Abstract
OBJECTIVE
To use spatial and epidemiologic analyses to understand disparities in mammography use and to formulate interventions to increase its uptake in low-income, high–recent immigration areas in Toronto, Canada.
DESIGN
We compared mammography rates in four income-immigration census tract groups. Data were obtained from the 1996 Canadian census and 2000 physician billing claims. Risk ratios, linear regression, multilayer maps, and spatial analysis were used to examine utilization by area for women age 45 to 64 years.
SETTING
Residential population of inner city Toronto, Canada, with a 1996 population of 780,000.
PARTICIPANTS
Women age 45 to 64 residing in Toronto's inner city in the year 2000.
MEASUREMENTS AND MAIN RESULTS
Among 113,762 women age 45 to 64, 27,435 (24%) had received a mammogram during 2000 and 91,542 (80%) had seen a physician. Only 21% of women had a mammogram in the least advantaged group (low income–high immigration), compared with 27% in the most advantaged group (high income–low immigration) (risk ratio, 0.79; 95% confidence interval, 0.75 to 0.84). Multilayer maps demonstrated a low income–high immigration band running through Toronto's inner city and low mammography rates within that band. There was substantial geographic clustering of study variables.
CONCLUSIONS
We found marked variation in mammography rates by area, with the lowest rates associated with low income and high immigration. Spatial patterns identified areas with low mammography and low physician visit rates appropriate for outreach and public education interventions. We also identified areas with low mammography and high physician visit rates appropriate for interventions targeted at physicians.
Keywords: mammography, socioeconomic factors, emigration and immigration, preventive health services, geography
Disparities in health by socioeconomic status, patterns of migration, and ethnicity have been well-documented using a variety of research methods.1–7 Geographic location has rarely been incorporated into investigations of disparities in health and it is uncommon for geographic methods to be used to examine these phenomena. Geographic Information Systems (GIS),8 however, have more recently found very useful roles in health research,9 including a variety of specific applications.10–13 These methods incorporate visual representations of spatial distributions, spatial statistical analyses, and the definition and manipulation of geographic objects. Important patterns and effects, not apparent using standard epidemiologic techniques, can be revealed using these methods.
Cancer screening is one area where health disparities are apparent14–16 and where considerable efforts have been focused on improving uptake of services and access to care. Early detection of breast cancer is recommended through screening mammography, with or without clinical breast examination, every 1 to 2 years for women aged 40 and older in the United States17 and every 1 to 2 years for women aged 50 and older in Canada.18 Despite organized efforts to promote breast cancer screening and public education efforts targeted to minority women, large disparities in rates of mammography persist in both Canadian and American settings.19,20
In Canada, mammography is a service covered by health insurance, yet its rate of uptake is lower among women with low socioeconomic status and among recent immigrants.20,21 Patient, provider, and system factors may all contribute to these disparities but their underlying mechanisms are poorly understood. Geographic methods have been used to examine breast cancer screening and outcomes in only a few studies.22–24 These analyses have the potential to inform clinicians, public health scientists, and policymakers about areas of need in relation to service provision and to aid in the development of the most appropriate interventions to increase use of preventive services.
The purpose of this study was to use spatial and epidemiologic analyses to understand patterns of mammography and to formulate interventions to increase its uptake in the least advantaged neighborhoods of Toronto, Canada.
METHODS
Setting
The city of Toronto is Canada's largest city and one of the most diverse urban areas in the world. In the 1990s, Toronto was the destination of almost half of Canadian immigrants. Recent immigration patterns reflect the most common countries of origin in Asia, Africa, the Caribbean, Latin America, and Eastern Europe.25 Socioeconomic diversity is also high, as Toronto contains many of the country's wealthiest and least wealthy neighborhoods. The study area occupies 127.5 square kilometers (49.2 square miles) in the south-central portion of Toronto, including the city's downtown core. In 1996, the population was 780,000, recent immigrants who arrived from 1991 to 1996 comprised 11% of the population, the average household income was Can$52,584 (US$33,654), and 29% of the population was identified by the Canadian census as low income. Recent immigration and low income were about twice as high as in the whole province of Ontario (5% and 15%, respectively). Like other Canadian settings, physician and hospital services in Toronto are covered by universal health insurance that is provided without deductibles or copayments. In 1996, the study area contained 1,151 enumeration areas (EAs) and 175 census tracts (CTs) for which socioeconomic information was available.
Sociodemographic Information
We obtained information on population characteristics from the 1996 Canadian census. Within major urban areas, two geographical units used by the Canadian census are CTs, which are similar in definition and size (about 4,000 people; range 2,500 to 8,000) to those used in the United States, and EAs, which are similar in size and population to U.S. block groups (400 to 600 people). Due to their small size, EAs are relatively homogeneous. When developing CT definitions, efforts are made to maximize the internal homogeneity of neighborhood characteristics such as socioeconomic status and living conditions. GIS literature notes that relationships between variables may vary at different levels of geography, a phenomenon referred to as the “Modifiable Areal Unit Problem” (MAUP).26 We chose to use EAs and CTs as units of analysis in this article in order to investigate the possible effects of MAUP. EAs with complete socioeconomic information were identified and aggregated to CTs. Our mapping was conducted at the CT level only due to the very small geographic size of some EAs.
Although Canada does not have an official poverty line, the Canadian census does include a measure of low income, the Low Income Cut-off (LICO). This measure takes into account family size, annual changes in the consumer price index, and controls for differences in living expenses in different sized communities. In Toronto in 1996, the LICO for a family of four (after government transfers and before taxes) was Can$31,753 (US$20,322) and for a single person Can$16,874 (US$10,799). We used the Canadian census definition of recent immigration as immigration to Canada within the previous 5 years.
In our study area, recent immigrants tend to settle in low-income areas, making it difficult to disentangle the separate effects of income and immigration on access to care at the area level. For this reason, we created a 4-level variable according to each group's expected advantage in accessing care: 1) low income–high immigration (least advantaged); 2) low income–low immigration; 3) high income–high immigration; and 4) high income–low immigration (most advantaged). We created this variable by examining the distributions of low income and immigration across the study area using frequency plots, 2-by-2 tables, and maps. It was not possible to create 4 groups with equal population, but the breakpoints of 30% for low income and 10% for recent immigration resulted in a reasonably even spread of EAs and CTs across the 4 groups.
Health Care Utilization
Ontario's health care registry, the Registered Persons Database (RPDB), includes all persons eligible for health coverage by age, gender, and address. All Ontario residents are eligible for health coverage if they are Canadian citizens, landed immigrants or convention refugees, make their permanent and principal home in Ontario, and are physically present in Ontario 153 days in any 12-month period. We used the RPDB to identify a denominator population of women age 45 to 64 resident in our study area in 2000. The Ontario Health Insurance Plan (OHIP) covers physician and hospital services and includes approximately 95% of ambulatory physician visits in the province. We used OHIP's Physicians Claims Database for 2000 to identify women age 45 to 64 who had at least 1 ambulatory physician visit (using OHIP “A” and “K” codes) and who had mammography (OHIP fee codes X184, X185, X186, X187). We used RPDB denominators to calculate the proportion of women seeing a physician and having a mammogram in 2000. We used the Postal Code Conversion File Plus from Statistics Canada to link the postal codes from the RPDB to the best-fitting EA and CT. OHIP claims were then assigned to EAs and CTs using a scrambled unique identifying number that enables linkage between OHIP physician claims and the RPDB.
Mapping
Most maps, including the ones in this article, are constructed with several spatial data layers. Base layers such as roads, water bodies, and green areas are normally placed on top of thematic layers, which show attribute variables. For example, a thematic layer of physician visits can be placed on top of a thematic layer of low income and immigration and both can be complemented with the base layer of census boundaries. In this article, we use one base layer and overlays of up to two thematic layers.
Choropleth, or shaded maps, are commonly used to depict rate and ratio data. The intensity of colors or shades indicates the magnitude of the variable within given boundaries. All data values are divided into classes that are created using criteria such as equal number of cases in each class, equal number of areas in each class, or using natural breaks in the data distribution. Shaded maps are particularly useful in making relative comparisons between areas on the map.27 We used choropleth maps in this article to depict the range of income and immigration values by census tract, with a different shade used for each level depicted. Proportional symbols, such as circles or squares, can be used to depict rate and ratio data as well as counts and frequencies. The size of the symbol varies in proportion to individual data values or to value ranges. Proportional symbols are commonly overlaid on top of a choropleth layer in multivariate thematic maps. We used circles to depict the proportion of women with or without mammograms. Dot density maps are suitable for discrete events or individuals, illustrating their variations in frequency in different locations on the map. Dots representing one or more occurrences are placed within geographic units such as zip codes or census tracts.27 In this article, we used dot density to depict the location and number of women who have not had a mammogram. Grid maps are appropriate for depicting values that change gradually over space.28 These are created using a regular lattice of small squares or hexagons which cover the entire displayed area. In this article, we used interpolated grids for physician visits. We kept grid elements very small because levels of physician visits can change rapidly across census tract boundaries.
Statistical Analysis
We aggregated the number of women with a physician visit and the number with a mammogram to correspond with our 4-level variable of low income and recent immigration. For each of the 4 levels we then calculated the proportion of women with a physician visit and the proportion of women with a mammogram and created rate ratios by comparing each group with the most advantaged group (high income–low immigration). We calculated 95% confidence intervals for rate ratios using bootstrapping methods.29 We also fit separate linear regression models to examine relationships between our main outcome, mammography, and low income, recent immigration, and having a physician visit.
When variables are clustered in space, usual epidemiologic analyses can produce biased estimates by violating the assumption that each data point is independent of other data points. This type of autocorrelation is similar to that which occurs when data are correlated in time, such as repeated measures on the same subject or population. We used Moran's scatterplot and Moran's I to examine the clustering of each variable used in our regression analyses and to examine regression residuals.30 These methods measure the correlation between area values and the values of neighboring areas. In these analyses, we used first-order neighborhood structure such that only spatial units that shared boundaries were considered as neighbors. Moran's I autocorrelation coefficient ranges from −1 to 1, with values of 0 representing no clustering. We considered important geographic clustering to occur at values of Moran's I < −0.2 or >0.2. In the case of important geographic clustering in regression analyses, we ran the regressions with and without correction for this autocorrelation using simultaneous autoregressive modeling (SAR).30 All statistical analyses were performed for both CTs and EAs.
This study was approved by the University of Toronto and Sunnybrook and Women's College Hospital research ethics boards.
RESULTS
Study Area Characteristics
Characteristics of the study setting and each of the 4 income–immigration groups appear in Table 1. The ranges for several characteristics demonstrated a high level of diversity, with CT household income varying from Can$18,310 to $231,187 (US$11,718 to $147,960), percent not completing high school varying from 7% to 62%, and percent unemployment varying from 0% to 29%. The same variables show even more extreme values by EA (not shown). Income is very similar in the two low-income groups (Can$39,103 and Can$41,931, respectively) but somewhat disparate in the two high-income groups (Can$45,858 and Can$65,482, respectively). Recent immigration is similar in both high immigration groups (14% to 15%) but somewhat different in the low immigration–low income and low immigration–high income groups (8% and 4%, respectively).
Table 1.
Characteristics of Inner City Toronto, Ontario, Canada by Income and Immigration Groups, 1996 Canadian Census
| Area Characteristics | Study Area | Low-income High-immigration | Low-income Low-immigration | High-income High-immigration | High-income Low-immigration |
|---|---|---|---|---|---|
| Female, % | 51 | 51 | 50 | 50 | 52 |
| (range) | (39 to 60) | (42 to 56) | (41 to 56) | (42 to 57) | (39 to 60) |
| Mean age, y | 35 | 34 | 35 | 35 | 37 |
| (range) | (27 to 46) | (27 to 38) | (32 to 44) | (32 to 38) | (33 to 46) |
| Recent immigration,*% | 9 | 15 | 8 | 14 | 5 |
| (range) | (0 to 37) | (10 to 37) | (6 to 10) | (10 to 19) | (0 to 10) |
| Low income,†% | 30 | 36 | 35 | 28 | 17 |
| (range) | (2 to 79) | (30 to 79) | (30 to 56) | (18 to 30) | (2 to 31) |
| Mean household income,‡ | 45,263 | 39,103 | 41,931 | 45,858 | 65,482 |
| Can$ (range) | (18,310 to 231,187) | (18,310 to 56,244) | (24,787 to 48,380) | (36,979 to 72,250) | (38,916 to 231,187) |
| No high school, % | 31 | 42 | 40 | 21 | 19 |
| (range) | (7 to 62) | (8 to 62) | (14 to 55) | (8 to 59) | (7 to 58) |
| Visible minority, % | 26 | 41 | 26 | 26 | 14 |
| (range) | (0 to 74) | (21 to 74) | (16 to 44) | (13 to 58) | (0 to 44) |
| No official language, % (English/French) | 5 | 9 | 9 | 3 | 2 |
| (range) | (0 to 31) | (2 to 31) | (0 to 22) | (1 to 21) | (0 to 19) |
| Unemployment, % | 10 | 13 | 12 | 10 | 7 |
| (range) | (0 to 29) | (7 to 29) | (8 to 17) | (5 to 13) | (0 to 14) |
| Not in labor force, % | 34 | 37 | 37 | 29 | 29 |
| (range) | (16 to 54) | (23 to 54) | (26 to 46) | (20 to 45) | (16 to 45) |
| Number of census tracts | 175 | 68 | 18 | 13 | 76 |
Immigration within the previous 5-year period.
As defined by Statistics Canada, identifying households relatively worse off than the national average.
Canadian dollar = 0.64 U.S. dollar in 1996.
Figure 1 shows a choropleth map of the study area with the 4-level income–immigration groups overlaid on base layers. The least advantaged CTs are distributed in a U-shaped band across the study area.
FIGURE 1.
Choropleth (shaded) map of census tracts showing distribution of income and immigration groups in Toronto's inner city, 1996.
Health Care Utilization
The proportion of women age 45 to 64 with at least 1 physician visit was 80% overall, with only small variation across income–immigration groups (Table 2). The most and least advantaged groups had similar access to physicians (80% and 81%, respectively). Rate ratios comparing each group to the most advantaged group are close to 1.0, indicating no difference between groups. The proportion of women with a mammogram was 24% overall and increased with each level of increasing advantage, from 21% in the least advantaged group to 27% in the most advantaged. Rate ratios all fell significantly below 1.0, and showed decreasing use of mammography with decreasing advantage, relative to the most advantaged group.
Table 2.
Proportion of Women with a Physician Visit and with a Mammogram by Income and Immigration* and Rate Ratios (with 95% Confidence Intervals) in Inner City Toronto, Ontario, Canada, 2000
| Visit to Any Physician | Having a Mammogram | ||||
|---|---|---|---|---|---|
| Neighborhood Category | Proportion | Rate Ratio†(95% CI) | Proportion | Rate Ratio†(95% CI) | |
| Least advantaged | Low-income High-immigration | 0.80 | 0.99 (0.97 to 1.01) | 0.21 | 0.79 (0.75 to 0.84) |
| Low-income Low-immigration | 0.80 | 0.99 (0.96 to 1.01) | 0.23 | 0.86 (0.81 to 0.92) | |
| High-income High-immigration | 0.78 | 0.96 (0.91 to 1.00) | 0.24 | 0.87 (0.80 to 0.93) | |
| Most advantaged | High-income Low-immigration | 0.81 | 1.00 | 0.27 | 1.00 |
| Total study area | 0.80 | — | 0.24 | — | |
Immigration within the previous 5-year period.
Rate ratio defined as the proportion of women with a physician visit or mammogram in a group/proportion of women with a physician visit in the most advantaged group. CI, confidence interval.
Figure 2 shows the 4-level income–immigration variable (choropleth layer) and proportional symbol overlay of women age 45 to 64 with a mammogram in 2000. The spatial patterns on this map confirm that mammography use was lowest in the least advantaged areas.
FIGURE 2.
Proportional symbol map of women with mammograms (circles) in relation to choropleth (shaded) layer of income and immigration group by census tract in Toronto's inner city.
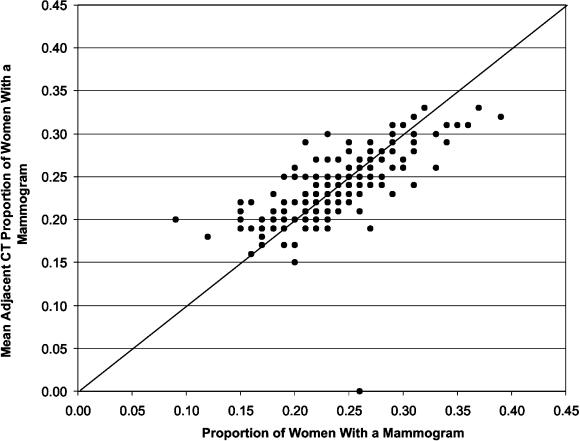
Figure 3 shows Moran's scatterplot for the proportion of women with a mammogram. The values in CTs across the study area were highly correlated with the values in neighboring CTs as demonstrated by the visible pattern and by a Moran's I of 0.56 (P < .001). Similar geographic clustering was found for low income, recent immigration, and any physician visit (Moran's I > 0.2, details not shown).
FIGURE 3.
Moran's scatterplot of proportion of women with mammograms (2000).
Regression analyses showed strong inverse relationships between low income and mammography and recent immigration and mammography (Table 3), confirming that low-income and recent immigration areas were associated with low mammography use. Having any physician visit was directly associated with mammography.
Table 3.
Regression Results for Proportion of Women Age 45 to 64 Having a Mammogram, Without and with Adjustment for Geographic Clustering
| Without Adjustment | Adjusted for Geographic Clustering | |||||
|---|---|---|---|---|---|---|
| Variable | Parameter Estimate | P Value | Spatial Autocorrelation of Residuals | Parameter Estimate | P Value | Spatial Autocorrelation of Residuals |
| Percent low income | −0.0024 | <.0001 | 0.48 | −0.0015 | <.0001 | 0.01 |
| Percent recent immigration* | −0.0039 | <.0001 | 0.63 | −0.0025 | <.0001 | 0.01 |
| Any physician visit | 0.3335 | <.0001 | 0.72 | 0.3276 | <.0001 | 0.15 |
Immigration within the previous 5-year period.
All the above analyses were repeated using EA as the geographical unit of analysis. Results were virtually identical to those from the CT analyses and are therefore not presented here.
Residuals from the regression analyses showed clustering for each variable at the CT level (Moran's I > 0.25; P < .001 for all variables) but to a lesser extent at the EA level (Moran's I < 0.27 for all variables). When SAR was used at the CT level to adjust for clustering, parameter estimates changed but statistical significance remained the same (Table 3). This adjustment greatly reduced autocorrelation among the residuals, producing a less biased estimate.
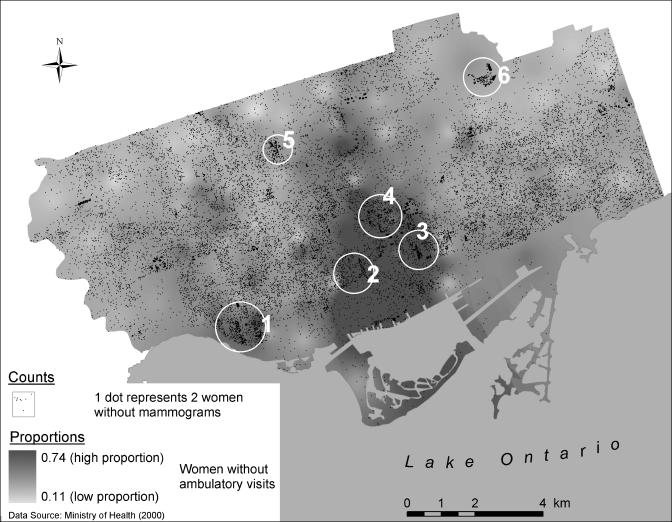
Both Figures 4A and 4B show the proportion of women without any ambulatory visit in 2000 as an interpolated grid. In Figure 4A, this variable is overlaid with proportional symbols depicting the proportion of women without a mammogram. Low mammography use occurs in areas with both high and low physician access. In Figure 4B, the dot density layer shows the number of women without a mammogram. Circles identify concentrations of women needing mammography in areas of low (labels 1 through 4) and high (labels 5 and 6) physician access.
FIGURE 4A.
Proportional symbol map of women needing a mammogram (circles) in relation to an interpolated grid layer (background shading) of women without an ambulatory care visit by census tract in Toronto's inner city.
FIGURE 4B.
Dot density map of number of women needing a mammogram (dots) in relation to an interpolated grid layer (background shading) of women without an ambulatory care visit by census tract in Toronto's inner city.
DISCUSSION
These results confirm the well-established relationship between low income and low rates of mammography, even in a universal health insurance setting.19,20 They further demonstrate that areas of high recent immigration have low mammography use, independent of income effects. GIS has helped to extend these findings in several important ways. Maps provided geographic identification of high-need areas, clusters of high-need women, and visualization of mammography needs in relation to physician services. We found moderately strong clustering effects and we were able to appropriately adjust our analyses to arrive at unbiased parameter estimates.
Mapping identified a U-shaped band across the study area with low income, high immigration, and low mammography use. It would have been challenging to identify this pattern without maps and almost impossible to identify specific areas for targeting of interventions. It is often important to know where people who need services are located, not just where rates of use are high or low. In this case, dot density maps were particularly useful in identifying concentrations of women needing mammography. Maps were also invaluable in identifying what types of interventions would best suit certain areas. For example, some low mammography areas also had low use of physician services. Appropriate interventions in these areas would be directed to the public through some combination of outreach, extended service provision, and public education.31,32 Other low mammography areas had high rates of physician use. Appropriate interventions in these areas would be directed toward changing clinical practice to improve mammography uptake.33
Geographic clustering effects are often ignored in epidemiologic and health services research, but such effects are as important as correlation over time and, when present, should be taken into account in analytic approaches. In our case, parameter estimates changed with this adjustment but there was no effect on our overall conclusions. In analyses where effect sizes are smaller and statistical significance is closer to P = .05, this adjustment can affect both the size and statistical significance of the effect. In our analyses, results were largely the same for EAs and CTs but aggregation often produces different results and careful attention should be given when choosing the appropriate geographic level of aggregation.26 More noticeable changes would likely be observed if we aggregated from EAs to areas larger than CTs.
Our analyses demonstrated important associations between low income, recent immigration, and mammography. Due to collinearity between income and immigration (correlation 0.79), we may not be able to identify adequately which is more important or explanatory from the regression analyses. Our 4-level variable, however, provided a comparison between groups with similar low income but differing levels of immigration. These analyses demonstrated the independent effects of both income and immigration. Not surprisingly, visiting a physician at least once was associated with having a mammogram, because these tests are physician ordered in our setting.
Reasons for underuse of mammography include patient factors such as knowledge, attitudes, beliefs, behaviors, literacy, and competing demands; physician factors such as communication skills, attitudes, knowledge, and payment incentives; and system factors such as patient tracking and follow-up, patient education and support, and access barriers.34 The patient factors addressed in this study were the income and immigration characteristics of the area of residence. While these factors are themselves difficult to modify, the associated barriers related to language, cultural norms, competing time demands, and lack of knowledge are modifiable and can be targeted to improve uptake of services.31,35 Physician recommendation is one of the strongest predictors of mammography use. Strategies for improving physician preventive interventions include educational materials, incentives, patient-mediated interventions, flow sheets, reminders, opinion leaders, or combinations of these strategies.36 System barriers to be considered include indirect financial barriers such as transportation costs and time off work, the lack of translated educational materials, lack of evening and weekend mammography hours for those without work flexibility, and a limited number of physicians accepting new patients in Toronto's inner city. In our setting, areas of high recent immigration are heterogeneous, with varying cultures and circumstances of immigration. Our analyses need to be interpreted in that light and interventions need to be tailored to account for cultural and language issues.
We cannot tell from these results whether low-income recent immigrant women are more or less likely than other women to have mammography, only that the areas in which they reside have low mammography rates and high concentrations of women needing mammography. In the case of mammography and other preventive services, however, it is often more important to identify areas for resource allocation and specific intervention than it is to be able to identify particular women.
In Ontario, some mammography is funded outside of fee for service through the Ontario Breast Screening Program (OBSP) and may not appear in OHIP files. OBSP program data indicate that about 10,000 women in our study area, or 10% of those eligible, may have had a mammogram through the program each year. This proportion would affect our results only if the majority of women screened in the OBSP resided in Toronto's least advantaged areas, a highly unlikely situation.
Coding errors and inaccuracies can occur in administrative data. Errors were likely to be small for the fee-for-service reimbursement codes used in this study but potentially larger for Ontario's health care registry, the RBDP, because it has no regular system for updating addresses and instead relies on voluntary reporting. In previous work, we found that RPDB-based socioeconomic levels and measures of association were reasonably unbiased.37 We applied area characteristics from the 1996 Canadian census to women in 2000. While it is likely that small changes in neighborhood composition occurred, both income and immigration patterns were consistent in our study area between the 1991 and 1996 census years.
We conclude that geographic information systems are extremely useful in conducting research into health disparities. Maps visualize effects and patterns that cannot otherwise be appreciated and can assist with targeting of interventions. Geospatial statistical analyses of clustered data provide unbiased estimates of effects and their significance. In the current study, GIS greatly helped to locate and characterize disparities in mammography and was used to formulate interventions to increase mammography use. GIS should be considered an essential tool in understanding and reducing health disparities.
Acknowledgments
Supported by the Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada, and the Ontario Ministry of Health and Long-Term Care. The opinions, results, and conclusions are those of the authors and no endorsement by the Ministry is intended or should be inferred.
REFERENCES
- 1.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–73. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 2.Marmot MG, Shipley MJ, Rose G. Inequalities in death-specific explanations of a general pattern? Lancet. 1984;1:1003–6. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 3.Marmot MG, Smith DG, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337:1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 4.Lieu TA, Newacheck PW, McManus MA. Race, ethnicity, and access to ambulatory care among US adolescents. Am J Public Health. 1993;83:960–5. doi: 10.2105/ajph.83.7.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cowie MR, Fahrenbruch CE, Cobb LA, Hallstrom AP. Out-of-hospital cardiac arrest: racial differences in outcome in Seattle. Am J Public Health. 1993;83:955–9. doi: 10.2105/ajph.83.7.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carr W, Zeitel L, Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am J Public Health. 1992;82:59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 8.DeMers MN. Fundamentals of Geographic Information Systems. New York: John Wiley & Sons; 2000. pp. 7–16. [Google Scholar]
- 9.Cromley EK. GIS and Public Health. New York: Guilford Press; 2002. pp. 35–7. [Google Scholar]
- 10.Phillips RL, Kinman EL, Schnitzer PG, Lindbloom EJ, Ewigman B. Using geographic information systems to understand health care access. Arch Fam Med. 2000;9:971–8. doi: 10.1001/archfami.9.10.971. [DOI] [PubMed] [Google Scholar]
- 11.Backman AM, Rigby JM, Rice MD, Rivers LM. Locating community health care centres in rural Saskatchewan: the case of the Living Sky Health District. Health Manage Forum. 1995;8:52–61. doi: 10.1016/S0840-4704(10)60896-4. [DOI] [PubMed] [Google Scholar]
- 12.Fosgate GT, Carpenter TE, Chomel BB, Case JT, DeBess EE, Reilly KF. Time-space clustering of human brucellosis, California, 1973–1992. Emerg Infect Dis. 2002;8:672–8. doi: 10.3201/eid0807.010351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buckeridge DL, Glazier R, Harvey BJ, Escobar M, Amrhein C, Frank J. Effect of motor vehicle emissions on respiratory health in an urban area. Environ Health Perspect. 2002;110:293–300. doi: 10.1289/ehp.02110293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med. 1998;27:821–9. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- 15.Caplan LS, Wells BL, Haynes S. Breast cancer screening among older racial/ethnic minorities and whites: barriers to early detection. J Gerontol. 1992;47:101–10. [PubMed] [Google Scholar]
- 16.Wells BL, Horm JW. Targeting the underserved for breast and cervical cancer screening: the utility of ecological analysis using the National Health Interview Survey. Am J Public Health. 1998;88:1484–9. doi: 10.2105/ajph.88.10.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Preventive Services Task Force (USPSTF) Available at: http://www.ahcpr.gov/clinic/3rduspstf/breastcancer/brcanrr.htm. Accessed January 7, 2004. [Google Scholar]
- 18.Canadian Taskforce on Preventive Health Care. Available at: http://www.ctfphc.org. Accessed January 7, 2004. [Google Scholar]
- 19.Katz SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite universal coverage. Breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272:530–4. [PubMed] [Google Scholar]
- 20.Katz SJ, Zemencuk JK, Hofer TP. Breast cancer screening in the United States and Canada, 1994: socioeconomic gradients persist. Am J Public Health. 2000;90:799–803. doi: 10.2105/ajph.90.5.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mercer SL, Goel V. Factors associated with the use of mammography: the Ontario Health Survey. Cancer Prev Control. 1997;1:144–51. [PubMed] [Google Scholar]
- 22.Hyndman J, Holman CD, Jamrozik K. The effect of spatial definition on the allocation of clients to screening clinics. Soc Sci Med. 1997;45:331–40. doi: 10.1016/s0277-9536(96)00348-6. [DOI] [PubMed] [Google Scholar]
- 23.Roche LM, Skinner R, Weinstein RB. syste. Use of a geographic information m to identify and characterize areas with high proportions of distant stage breast cancer. Public Health Manag Pract. 2002;8:26–32. doi: 10.1097/00124784-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Wanner P, Raymond L, Bouchardy C. Geographical disparities in self-reported use of mammography and breast self-examination according to the Swiss Health Survey. Ann Oncol. 2001;12:573–4. doi: 10.1023/a:1011147027410. [DOI] [PubMed] [Google Scholar]
- 25.Citizenship and Immigration Canada. Ottawa: Strategic Policy, Planning and Research, Citizenship and Immigration Canada. Canada: Minister of Public Works and Government Services; 2001. Facts and Figures, 2000—Immigration Overview. [Google Scholar]
- 26.Fotheringham AS, Brunsdon C, Charlton M. Quantitative Geography Perspectives on Spatial Data Analysis. London: SAGE Publications Ltd; 2002. pp. 237–40. [Google Scholar]
- 27.Dent BD. Cartography: Thematic Map Design. 5th ed. Dubuque, IA: Wm. C. Brown; 1999. pp. 138–86. [Google Scholar]
- 28.Jones CB. Geographic Information Systems and Computer Cartography. Harlow, Essex: Addison Wesley Longman Ltd; 1997. pp. 197–208. [Google Scholar]
- 29.Davison AC, Hinkley DV. Bootstrap Methods and Their Applications. New York: Cambridge Press; 1997. [Google Scholar]
- 30.Bailey TC, Gatrell AC. Interactive Spatial Data Analysis. New York: Longman Scientific & Technical Publications; 1995. pp. 274–89. [Google Scholar]
- 31.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3:19–30. [PubMed] [Google Scholar]
- 32.Yabroff KR, Mandelblatt JS. Interventions targeted toward patients to increase mammography use. Cancer Epidemiol Biomarkers Prev. 1999;8:749–57. [PubMed] [Google Scholar]
- 33.Mandelblatt JS, Yabroff KR. Effectiveness of interventions designed to increase mammography use: a meta-analysis of provider-targeted strategies. Cancer Epidemiol Biomarkers Prev. 1999;8:759–67. [PubMed] [Google Scholar]
- 34.Bickell NA. Race, ethnicity, and disparities in breast cancer: victories and challenges. Womens Health Issues. 2002;12:238–51. doi: 10.1016/s1049-3867(02)00145-7. [DOI] [PubMed] [Google Scholar]
- 35.Hubbell FA, Chavez LR, Mishra SI, Magana JR, Valdez R. From ethnography to intervention: developing a breast cancer control program for Latinas. Monogr Natl Cancer Inst. 1995;18:109–15. [PubMed] [Google Scholar]
- 36.Mazmanian PE, Davis DA. Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288:1057–60. doi: 10.1001/jama.288.9.1057. [DOI] [PubMed] [Google Scholar]
- 37.Glazier RH, Creatore MI, Agha M, Steele LS. Socioeconomic misclassification in Ontario's health care registry. Can J Public Health. 2003;94:140–3. doi: 10.1007/BF03404588. [DOI] [PMC free article] [PubMed] [Google Scholar]