Abstract
OBJECTIVE
To examine changes in the quality of primary care experienced and reported by Medicare beneficiaries from 1998 to 2000.
DESIGN
Longitudinal observational study.
SETTING
Thirteen states with large, mature Medicare HMO markets.
PARTICIPANTS
Probability sample of noninstitutionalized Medicare beneficiaries aged 65 and older enrolled in traditional Medicare (FFS) or a Medicare HMO.
MEASUREMENTS AND MAIN RESULTS
We examined 2-year changes in 9 measures derived from the Primary Care Assessment Survey (PCAS). The measures covered 2 broad areas of primary care performance: quality of physician-patient interactions (5 measures) and structural/organizational features of care (4 measures). For each measure, we computed the change in each beneficiary's score (1998 vs 2000) and standardized effect sizes (ES). Results revealed significant declines in 3 measures of physician-patient interaction quality (communication, interpersonal treatment, and thoroughness of physical exams; P≤ .0001). Physicians’ knowledge of patients increased significantly over the 2-year period (P≤ .001). Patient trust did not change (P = .10). With regard to structural/organizational features of care, there were significant declines in financial access (P ≤ .001), visit-based continuity (P < .001), and integration of care (P≤ .05), while organizational access increased (P ≤ .05). With the exception of financial access, observed changes did not differ by system (FFS, HMO).
CONCLUSIONS
Over a 2-year period, the quality of seniors’ interactions with their primary physicians declined significantly, as did other hallmarks of primary care such as continuity, integration of care, and financial access. This decline is in sharp contrast to the marked improvements in technical quality that have been measured over this period. In an era marked by substantial national investment in quality monitoring, measures of these elements of care are notably absent from the nation's portfolio of quality indicators.
Keywords: primary care quality, doctor-patient relationships, access to care, quality assessment, Medicare
Almost 30 years ago, the concept of primary care was introduced and characterized as having 5 essential and defining elements: accessibility, comprehensiveness, coordination, continuity, and accountability.1 In 1996, the Institute of Medicine (IOM) proposed a revised definition expanding upon previous definitions1–4 and enunciating the importance of “sustained clinician-patient partnerships” and a whole-person orientation to care.5
There continues to be widespread agreement that increased emphasis on primary care is desirable for the U.S. health care system, and a recent IOM report on our nation's most important quality gaps underscores the importance of achieving systems that are patient centered.6 Yet there are few metrics by which to gauge our progress toward these ends. The majority of U.S. adults report having a source of primary care, and primary care relationships are generally sustained over a period of many years.7–10 However, there is evidence that performance on the other defining characteristics of primary care leaves substantial room for improvement,5,8,11–13 and some evidence suggests that we are losing ground.14 A recent study in a population of employed adults showed significant declines in the quality of physician-patient interactions over a 3-year period (1996 to 1999).14 The primary care experiences of older adults during this time period have not been evaluated. For older people, many of the defining attributes of primary care assume heightened importance given the prevalence of multiple chronic medical conditions.15
We examined changes in the primary care experiences of older adults from 1998 to 2000 using data from a longitudinal study of Medicare beneficiaries in 13 states. Each year, participants completed the Primary Care Assessment Survey (PCAS), a brief, validated questionnaire that measures the defining attributes of primary care named by the IOM and others.16 Using these data, we evaluated 2-year changes in 9 measures covering 2 broad areas of primary care: the quality of physician-patient interactions (communication quality, interpersonal treatment, whole-person care orientation, thoroughness of physical exams, and patient trust), and structural/organizational features of care (financial access, organizational access, visit-based continuity, and integration).
METHODS
The Study of Choice and Quality in Senior Health Care is a longitudinal observational study of noninstitutionalized Medicare beneficiaries aged 65 and older in 13 states (Arizona, California, Colorado, Florida, Illinois, Massachusetts, Minnesota, New Mexico, New York, Oregon, Pennsylvania, Texas, Washington). A principal objective of the study was to compare the primary care provided to seniors under the traditional Medicare (FFS) and Medicare HMO systems. These 13 states have the largest, most mature Medicare HMO systems and encompass approximately 80% of Medicare HMO enrollees nationwide.17 Details of the study design and methods are documented elsewhere11 and will be summarized here.
Study Design and Sampling
Sampling for the study occurred in three stages.11 First, states were selected; then HMOs within states; then beneficiaries from qualifying HMOs and from traditional Medicare. Because the study's primary goal was to evaluate Medicare HMOs in their mature—not nascent—stages, we excluded states as well as plans within states where managed Medicare was newly emerging.
We included all states that had at least 5% managed Medicare enrollment as of 1994 or earlier, with at least one market containing two or more mature Medicare HMOs (N = 13). Inclusion criteria for Medicare HMOs within qualifying states were: a risk contract with the Centers for Medicare and Medicaid Services (CMS), substantial enrollment (≥2,500) since 1994 or earlier, and at least 3,000 enrollees at the time of sampling (fall 1998). All Medicare HMOs meeting these criteria (N = 121) were included. Finally, beneficiaries had to be 65 or older, enrolled in Medicare Part B, reside in an eligible state, and be continuously enrolled for at least a year prior to sampling in either traditional Medicare or one of the qualifying Medicare HMOs. In addition, because data were collected principally by self-administered questionnaires, we excluded beneficiaries meeting any of the following criteria as indicated on the CMS data file: 1) primary language not English, 2) residence in a skilled nursing facility, or 3) representative payee listed, which indicates that the individual does not manage his/her own affairs.
Data Collection
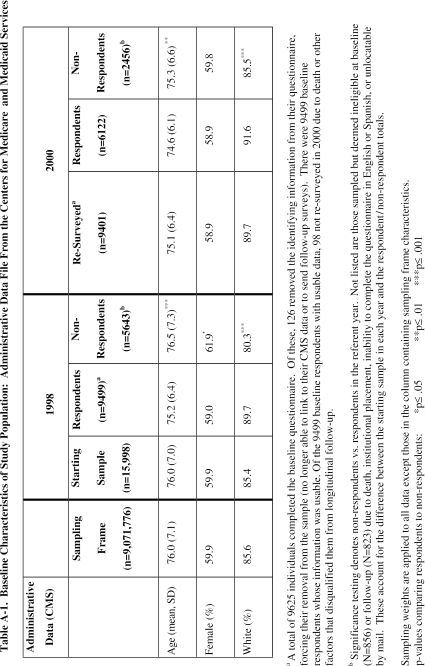
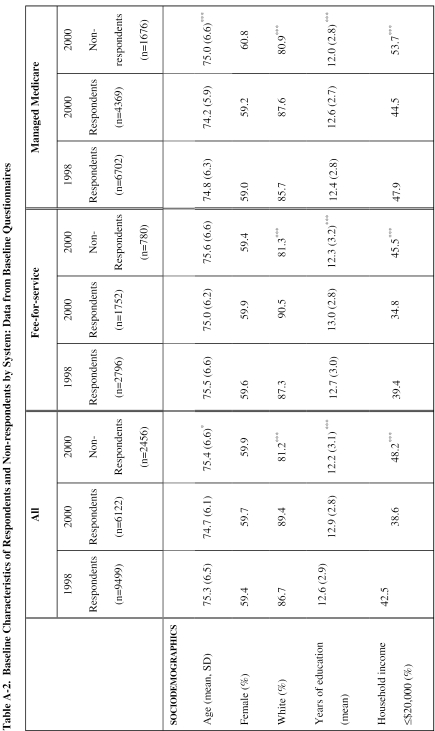
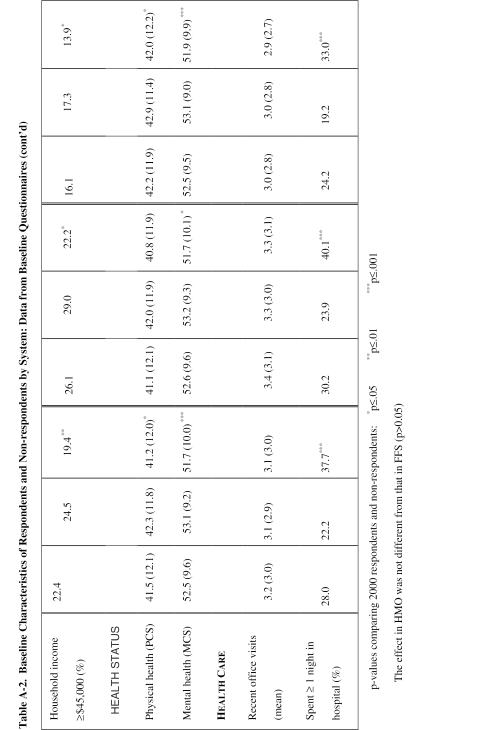
Baseline data were obtained between October 1998 and March 1999 using a standard 5-stage survey protocol involving mail and telephone.18 The protocol included an advance letter signed by the CMS administrator, initial survey mailing, reminder postcard, second survey mailing, and telephone follow-up. An abbreviated (short-form) survey was administered in telephone interviews. The short-form survey was also mailed to nonrespondents for whom no telephone number was available. This protocol yielded 9,625 responses for a 64% baseline response rate after deceased beneficiaries and bad addresses were removed (9,625/15,144). Administrative data from CMS revealed that nonrespondents were older and included more nonwhites and women than respondents (see online Appendix at http://www.jgim.org, Table A.1). Similarly, delayed responders (i.e., short-form mail and telephone)—whose characteristics are presumed to approximate those of nonresponders—were more likely to be nonwhite and to have less education and income than early responders (see online Appendix, Table A.2).
Follow-up occurred 24 months after baseline and employed the same mode of data collection. Baseline long-form respondents who did not respond to follow-up were either sent the short-form survey or contacted by telephone. This protocol resulted in 6,127 responses, yielding a response rate of 71% after correcting for exclusions (deaths, n = 405; severe illness, n = 41; unlocatable by mail, n = 360; nursing home, n = 3).
The questionnaire covered primary care quality, health care coverage and spending, medication regimen, health status, health care utilization, and sociodemographic characteristics. All modules were derived from instruments that had been extensively tested and validated.16,19–24 The primary care module included the PCAS, a validated questionnaire that measures 7 defining characteristics of primary care named by the IOM and others: accessibility, continuity, integration, comprehensiveness, whole-person orientation, clinical management, and sustained clinician-patient partnership.1–5,25 These analyses examine change over a 2-year period in patients’ experiences summarized by 9 PCAS measures amenable to this form of longitudinal analysis. The PCAS does not assess technical aspects of clinical quality because of known limitations of patient-provided information about this domain.26–29 Further detail about the development and validation of the PCAS is available elsewhere.8,16,30
Statistical Analyses
These analyses use the longitudinal study sample (n = 6,127), excluding respondents who reported not having a primary care physician at baseline (n = 653), respondents who reported changing physicians during the study period (n = 1,471), and respondents for whom we had incomplete data (n = 144). The resulting analytic sample (n = 4,173) is thus limited to respondents who retained the same primary care physician over the 2-year study period, which avoids confounding any observed changes in PCAS scores with changes in physician.
For each respondent, we calculated a change score for each of 9 PCAS scales (quality of communication, interpersonal treatment, physician's knowledge of the patient, thoroughness of the physical examinations, patient trust, financial access, organizational access, visit-based continuity, and integration of care). The short-form version of each scale was used so that both long- and short-form respondents could be included. The change score was defined as the 2000 score minus the 1998 score (i.e., a negative score indicates decline over the study period, a positive score indicates improvement). We determined the unadjusted mean change in each scale and calculated the 95% confidence interval around this change. To provide a meaningful comparison across scales, we computed the standardized effect size (ES), defined as the mean change observed for each scale divided by the standard deviation of the scale.
To better understand specific changes in the scales, item-level analyses were conducted for each scale. Report-based items corresponding to ratings in financial access, along with an item reporting the amount of time the physician spends with the patient, were used to aid in quantifying the observed results.
To test the sensitivity of the observed changes in primary care to geographic location, system (FFS vs HMO), individual health plans, and changes in patients’ health status, we estimated regression and analysis of variance models controlling for age, gender, income, race (white vs other), education, state, system, plan identifier, number of chronic conditions reported at baseline (from a checklist of 20 conditions with high prevalence among U.S. adults), physical and mental functioning of the patient averaged over the study period, change in physical and mental functioning over the study period, and a binary indicator of chronic conditions acquired (1998 to 2000). Physical and mental functioning were measured using the 12-Item Short-Form Health Survey (SF-12).31 We examined predicted changes in scores assuming no changes in health with all other variables set to their means.
Probability sampling weights, defined as the inverse of the sampling probability, were applied to all analyses to correct for matching done during sampling. The statistical software used (Stata 7.0 SE, Stata Corporation, College Station, Tex) takes these weights into account when computing standard errors.
RESULTS
The baseline sociodemographic and health characteristics of the analytic sample are presented in Table 1. Study participants ranged in age from 66 to 100, with a mean of 74.8 years. The majority of the sample was female, white, and had at least a high school education. Over 80% of the sample had been with their primary care physician for more than 3 years. Physical and mental functioning scores were consistent with national norms for this age group.32
Table 1.
Baseline Demographic and Health Characteristics of Analytic Sample*
| Characteristic | Analytic Sample (N = 4,173) |
|---|---|
| Mean age, y (SD) | 74.8 (5.8) |
| Female, % | 59.9 |
| White, % | 91.7 |
| Household income, % | |
| <$20 K | 37.7 |
| >$20 K | 62.3 |
| Educational attainment, % | |
| Less than high school | 17.9 |
| Completed high school and/or college | 82.1 |
| Baseline length of relationship with PCP, % | |
| <3 years | 18.8 |
| ≥3 years | 81.2 |
| Health insurance, % | |
| FFS | 67.1 |
| Open-model HMO† | 20.4 |
| Closed-model HMO† | 12.5 |
| Mean number of chronic conditions‡ (SD) | 1.9 (1.4) |
| Mean physical health summary§ (SD) | 42.4 (11.4) |
| Mean mental health summary§ (SD) | 53.3 (8.8) |
Sampling weights are applied to all results to correct for differences in sampling probabilities across strata.
Open model includes IPA/network-model HMOs. Closed model includes Staff and Group Model HMOs.
From a list of 20 of the chronic conditions: hypertension, myocardial infarction, congestive heart failure, diabetes, angina, cancer, migraines, seasonal allergies, nonseasonal allergies, arthritis, back pain, blindness, asthma/emphysema, liver disease, insomnia, heartburn/ulcers, deafness, limb paralysis or amputation, weight problems, and depression.
From the Short-form 36-item Health Survey.19
SD, standard deviation; PCP, primary care physician; FFS, traditional Medicare.
Average changes in each PCAS scale over the 2-year period are shown in Table 2. Significant declines were observed in 3 of the 5 measures of physician-patient interaction quality (communication, interpersonal treatment, thoroughness of physical examinations; P≤ .001), with standardized ES ranging from −0.12 to −0.19. There was no significant change in patient trust (P = .10), while physicians’ knowledge of the patients increased significantly (ES = 0.12; P≤ .001).
Table 2.
Changes in Primary Care Performance from 1998 to 2000, Unadjusted
| 1998 Average (N = 4,173) | 2000 Average (N = 4,173) | 2000 to 1998 Difference (95 % Confidence Interval) | Effect Size* | |
|---|---|---|---|---|
| Quality of physician-patient interaction | ||||
| Communication | 80.3 | 77.3 | −3.0 (−3.7 to −2.3) | −0.19‡ |
| Interpersonal treatment | 75.8 | 73.5 | −2.3 (−3.2 to −1.6) | −0.12‡ |
| Thoroughness of physical exam | 76.6 | 74.0 | −2.6 (−3.5 to −1.7) | −0.13‡ |
| Trust | 79.8 | 80.5 | 0.7 (−0.07 to 1.5) | 0.05 |
| MD knowledge of patient | 68.9 | 71.4 | 2.5 (1.6 to 3.3) | 0.12‡ |
| Structural/organizational features of care | ||||
| Financial access | 39.7 | 36.6 | −3.1 (−4.2 to −2.0) | −0.15‡ |
| Organizational access | 65.5 | 66.6 | 1.1 (0.2 to 2.0) | 0.06† |
| Visit-based continuity | 92.7 | 88.3 | −4.4 (−5.4 to −3.3) | −0.26‡ |
| Integration | 76.7 | 75.5 | −1.2 (−2.3 to −0.01) | −0.06† |
Effect size is computed as mean change in score from 1998 to 2000, divided by standard deviation of scale (1998).
P ≤ .05;
P ≤ .001.
Three of the four measures of structural and organizational features of care declined (Table 2). The largest change occurred in visit-based continuity, which declined 4.4 points between 1998 and 2000 (ES =−0.26; P≤ .001). Financial access and integration also declined, with effect sizes of −0.15 (P≤ .001) and −0.06 (P≤ .05), respectively. Organizational access increased 1.1 points over the 2-year period (ES = 0.06; P≤ .05).
Item-level results are shown in Table 3. In general, items comprising the 5 measures of physician-patient interaction quality showed change that was consistent in magnitude and direction with the overall scale change—suggesting that none of the items was dominating or opposing the observed result at the scale level. However, item-level results for measures of organizational/structural features of care were less internally consistent. For instance, while organizational access improved overall (ES = 0.06; P ≤ .05), item-level results reveal a decline in patients’ assessment of phone access (ES =−0.08; P≤ .01), and uneven improvement in the other 2 areas of access evaluated. Similarly, there was an uneven decline in the 2 components of the financial access scale—with a significant decline in patients’ assessments of their prescription drug costs (ES =−0.20; P≤ .001) and no significant change in their assessments of costs for office visits (P = .35). In 1998, 11% spent more than $100 a month on prescription drugs, while in 2000 this number rose to 17%. By comparison, the percentage of people spending more than $50 out of pocket on office visits increased only slightly from 3% to 4% over the same time period (results not shown).
Table 3.
Item-level Analysis for Primary Care Scales
| Actual Change | Effect Size | |
|---|---|---|
| Quality of physician-patient interaction | ||
| Communication | −3.0 | −0.19‡ |
| Thoroughness of doctor's questions about your symptoms and how you are feeling | −3.0 | −0.16‡ |
| Doctor's explanations of your health problems or treatments | −3.1 | −0.16‡ |
| How often do you leave your doctor's office with unanswered questions | −2.9 | −0.16‡ |
| Interpersonal treatment | −2.3 | −0.12‡ |
| Doctor's caring and concern for you | −2.5 | −0.12‡ |
| Amount of time doctor spends with you | −2.2 | −0.11‡ |
| Thoroughness of physical exam | −2.6 | −0.13‡ |
| Trust | 0.7 | 0.05 |
| I completely trust my doctor's judgments about my medical care | 0.5 | 0.03 |
| My doctor cares more about holding costs down than about doing what is needed for my health | 0.7 | 0.02 |
| If a mistake was made in my treatment, my doctor would try to hide it from me | 1.5 | 0.07* |
| All things considered, how much do you trust your doctor | −0.9 | −0.06* |
| MD knowledge of patient | 2.5 | 0.12‡ |
| Doctor's knowledge of entire medical history | 1.6 | 0.08‡ |
| Doctor's knowledge about what worries you the most about your health | 3.1 | 0.13‡ |
| Doctor's knowledge about you as a person (your values and beliefs) | 3.4 | 0.13‡ |
| Structural/organizational features of care | ||
| Financial access | −3.1 | −0.15‡ |
| Amount of money you pay for doctor's visits | −0.3 | −0.01 |
| Amount of money you pay for medication and other prescribed treatments | −4.9 | −0.20‡ |
| Organizational access | 1.1 | 0.06* |
| How quickly you can see doctor when you are sick and call for an appointment | 1.6 | 0.08† |
| How many minutes you wait to see the doctor once you arrive for your appointment | 3.3 | 0.16‡ |
| Ability to speak to your doctor by phone when you have a question/need medical advice | −1.9 | −0.08† |
| Visit-based continuity | ||
| See your regular doctor when you are sick | −4.4 | −0.26‡ |
| Integration | −1.2 | −0.06* |
| Help regular doctor gave you in understanding what specialists or other doctors said about you | −0.7 | −0.03 |
| Quality of specialists or other doctors that your regular doctor sent you to | −1.5 | −0.08* |
P ≤ .05;
P ≤ .01;
P ≤ .001.
We analyzed patients’ reports about the number of minutes their physician spends with them to interpret the patients’ ratings of the adequacy of time. While Table 3 reveals a significant decline in patients’ assessments of the adequacy of the time their physician spends with them in a visit (ES =−0.11; P≤ .001), a nonparametric test for trends showed no change in patients’ report of the number of minutes their doctor spends (P = .91).
Results were insensitive to controls for health status or changes in health status. And with the exception of the “financial access” scale, analysis of variance results revealed no significant effects of system or individual health plans. For financial access, significant system and plan effects were observed for both scale and item-level analyses. Compared with FFS enrollees, HMO enrollees showed larger declines in financial access (ESFFS=−0.08; ESHMO=−0.32; P≤ .001), though variation among individual Medicare HMOs appeared larger than FFS-HMO differences. F-statistics testing for state effects, while significant in some cases, did not show results that would change the overall picture (e.g., communication declined in all 13 states, but at slightly different rates).
DISCUSSION
The results of the study show significant decrements in older adults’ primary care experiences between 1998 and 2000. The largest declines occurred in the quality of physician-patient interactions, and in seniors’ financial access and continuity of care. Item-level analyses further elucidated a growing distance between patients and their primary physicians. In 2000, seniors reported less thorough discussions about their problems and symptoms, greater difficulty reaching their doctor by phone for medical advice and in seeing their doctor when sick, and interpersonal treatment that felt less caring and more rushed. Yet the data revealed no significant change in the actual amount of time physicians and patients spent together during visits.
The study's results support and extend earlier findings in several important ways. The significant erosion in the quality of physician-patient interactions seen in this study is consistent with changes observed in a previous study of employed adults in Massachusetts (1996 to 1999).14 In this case, adults aged 65 and older enrolled in traditional Medicare and Medicare HMOs in 13 states nationwide were studied, suggesting that the observed effects are not confined to a narrow geographic area or single delivery system. Second, the magnitude of the observed declines in several features of primary care in the present study were equal to or larger than previously observed, despite the briefer follow-up period (2 vs 3 years). In particular, the magnitude of the declines seen in communication quality, interpersonal treatment, and thoroughness of physical exams suggests a sharper rate of change than seen previously.14 Third, the insensitivity of the results to models controlling for changes in patients’ health status suggests that the observed changes in health care manifest something beyond simply the effects of a population whose health care needs grew more complicated. Fourth, the observed changes in an elderly population are surprising in light of considerable empirical evidence suggesting that this generation of U.S. adults holds physicians in high esteem and is generally less critical of their health care than younger generations.33–37
The study design does not permit us to definitively identify the mechanisms through which the observed changes in primary care occurred. However, the data afford some important clues. First, the overall picture conveyed by the results suggests that during this period, health care organizations grew increasingly attentive to appointment access—seen as shorter waits for appointments and shorter office waits. However, in doing so, they may have traded off patients’ continuity with their primary physicians. The observed decline in visit-based continuity was the largest of all observed changes. It is possible that this reduced continuity between patients and their physicians contributed to the growing distance between patients and their primary physician over the study period.
In addition, there appears to be something changing with respect to the perceived adequacy of time. While the data clearly illuminate an experience in which patients felt more rushed, less cared about, and less thoroughly attended to by their physicians during medical visits, the actual amount of time spent together during medical visits did not change. The latter accords with several recent studies which document that visits are not growing shorter38,39 despite widespread perceptions by patients and physicians that they are. Our findings underscore this seeming paradox: why does a medical visit that has not changed in duration now seem to be too short and to feel rushed?
A number of factors could contribute to this. First, the past decade has seen a dramatic increase in “consumerism” in U.S. health care.40–42 There is a clear and growing message that individuals should be informed and knowledgeable about their health and health care, and this is supported by an explosion of information directed to the public—from direct-to-consumer advertising to the ever-expanding volume of information on the Internet. Many older adults now arrive at medical visits with more information in-hand and more issues to discuss. However, the physician may approach the visit with a separate and potentially conflicting agenda which now includes the need to attend to and document specific care processes that are being measured and reported as indicators of health care quality (e.g., preventive screening procedures and chronic disease management activities). Thus, it is possible that the same amount of time no longer feels like enough. And conflicting notions about what needs to get accomplished during the visit may leave patients feeling that they were not listened to as thoroughly or given the same level of attention.
Whatever the root cause, the magnitude of the observed decline in the interpersonal quality of care experienced and reported by older adults merits attention. Considerable empirical evidence underscores the high value that patients place on the interpersonal aspects of care, including continuity with their doctor, and demonstrates the important role these factors play in determining outcomes of care—including patients’ adherence to medical advice,43–47 improved clinical outcomes,48–51 loyalty to a physician's practice,52 and reduced malpractice litigation.53–55
Finally, the more severe decline in financial access seen among HMO enrollees compared with their FFS counterparts, is consistent with documented changes in Medicare HMO cost-sharing policies and coverage that began in 1999 and accelerated in the next few years.56–58 While increased cost-sharing also occurred in the supplemental insurance policies of many FFS enrollees,59,60 these changes appear to have been somewhat less severe. The newly enacted Medicare Prescription Drug Improvement & Modernization Act will almost certainly change these prescription spending trajectories—though the extent and direction of the changes is highly uncertain. It is likely, however, that for HMO enrollees, the new law will either abate or reverse the trend toward rapidly rising medication costs in the near-term. Under the new law, Medicare HMOs will receive $1.3 billion in additional funds in 2004–2005, and are required to use the funds to advantage their enrollees (e.g., enhance benefits, decrease copayments). If HMOs focus the additional funds in ways that enhance prescription coverage and reduce cost-sharing, Medicare HMOs may resume the position they held in the 1990s, when their prescription benefits represented a clear advantage over traditional Medicare and helped fuel substantial HMO enrollment growth.
There are several relevant study limitations. First, our study was restricted to states, or regions within the selected states, where Medicare HMO penetration was high. Although 80% of Medicare HMO enrollees nationwide reside in these 13 states, only 28% of traditional (FFS) Medicare beneficiaries reside there. We do not know whether our findings generalize to states lacking a substantial Medicare HMO presence. It is possible that the primary care performance and changes in performance in traditional Medicare (FFS) are different when Medicare HMOs are absent from the market.
Second, the study population underrepresents vulnerable subgroups of seniors due to higher rates of nonresponse and loss to follow-up associated with older age, minority race/ethnicity, low income, low education, and poorer health status. Given widespread evidence of poorer health care quality provided to vulnerable subgroups,61 the observed findings may overstate the quality of primary care generally and may underestimate the decline in care experienced by the subgroups underrepresented here.
Third, the study's measures cover a brief 2-year period. We do not know whether and how seniors’ health care experiences were changing in the years leading up to this study or after it. The magnitude of the observed changes in this brief period and the fact that similar patterns were observed in a separate study of a younger adult population suggest the importance of continuing to monitor these aspects of health care.
Finally, the study did not include indicators of change in the technical quality of care. However, recent evidence suggests that performance on technical aspects of care improved during the study period. For example, Jencks et al. found that performance on a set of 22 indicators of technical quality of care monitored in the traditional (FFS) Medicare program improved nationwide since 1998, when monitoring began.62 Similarly, data from the National Committee on Quality Assurance (NCQA) show improvements in technical quality indicators, including the use of beta blockers following a myocardial infarction, diabetic eye exams, and adolescent immunizations since routine monitoring of these began.63,64 A study including robust measures of both technical and interpersonal quality is critical to clarify whether these are moving in opposite directions, and if so, to understand why.
In conclusion, while public and private sector goals for advancing health care quality underscore the importance of strengthening primary care, and while there is widespread agreement that we must move toward a more “patient-centered” system, data from the present study suggest that we are moving in the wrong direction. Over a 2-year period, the quality of seniors’ interactions with their primary physicians declined significantly, as did other hallmarks of primary care such as continuity, integration of care, and financial accessibility. The marked decline in these aspects of care contrasts sharply with evidence from other studies that the technical quality of care is improving in the United States.62–64 The improvements in technical health care quality, seemingly spurred by the routine monitoring and reporting of performance on these measures, lend credence to the aphorism that “what gets measured gets attended to.” In an era marked by substantial national investment in health care quality monitoring and reporting, measures of interpersonal health care quality are notably absent from the nation's portfolio of quality indicators. The results suggest that we cannot afford to continue to ignore this side of the quality scorecard.
Acknowledgments
This research was supported by grant number R01 HS09622 from the Agency for Healthcare Research and Quality and the National Institute on Aging. The authors gratefully acknowledge Renee Mentnech, Kim Elmo, and Russ Patterson at CMS, whose commitment to this research and facilitation of our data requests have made the study possible. The authors are also indebted to Michael Hagan, PhD (AHRQ), Carlos Zarabozo (CMS), and Joseph P. Newhouse, PhD (Harvard Medical School), who have been invaluable resources and offered keen insights throughout the project. We gratefully acknowledge Brian Clarridge, PhD (Center for Survey Research, University of Massachusetts) and Tim Nanneman, PhD (Roper Starch Worldwide), and their colleagues for their technical expertise and commitment to excellence in obtaining the data from Medicare enrollees.
Appendix
Appendix
REFERENCES
- 1.Institute of Medicine. Report of a Study: A Manpower Policy for Primary Health Care. Washington, DC: National Academy of Sciences; 1978. [Google Scholar]
- 2.Millis JS. The Millis Commission Report. Chicago, Ill: American Medical Association; 1966. [Google Scholar]
- 3.Starfield B. Primary Care: Concept, Evaluation and Policy. New York, NY: Oxford University Press; 1992. [Google Scholar]
- 4.Alpert J, Charney E. The Education of Physicians for Primary Care. Washington, DC: U.S. DHEW; 1973. [Google Scholar]
- 5.Institute of Medicine. Primary Care: America's Health in a New Era. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 6.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the Twenty-first Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 7.Agency for Health Care Policy and Research, Center for Cost and Financing Studies. Version AHCPR 98-DP02. Rockville, Md: AHCPR; 1998. 1987 NMES Household Survey and Health Insurance Plans Survey Data (CD-ROM) [Google Scholar]
- 8.Safran DG. The future of primary care: views from the patient. Ann Intern Med. 2003;138:248–55. doi: 10.7326/0003-4819-138-3-200302040-00033. [DOI] [PubMed] [Google Scholar]
- 9.Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996;86:1742–7. doi: 10.2105/ajph.86.12.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Medicare and Medicaid Services. Medicare Current Beneficiary Survey Data from Access to Care File. Medicare Current Beneficiary Survey 1999. Available at: http://cms.hhs.gov/MCBS/. Accessed February 13, 2004. [Google Scholar]
- 11.Safran DG, Wilson IB, Rogers WH, Montgomery JE, Chang H. Primary care quality in the Medicare program: comparing the performance of HMOs and traditional Medicare. Arch Intern Med. 2002;162:757–65. doi: 10.1001/archinte.162.7.757. [DOI] [PubMed] [Google Scholar]
- 12.Keating NL, Green DC, Kao AC, Gazmararian JA, Wu VY, Cleary PD. How are patients’ specific ambulatory care experiences related to trust, satisfaction, and considering changing physicians? J Gen Intern Med. 2002;17:29–39. doi: 10.1046/j.1525-1497.2002.10209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emanuel EJ, Dubler NN. Preserving the physician-patient relationship in the era of managed care. JAMA. 1995;273:323–9. [PubMed] [Google Scholar]
- 14.Murphy J, Chang H, Montgomery J, Rogers WH, Safran DG. The quality of physician-patient relationships: patients’ experiences 1996–1999. J Fam Pract. 2001;50:123–9. [PubMed] [Google Scholar]
- 15.Hoffman C, Rice D, Sung H-Y. Persons with chronic conditions: their prevalence and costs. JAMA. 1996;276:1473–9. [PubMed] [Google Scholar]
- 16.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Medicare Managed Care Contract Plans Monthly Summary Report. Washington, DC: CMS; 2002. Centers for Medicare and Medicaid Services. [Google Scholar]
- 18.Dillman DA. Mail and Telephone Surveys: The Total Design Method. New York, NY: John Wiley; 1978. [Google Scholar]
- 19.McHorney CA, Ware JEJ, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 20.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Shea S, Stein AD, Lantigua R, Basch CE. Reliability of the behavioral risk factor survey in a triethnic population. Am J Epidemiol. 1991;133:489–500. doi: 10.1093/oxfordjournals.aje.a115916. [DOI] [PubMed] [Google Scholar]
- 22.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 24.Adams PF, Morano MA. Vital Health Stat 10. Vol. 193. Hyattsville, Md: National Center for Health Statistics; 1995. Current Estimates from the National Health Interview Survey, 1994: Supplement on Aging; pp. 413–60. [PubMed] [Google Scholar]
- 25.Safran DG. Defining Primary CareA Background Paper Prepared for the Institute of Medicine Committee on the Future of Primary Care. Boston, Mass: New England Medical Center; 1994. [Google Scholar]
- 26.Davies AR, Ware JE, Brook RH, Peterson JR, Newhouse JP. Consumer acceptance of prepaid and fee-for-service medical care: results from a randomized controlled trial. Health Serv Res. 1986;21:429–52. [PMC free article] [PubMed] [Google Scholar]
- 27.Ware JE, Snyder MK, Wright WR. In: Development and Validation of Scales to Measure Patient Satisfaction with Health Care Services, I. Development and Validation of Scales to Measure Patient Satisfaction with Health Care Services. Springfield, VA: National Technical Service; 1976. Results regarding scales constructed from the patient satisfaction questionnaire and measure of other health perceptions. NTIS publication PB:288–330. [Google Scholar]
- 28.United States Congress Office of Technology Assessment. The Quality of Medical Care: Information for Consumers. U.S. Congress Report OTA-H-386. Washington, DC: U.S. Government Printing Office; 1988. pp. 231–43. [Google Scholar]
- 29.Sox HC, Margulies I, Sox CH. Psychologically mediated effects of diagnostic tests. Ann Intern Med. 1981;95:680–5. doi: 10.7326/0003-4819-95-6-680. [DOI] [PubMed] [Google Scholar]
- 30.Murray A, Safran DG. The Primary Care Assessment Survey: a tool for measuring, monitoring, and improving primary care. In: Maruish ME, editor. Handbook of Psychological Assessment in Primary Care Settings. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 2000. pp. 623–51. [Google Scholar]
- 31.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston, Mass: New England Medical Center; 1993. [Google Scholar]
- 33.Hargraves JL, Wilson IB, Zaslavsky A, et al. Adjusting for patient characteristics when analyzing reports from patients about hospital care. Med Care. 2001;39:635–41. doi: 10.1097/00005650-200106000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Zaslavsky AM, Zaborski LB, Ding L, Shaul JA, Cioffi MJ, Cleary PD. Adjusting performance measures to ensure equitable plan comparisons. Health Care Financ Rev. 2002;22:109–26. [PMC free article] [PubMed] [Google Scholar]
- 35.Pascoe GC. Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann. 1983;6:185–210. doi: 10.1016/0149-7189(83)90002-2. [DOI] [PubMed] [Google Scholar]
- 36.Smith R, Woodward N, Wallston B, Wallston K. Health care implications of desire and expectancy for control in elderly adults. J Gerontol. 1998;43:P1–P7. doi: 10.1093/geronj/43.1.p1. [DOI] [PubMed] [Google Scholar]
- 37.Haug M, Ory MG. Issues in elderly patient-provider interactions. Res Aging. 1987;3:3–44. doi: 10.1177/0164027587009001001. [DOI] [PubMed] [Google Scholar]
- 38.Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter? N Engl J Med. 2001;344:198–204. doi: 10.1056/NEJM200101183440307. [DOI] [PubMed] [Google Scholar]
- 39.Stafford RS, Saglam D, Causino N, et al. Trends in adult visits to primary care physicians in the United States. Arch Fam Med. 1999;8:26–32. doi: 10.1001/archfami.8.1.26. [DOI] [PubMed] [Google Scholar]
- 40.Counte M. The emerging role of the client in the delivery of primary care to older Americans. In: Ory MG, Cooper J, Siu A, editors. Special Supplement to Health Services Research. Vol. 32. Organizational Issues in the Delivery of Primary Care to Older Americans; 1998. pp. 402–23. [PMC free article] [PubMed] [Google Scholar]
- 41.Kizer KW. Establishing health care performance standards in an era of consumerism. JAMA. 2001;286:1213–7. doi: 10.1001/jama.286.10.1213. [DOI] [PubMed] [Google Scholar]
- 42.Robinson JC. The end of managed care. JAMA. 2001;285:2622–8. doi: 10.1001/jama.285.20.2622. [DOI] [PubMed] [Google Scholar]
- 43.DiMatteo MR. Enhancing patient adherence to medical recommendations. JAMA. 1994;271:79–83. doi: 10.1001/jama.271.1.79. [DOI] [PubMed] [Google Scholar]
- 44.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 45.Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication: patients’ response to medical advice. N Engl J Med. 1969;280:535–40. doi: 10.1056/NEJM196903062801004. [DOI] [PubMed] [Google Scholar]
- 46.Safran DG, Murray A, Chang H, Montgomery JE, Murphy J, Rogers WH. Linking doctor-patient relationship quality to outcomes. J Gen Intern Med. 2000;15(suppl):116. [Google Scholar]
- 47.Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47:213–20. [PubMed] [Google Scholar]
- 48.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102:520–8. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 49.Greenfield S, Kaplan SH, Ware JEJ, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 50.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 51.Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155:1877–84. [PubMed] [Google Scholar]
- 52.Safran DG, Montgomery JE, Chang H, Murphy J, Rogers WH. Switching doctors: predictors of voluntary disenrollment from a primary physician's practice. J Fam Pract. 2001;50:130–6. [PubMed] [Google Scholar]
- 53.Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553–9. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- 54.Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice: lessons from plaintiff depositions. Arch Intern Med. 1994;154:1365–70. [PubMed] [Google Scholar]
- 55.Hickson GB, Clayton EW, Entman SS, et al. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994;272:1583–7. [PubMed] [Google Scholar]
- 56.Health Care Financing Administration. Medicare Managed Care Compare. Health Care Financing Administration [cited October 15, 1998] Available at: http://www.medicare.gov/mphCompare/home.asp. Accessed February 13, 2004. [Google Scholar]
- 57.Health Care Financing Administration. Medicare+Choice: Changes for the Year 2000. Health Care Financing Administration. Available at: http://www.hcfa.gov/medicare/mgdcar1.htm. Accessed February 13, 2004. [Google Scholar]
- 58.Achman L, Gold M. Report No533Medicare+Choice: Beneficiaries Will Face Higher Cost-sharing in 2002. New York, NY: The Commonwealth Fund; 2002. [Google Scholar]
- 59.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: how well are states closing the gap? Health Aff (Millwood) 2002;21:W253–W268. doi: 10.1377/hlthaff.w2.253. [DOI] [PubMed] [Google Scholar]
- 60.Laschober MA, Kitchman M, Neuman P, Strabic AA. Trends in Medicare supplemental insurance and prescription drug coverage, 1996–1999. Health Affairs—Web Exclusive. 2002:W127–W138. doi: 10.1377/hlthaff.w2.127. 21(February 27) [DOI] [PubMed] [Google Scholar]
- 61.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 62.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998–1999 to 2000–2001. JAMA. 2003;289:305–12. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 63.National Committee for Quality Assurance. State of Managed Care Quality 2000. Washington, DC: NCQA; 2000. [Google Scholar]
- 64.National Committee for Quality Assurance. State of Managed Care Quality, 2001. Washington, DC: NCQA; 2001. [Google Scholar]