Abstract
OBJECTIVE
To use the ecology model of health care to contrast participation of black, non-Hispanics (blacks); white, non-Hispanics (whites); and Hispanics of any race (Hispanics) in 5 health care settings and determine whether disparities between those individuals exist among places where they receive care.
DESIGN
1996 Medical Expenditure Panel Survey data were used to estimate the number of black, white, and Hispanic people per 1,000 receiving health care in each setting.
SETTING
Physicians’ offices, outpatient clinics, hospital emergency departments, hospitals, and people's homes.
MAIN MEASUREMENT
Number of people per 1,000 per month who had at least one contact in a health care setting.
RESULTS
Fewer blacks and Hispanics than whites received care in physicians’ offices (154 vs 155 vs 244 per 1,000 per month, respectively) and outpatient clinics (15 vs 12 vs 24 per 1,000 per month, respectively). There were no significant differences in proportions hospitalized or receiving care in emergency departments. Fewer Hispanics than blacks or whites received home health care services (7 vs 14 vs 14 per 1,000 per month, respectively). After controlling for 7 variables, blacks and Hispanics were less likely than whites to receive care in physicians’ offices (odds ratio [OR], 0.65, 95% confidence interval [CI], 0.60 to 0.69 for blacks and OR, 0.79, 95% CI, 0.73 to 0.85 for Hispanics), outpatient clinics (OR, 0.73, 95% CI, 0.60 to 0.90 for blacks and OR, 0.71, 95% CI, 0.58 to 0.88 for Hispanics), and hospital emergency departments (OR, 0.80, 95% CI, 0.69 to 0.94 for blacks and OR, 0.80, 95% CI, 0.68 to 0.93 for Hispanics) in a typical month. The groups did not differ in the likelihood of receiving care in the hospital or at home.
CONCLUSIONS
Fewer blacks and Hispanics than whites received health care in physicians’ offices, outpatient clinics, and emergency departments in contrast to hospitals and home care. Research and programs aimed at reducing disparities in receipt of care specifically in the outpatient setting may have an important role in the quest to reduce racial and ethnic disparities in health.
Keywords: race, ethnicity, disparities, health services research
According to a recent report by the Centers for Disease Control (CDC), racial and ethnic minorities fare worse than nonminorities in several major health status categories, with little progress in reduction of disparities in most areas since 1990.1 For blacks and Hispanics, the incidence of infant and maternal mortality is higher, life expectancy is lower, and rates of some chronic diseases are greater than for whites.1,2 For more than 30 years, as reflected in a 2002 report by the Institutes of Medicine,3 the medical and health policy literatures have provided evidence of racial and ethnic disparities in treatment, preventive services, and access to care. In cardiac care, cancer treatment, HIV/AIDS, peripheral vascular disease, pain management, and mental health, blacks and Hispanics receive different and possibly worse care than that given to whites.3,4 Minorities are less likely to be tested for hypercholesterolemia,5 screened for cancer,6 or receive immunizations,2,7 and are more likely to be evaluated for substance abuse.8 They are also less likely to have health insurance or a usual source of care.2,9,10 Even among patients enrolled in Medicare managed care, disparities persist that are unrelated to age, gender, education, socioeconomic status, geography, income, and health plan type.11 Researchers and health policy analysts have suggested many potential explanations, such as individual patient behaviors,12 physician bias,13 and systemic discrimination.14 While most Americans are unaware of disparities in health,15 members of minority populations perceive differences in quality and access to care.16,17 Additionally, physicians and patients have differing perceptions, with physicians less likely than the general public to say they believe the health care system discriminates based on race or ethnicity.18
The overwhelming evidence of disparities in health and health care has sparked research comparing populations in terms of their characteristics or receipt of specific services. However, this perspective does not address the broader interactions of populations with the various settings of health care. Looking at populations and where they go when they decide to seek health care provides an “outside-in” view that helps explain where there is the greatest contribution to disparities.
The Ecology of Medical Care by White et al. in 196119 and reprised by Green et al. in 200120 is an example of such a perspective. The ecology model depicts the number of people per 1,000 who access the health care system in an average month. The model does not report the quantity of services provided, focusing instead on individuals and whether they received any care in a health care setting. The methods of the ecology model do not permit conclusions about cause and effect, but they do elucidate who is getting care in those settings.
We applied the ecology model to a nationally representative sample to estimate receipt of care in 5 health settings by individuals according to their race and ethnicity. We hypothesized that race and ethnicity would have independent effects on receiving care in each of the health care settings studied.
METHODS
Study Population
Data for the U.S. civilian, noninstitutionalized population were taken from the 1996 Medical Expenditure Panel Survey (MEPS) sponsored by the Agency for Healthcare Research and Quality (AHRQ). MEPS is an ongoing nationally representative survey with a rotating panel design that enables longitudinal study of a large cohort over a 2.5-year period. Its sample consists of households and individuals who had taken part in the 1995 National Health Interview Survey (NHIS). In this study, household component records characterizing individuals and families were linked to data from event files profiling their health care encounters in calendar year 1996. MEPS records are weighted to permit the calculation of national estimates, usually with small standard errors. MEPS oversamples certain racial and ethnic minorities, making it particularly rich for this study.
Data were limited to the 20,191 MEPS records that included information on each of the variables ultimately included in the multivariate equation (97.1%) excluding participants who identified their race as being neither black nor white except for the Hispanic group (in order to include people who did not self-identify as one of these two racial categories but who did identify as Hispanic). The 20,191 records infer to 257,174,573 civilian, noninstitutionalized Americans comprising the three study groups.
Study Variables
Health Care Setting
Dependent variables consisted of the number per 1,000 people who in an average month received health care in any of the 5 health care settings identified in MEPS: 1) a physician's office, 2) an outpatient clinic, 3) a hospital emergency department, 4) a hospital, 5) their own home.
Race and Ethnicity
For our comparisons, we grouped data into the categories of black, non-Hispanics (blacks); white, non-Hispanics (whites); and Hispanics of any race (Hispanics). The limited sample size of the four additional racial categories (American Indian, Aleut/Eskimo, Asian/Pacific Islander, and other) precluded their inclusion in study analyses. Predictor variables were taken from MEPS household files. We evaluated the following variables for inclusion in multivariate analyses:
Age: 6 age groups used by AHRQ for reporting purposes.
Gender.
Residence: resident of a Metropolitan Statistical Area (MSA) county or a resident of a non-MSA county.
Education: 3 categories for highest degree obtained by head of household: no high school/GED; high school/GED; or postsecondary education.
Household income: reported family income divided by the federal poverty line based on family size and composition, with the resulting percentages grouped into 5 categories.
Health insurance: having any health insurance, without regard to adequacy of coverage, or having no health insurance.
Usual source of care: response to the question: “Is there a particular doctor's office, clinic, health center, or other place that you go to if you are sick or need advice about your health?”
Analytical Strategy
The pattern of medical care for each group was described by estimating the number of MEPS participants in 1996 who, in a month, experienced illness and received care in any of the 5 health care settings. Descriptive analyses were performed as in previous studies using the ecology model.19,20 We first created person-month records, 251,700 in total, for 1996 MEPS participants. A person-month was the unit of analysis, and indicated receipt of services in a health care setting at least once in a month, but not the total number of times care was received in the setting during the month. The individual's survey weight was applied to each person-month, and the result was multiplied by 1,000 to produce estimates.
We evaluated the predictor variables for inclusion in multivariate analyses. Bivariate tests indicated strong associations between each of these variables and receipt of health care services in the various settings. Thus, separate logistic regressions were used to isolate the effects of race and ethnicity on the receipt of care in each of the 5 settings studied, controlling for all 7 variables. Adjusted odds ratios were derived to indicate differences in likelihood of receiving care in each setting based on race and ethnicity, controlling for the effects of all other variables. All analyses utilized the SUDAAN statistical package (Research Triangle Institute, Research Triangle Park, NC) to adjust variance estimates due to MEPS survey design complexity, particularly the substantial oversampling of certain racial and ethnic minorities.
RESULTS
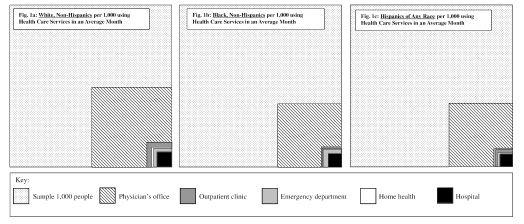
Table 1 depicts participation in 5 health care settings for blacks, whites, and Hispanics. Fewer blacks and Hispanics than whites received care in a physician's office or outpatient clinic than whites, and fewer Hispanics received home health care services than both blacks and whites. These findings achieved significance with a P value of less than .05. There were no significant differences between all 3 groups for receiving care in emergency departments or hospitals. Figure 1 models these findings as a series of boxes for whites (Fig. 1a), blacks (Fig. 1b), and Hispanics (Fig. 1c). Adjusted odds ratios, also presented in Table 1, isolate the effects of race and ethnicity on the likelihood of receiving health care in each of the 5 settings in an average month. In general, after controlling for the predictor variables, the independent effect of being black or Hispanic was associated with fewer people receiving care in physicians’ offices, outpatient clinics, and emergency departments.
Table 1.
Persons per 1,000 Receiving Health Care Services in an Average Month by Race and Ethnicity with Odds Ratios of Likelihood of Receiving Care at Least Once in a Month
| Black, Non-Hispanic | Hispanic, All Races | White, Non-Hispanic | |
|---|---|---|---|
| n per 1,000 who visited a physician's office (SE) | 154.4* (4.5) | 155.4* (5.23) | 243.7 (3.3) |
| OR (95% CI) | 0.65* (0.60 to 0.69) | 0.79* (0.73 to 0.85) | 1.0 |
| n per 1,000 who visited an outpatient clinic | 15.4* (1.6) | 12.2* (1.1) | 24.5 (0.9) |
| OR (95% CI) | 0.73* (0.60 to 0.90) | 0.71* (0.58 to 0.88) | 1.0 |
| n per 1,000 who visited an ER (SE) | 13.0 (0.9) | 12.6 (0.7) | 13.2 (0.4) |
| OR (95% CI) | 0.80* (0.69 to 0.94) | 0.80* (0.68 to 0.93) | 1.0 |
| n per 1,000 who are hospitalized (SE) | 7.1 (0.8) | 6.6 (0.62) | 8.4 (0.4) |
| OR (95% CI) | 0.85 (0.69 to 1.05) | 0.98 (0.79 to 1.22) | 1.0 |
| n per 1,000 who received home care services (SE) | 14.2 (2.2) | 6.9* (1.1) | 13.8 (1.0) |
| OR (95% CI) | 1.12 (0.81 to 1.57) | 0.80 (0.53 to 1.20) | 1.0 |
P < .05.
Odds ratios are controlled for age, gender, residence, education, household income, health insurance, and usual source of care.
OR, odds ratio; CI, confidence interval; SE, standard error; ER, emergency room.
FIGURE 1.
People per 1,000 seeking health care services in particular settings in an average month by race and ethnicity (figure design based on the original ecology study by White et al., 196119).
DISCUSSION
The application of the ecology model to racial and ethnic minority populations found that during an average month, blacks and Hispanics were significantly less likely than whites to receive services in physicians’ offices and outpatient clinics. These differences persisted after controlling for the effects of age, gender, geography, education, economic status, insurance, and having a usual source of care.
The same multivariate model found that blacks and Hispanics were less likely than whites to receive care in an emergency department, a result that runs contrary to some of the literature21,22 but has some support in the findings of smaller studies.23,24 The unadjusted ecology model suggests that Hispanics were less likely to receive care at home than blacks or whites. However, after controlling for the same 7 variables, we found no significant difference in the likelihood of receiving care in the hospital or at home between all 3 population groups.
Is it possible that disparities in health care are a consequence of minorities’ relative absence from outpatient settings? There is considerable evidence that preventive, primary, and secondary interventions can reduce or prevent the complications of most major chronic diseases, and minorities suffer disproportionately from those conditions.25 The majority of primary and preventive care takes place in the setting of primary care physicians’ offices or hospital outpatient clinics. People with a regular source of primary care receive more preventive services, and require less specialty care.26 A good primary care experience has also been associated with better self-rated health status, and tends to reduce disparities in self-rated health status between people of more- and less-disadvantaged communities.27 Studies have shown that once they have accessed primary care, black patients receive preventive services at rates equal to or greater than white patients.28,29 Perhaps, as recently suggested by Schneider et al., persistent disparities in health are partially an effect of smaller proportions of disadvantaged populations receiving care in primary care settings.11 However, it has also been found that racial and ethnic minorities experience worse primary care than the majority population, including care at first contact and longitudinally, comprehensiveness, and coordination.30
Why do fewer blacks and Hispanics receive care in physicians’ offices and outpatient clinics? There are several potential explanations. A majority of blacks perceive that their access to care is different from whites. They cite race as a major issue in the health care system, but feel that the lack of sufficient providers and insurance affordability are more urgent problems.15 In general, blacks and Hispanics are more likely than whites to believe that they receive lower-quality care, that they receive lesser treatment because of their minority status, and that they have been the victims of overt racism.15 While perceptions of racism and discrimination have diminished substantially in the last 30 years,31 there is still a dramatic gap between minorities and nonminorities in their perceptions of the level of equity in the health care system. In 1986, blacks were less likely than whites to feel satisfied with ambulatory or hospital care, and were more likely to have to wait longer.32 These perceptions had changed little by 1994, with all minority groups less likely to be “very satisfied” with the quality of their health care and less likely than whites to have positive perceptions of their physicians.33–35 In surveys conducted in the last few years, minorities were more likely than whites to feel that race and ethnicity negatively impacted their ability to access routine medical care and were much more likely to have experienced discrimination in the health care system based on their racial or ethnic background.17,36 Mistrust and perceived discrimination may contribute to differences in health care decision making and pursuit of care.37 These perceptions may be justified, as studies have shown that faced with identical scenarios, physicians prescribe different diagnostic and treatment regimens to patients based on race.13
Current problems with low Medicaid reimbursements and provider nonparticipation may play a role in minorities receiving less care in outpatient settings, as minorities depend in greater proportion on Medicaid. Controlling for income may partly correct this, but considerations of type of insurance and availability of providers who accept that insurance are important. Minorities are also more likely to live in Health Professional Shortage Areas (HPSAs), particularly in rural areas with high proportions of minorities.38–40 Our study controlled for geography, but as with type of insurance, it is important to consider provider availability when examining reasons for disparities in receipt of care. Minority physicians are more likely to serve racial and ethnic minorities and the underserved in general,41 so the racial and ethnic mix of physician supply also should be considered.
Given similar rates of receipt of care in hospital and home health settings but lower rates of outpatient services, it could be argued that blacks and Hispanics perceive themselves to be generally healthier; however, surveys have found they are actually more likely than whites to consider themselves in fair or poor health.15 Another explanation is that minorities may not perceive the value of obtaining early and preventive health care, thus diminishing their use of outpatient services.42–44 However, as above, minorities with equal access to primary care receive equal or greater preventive services, and multiple programs directed at increasing specific preventive care interventions have succeeded in diminishing or eliminating the gap between minorities and nonminorities, particularly in the areas of breast and cervical cancer screening.45,46 Despite lower receipt of care in the outpatient setting, it does not appear that minorities turn to emergency rooms for care disproportionately. In fact, this study suggests that, when controlling for important variables, blacks and Hispanics are actually less likely than whites to receive care in emergency departments.
Our study has several strengths. Our findings reflect the national health care experience of blacks and Hispanics versus whites. The study isolates those findings to race and ethnicity in all regions of the country for rural and urban populations, and controls for possible confounding by education, income, age, gender, insurance status, and presence of usual source of care, all of which have been shown to affect health care utilization. Our study also takes advantage of oversampling of blacks and Hispanics by MEPS to focus on their unique experiences in the health care system. Additionally, it localizes where differences in receipt of health care occur, and may identify priority areas for further research to understand health and health care disparities.
Our study has limitations. Race and ethnicity are not objective categories, but “historical, social, and political constructs.”47 Imprecision in self-designation by race or ethnicity may generate over- or underestimation of receiving care in each setting. Within each large group designation used there is little homogeneity. Hispanics, for example, may share little more than language, and blacks include both those born and raised in the United States as well as recent African immigrants. There is also substantial overlap between groups that is not entirely accounted for by the categories used for this investigation. These and other problems with using race and ethnicity as variables in health care research are well documented in the literature48–50 and create substantial challenges in the design and interpretation of studies. However, the association of race and ethnicity with identifiable disparities makes this ecologic investigation of differences in receiving care across medical settings a valuable tool in the effort to “root out social injustice in medical practice.”51 Four racial groups with small MEPS samples were excluded from this study because national estimates for these races had unacceptably large standard errors. The rotating panel design of MEPS will provide larger study cohorts over time and this will allow inclusion of additional racial groups in future studies.
Current problems with Medicaid reimbursement and provider dropout may confound the use of insurance as a whole as a simple variable. Additionally, it is possible that health status, whether self-perceived or by objective measures, could provide additional explanatory power to the model. The most appropriate variable in the 1996 MEPS database would be the presence of a priority condition as designated by the AHRQ (i.e., conditions that are life threatening, chronic but manageable, or associated with mental health). However, AHRQ has identified problems with the priority condition designation in the 1996 MEPS (including variation in the source of the data), and therefore it is a weak variable. Subsequent MEPS databases will have stronger data in the area of health status and may shed more light on the contribution of this variable to variations in participation in health care settings.
Our study does not establish causality between the ecology of health care and disparities in health status, and it does not indicate an ideal. However, it reveals differences in patterns of receipt of care in outpatient settings that are strongly associated with race and ethnicity.
Future Research
Racial and ethnic differences in receiving health care in various settings may or may not result in health disparities. Our ecological approach, however, highlights an association and possible direct relation between lower use of outpatient services by racial and ethnic minorities and health disparities. Evidence supporting the role and function of primary care in improving receipt of preventive services and health outcomes suggests that this association has some merit. It is important to build on these findings and expand research about disparate use of outpatient services by racial and ethnic minorities by 1) investigating the barriers that minority populations experience in using and valuing outpatient services; 2) investigating the utilization of outpatient primary care versus subspecialty care by racial and ethnic minorities; 3) investigating whether minority populations receiving similar care to that of nonminorities experience similar quality of care and health outcomes; and 4) identifying how improved utilization of outpatient and primary care services can improve the quality of care and health outcomes. Our findings of similar or reduced receipt of care in emergency departments and similar or increased receipt of care at home also warrant further research to determine the significance of these disparities.
Conclusion
When other important demographic factors are equal, a smaller proportion of black and Hispanic populations receive care in outpatient settings than whites. Disparate receipt of care in the outpatient setting does not translate into increased receipt of care in emergency departments or hospitals. Our findings suggest that disparities in receipt of health services among Hispanics and blacks might be remedied in part by increasing their receipt of care in physicians’ offices and outpatient departments. Applying the ecology model to receipt of care by racial and ethnic minorities raises questions related to the roots of health care disparities and suggests that public policy that attempts to address health disparities might productively focus on the settings of health care as a mediator in improving both the use of appropriate care by minorities and increasing their access to that care.
REFERENCES
- 1.Keppel KG, Pearcy JN, Wagener DK. Trends in racial and ethnic-specific rates for the health status indicators: United States, 1990–98. Healthy People 2000 Stat Notes. 2002;23:1–16. [PubMed] [Google Scholar]
- 2.National Center for Health Statistics. Healthy People 2000 Final Review. Hyattsville, Md: Public Health Service; 2001. [Google Scholar]
- 3.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 4.Mayberry RM, Mili F, Vaid IGM, et al. A Synthesis of the Literature: Racial and Ethnic Differences in Access to Medical Care. Menlo Park, Calif: The Henry J. Kaiser Family Foundation; 1999. [Google Scholar]
- 5.Naumburg EH, Franks P, Bell B, Gold M, Engerman J. Racial differentials in the identification of hypercholesterolemia. J Fam Pract. 1993;36:425–30. [PubMed] [Google Scholar]
- 6.Burns RB, McCarthy EP, Freund KM, et al. Black women receive less mammography even with similar use of primary care. Ann Intern Med. 1996;125:173–82. doi: 10.7326/0003-4819-125-3-199608010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Schneider EC, Cleary PD, Zaslavsky AM, Epstein AM. Racial disparity in influenza vaccination: does managed care narrow the gap between African Americans and whites? JAMA. 2001;286:1455–60. doi: 10.1001/jama.286.12.1455. [DOI] [PubMed] [Google Scholar]
- 8.Strakowski SM, Shelton RC, Kolbrener ML. The effects of race and comorbidity on clinical diagnosis in patients with psychosis. J Clin Psychiatry. 1993;54:96–102. [PubMed] [Google Scholar]
- 9.Cunningham W, Levan R, Brown ER, Wyn R. African Americans Remain Uninsured at Higher Rates Than Whites Despite Their Increasing Job-based Coverage. Los Angeles, Calif: UCLA Center for Health Policy Research; 1999. [PubMed] [Google Scholar]
- 10.Levan R, Brown ER, Hays N, Wyn R. Disparity in Job-based Health Coverage Places California's Latinos at Risk of Being Uninsured. Los Angeles, Calif: UCLA Center for Health Policy Research; 1999. [PubMed] [Google Scholar]
- 11.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in quality of care for enrollees in Medicare managed care. JAMA. 2002;287:1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 12.Myers HF, Kagawa-Singer M, Kumanyika SK, Lex BW, Markides KS. Behavioral risk factors related to chronic diseases in ethnic minorities. Health Psychol. 1995;14:613–21. doi: 10.1037//0278-6133.14.7.613. [DOI] [PubMed] [Google Scholar]
- 13.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 14.Rosenbaum S, Serrano R, Magar M, Stern G. Civil rights in a changing health care system. Health Aff (Millwood) 1997;16:90–105. doi: 10.1377/hlthaff.16.1.90. [DOI] [PubMed] [Google Scholar]
- 15.Race, Ethnicity and Medical Care: A Survey of Public Perceptions and Experiences. Menlo Park, Calif: The Henry J. Kaiser Family Foundation; 1999. [Google Scholar]
- 16.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–63. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- 17.Scott Collins K, Hughes DL, Doty MM, Ives BL, Edwards JN, Tenney K. Diverse Communities, Common Concerns: Assessing Health Care Quality for Minority Americans. New York: The Commonwealth Fund; 2002. [Google Scholar]
- 18.National Survey of Physicians, Part I: Doctors on Disparities in Medical Care. Menlo Park, Calif: The Kaiser Family Foundation; 2002. [Google Scholar]
- 19.White KL, Williams TF, Greenberg BG. The ecology of medical care. N Engl J Med. 1961;265:885–92. doi: 10.1056/NEJM196111022651805. [DOI] [PubMed] [Google Scholar]
- 20.Green LA, Fryer GE, Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited. N Engl J Med. 2001;344:2021–5. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 21.Baker DW, Stevens CD, Brook RH. Determinants of emergency department use: are race and ethnicity important? Ann Emerg Med. 1996;28:677–82. doi: 10.1016/s0196-0644(96)70093-8. [DOI] [PubMed] [Google Scholar]
- 22.White-Means SI, Thornton MC. Non-emergency visits to hospital emergency rooms: a comparison of blacks and whites. Millbank Q. 1989;67:35–7. [PubMed] [Google Scholar]
- 23.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271:1909–12. [PubMed] [Google Scholar]
- 24.Lewin-Epstein N. Determinants of regular source of health care in black, Mexican, Puerto Rican, and non-Hispanic white populations. Med Care. 1991;29:543–57. doi: 10.1097/00005650-199106000-00013. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2nd ed. Alexandria, Va: International Medical Publishing; 1996. [Google Scholar]
- 26.Hargraves JL, Cunningham PJ, Hughes RG. Racial and ethnic differences in access to medical care in managed care plans. Health Serv Res. 2001;36:853–68. [PMC free article] [PubMed] [Google Scholar]
- 27.Shi L, Starfield B, Politzer R, Regan J. Primary care, self-rated health, and reductions in social disparities in health. Health Serv Res. 2002;37:529–50. doi: 10.1111/1475-6773.t01-1-00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams RL, Flocke SA, Stange KC. Race and preventive services delivery among black patients and white patients seen in primary care. Med Care. 2001;39:1260–7. doi: 10.1097/00005650-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Hueston WJ, Hubbard ET. Preventive services for rural and urban African American adults. Arch Fam Med. 2000;9:263–6. doi: 10.1001/archfami.9.3.263. [DOI] [PubMed] [Google Scholar]
- 30.Shi L. Experience of primary care by racial and ethnic groups in the United States. Med Care. 1999;37:1068–77. doi: 10.1097/00005650-199910000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Weaver JL, Garrett SD. Sexism and racism in the American health care industry: a comparative analysis. Int J Health Serv. 1978;8:677–701. doi: 10.2190/AK0C-M9JF-1TR1-5UYF. [DOI] [PubMed] [Google Scholar]
- 32.Blendon RJ, Aiken LH, Freeman HE, Corey CR. Access to medical care for black and white Americans: a matter of continuing concern. JAMA. 1989;261:278–81. [PubMed] [Google Scholar]
- 33.Rowland Hogue CJ, Hargraves MA, Scott Collins K. Minority Health in America. Baltimore, Md: Johns Hopkins University Press; 2000. [Google Scholar]
- 34.Saha S, Komaromy M, Koepsell T, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 35.Cooper-Patrick L, Gallo JJ, Gonzalez JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 36.Race, Ethnicity and Medical Care: A Survey of Public Perceptions and Experiences. Menlo Park, Calif: The Henry J. Kaiser Family Foundation; 1999. [Google Scholar]
- 37.Ferguson JA, Weinberger M, Westmoreland GR, et al. Racial disparity in cardiac decision making. Arch Intern Med. 1998;158:1450–3. doi: 10.1001/archinte.158.13.1450. [DOI] [PubMed] [Google Scholar]
- 38.Grumbach K, Coffman J, Lui R, Mertz E. Strategies for Increasing Physician Supply in Medically Underserved Communities in California. Berkeley, Calif: California Policy Research Center; 1999. p. 11. [Google Scholar]
- 39.Grumbach K, Coffman JM, Young JQ, Vranizan K, Blick N. Physician supply and medical education in California: a comparison with national trends. West J Med. 1998;168:412–21. [PMC free article] [PubMed] [Google Scholar]
- 40.Kindig DA, Yan G. Physician supply in rural areas with large minority populations. Health Aff (Millbank) 1993;12:177–84. doi: 10.1377/hlthaff.12.2.177. [DOI] [PubMed] [Google Scholar]
- 41.Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334:1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 42.Jepson C, Kessler LG, Portnoy B, Gibbs T. Black-white differences in cancer prevention knowledge and behavior. Am J Public Health. 1991;81:501–4. doi: 10.2105/ajph.81.4.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strogatz D. Use of medical care for chest pain: differences between blacks and whites. Am J Public Health. 1990;80:290–4. doi: 10.2105/ajph.80.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stein J, Fox S, Murata P. The influence of ethnicity, socioeconomic status, and psychological barriers on use of mammography. J Health Soc Behav. 1991;32:101–13. [PubMed] [Google Scholar]
- 45.Corbie-Smith G, Flagg EW, Doyle JP, O'Brien MA. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002;17:458–64. doi: 10.1046/j.1525-1497.2002.10733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pearlman DN, Rakowski W, Ehrich B. Mammography, clinical breast exam, and pap testing: correlates of combined screening. Am J Prev Med. 1996;12:52–64. [PubMed] [Google Scholar]
- 47.Oppenheimer GM. Paradigm lost: race, ethnicity, and the search for a new population taxonomy. Am J Public Health. 2001;91:1049–55. doi: 10.2105/ajph.91.7.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. JAMA. 2003;289:2709–16. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- 49.Bhopal R. Revisiting race/ethnicity as a variable in health research. Am J Public Health. 2002;92:156–7. doi: 10.2105/ajph.92.2.156-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Senior PA, Bhopal R. Ethnicity as a variable in epidemiological research. BMJ. 1994;309:327–30. doi: 10.1136/bmj.309.6950.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schwartz RS. Racial profiling in medical research. N Engl J Med. 2001;344:1392–3. doi: 10.1056/NEJM200105033441810. [DOI] [PubMed] [Google Scholar]