Abstract
OBJECTIVES
While patient-centered care (PCC) is desirable for many reasons, its relationship to treatment outcomes is controversial. We evaluated the relationship between PCC and the provision of preventive services.
METHODS
We obtained facility-level estimates of how well each VA hospital provided PCC from the 1999 ambulatory Veterans Satisfaction Survey. PCC delivery was measured by the average percentage of responses per facility indicating satisfactory performance from items in 8 PCC domains: access, incorporating patient preferences, patient education, emotional support, visit coordination, overall coordination of care, continuity, and courtesy. Additional predictors included patient population and facility characteristics. Our outcome was a previously validated hospital-level benchmarking score describing facility-level performance across 12 U.S. Preventive Services Task Force-recommended interventions, using the 1999 Veterans Health Survey.
RESULTS
Facility-level delivery of preventive services ranged from an overall mean of 90% compliance for influenza vaccinations to 18% for screening for seat belt use. Mean overall PCC scores ranged from excellent (>90% for the continuity of care and courtesy of care PCC domains) to modest (<70% for patient education). Correlates of better preventive service delivery included how often patients were able to discuss their concerns with their provider, the percent of visits at which patients saw their usual provider, and the percent of patients receiving >90% of care from a VA hospital.
CONCLUSION
Improved communication between patients and providers, and continuity of care are associated with increased provision of preventive services, while other aspects of PCC are not strongly related to delivery of preventive services.
Keywords: prevention, patient-centered care, primary care, benchmarking, patient-doctor communication
Prevention is a vital component of improving individual and public health.1 However, clinicians often fail to provide recommended preventive services.2–5 Commonly cited barriers to preventive care include insufficient time during the clinical encounter, organizational barriers, physician beliefs and knowledge concerning the evidence supporting the guidelines, and the lack of financial incentives encouraging prevention.6–10 Another potential barrier to delivering preventive services is failure to provide patient-centered care (PCC), which can be defined as care that elicits, respects, and incorporates patients’ wishes.11–14 PCC is considered desirable in its own right, but it is not known whether PCC is related to improved delivery of preventive care, or whether particular aspects of PCC are more strongly related to prevention.
This paper examines the hypothesis that facilities that provide patient-centered ambulatory care are more likely to deliver recommended preventive services. Our work builds on an analysis of benchmarking methods15 that provides estimates of preventive services delivery across a range of recommended interventions at the facility level. The Veteran's Satisfaction Survey (VSS),16 a validated patient satisfaction instrument based on a similar instrument developed by the Picker Foundation,17,18 was used to measure the degree of PCC at each facility across the 8 dimensions of PCC defined by the VA. The relationships between preventive services delivery and organizational and patient population characteristics were also examined.
The Veterans Health Administration (VHA), as the largest integrated delivery system in the United States, offers an excellent opportunity to examine the relationship between PCC and prevention. The VHA has been reengineering care to encourage prevention since 1995.19–21 However, preventive services delivery varies substantially at the facility level.15 With its rich data sources measuring PCC and performance in delivering preventive care, the VHA is an attractive natural laboratory in which to study our hypotheses that improved delivery of PCC is related to improved delivery of standard preventive services, and that this relationship varies across the different dimensions of PCC.
Conceptual Model
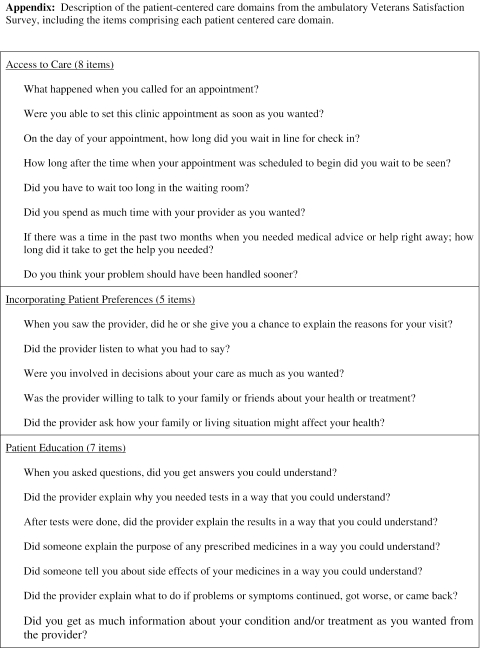
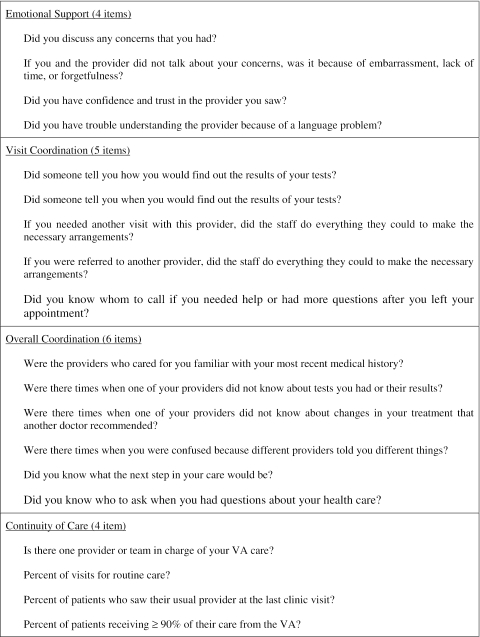
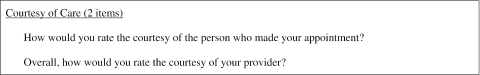
PCC is a multidimensional construct, composed of different domains, or aspects, of patient-focused care. We examine the 8 domains of PCC as defined and measured by the VHA16: 1) access to care, 2) incorporating patient preferences, 3) patient education, 4) visit coordination, 5) overall coordination of care, 6) courtesy of care, 7) continuity of care, and 8) emotional support. By examining the relationship between these dimensions of PCC and the level of benchmarking performance at the facility, we can determine the extent to which specific aspects of PCC are related to prevention delivery. Making the distinction between different aspects of PCC is important because not all experts agree on what constitutes PCC; some experts classify certain of our PCC domains (e.g., access to care, coordination of care, continuity of care) as elements of primary care as opposed to PCC.11,12
It is theoretically likely that some PCC domains are more strongly related to prevention than others. Greater incorporation of patient preferences and emotional support for patients might lead to patients’ requesting more prevention than would otherwise be supplied.22 Greater access to care could increase the amount of time during which preventive care might occur, and decrease the likelihood of acute complaints “crowding out” prevention. It is possible that greater continuity and coordination of care could improve clinicians’ knowledge of the patient, leading to more prevention. Other PCC domains, such as courtesy and visit coordination, are likely to have a more indirect effect on prevention, and, therefore, we hypothesized that these 2 aspects of PCC would be more weakly related to prevention than PCC domains reflecting more direct patient involvement.
Patient population characteristics might also influence the perceived benefits of prevention and how frequently prevention is delivered. For example, educational attainment, age, and health status have all been related to delivery of preventive services.23–30 In addition, organizational characteristics (e.g., teaching status), organizational capacity (e.g., bed size, number of employees), and employee qualifications appear to influence the likelihood of delivering preventive services.31
METHODS
This project investigated the variation in a previously validated measure of preventive service delivery that reflects facility performance across 12 U.S. Preventive Services Task Force (USPSTF)-recommended prevention activities.1 Explanatory variables reflecting the degree of PCC at each hospital and patient and organizational variables were measured at the hospital level, due to our interest in understanding performance at the organizational level.
Data Sources and Variables
The data used in this analysis were from 3 national surveys conducted in 1999: the Veterans Health Survey,32–35 the VSS, and the American Hospital Association Annual Survey.36
Veterans Health Survey (VHS)
The VHS contains patient-reported information on receipt of a broad range of preventive services recommended for all average-risk veterans during the previous year. Survey respondent characteristics, such as age, gender, health status, amount of care received at a VHA hospital, and travel time to a VHA hospital are also included. The VHS was collected from a national sample of nearly 40,000 patients who had received outpatient primary care in the prior year. The sample was stratified by gender (300 men and 150 women if available) for a total of 450 veterans from each VHA facility. The VHS had a 68% response rate.
Veterans Satisfaction Survey (VSS)
This survey was sent to a sample of up to 175 veterans at each VHA facility who received outpatient primary care. Detailed patient perceptions of their most recent clinical encounter in the VHA ambulatory setting are available in the outpatient VSS, and serve as measures of PCC. The VSS had a 73% response rate.
American Hospital Association (AHA) Annual Survey
The AHA survey is a national survey of U.S. hospitals that contains measures of organizational size, clinical orientation, resources, and employee qualifications for each facility.
Dependent Measures
Our dependent variable was a benchmarking score that reflected preventive service delivery across 12 recommended interventions (screening for hypertension, alcohol abuse, and seat belt use, counseling to reduce cigarette use, increase physical activity, and lose excess weight, and ordering of cholesterol tests, fecal occult blood tests, vaccinations against tetanus, influenza, and pneumococcal infections, and flexible sigmoidoscopy) as reported by respondents in the 1999 VHS. VHS scores were adjusted by excluding responses from items that did not apply to respondents (e.g., counseling for cigarette cessation among nonsmokers).15 All 12 preventive services are broadly accepted, indicated for normal-risk ambulatory patients, and are recommended by both the USPSTF and the VHA. Because of the small number of female patients in some facilities surveyed, we excluded 2 services (cervical Pap smear screening and mammography) that applied only to females.
Patients receiving care at VHA facilities were surveyed about whether they had received preventive services within an appropriate time frame at either the VHA or at a non-VHA facility. Veterans were counted as receiving the service regardless of where it was performed, so that facilities were not penalized for services provided elsewhere. In addition, we included the percent of patients receiving more than 90% of their care from the VA as a predictor reflecting enhanced continuity of care.
A previously published benchmarking method was used to describe facility-level performance of preventive care delivery.15 This methodology identified facilities that provided high levels of consistent adherence across a variety of performance measures and included the following steps. First, all hospitals were ranked based on their adherence rate for each of the 12 services relative to other hospitals, and the ranks were converted to percentile scores. Second, a value of 1 was assigned if the hospital performed above the 50th percentile for a given service, and a value of 2 was assigned if the hospital performed above the 75th percentile. Thus, for each of the 12 preventive services evaluated, a hospital could be assigned 0, 1, or 2 points. Third, the scores for the 12 preventive services were summed to obtain the hospital's overall score. The possible range of overall scores was 0 to 24.
Independent Measures
All independent variables were measured at the facility level. To measure PCC performance, we grouped independent variables into the 8 PCC domains using the VA's proposed variable classification scheme (with the addition of items in the continuity of care domain) and assessed the internal reliability of the 8 PCC scores with Crohnbach's α (see Appendix available online at http://www.jgim.org for a description of the items within each domain). Six scales had an α > .70; for those domains, we used the PCC scales from the VSS. For the 2 domains with α < .70 (emotional support, α= 0.37, and continuity of care, α= 0.24), we considered the variables from those domains as individual items. To control for confounding factors, we created domains reflecting patient population characteristics, clinical emphasis, organizational capacity, and the work setting.
For the 6 PCC domains with α > .70, we calculated scores based on the “problem scores” as defined by the VHA. The VHA defines the problem score for a domain as the average percent of patients reporting a “problem” answer on each of the questions within a given PCC domain.16 We subtracted the problem score from 100 to obtain a PCC score with a more intuitive interpretation (i.e., a higher number represents better PCC).
Statistical Analysis
Explanatory variables were systematically evaluated to develop a multivariable regression equation explaining the benchmarking scores. Initial models considered conceptually related predictors from within each domain.37 The benchmarking scores were regressed on each explanatory variable using ordinary least squares (OLS), due to the approximately normal distribution of the benchmarking scores (mean = 9, median = 8, range = 0 to 18). Domain models were developed evaluating variables that were related to the outcome at P < .25. A multivariable regression model was performed within each domain, retaining variables significant at P < .15.
To determine our final set of predictors, the benchmarking scores were regressed on all variables that were retained in the within-domain regressions. The final model retained variables significant at P < .05.
To examine the relationship between our final set of predictors and the provision of individual preventive service items, we regressed the hospital's performance for each preventive service (measured by their percentile rank for performing the service) on our final predictors using OLS.
OLS regression was also performed considering simultaneously all variables significant in univariate models at P < .25, to investigate whether the results were influenced by the modeling approach used. Regression diagnostics were conducted to investigate the assumptions underlying the use of OLS. Our use of facility-level data assumes independent observations across hospitals. All analyses were done with SAS, version 8.02 (SAS Institute, Cary, NC).
RESULTS
Descriptive statistics for the explanatory and outcome variables are shown in Table 1. and 2. Because our data included information collected throughout the VHA, the sample characteristics reflect the VHA system (n = 141). One half (50%) of facilities were members of the Council of Teaching Hospitals, with an average bed size of 335 and occupancy rate of 79%. Facilities averaged 268,134 nonemergency outpatient visits per year, and employed an average of 1,408 people.
Table 1.
Descriptive Statistics for Explanatory Variables Measured at the Facility Level (N = 141)
| Explanatory Variables | Mean or Percent | Standard Deviation | Range |
|---|---|---|---|
| Patient population | |||
| White, % | 82 | 17 | 4 to 100 |
| Black, % | 14 | 15 | 0 to 64 |
| Hispanic, % | 3 | 9 | 0 to 95 |
| ≥65 years old, % | 56 | 9 | 33 to 81 |
| Male, % | 95 | 2 | 82 to 100 |
| With no education beyond high school, % | 56 | 10 | 27 to 76 |
| Reporting excellent health status, % | 5 | 2 | 1 to 16 |
| Traveling at least 1 hour to get to the VA, % | 37 | 14 | 11 to 78 |
| Clinical emphasis | |||
| Council of Teaching Hospitals members, % | 50 | ||
| With a residency training program. % | 71 | ||
| Number of trainee and resident FTEs, % | 63 | 79 | 0 to 408 |
| Organizational capacity | |||
| Bed size | 335 | 281 | 41 to 1,852 |
| Number of employees | 1,408 | 881 | 305 to 6,136 |
| Nonemergency outpatient visits per year | 268,134 | 161,554 | 45,311 to 1,130,527 |
| Ratio of FTEs to average daily census | 7 | 4 | 2 to 27 |
| Physician FTEs per 1,000 outpatient visits | 0.3 | 0.1 | 0.1 to 0.6 |
| Nurses who are RNs, % | 77 | 8 | 46 to 100 |
| In a rural setting, % | 16 | ||
| Patient-centered care domains* | |||
| Access to care | 74 | 6 | 58 to 88 |
| Incorporating patient preferences | 71 | 4 | 53 to 81 |
| Patient education | 68 | 5 | 53 to 79 |
| Visit coordination | 84 | 3 | 75 to 91 |
| Overall coordination | 70 | 4 | 59 to 79 |
| Courtesy of care | 93 | 3 | 85 to 98 |
| Continuity of care† | |||
| Patients for whom there is one provider or team in charge of their VA care, % | 90 | 4 | 78 to 98 |
| Visits for routine care, % | 64 | 5 | 48 to 78 |
| Patients who saw their usual provider at the last clinic visit, % | 73 | 6 | 51 to 89 |
| Patients receiving ≥90% of their care from the VA, % | 56 | 9 | 25 to 75 |
| Emotional support† | |||
| Did you discuss any concerns that you had?, % | 80 | 4 | 65 to 91 |
| If you and the provider did not talk about your concerns, was it because of embarrassment, lack of time, or forgetfulness?, % | 63 | 6 | 42 to 79 |
| Did you have confidence and trust in the provider you saw?, % | 71 | 5 | 55 to 84 |
| Did you have trouble understanding the provider because of a language problem?, % | 12 | 9 | 0 to 43 |
See Appendix available online at http://www.jgim.org for listing of items within each domain.
Items within these domains were analyzed separately based on factor analysis results.
FTE, full-time employee.
Table 2.
Descriptive Statistics for Outcome Variables
| Outcome Variables | Mean or Percent | Standard Deviation | Range |
|---|---|---|---|
| Mean facility benchmarking score* | 9 | 4 | 0 to 18 |
| Screened for hypertension, % | 82 | 4 | 69 to 92 |
| Screened for alcohol abuse, % | 39 | 5 | 27 to 53 |
| Screened for seat belt use, % | 18 | 6 | 5 to 38 |
| Counseled to quit cigarettes, % | 83 | 5 | 66 to 92 |
| Counseled to increase physical activity, % | 62 | 5 | 47 to 76 |
| Counseled to lose weight, % | 72 | 7 | 48 to 91 |
| With cholesterol screening, % | 77 | 6 | 59 to 89 |
| With fecal occult blood screening, % | 44 | 8 | 25 to 62 |
| With tetanus vaccination, % | 73 | 9 | 42 to 88 |
| With influenza vaccination, % | 90 | 4 | 64 to 97 |
| With pneumococcal vaccination, % | 76 | 7 | 40 to 91 |
| Undergoing flexible sigmoidoscopy, % | 53 | 9 | 27 to 73 |
Facility-level compliance rates with recommended preventive services based on the 1999 nationwide Veterans Health Survey. Percentages indicate the percent of respondents who received recommended services within an appropriate time frame at either the VHA or at a non-VHA facility.
Hospital-level benchmarking scores were developed by ranking adherence rates for each of the 12 services relative to other hospitals, and converting the ranks to percentile scores. A value of 1 was assigned if the hospital performed above the 50th percentile for a given service, and a value of 2 was assigned if the hospital performed above the 75th percentile. Scores for each service were summed to determine each hospital's benchmarking score.
As previously reported, there was considerable variation in receipt of preventive services and in benchmarking scores.15 Some interventions were performed on more than 80% of patients (hypertension screening, flu shots, counseling smokers to quit), while others were performed for less than 50% of patients (alcohol screening, seat belt screening, fecal occult blood testing). In general, interventions requiring a laboratory test or immunization were performed more frequently than interventions requiring more time and discussion. However, one time-intensive item, counseling for cigarette smoking cessation, was done fairly often. For every intervention, though, compliance rates indicated room for improvement. The benchmarking scores had an overall mean of 9 (standard deviation [SD] of 5, range from 0 to 18). Thus, none of the hospitals performed at greater than the 75th percentile for 10 or more of the 12 services.
There was significant variation in the degree of PCC, with specific domains identifying opportunities for improvement. On the whole, VHA hospitals performed best in the courtesy domain, with no problems reported on 93% of the items from that domain. In contrast, the patient education domain indicated the most room for improvement (score of 68%), and only 71% reported moderate or complete trust in their provider. When patients were not able to discuss their concerns, 63% reported this occurred because of embarrassment, lack of time, or forgetfulness.
In univariate regressions, better performance in 2 PCC domains, incorporating patient preferences and overall coordination of care, were highly related to higher prevention benchmarking scores (Table 3 and Table 4). Most of the other PCC domains were positively related to prevention, but the relationships only approached significance. Several individual items reflecting continuity of care and emotional support were significant in the expected directions.
Table 3.
Univariate Regression Results for the Relationship Between Hospital Characteristics and Benchmarking Scores
| Explanatory Variables | Beta | Standard Error | P Value |
|---|---|---|---|
| Patient population | |||
| White, % | 0.04 | 0.02 | .08 |
| Black, % | −0.02 | 0.03 | .35 |
| Hispanic, % | 0.06 | 0.04 | .13 |
| ≥65 years old, % | 0.06 | 0.04 | .14 |
| Male, % | 0.06 | 0.15 | .70 |
| With no education beyond high school, % | 0.11 | 0.04 | <.01 |
| Reporting excellent health status, % | −0.30 | 0.15 | .05 |
| Traveling at least 1 hour to get to the VA, % | 0.02 | 0.03 | .39 |
| Clinical emphasis | |||
| Council of Teaching Hospitals member | 0.18 | 0.78 | .82 |
| Residency training program | 0.30 | 0.86 | .73 |
| Number of trainee and resident FTEs | −0.00 | 0.00 | .41 |
| Organizational capacity | |||
| Bed size | −0.00 | 0.00 | .28 |
| Number of employees | −0.00 | 0.00 | .28 |
| Nonemergency outpatient visits per year | −0.00 | 0.00 | .29 |
| Ratio of FTEs to average daily census | −0.08 | 0.10 | .44 |
| Physician FTEs per 1,000 outpatient visits | −3.65 | 4.13 | .38 |
| Work setting | |||
| Nurses who are RNs, % | −0.07 | 0.05 | .16 |
| In rural setting, % | −0.88 | 1.07 | .41 |
Variables significant at P < .25 in univariate regression were considered for the “within domain” regressions.
FTE, full-time employee.
Table 4.
Univariate Regression Results for Patient-centered Care Performance and Benchmarking Scores
| Explanatory Variables | Beta | Standard Error | P Value |
|---|---|---|---|
| Patient-centered care domains | |||
| Access to care | 0.09 | 0.07 | .16 |
| Incorporating patient preferences | 0.25 | 0.09 | <.01 |
| Patient education | 0.14 | 0.08 | .08 |
| Visit coordination | 0.18 | 0.12 | .13 |
| Overall coordination | 0.22 | 0.09 | .02 |
| Courtesy of care | 0.23 | 0.15 | .11 |
| Continuity of care | |||
| Patients for whom there is one provider or team in charge of their VA care, % | 0.16 | 0.10 | .10 |
| Visits for routine care, % | 0.16 | 0.07 | .03 |
| Patients receiving ≥90% of their care from the VA, % | 0.07 | 0.04 | .09 |
| Emotional support | |||
| Did you discuss any concerns that you had? | 0.28 | 0.08 | <.01 |
| If you and the provider did not talk about your concerns, was it because of embarrassment, lack of time, or forgetfulness? | 0.08 | 0.06 | .17 |
| Did you have confidence and trust in the provider you saw? | 0.15 | 0.07 | .04 |
| Did you have trouble understanding the provider because of a language problem? | 0.05 | 0.04 | .29 |
Variables significant at P < .25 in univariate regression were considered for the “within domain” regressions.
Several patient population and continuity of care measures were significantly related to prevention in univariate regressions. Greater percentages of patients with less than a high school education and patients reporting less than excellent health were associated with more preventive care. There were no significant associations between prevention and organizational characteristics.
Within-domain regression models indicated several significant measures including incorporating patient preferences, the percent of patients who had concerns but did not discuss them, the percent of patients with less than a high school education, the percent seeing their usual provider at their last clinic visit, and the percent receiving more than 90% of their care from the VHA (Table 5).
Table 5.
Variables Significant in Domain Regressions
| Explanatory Variables | Beta | Standard Error | P Value |
|---|---|---|---|
| Patient population | |||
| With no education beyond high school, % | 0.11 | 0.04 | <.01 |
| Patient-centered care domains | |||
| Access to care | −0.13 | 0.08 | .12 |
| Incorporating patient preferences | 0.34 | 0.18 | .06 |
| Patient education | −0.28 | 0.14 | .06 |
| Patients who saw their usual provider at the last clinic visit, % | 0.17 | 0.06 | <.01 |
| Patients receiving ≥90% of their care from the VA, % | 0.11 | 0.04 | <.01 |
| Patients who had concerns they wanted to discuss but did not—% no | 0.41 | 0.12 | <.01 |
Our final multivariable equation included 2 measures of continuity of care (greater percentage of overall care received at the VHA, and an increased frequency of seeing one's usual provider at the last clinic visit) and the emotional support item (the percent of patients who had concerns to discuss but did not raise them). The adjusted R2 of .15 indicates that unmeasured factors play a large role in the provision of prevention services (Table 6). Results from the fully saturated OLS regression (i.e., no stepwise procedure) using predictors significant in univariate regressions at P < .25 produced almost identical results.
Table 6.
Final Multivariate Regression>
| Explanatory Variables | Beta | Standard Error | P Value |
|---|---|---|---|
| Percent of patients who had concerns they wanted to discuss but did not—% no | 0.31 | 0.08 | <.01 |
| Patients who saw their usual provider at the last clinic visit, % | 0.18 | 0.05 | <.01 |
| Patients receiving ≥90% of their care from the VA, % | 0.10 | 0.04 | <.01 |
Adjusted R2 = 0.17. N = 141.
Regressions for the individual preventive service items revealed several findings. One preventive item, counseling for tobacco cessation, was significantly related to all 3 predictors in our final model. Another item, the ordering of fecal occult blood testing, was related to being able to discuss concerns and seeing one's usual provider. Each of the 3 predictors was significantly related to multiple preventive services (range of 4 to 6).
Regression diagnostics did not indicate problems. There was no obvious relationship between predicted values and residuals, the distribution of the residuals did not appear to violate the assumption of normality, and the variance inflation factors did not indicate multicolinearity.
DISCUSSION
Our results suggest that some components of PCC are related to prevention activities at the hospital level. Two particular aspects of PCC—improved communication between patients and providers, and continuity of care—are associated with improved preventive care delivery, while other aspects of PCC have a weaker relationship to prevention. These results underscore the importance of further defining the elements of PCC and determining how each element contributes to important health outcomes. Most of the elements of PCC, while desirable in their own right, were not significantly related to prevention in our multivariate analysis. Two relatively time-consuming preventive items, counseling for tobacco cessation and ordering fecal occult blood testing, appear to be most strongly related to PCC; continuity of care and improved communication between patients and providers were related to multiple preventive services.
Neither the relationship between PCC and outcomes nor the mechanism whereby PCC might improve outcomes is well defined. Research has shown that greater patient centeredness is related to improved patient satisfaction and symptom improvement38–40 and improved treatment of chronic diseases (diabetes mellitus, hypertension).41–43 However, other studies have failed to demonstrate any association between PCC and outcomes other than patient satisfaction.44–50
The finding that better performance in discussing issues of importance to patients is related to improved prevention activity raises questions about how and why this occurs. It is possible, for example, that patients prefer to receive more prevention than is routinely provided, and this discrepancy is addressed through improved communication. Or, improvements in physician-patient communication might make prevention easier to accomplish by reducing the “friction costs” associated with poor communication. Interventions to reduce the commonly cited reasons for not discussing concerns (lack of time, embarrassment, forgetfulness) are needed.
Consistent with other studies, this research found that an ongoing relationship with a primary care physician enhances the delivery of preventive care.51–54 The inclusion of continuity of care as an element of PCC is controversial; some experts would classify continuity as an element of primary care as opposed to PCC. However, others have categorized elements of continuity under the topic of patient-centered access.55 It is important to note that our analytical approach makes it unlikely that improved continuity of care is serving as a “proxy” for other aspects of PCC. Continuity of care might enhance prevention by facilitating the transfer of information between patients and providers. In addition, continuity of care may build trust between the provider and the patient, leading to greater likelihood of open communication. There may also be a sense of obligation on the part of the patient about receiving services that entail receiving extra testing or vaccinations.
Unfortunately, not all primary care encounters are with one's regular physician. Economic forces may disrupt continuity of care and diminish quality of care. Efforts to promote continuity of care should be emphasized, or in lieu of that, provision of patient-specific information regarding previous delivery of preventive care and recommended quality of care measures should be encouraged at the clinical encounter.
The control variables representing patient population and organizational characteristics were generally not significant. The univariate finding that lower educational status is associated with enhanced prevention did not hold up in the multivariable analysis. Our results stress understanding the “microenvironment” of the clinical encounter, and suggest that improvements in prevention may result from improving the quality of clinical encounters.
This study has a number of strengths. The VHA is an excellent setting in which to examine the role of PCC, because of the comprehensive, national scale of the data, and because other important factors are either controlled for or do not apply to the VHA. Clinicians are paid on a salary basis, so financial incentives to physicians are not commonly used, and all patients are eligible to receive preventive services. An additional strength is our use of previously validated measures of PCC and prevention delivery.16–18 Using data from the VSS provided us with information that would otherwise have been difficult, if not impossible, to obtain. Because the benchmarking score we chose as the outcome variable for this study reflects service delivery across 12 preventive services, our findings are likely robust across a wide range of preventive services. Our findings are strengthened by the fact that our explanatory and outcome variables were obtained independently of one another, reducing the chances of a “common source” bias.
The limitations of this study should be kept in mind. We did not have information on physician beliefs concerning the value of our set of preventive services. However, the preventive services we examined are evidence based, widely accepted, and recommended by the VHA and the USPSTF, thereby reducing the likelihood that unmeasured physician beliefs confounded the results. In addition, organizational characteristics, which are likely correlated with physician beliefs (e.g., teaching status of hospital and beliefs of academic physicians), were not significant. The accuracy of patient reports for each of the variables considered has not been evaluated, and may be inaccurate. Previous studies, however, have demonstrated good recall of VHA patients for several of the items in this study: receipt of influenza and pneumococcal vaccinations,56 tobacco counseling,57 and hypertension and alcohol screening.15 Inaccurate reporting of preventive services would lead to measurement error, which increases the difficulty of establishing significant relationships. Thus, our results may be conservative estimates. It is not known whether there is a systematic bias in the reporting of preventive services, but our use of data from different sources limits the effect of biased reporting. Finally, because the variables were measured at the hospital level using different data sources, the results are subject to the ecological fallacy. However, the level of detail available to us in the VSS and VHS data reduces the chances of finding a spurious relationship due to an omitted variable.
Our findings indicate several potentially fruitful areas for research, as well as an important take home message for clinicians and administrators. Improvements in certain aspects of PCC, namely continuity of care and emotional support, as manifested in improved communication between patients and providers, appear to be associated with improved preventive care delivery. Further research is needed to delineate the differential effect of various PCC domains on other health outcomes and the mechanisms whereby improved PCC leads to improved outcomes. In addition, further investigation regarding why some settings have a more patient-centered culture, or how they facilitate PCC is needed. Efforts to facilitate PCC may result in improvements in delivery of preventive services and better health outcomes.
Acknowledgments
The research reported here was supported by the Department of Veterans Affairs, the Veterans Health Administration, Health Services Research and Development Service, Investigator Initiated Research grants CPI 99-126 and CPI 01-141, and the VA Quality Enhancement Research Initiative.
Dr. Flach is a staff physician and HSR&D Career Development Award recipient at the Iowa City VAMC. Dr. Doebbeling is principal investigator for this grant, staff physician, and director of the Research Enhancement Award Program in Health Services Research at the Roudebush Veterans Affairs Medical Center, Indianapolis, Ind.
We appreciate the efforts of the respondents to this survey. Toni Tripp-Reimer, PhD, Bernard Sorofman, PhD, and Jane E. DeWitt, PhD helped with survey development. We would like to recognize the contributions of the Research Enhancement Award Program staff at the Iowa City VAMC, especially Elise Acosta and Carrie Franciscus, and thank them for their assistance in preparing this manuscript. Staff at the Public Policy Center at the University of Iowa provided valuable assistance in reviewing and preparing the manuscript.
Appendix
REFERENCES
- 1.Agency for Health Care Research and Quality. Guide to Clinical Preventive Services. 3rd ed. Washington, DC: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- 2.McGlynn EA, Cassel CK, Leatherman ST, DeCristofaro A, Smits HL. Establishing national goals for quality improvement. Med Care. 2003;41(1 suppl):I16–I29. doi: 10.1097/00005650-200301001-00003. [DOI] [PubMed] [Google Scholar]
- 3.Walsh JM, McPhee SJ. Prevention in the year 2002: some news, some issues. Prim Care. 2002;29:727–49. doi: 10.1016/s0095-4543(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 4.Solberg LI, Kottke TE, Brekke ML. Variation in clinical preventive services. Eff Clin Pract. 2001;4:121–6. [PubMed] [Google Scholar]
- 5.Davis K, Schoenbaum SC, Collins KS, Tenney K, Hughes DL, Audet AM. Room for Improvement: Patients Report on the Quality of Their Health Care. The Commonwealth Fund. 2002.
- 6.Hulscher ME, Wensing M, Grol RP, van der Weijden T, van Weel C. Interventions to improve the delivery of preventive services in primary care. Am J Public Health. 1999;89:737–46. doi: 10.2105/ajph.89.5.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson LA, Janes GR, Jenkins C. Implementing preventive services: to what extent can we change provider performance in ambulatory care? A review of the screening, immunization, and counseling literature. Ann Behav Med. 1998;20:161–7. doi: 10.1007/BF02884956. [DOI] [PubMed] [Google Scholar]
- 8.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 9.Mullahy J. It’ll only hurt a second? Microeconomic determinants of who gets flu shots. Health Econ. 1999;8:9–24. doi: 10.1002/(sici)1099-1050(199902)8:1<9::aid-hec396>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 10.Kenkel D. The demand for preventive medical care. Appl Econ. 1994;26:313–25. [Google Scholar]
- 11.Institute of Medicine (IOM) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 12.Mead N, Bower P. Patient-centeredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51:1087–110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 13.Stewart M, Brown JB, Weston WW, McWhinney IR, McWilliam CL, Freeman TR. Patient-centered Medicine: Transforming the Clinical Method. Thousand Oaks, Calif: Sage Publications; 1995. [Google Scholar]
- 14.Epstein RM. The science of patient-centered care. J Fam Pract. 2000;49:805–7. [PubMed] [Google Scholar]
- 15.Doebbeling BN, Vaughn TE, Woolson RF, et al. Benchmarking veterans affairs medical centers in the delivery of preventive health services: comparison of methods. Med Care. 2002;40:540–54. doi: 10.1097/00005650-200206000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Performance on Customer Service Standards, Ambulatory Care: 1999 National Survey Report. Washington, DC: Veterans Health Administration; 2000. National Performance Feedback Center and Office of Quality and Performance, Department of Veterans Affairs. [Google Scholar]
- 17.Edgman-Levitan S, Cleary PD. What information do consumers want and need? Health Aff. 1996;15:42–56. doi: 10.1377/hlthaff.15.4.42. [DOI] [PubMed] [Google Scholar]
- 18.Beatrice DF, Thomas CP, Biles B. Grant making with an impact: the picker/commonwealth patient-centered care program. Health Aff. 1998;17:236–44. doi: 10.1377/hlthaff.17.1.236. [DOI] [PubMed] [Google Scholar]
- 19.Feussner JR, Kizer KW, Demakis JG. The quality enhancement research initiative (QUERI): from evidence to action. Med Care. 2000;38(1 suppl):I1–I6. doi: 10.1097/00005650-200006001-00001. [DOI] [PubMed] [Google Scholar]
- 20.Kizer KW, Demakis JG, Feussner JR. Reinventing VA health care: systematizing quality improvement and quality innovation. Med Care. 2000;38(1 suppl):I7–I16. [PubMed] [Google Scholar]
- 21.Department of Veterans Affairs. VA Handbook 1101.8. Health Promotion and Disease Prevention. RCN-10-06666. Washington, DC: US Government Printing Office; 1996. [Google Scholar]
- 22.Kenkel DS. Prevention. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Vol. 2. New York, NY: Elsevier Science; 2000. pp. 1675–720. [Google Scholar]
- 23.Hegarty V, Burchett BM, Gold DT, Cohen HJ. Racial differences in use of cancer prevention services among older Americans. J Am Geriatr Soc. 2000;48:735–40. doi: 10.1111/j.1532-5415.2000.tb04746.x. [DOI] [PubMed] [Google Scholar]
- 24.Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Med Care. 1998;36:180–9. doi: 10.1097/00005650-199802000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Franks P, Fiscella K. Effect of patient socioeconomic status on physician profiles for prevention, disease management, and diagnostic testing costs. Med Care. 2002;40:717–24. doi: 10.1097/00005650-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Moinpour CM, Lovato LC, Thompson IM, Jr, et al. Profile of men randomized to the prostate cancer prevention trial: baseline health-related quality of life, urinary and sexual functioning, and health behaviors. J Clin Oncol. 2000;18:1942–53. doi: 10.1200/JCO.2000.18.9.1942. [DOI] [PubMed] [Google Scholar]
- 27.Devons CA. Comprehensive geriatric assessment: making the most of the aging years. Curr Opin Clin Nutr Metab Care. 2002;5:19–24. doi: 10.1097/00075197-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Hogan DB, Fung TS, Ebly EM. Health, function and survival of a cohort of very old Canadians: results from the second wave of the Canadian study of health and aging. Can J Public Health. 1999;90:338–42. doi: 10.1007/BF03404524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sundquist J, Johansson SE. Impaired health status, and mental health, lower vitality and social functioning in women general practitioners in Sweden. A cross-sectional survey. Scand J Prim Health Care. 1999;17:81–6. doi: 10.1080/028134399750002692. [DOI] [PubMed] [Google Scholar]
- 30.Weinehall L, Hallgren CG, Westman G, Janlert U, Wall S. Reduction of selection bias in primary prevention of cardiovascular disease through involvement of primary health care. Scand J Prim Health Care. 1998;16:171–6. doi: 10.1080/028134398750003133. [DOI] [PubMed] [Google Scholar]
- 31.Vaughn TE, McCoy K, BootsMiller BJ, et al. Organizational predictors of adherence to ambulatory care screening guidelines. Med Care. 2002;40:1172–85. doi: 10.1097/00005650-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Branch LG, Rabiner DJ, Patterson P, Sullivan RJ. Prevention services received by veterans visiting VHA facilities. Prev Med. 1998;27:604–10. doi: 10.1006/pmed.1998.0333. [DOI] [PubMed] [Google Scholar]
- 33.Rabiner DJ, Branch LG, Sullivan RJ. The receipt of prevention services by veterans using VA versus non-VA facilities. Prev Med. 1998;27:690–6. doi: 10.1006/pmed.1998.0345. [DOI] [PubMed] [Google Scholar]
- 34.Branch LG, Rabiner DJ. Rediscovering the patient's role in receiving health promotion services. Med Care. 2000;38:70–7. doi: 10.1097/00005650-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Med Care. 2002;40:129–36. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 36.American Hospital Association. American Hospital Association Annual Survey Database: Fiscal Year 1999 Documentation. Chicago, Ill: American Hospital Association; 2001. [Google Scholar]
- 37.Harrell FE, Lee KL, Califf RM, Pryor DB, Rosati RA. Regression modeling strategies for improved prognostic prediction. Stat Med. 1984;3:143–52. doi: 10.1002/sim.4780030207. [DOI] [PubMed] [Google Scholar]
- 38.Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–11. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 40.Kaplan SH, Greenfield S, Gandek B, Rogers WH, Ware JE., Jr Characteristics of physicians with participatory decision-making styles. Ann Intern Med. 1996;124:497–504. doi: 10.7326/0003-4819-124-5-199603010-00007. [DOI] [PubMed] [Google Scholar]
- 41.Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 42.Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47:213–20. [PubMed] [Google Scholar]
- 43.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–51. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 44.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48:51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 45.Mead N, Bower P, Hann M. The impact of practitioners’ patient-centredness on patients’ post-consultation satisfaction and enablement. Soc Sci Med. 2002;55:283–99. doi: 10.1016/s0277-9536(01)00171-x. [DOI] [PubMed] [Google Scholar]
- 46.Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001;50:1057–62. [PubMed] [Google Scholar]
- 47.Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J. Interventions for providers to promote a patient-centered approach in clinical consultations. Cochrane Database Syst Rev. 2001;4:CD003267. doi: 10.1002/14651858.CD003267. [DOI] [PubMed] [Google Scholar]
- 48.Kinnersley P, Stott N, Peters TJ, Harvey I. The patient-centredness of consultations and outcome in primary care. Br J Gen Pract. 1999;49:711–6. [PMC free article] [PubMed] [Google Scholar]
- 49.Kinmonth AL, Woodcock A, Griffin S, Spiegal N, Campbell MJ. Randomized control trial of patient centred care of diabetes in general practice: impact on current well being and future disease risk. The Diabetes Care from Diagnosis Research Team. BMJ. 1998;317:1202–8. doi: 10.1136/bmj.317.7167.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pill R, Stott NC, Rollnick SR, Rees M. A randomized controlled trial of an intervention designed to improve the care given in general pratice to type II diabetic patients: patient outcomes and professional ability to change behaviour. Fam Pract. 1998;15:229–35. doi: 10.1093/fampra/15.3.229. [DOI] [PubMed] [Google Scholar]
- 51.Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. 2002;37:1509–29. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blustein J, Weiss LJ. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of healthcare by older Americans. Am J Public Health. 1996;86:1742–7. doi: 10.2105/ajph.86.12.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ettner SL. The relationship between continuity of care and health behaviors of patients. Does having a usual physician make a difference? Med Care. 1999;37:547–55. doi: 10.1097/00005650-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 54.Lambrew J, DeFriese G, Carey T, Ricketts T, Biddle A. The effects of having a regular doctor on access to primary care. Med Care. 1996;34:138–51. doi: 10.1097/00005650-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 55.Berry LL, Seiders K, Wilder SS. Innovations in access to care: a patient-centered approach. Ann Intern Med. 2003;139:568–74. doi: 10.7326/0003-4819-139-7-200310070-00009. [DOI] [PubMed] [Google Scholar]
- 56.MacDonald R, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med. 1999;16:173–7. doi: 10.1016/s0749-3797(98)00159-7. [DOI] [PubMed] [Google Scholar]
- 57.Ward MM, Doebbeling BN, Vaughn TE, et al. Effectiveness of a nationally implemented smoking cessation guideline on provider and patient practices. Prev Med. 2003;36:265–71. doi: 10.1016/s0091-7435(02)00046-4. [DOI] [PubMed] [Google Scholar]