Abstract
OBJECTIVE
To assess the effectiveness of mailed hypertension educational materials.
DESIGN
Prospective, randomized, controlled single-blind trial.
SETTING
Primary care practice–based research network in which 9 clinics located in Portland, Oregon participated.
PARTICIPANTS
Patients with mildly uncontrolled hypertension as defined as a last blood pressure of 140 to 159/90 to 99 mmHg from query of an electronic medical record database.
INTERVENTIONS
Patients randomized to intervention were mailed 2 educational packets approximately 3 months apart. The first mailer included a letter from each patient's primary care provider. The mailer included a booklet providing an overview of hypertension and lifestyle modification and a refrigerator magnet noting target blood pressure. The second mailing also included a letter from the patient's primary care provider, a second educational booklet focused on medication compliance and home blood pressure monitoring, and a blood pressure logbook. The control group consisted of similar patients receiving usual care for hypertension.
MEASUREMENTS AND MAIN RESULTS
Patients from each group were randomly selected for invitation to participate in a study visit to measure blood pressure and complete a survey (intervention n = 162; control n = 150). No significant difference was found in mean blood pressure between intervention and control patients (135/77 mmHg vs 137/77 mmHg; P = .229). Patients in the intervention arm scored higher on a hypertension knowledge quiz (7.48 ± 1.6 vs 7.06 ± 1.6; P = .019), and reported higher satisfaction with several aspects of their care. No significant difference was seen in the prevalence of home blood pressure monitoring ownership or use.
CONCLUSIONS
In patients with mildly uncontrolled hypertension, educational mailers did not yield a significant decrease in blood pressure. However, significant improvement in patient knowledge, frequency of home monitoring, and satisfaction with care were demonstrated.
Keywords: hypertension, randomized controlled study, patient education, postal service, pamphlet
Hypertension is a major health problem in the United States, affecting more than 43 million people.1,2 Numerous large, randomized controlled trials have demonstrated that treatment of hypertension decreases the incidence of stroke, cardiac events, and death without negatively impacting quality of life.3 The abundance of antihypertensive agents currently available allow clinicians to customize therapy based on individual patient characteristics and needs with regard to frequency of dosing, cardiac and noncardiac benefits, side effect profile, and cost. Despite increased awareness of hypertension and the availability of effective pharmacotherapy, only 34% of hypertensive patients nationally achieve a blood pressure less than 140/90 mmHg.4
As with other chronic conditions, optimal outcomes of hypertension management are facilitated by patient self-management.5 The components of self-management include daily compliance and long-term adherence to lifestyle modifications and pharmacotherapy, as well as attention to monitoring and follow-up.6 Health care organizations are challenged with the development and implementation of cost-effective strategies for improving control of hypertension in large patient populations. Recognizing that patient knowledge and motivation are central to self-management, strategies to improve population health should benefit from including a patient education component.
Written patient educational materials are among the self-management interventions frequently implemented. Despite the common use of mailed educational materials by health care organizations, there is a paucity of randomized controlled studies evaluating the impact of this strategy on blood pressure. Several published studies evaluate hypertension educational materials,7–11 but to our knowledge there is only one randomized controlled study evaluating the effect of these materials on the outcome of blood pressure.11 This study, conducted in 6 general medicine practices in London, randomized 552 hypertensive patients to usual care or a mailed educational hypertension booklet with an introductory letter from the patient's general practitioner. One year after the mailing, home visits were made to assess blood pressure and for completion of a patient questionnaire. There was no significant difference in diastolic or systolic blood pressure between the groups. However, the investigators reported a slightly higher mean adjusted score on the knowledge questionnaire in the study group as compared to control.
This study addresses this important gap in the literature by determining the impact of mailed hypertension educational materials on blood pressure in a community-based primary care setting in the United States.
METHODS
This study was a prospective, randomized, controlled, single-blind study. The study was approved by the local institutional review board.
Study Site
This study was conducted within the Providence Primary Care Research Network in Oregon. Network clinics participating in the study comprised approximately 80 internal medicine and family practice providers caring for 110,000 patients in nine clinic locations. All 9 participating Network clinics utilize Logician, a standardized electronic medical record (EMR), to facilitate and document all patient care activities. Use of the EMR allows for storage and retrieval of demographic information, diagnoses, medications, laboratory data, vital signs, and visit records.
Population
Patients with mildly uncontrolled hypertension were identified from query of the EMR database using the following criteria: 1) active patients with documentation of an office visit within the past 2 years, 2) problem list entry of hypertension, 3) a last systolic blood pressure of 140 to 159 mmHg, and/or a last diastolic blood pressure of 90 to 99 mmHg. In order to limit contamination, subjects were excluded if they or their spouse were enrolled in another hypertension study.
Intervention
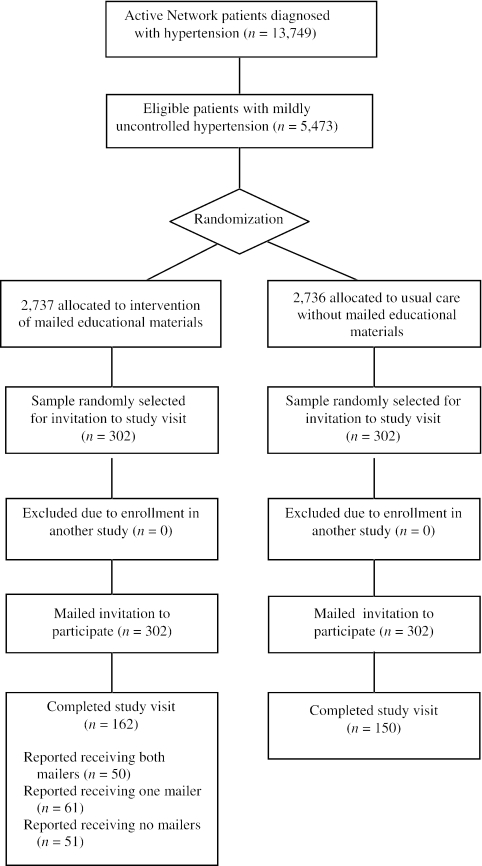
Patients were randomly allocated to intervention or control using a computer-generated random sequence (Fig. 1). A series of two educational packets was mailed to the patients randomized to the intervention arm. The first mailer included a letter from each patient's primary care provider introducing the educational materials and highlighting the importance of blood pressure control. The initial educational booklet was selected from available materials based on content, widespread availability, reading level, and style. The booklet provided a basic overview of hypertension and lifestyle modification (Table 1). Also included in the packet was a refrigerator magnet reminding patients that their target blood pressure is less than 140/90 mmHg. A magnet with a lower blood pressure target specification was provided to patients identified as also having diabetes.
FIGURE 1.
Flow diagram of a trial comparing mailed educational materials with usual care in patients with mildly controlled hypertension.
Table 1.
Content of Mailed Educational Packets
| First Packet | Second Packet |
|---|---|
| Introductory letter from primary care provider | Introductory letter from primary care provider |
| Pamphlet (Understanding & Controlling High Blood Pressure. Krames 159021–01/99) providing an overview of hypertension, including: | Pamphlet (Part 2: High Blood Pressure Treatment & Monitoring. Providence Medical Group 05/01) providing an overview of hypertension monitoring and treatment, including: |
| Definition of hypertension | Review of antihypertensive drug classes |
| Complications of hypertension | Factors that influence the selection of antihypertensive medications |
| Measurement of blood pressure | Medication side effects |
| Tips for healthy eating | Tips to improve compliance |
| Tips for healthy lifestyle | Introduction to home monitoring |
| Tips for taking medications | Recommendations for selection of a home blood pressure monitor |
| Community resources | Tips for accurate blood pressure measurement |
| Refrigerator magnet displaying blood pressure target | Home blood pressure monitoring log |
The second educational packet, mailed approximately 3 months later, included another letter from the patient's primary care provider and a second educational booklet. This booklet was designed by Network practitioners to augment the initial booklet, focusing on medication compliance and home blood pressure monitoring (Table 1). A separate blood pressure log encouraged patients to record home blood pressure measurements in a graph format.
METHODS
One year (± 3 months) following the mailings, a random sample of patients from each arm received an IRB-approved letter inviting them to attend the clinic for a study visit. Patients not responding to the letter were contacted by phone. Patients consenting to participate attended open clinic sessions in which blood pressure was assessed and questionnaires were completed. Blood pressure was assessed in the patient's primary care office by a registered nurse recently exposed to updated training in blood pressure assessment. The nurse was blinded to intervention allocation. Three blood pressure measurements were taken with no less than 5 minutes and no more than 10 minutes between measurements. The average of the second and third blood pressures was used for analysis. Heart rate was measured between the second and third blood pressure assessments. Patients were offered a blood pressure home monitoring device or a $40 gift certificate for their participation.
Outcome Measures
The primary outcome measure was the difference in mean blood pressure between patients receiving the educational hypertension packets (intervention group) and patients not receiving those materials (usual care group).
Several secondary outcomes were also assessed, including patient satisfaction with several aspects of their health care, patient knowledge about hypertension, patient compliance with medications, and prevalence of home blood pressure monitoring. The knowledge quiz was constructed to assess basic understanding of hypertension and the principles of self-management. The range of possible scores was 0 to 10, 10 points representing a perfect score (see Appendix). The satisfaction survey included several aspects of care specific to the management of hypertension. The assessment of medication compliance consisted of four validated questions. The range of possible scores was 0 to 4, where 4 points represented good medication compliance.12 Last, patients receiving the educational packets were surveyed regarding the quality, usefulness, and value of the mailings.
Statistical Analysis
A total sample size of 302 subjects was required for 90% power to detect a 3-mmHg difference in mean systolic (SBP) or diastolic (DBP) blood pressure between intervention and usual care groups, at a significance level of P < .05 (two-sided), assuming a standard deviation for SBP or DBP of 8 mmHg.
Continuous data were described by mean (standard deviation) and were compared using unpaired t tests. Categorical data were described by percentages and were compared by χ2 tests with continuity correction or Fisher's Exact test, as appropriate. All analyses were performed on the entire study population. A second analysis was performed for the subset of patients in the intervention arm who recalled receiving one or both mailings. A P value less than .05 was considered statistically significant.
The cost of the educational mailings and the conduction of the study were funded through grant support from Boehringer Ingelheim and AstraZeneca Pharmaceuticals. All aspects of study design, data collection, analysis, and reporting were conducted by the study investigators and the Providence research staff.
RESULTS
Query of the EMR database revealed 13,749 active Network patients diagnosed with hypertension. Forty percent of the hypertensive population (n = 5,473) met the criteria for mild hypertension based on their last charted blood pressure. Half of these patients (n = 2,737) were mailed the hypertension educational materials.
From the total population of mild hypertensive patients, 302 patients in each arm were randomly selected to participate in the study. Eligible patients were mailed an invitation. Of these, a total of 312 patients agreed to participate in the study, 162 from the intervention group and 150 from the control group (Fig. 1).
The groups were comparable with respect to age, gender, race, income, education, awareness of hypertension diagnosis, duration of hypertension, and baseline blood pressure. No other significant differences were found, except for a 4.90% difference in the prevalence of Asian race (Table 2).
Table 2.
Baseline Characteristics
| Usual Care Group (N = 150) | Intervention Group (N = 162) | P Value | |
|---|---|---|---|
| Mean age, y (SD) | 69.3 (12.3) | 69.2 (12.4) | .920 |
| Women, % | 59 | 57 | .822 |
| Mean body mass index (± SD) | 29.6 (6.7) | 28.5 (7.1) | .157 |
| Ethnicity, % | |||
| White | 90.7 | 88.9 | .741 |
| Black | 4.0 | 1.2 | .236 |
| Hispanic | 0.7 | 2.5 | .415 |
| Pacific Islander | 1.3 | 0 | .445 |
| Asian | 0 | 4.9 | .016 |
| American Indian or Alaska Native | 1.3 | 1.2 | .999 |
| Education, y (mean ± SD) | |||
| Less than a high school diploma | 8.0 | 6.8 | .848 |
| High school graduate | 31.3 | 29.0 | .747 |
| College graduate | 15.3 | 18.5 | .550 |
| Graduate degree | 10 | 6.2 | .330 |
| Current smoker, % | 6.7 | 9.3 | .526 |
| Diabetes, % | 12.7 | 17.9 | .346 |
| Patient-reported duration of hypertension | |||
| <5 years | 35.7 | 37.1 | .670 |
| 5 to 10 years | 22.1 | 29.1 | .228 |
| >10 years | 41.0 | 33.1 | .181 |
| Baseline systolic blood pressure (SD) | 144 (7.0) | 144 (7.3) | .984 |
| Baseline diastolic blood pressure (SD) | 80 (10.2) | 82 (8.9) | .139 |
SD, standard deviation.
Blood Pressure
In the primary analysis, assessment of blood pressure between the groups showed a nonsignificant trend toward improved systolic pressure in the intervention arm as compared to control (135 mmHg vs 137 mmHg; P = .229). Blood pressure was evaluated separately in the subset of subjects in the intervention group (N = 111) who reported receiving one (n = 61) or both of the mailers (n = 50). The analysis of the subset of patients who recalled receiving the mailer showed that SBP was lower, but still not significantly different as compared to control (134 mmHg vs 137 mmHg; P = .098; Table 3).
Table 3.
Blood Pressure Assessments
| Usual Care Group | Intervention Group | P Value | Subset Recalling Mailer Receipt | P Value | |
|---|---|---|---|---|---|
| Patients, N | 150 | 162 | 111 | ||
| Systolic blood pressure, mmHg (SD) | 137 (15.4) | 135 (14.7) | .229 | 134 (13.8) | .098 |
| Diastolic blood pressure, mmHg (SD) | 77 (10.7) | 77 (11.1) | .858 | 77 (11.1) | .887 |
Hypertension Knowledge and Medication Compliance
The knowledge quiz was constructed to assess basic understanding of hypertension and the principles of self-management. Subjects in the intervention arm scored a mean 7.48 ± 1.6 as compared to 7.09 ± 1.6 in the control arm (P = .019). This difference was greater in the subset of patients who recalled receiving one or more mailers scored 7.6 ± 1.6 as compared to controls (P = .003).
Despite performance on the knowledge quiz, there was no significant difference in the proportion of subjects who were able to accurately state their blood pressure target of 140/90 mmHg (8.02% intervention vs 7.33% control; P = .999). Similarly, there was no significant difference in patient-reported medication compliance (0.35 intervention vs 0.35 control; P = ns).
Prevalence of Home Blood Pressure Monitoring
Subjects in the intervention arm reported owning a home blood pressure monitoring device more frequently than subjects in the control arm (37% vs 32%; P = .415). The intervention group also reported assessing their blood pressure more often in the previous 30 days as compared to control (8.7 days vs 5.7 days; P = .078). Intervention subjects reported a higher prevalence of logbook use as compared to control subjects (65% vs 54.2%; P = .345). However, none of these differences was statistically significant.
In the subset analysis, there was no significant difference in the proportion of subjects reporting owning a home monitoring device (40% vs 32%; P = .252); however, intervention subjects reported assessing their blood pressure significantly more often in the previous 30 days than controls (9.6 vs 5.7; P = .042). Intervention subjects also reported a significantly higher prevalence of logbook use (73% vs 54%; P = .05).
Satisfaction with Care
Patients were asked to rate their satisfaction with aspects of health care and treatment of hypertension. Patients in the intervention arm reported significantly higher satisfaction with their personal physician and respect shown by physicians and staff. Intervention patients also reported higher satisfaction with explanations of the condition of hypertension and of antihypertensive medications, as well as the frequency of blood pressure monitoring. There was a trend toward a significant increase in satisfaction with overall treatment, selection of hypertension medication, and with the amount of time spent by staff and physician in the care of hypertension in the intervention group compared with the control group (Table 4).
Table 4.
Patient Satisfaction
| Usual Care Group (N = 150) | Intervention Group (N = 162) | P Value | |
|---|---|---|---|
| Overall treatment | 8.18 | 8.51 | .180 |
| Personal physician | 8.91 | 9.28 | .037 |
| Respect shown by physician and staff | 9.12 | 9.41 | .037 |
| Explanation of hypertension | 8.09 | 8.66 | .008 |
| Explanation of hypertension medications | 7.93 | 8.51 | .017 |
| Selection of hypertension medications | 8.57 | 8.88 | .115 |
| Frequency of blood pressure monitoring | 8.01 | 8.77 | .011 |
| Staff/doctor time spent on hypertension | 7.31 | 7.84 | .078 |
1 = worst possible, 10 = best possible.
Satisfaction with Mailings
Of the 111 patients in the intervention group who reported receiving one or both of the hypertension mailings, 82% reported that it was moderately to extremely valuable. The lifestyle modification information was felt to be moderately to extremely helpful by 77% of subjects. This compares to 68% of subjects who felt the information on antihypertensive medications was moderately to extremely helpful and 61% of subjects who felt information on home monitoring was similarly helpful. Of note, 50% of subjects reported that the materials were valuable enough that they would be willing to pay out of pocket.
DISCUSSION
Management of hypertension is a critical public health issue. Inadequate control among the majority of hypertensive patients contributes significantly to the morbidity and mortality of cardiovascular disease and stroke. As is the case with other chronic conditions, hypertension control is facilitated by patient self-management, including lifestyle change and compliance and adherence to therapy. It might be hypothesized that patient awareness and knowledge about their hypertension correlate positively with self-management, but this assumption remains unproven. Time constraints imposed by the traditional health care delivery model limit the quality of hypertension education that can be delivered by a clinician in the course of an office visit. The purpose of this study was to investigate the benefits of mailed hypertension education materials to a group of patients with mildly uncontrolled hypertension. Patients are exposed to and can access health care information from multiple sources, including health insurers, government agencies, lay press, and the Internet. In this study, we have specifically evaluated the effects of printed educational materials mailed from the office of the primary care physician.
Similar to the study by Watkins et al.,11 our study failed to demonstrate a significant improvement in blood pressure as a result of mailed hypertension educational materials. However, this study did demonstrate several other tangible benefits of the mailers. Intervention patients had significantly higher scores on a knowledge survey, designed to assess basic understanding of hypertension and its management. Heightened awareness of hypertension and understanding of management goals and processes should be considered cornerstones of self-management and may promote long-term adherence to therapy. Subjects in the intervention group also had significantly higher satisfaction with their physician, and with several other aspects of their health care.
Based on these results, it does not appear that there is sufficient clinical benefit, in terms of reduced blood pressure in patients with mildly uncontrolled hypertension, to warrant the expense of educational mailings. Before abandoning this educational strategy, however, our research network is interested in investigating whether the number of mailings or the selection of the study population would result in more significant blood pressure reductions. Periodic mailings of hypertension-specific educational materials may reinforce the evolution of enhanced knowledge and satisfaction, and contribute to better long-term control of hypertension. Also, patients with hypertension that is more poorly controlled might experience greater reductions in blood pressure as a result of mailed educational materials than patients whose current blood pressure is closer to target. Elucidation of these factors will require further investigation.
Additionally, patient satisfaction is of considerable interest to physicians and provider organizations. Our study demonstrated improvements in several categories of satisfaction. Improvements in patient satisfaction may justify the resource expenditures required for mailed educational materials, irrespective of any assurance of improved hypertension control.
The characteristics of the study population support generalizability of these study results. The study was conducted in a community-based practice-based research network. As such, the study subjects may be more representative of the American hypertensive population than those participating in research conducted in a staff model or academic medical center.
There were several limitations of this study. First, the study was not powered to detect systolic or diastolic blood pressure improvements of less than 3 mmHg on the primary objective. The relatively small blood pressure decrement required to reach target in a population of patients with mildly uncontrolled hypertension may have blunted the ability to demonstrate a 3-mmHg blood pressure difference between intervention and control. Contributing to the lack of significant improvement in blood pressure was the higher than expected standard deviation of subjects’ blood pressures (15 mmHg). Second, a substantial proportion of intervention patients (31%) reported that they did not receive the mailed materials. It is not feasible to determine whether these mailings were not delivered, not opened, not read, or whether the effect of the material was so negligible in these patients that they failed to recall receipt. Third, preferred language and literacy for the English language in the study population is not known. As such, it may be difficult to generalize these findings to primary care patients who do not speak English or have a low level literacy.
Conclusion
Educational hypertension mailers sent from the office of the primary care physician result in improvements in patient knowledge, frequency of home monitoring, and satisfaction with care. In patients with mildly uncontrolled hypertension, educational mailers did not yield a significant decrease in blood pressure. Further investigation is needed to determine the effect of educational mailers in patients with moderate to severe hypertension.
Acknowledgments
Grant support from Boehringer Ingelheim and AstraZeneca Pharmaceuticals was used to fund the cost of the educational mailings and the conduction of the study. All data collection, analysis, and reporting was conducted by the study investigators and the PBRN research staff. The investigators report no other conflict of interest.
APPENDIX: Patient Hypertension Knowledge Quiz
From your memory, mark the correct box after each of the statements below
| True | False | Don't Know | |
|---|---|---|---|
| a. Hypertension mainly affects people who are under a lot of stress. | ○ | ○ | ○ |
| b. Home blood pressure monitoring is never reliable. | ○ | ○ | ○ |
| c. If your doctor prescribes medication for high blood pressure, it is important to take it every day. | ○ | ○ | ○ |
| d. Your blood pressure goal is 100 plus your age. | ○ | ○ | ○ |
| e. A beta-blocker is a medication often prescribed for high blood pressure. | ○ | ○ | ○ |
| f. High blood pressure is not very common. | ○ | ○ | ○ |
| g. High blood pressure can increase your risk for stroke. | ○ | ○ | ○ |
| h. High blood pressure usually causes no symptoms. | ○ | ○ | ○ |
| i. Once your blood pressure improves to normal levels, you should stop your medication. | ○ | ○ | ○ |
| j. If you have high blood pressure you should try to increase the amount of salt in your diet. | ○ | ○ | ○ |
REFERENCES
- 1.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 2.Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population: results from the third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;26:60–9. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 3.Gueyffier F, Boutitie F, Boissel JP, et al. Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. A meta-analysis of individual patient data from randomized, controlled trials. The INDANA Investigators. Ann Intern Med. 1997;126:761–7. doi: 10.7326/0003-4819-126-10-199705150-00002. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 5.Clark NM. Management of chronic disease by patients. Annu Rev Public Health. 2003;24:289–313. doi: 10.1146/annurev.publhealth.24.100901.141021. [DOI] [PubMed] [Google Scholar]
- 6.Neutel JM, Smith DH. Improving patient compliance: a major goal in the management of hypertension. J Clin Hypertens. 2003;5:127–32. doi: 10.1111/j.1524-6175.2003.00495.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.St. George IM. Patient education leaflet for hypertension: a controlled study. J R Coll Gen Pract. 1983;33:508–10. [PMC free article] [PubMed] [Google Scholar]
- 8.Laher M, O'Malley K, O'Brien E, O'Hanrahan M, O'Boyle C. Educational value of printed information for patients with hypertension. Br Med J (Clin Res Ed) 1981;282:1360–1. doi: 10.1136/bmj.282.6273.1360-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray DM, Kurth CL, Finnegan JR, Pirie PL, Admire JB, Luepker RV. Direct mail as a prompt for follow-up care among persons at risk for hypertension. Am J Prev Med. 1988;4:331–5. [PubMed] [Google Scholar]
- 10.Newell S, Girgis A, Sanson-Fisher RW. Recall, retention, utilisation and acceptability of written health education materials. Aust J Public Health. 1995;19:368–74. doi: 10.1111/j.1753-6405.1995.tb00388.x. [DOI] [PubMed] [Google Scholar]
- 11.Watkins CJ, Papacosta AO, Chinn S, Martin J. A randomized controlled trial of an information booklet for hypertensive patients in general practice. J R Coll Gen Pract. 1987;37:548–50. [PMC free article] [PubMed] [Google Scholar]
- 12.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]