 |
| Comorbidity, % | ||||
| Hypertension | 75 | 70 | 82 | .04 |
| Diabetes mellitus | 43 | 35 | 54 | .003 |
| Congestive heart failure | 15 | 15 | 15 | .93 |
| Cerebrovascular disease | 14 | 8 | 21 | .003 |
| Mean comorbidity score (SD) | 2.06 (1.75) | 1.69 (1.43) | 2.56 (2.0) | <.001 |
| Mean depression score (SD) | 11.7 (10.2) | 11.2 (9.7) | 12.4 (10.9) | .362 |
| Mean functional status (SD) | 20.5 (12.7) | 21.6 (13.2) | 19.0 (11.9) | .119 |
| Type of event, % | .23 | |||
| PCI | 59 | 61 | 57 | |
| CABG | 26 | 28 | 24 | |
| MI | 15 | 12 | 19 | |
| Angina class, % | .04 | |||
| 0 (no angina) | 61 | 66 | 53 | |
| 1 to 2 | 4 | 2 | 7 | |
| 3 to 4 | 36 | 32 | 41 |
PCI, percutaneous coronary intervention; CABG, coronary artery bypass surgery; MI, myocardial infarction; SD, standard deviation.
Differences in Referral to and Enrollment in Cardiac Rehabilitation
Only 44 (19%) of the women reported receiving a referral to outpatient phase 2 cardiac rehabilitation from any health care professional. The rate of referral was lower for African-American women compared with white women, 12 (12%) versus 33 (24%) (P = .03). Only 35 (15%) of women reported enrollment in outpatient phase 2 cardiac rehabilitation programs, with fewer African-American women reporting enrollment compared to white women, 9 (9%) versus 26 (19%) (P = .03).
More than half (51%) of the women reported no knowledge of cardiac rehabilitation. Almost two thirds (61%) had no knowledge of their personal health insurance coverage for cardiac rehabilitation. However, among those who reported receiving information or referral to cardiac rehabilitation, 80% subsequently enrolled. None of the participants who reported no referral subsequently enrolled in cardiac rehabilitation programs.
Among the 219 women who did not enroll in cardiac rehabilitation, the most common reason was lack of a referral or follow-up after discharge (Table 2). This lack of this enabling factor was more prevalent in African-American women. Some of the other reasons for not enrolling included feeling too sick, the belief that they either did not need cardiac rehabilitation or could exercise on their own, or they were too busy to attend. Factors such as transportation, cost, and other characteristics of the rehabilitation services were not described as major barriers. Factors did not differ by race.
Table 2.
Barriers to Enrollment in Phase 2 Cardiac Rehabilitation Among Women Who Did Not Enroll
| Reason | Total (N = 219) n (%) | Whites (N = 123) n (%) | African American (N = 96) n (%) |
|---|---|---|---|
| No referral | 100 (46) | 49 (40) | 51 (53) |
| Illness/too sick | 39 (18) | 23 (19) | 16 (17) |
| Don't need/exercise alone | 23 (11) | 17 (14) | 6 (6) |
| Too busy | 16 (7) | 9 (7) | 7 (7) |
| Transportation | 15 (7) | 10 (8) | 5 (5) |
| Cost | 13 (6) | 10 (8) | 3 (3) |
The results of logistic regression analyses to examine demographic and clinical variables that predict referral to and enrollment in cardiac rehabilitation are shown in Table 3. Interaction terms of income and race, age and race, and education and race were included in preliminary models; however, no interactions were significant so they were not included in the final models.
Table 3.
Predictors of Referral to and Enrollment in Phase 2 Cardiac Rehabilitation
| Characteristic | Odds Ratio for Referral (95% CI) | Odds Ratio for Enrollment (95% CI) |
|---|---|---|
| Income <$20,000 | 0.34 (0.15 to 0.77)* | 0.40 (0.16 to 0.98)* |
| African-American | 0.45 (0.20 to 1.03)† | 0.42 (0.17 to 1.04)† |
| Younger age‡ | 0.99 (0.97 to 1.03) | 0.99 (0.96 to 1.03) |
| ≤ High school education | 0.66 (0.32 to 1.37) | 0.64 (0.29 to 1.42) |
| Less angina‡ | 0.99 (0.81 to 1.20) | 1.03 (0.84 to 1.28) |
| More comorbidities‡ | 1.19 (0.97 to 1.47) | 1.16 (0.93 to 1.45) |
P ≤ .05.
P= .059.
Entered as continuous variables: age in 1-year increments; angina in 1-level increments of I to IV; comorbidities in 1-point increments of 0 to 36.
CI, confidence interval.
Controlling for age, education, angina class, and comorbidities, women with annual incomes <$20,000 were 66% less likely to be referred to cardiac rehabilitation compared to women with incomes >$20,000 (P = .01). African American women were 55% less likely to be referred, although borderline significant (P = .059).
Predictors of enrollment in cardiac rehabilitation produced similar results. Women with incomes <$20,000 were 60% less likely to enroll compared to those with incomes >$20,000 (P = .05) and although borderline significant, African-American women were 58% less likely to enroll than white women (P = .059).
DISCUSSION
This study provides one of the largest women-only examination of potential disparities by race in referral to cardiac rehabilitation and enrollment. Furthermore, it explores multiple sociodemographic, clinical, psychosocial, and structural factors that may be associated with these disparities using an internationally recognized ecological conceptual framework.15 The present results confirm trends on predictors of referral and rates of enrollment that were observed in subsets of women and minorities that were participants in studies that included a predominance of white and male patients.16
The receipt of a referral or a recommendation from a health professional has been a consistently important predictor of enrollment in cardiac rehabilitation in prior studies.4,5,8,23–25 The majority of our women (80%) who reported receiving information about cardiac rehabilitation from a health professional also reported enrolling in a program. However, only about one half of the women reported any knowledge of cardiac rehabilitation when asked 6 months after their hospital discharge, and less than 20% actually reported receiving a referral to enroll in a program. Being informed about the availability of cardiac rehabilitation services and receiving a referral to enroll seem to be critical predisposing and enabling factors for women to utilize this vital intervention.
Although younger persons are more likely to receive a referral for cardiac rehabilitation,26,27 women who actually enroll in programs tend to be older.11,28 In our study, African Americans were significantly younger than the whites, though they were 55% less likely to be referred to cardiac rehabilitation than white women. We also found that age was not a significant predictor of referral or enrollment in the final regression models. The present overall enrollment rate of 15% is consistent with prior reports for eligible women.4,26
There was a trend for less referral and enrollment of African-American women. The proportion of women who actually received a referral or who enrolled was relatively small, which likely reduced statistical power for some of the predictor variables. One other study11 found that women with a recent myocardial infarction or bypass surgery were less likely than men to be referred, but women with a diagnosis of angina were more likely to be referred; other studies have found no gender differences with regard to diagnosis or type of event/procedure.23,29
Although cost was not described as a significant barrier by those who did not enroll in cardiac rehabilitation, income was a significant predictor of both referral and enrollment in our study. This finding agrees with the results of a systematic literature review of 15 studies identifying factors associated with cardiac rehabilitation attendance, which reported that nonattenders were more likely to have lower incomes.28
The presence of depression may be a variable worthy of further study. Although there were no racial differences in levels of depression and depression scores did not predict referral or enrollment, 33% of the women had scores on the CES-D indicative of mild to severe depression. Results of other studies of depression after myocardial infraction have found similar prevalence rates for mild to moderate depression,30 associations between higher levels of depression and higher mortality in older adults,31 and that depressed patients have less adherence to recommended behavior and lifestyle changes intended to reduce risk of subsequent cardiac events.32 There may be a need for clinicians to systematically assess the mental health of women after a cardiovascular disease event and direct them to appropriate therapeutic services.
This study has several limitations. The data collection relied upon women's self-report of referral and enrollment and we were not able to verify whether a referral was or was not issued, presenting the potential for recall bias. We used a convenience sample that was limited to white and African-American women because these are the two populations in Baltimore in sufficient numbers to be able to have adequate statistical power for group analysis. It is possible that the women sampled for this study are not representative of all women who qualify for cardiac rehabilitation, especially in other areas of the country or those without telephones. Future studies should explore cardiac rehabilitation disparities among other populations such as Hispanics, Asians, and Native Americans, as the burden of cardiovascular disease is prevalent across ethnic categories.
Despite these limitations, the findings show that disparities in referral and encouragement for cardiac rehabilitation from health care providers exist. Because almost all patients who have had an acute coronary event, with or without revascularization procedures, will benefit from cardiac rehabilitation, automatic referral systems should be considered to increase utilization and reduce disparities in referral and participation.
Further research is needed to determine whether racial disparities in referral to and enrollment in cardiac rehabilitation remain after adjustment for socioeconomic status, although there is evidence that racial disparities do exist for other areas of cardiac care.33 A recent analysis from the Heart and Estrogen/progestin Replacement Study (HERS) revealed that African-American women less often received appropriate preventive therapy and adequate risk factor control despite a greater coronary heart disease event risk.34 Further studies are needed to focus on the reasons why African-American women seem to receive less aggressive referral and participate less in cardiac rehabilitation. Although race is a difficult social construct to study, it may have important implications for how patients perceive cardiac rehabilitation and how they are perceived by medical providers.35
Acknowledgments
The authors gratefully acknowledge funding support from the Centers for Disease Control and Prevention (grant U48/CCU309674SIP1). The authors also gratefully acknowledge the assistance of Carol Curtis, Amy Lavis, and Grace Bigelow in the collection and analysis of data and manuscript preparation.
REFERENCES
- 1.Heart and Stroke Statistical Update. Dallas, Tex: American Heart Association; 2003. [Google Scholar]
- 2.O'Connor GT, Buring JE, Yusuf S, et al. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–44. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- 3.Oldridge NB, Guyatt GH, Fischer ME, Rimm AA. Cardiac rehabilitation after myocardial infarction. Combined experience of randomized clinical trials. JAMA. 1988;260:945–50. [PubMed] [Google Scholar]
- 4.Ades PA, Waldmann ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69:1422–5. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- 5.Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–5. [PubMed] [Google Scholar]
- 6.Cannistra LB, Balady GJ, O'Malley CJ, Weiner DA, Ryan TJ. Comparison of the clinical profile and outcome of women and men in cardiac rehabilitation. Am J Cardiol. 1992;69:1274–9. doi: 10.1016/0002-9149(92)91220-x. [DOI] [PubMed] [Google Scholar]
- 7.Oldridge NB. Compliance bias as a factor in longitudinal exercise research. Osteoporosis. Sports Med. 1992;13:78–85. doi: 10.2165/00007256-199213020-00002. [DOI] [PubMed] [Google Scholar]
- 8.King KM, Teo KK. Cardiac rehabilitation referral and attendance: not one and the same. Rehabil Nurs. 1998;23:246–51. doi: 10.1002/j.2048-7940.1998.tb01794.x. [DOI] [PubMed] [Google Scholar]
- 9.Wenger NK, Speroff L, Packard B. Cardiovascular health and disease in women. N Engl J Med. 1993;329:247–56. doi: 10.1056/NEJM199307223290406. [DOI] [PubMed] [Google Scholar]
- 10.Cannistra LB, O'Malley CJ, Balady GJ. Comparison of outcome of cardiac rehabilitation in black women and white women. Am J Cardiol. 1995;75:890–3. doi: 10.1016/s0002-9149(99)80682-1. [DOI] [PubMed] [Google Scholar]
- 11.Thomas RJ, Miller NH, Lamendola C, et al. National Survey on Gender Differences in Cardiac Rehabilitation Programs. Patient characteristics and enrollment patterns. J Cardiopulm Rehabil. 1996;16:402–12. doi: 10.1097/00008483-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. Washington, DC: U.S. Government Printing Office, Healthy People 2010; 2000. November 1. [Google Scholar]
- 13.American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 6th ed. Baltimore, Md: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 14.American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation Programs. 3rd ed. Champaign, Ill: Human Kinetics; 1998. [Google Scholar]
- 15.Greene L, Kreuter M. Health Promotion Planning: An Educational and Environmental Approach. Mountain View, Calif: Mayfield Publishing Company; 1991. [Google Scholar]
- 16.Scott LA, Ben Or K, Allen JK. Why are women missing from outpatient cardiac rehabilitation programs? A review of multilevel factors affecting referral, enrollment, and completion. J Womens Health Gend Based Med. 2002;11:773–91. doi: 10.1089/15409990260430927. [DOI] [PubMed] [Google Scholar]
- 17.Campeau L. Letter: grading of angina pectoris. Circulation. 1976;54:522–3. [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Jette AM, Davies AR, Cleary PD, et al. The Functional Status Questionnaire: reliability and validity when used in primary care. J Gen Intern Med. 1986;1:143–9. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: A Self-report Depression Scale for Research in the General Population. Applied Psychological Measurement 1. 1977:385–401. [Google Scholar]
- 21.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–14. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 22.Moore SM, Kramer FM. Women's and men's preferences for cardiac rehabilitation program features. J Cardiopulm Rehabil. 1996;16:163–8. doi: 10.1097/00008483-199605000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Caulin-Glaser T, Blum M, Schmeizl R, Prigerson HG, Zaret B, Mazure CM. Gender differences in referral to cardiac rehabilitation programs after revascularization. J Cardiopulm Rehabil. 2001;21:24–30. doi: 10.1097/00008483-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Lieberman L, Meana M, Stewart D. Cardiac rehabilitation: gender differences in factors influencing participation. J Womens Health. 1998;7:717–23. doi: 10.1089/jwh.1998.7.717. [DOI] [PubMed] [Google Scholar]
- 25.Pasquali SK, Alexander KP, Coombs LP, Lytle BL, Peterson ED. Effect of cardiac rehabilitation on functional outcomes after coronary revascularization. Am Heart J. 2003;145:445–51. doi: 10.1067/mhj.2003.172. [DOI] [PubMed] [Google Scholar]
- 26.Barber K, Stommel M, Kroll J, Holmes-Rovner M, McIntosh B. Cardiac rehabilitation for community-based patients with myocardial infarction: factors predicting discharge recommendation and participation. J Clin Epidemiol. 2001;54:1025–30. doi: 10.1016/s0895-4356(01)00375-4. [DOI] [PubMed] [Google Scholar]
- 27.Bittner V, Sanderson B, Breland J, Green D. Referral patterns to a university-based cardiac rehabilitation program. Am J Cardiol. 1999;83:252–5. doi: 10.1016/s0002-9149(98)00830-3. A5. [DOI] [PubMed] [Google Scholar]
- 28.Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. 2002;16:541–52. doi: 10.1191/0269215502cr524oa. [DOI] [PubMed] [Google Scholar]
- 29.Richardson LA, Buckenmeyer PJ, Bauman BD, Rosneck JS, Newman I, Josephson RA. Contemporary cardiac rehabilitation: patient characteristics and temporal trends over the past decade. J Cardiopulm Rehabil. 2000;20:57–64. doi: 10.1097/00008483-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Frasure-Smith N, Lesperance F, Gravel G, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101:1919–24. doi: 10.1161/01.cir.101.16.1919. [DOI] [PubMed] [Google Scholar]
- 31.Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160:1761–8. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 32.Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000;160:1818–23. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]
- 33.National Academy Press. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 34.Jha AK, Varosy PD, Kanaya AM, et al. Differences in medical care and disease outcomes among black and white women with heart disease. Circulation. 2003;108:1089–94. doi: 10.1161/01.CIR.0000085994.38132.E5. [DOI] [PubMed] [Google Scholar]
- 35.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]