Abstract
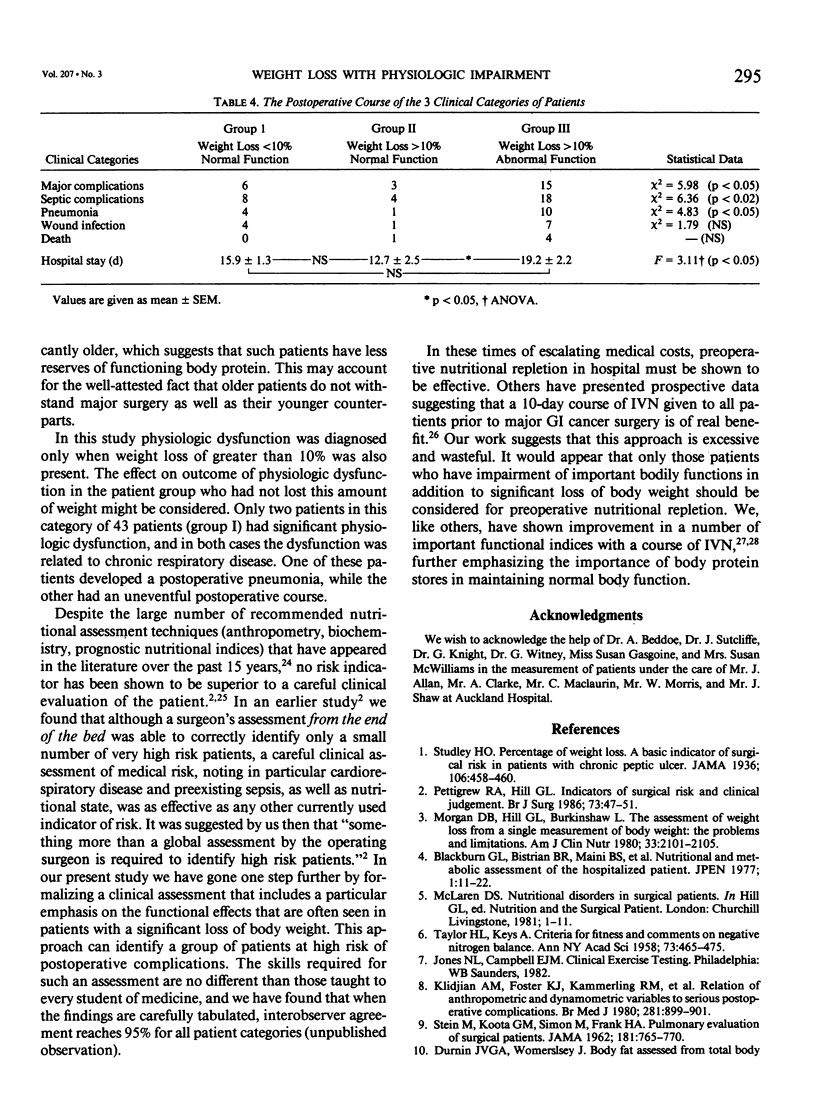
It is a long held belief that weight loss is a basic indicator of surgical risk. Many experienced surgeons, however, think otherwise. We have investigated the proposition that weight loss is a risk factor for postoperative complications but only when associated with clinically obvious physiologic impairment. Before major surgery, 102 patients had a careful history taken to ascertain if there had been recent weight loss and a reduction in the capacity for activity. Physical examination included assessment of mood, skeletal muscle function, respiratory muscle function, and wound healing. Plasma albumin was also measured. Using this information the patients were placed into one of three groups. Group I (N = 43) were normal, group II (N = 17) had weight loss greater than 10% but no clinical evidence of physiologic impairment, and group III (N = 42) had weight loss greater than 10% with clear evidence of dysfunction of two or more organ systems. The patients in group III had significantly more postoperative complications (p less than 0.05). They also had more septic complications (p less than 0.02) including a higher incidence of pneumonia (p less than 0.05) and a longer hospital stay (p less than 0.05) than patients in each of the other two groups. Objective measurements of body stores of protein and liver, and psychologic, respiratory, and skeletal muscle function, confirmed the validity of the clinical classification into the risk groups. The results demonstrate that weight loss is a basic indicator of surgical risk in modern practice providing it is associated with clinically obvious impairment of organ function. They suggest that adequate body protein stores are necessary for normal body function and for minimizing the risks of surgery.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arora N. S., Rochester D. F. Respiratory muscle strength and maximal voluntary ventilation in undernourished patients. Am Rev Respir Dis. 1982 Jul;126(1):5–8. doi: 10.1164/arrd.1982.126.1.5. [DOI] [PubMed] [Google Scholar]
- Beddoe A. H., Streat S. J., Hill G. L. Hydration of fat-free body in protein-depleted patients. Am J Physiol. 1985 Aug;249(2 Pt 1):E227–E233. doi: 10.1152/ajpendo.1985.249.2.E227. [DOI] [PubMed] [Google Scholar]
- Blackburn G. L., Bistrian B. R., Maini B. S., Schlamm H. T., Smith M. F. Nutritional and metabolic assessment of the hospitalized patient. JPEN J Parenter Enteral Nutr. 1977;1(1):11–22. doi: 10.1177/014860717700100101. [DOI] [PubMed] [Google Scholar]
- Church J. M., Choong S. Y., Hill G. L. Abnormalities of muscle metabolism and histology in malnourished patients awaiting surgery: effects of a course of intravenous nutrition. Br J Surg. 1984 Jul;71(7):563–569. doi: 10.1002/bjs.1800710732. [DOI] [PubMed] [Google Scholar]
- Edwards R. H., Young A., Hosking G. P., Jones D. A. Human skeletal muscle function: description of tests and normal values. Clin Sci Mol Med. 1977 Mar;52(3):283–290. doi: 10.1042/cs0520283. [DOI] [PubMed] [Google Scholar]
- Godfrey K. Statistics in practice. Comparing the means of several groups. N Engl J Med. 1985 Dec 5;313(23):1450–1456. doi: 10.1056/NEJM198512053132305. [DOI] [PubMed] [Google Scholar]
- Gregg I., Nunn A. J. Peak expiratory flow in normal subjects. Br Med J. 1973 Aug 4;3(5874):282–284. doi: 10.1136/bmj.3.5874.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydock D. A., Hill G. L. Improved wound healing response in surgical patients receiving intravenous nutrition. Br J Surg. 1987 Apr;74(4):320–323. doi: 10.1002/bjs.1800740432. [DOI] [PubMed] [Google Scholar]
- Heymsfield S. B., McManus C., Stevens V., Smith J. Muscle mass: reliable indicator of protein-energy malnutrition severity and outcome. Am J Clin Nutr. 1982 May;35(5 Suppl):1192–1199. doi: 10.1093/ajcn/35.5.1192. [DOI] [PubMed] [Google Scholar]
- Klidjian A. M., Foster K. J., Kammerling R. M., Cooper A., Karran S. J. Relation of anthropometric and dynamometric variables to serious postoperative complications. Br Med J. 1980 Oct 4;281(6245):899–901. doi: 10.1136/bmj.281.6245.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macklem P. T. Muscular weakness and respiratory function. N Engl J Med. 1986 Mar 20;314(12):775–776. doi: 10.1056/NEJM198603203141209. [DOI] [PubMed] [Google Scholar]
- Morgan D. B., Hill G. L., Burkinshaw L. The assessment of weight loss from a single measurement of body weight: the problems and limitations. Am J Clin Nutr. 1980 Oct;33(10):2101–2105. doi: 10.1093/ajcn/33.10.2101. [DOI] [PubMed] [Google Scholar]
- Morris J. F., Koski A., Johnson L. C. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971 Jan;103(1):57–67. doi: 10.1164/arrd.1971.103.1.57. [DOI] [PubMed] [Google Scholar]
- Müller J. M., Keller H. W., Brenner U., Walter M., Holzmüller W. Indications and effects of preoperative parenteral nutrition. World J Surg. 1986 Feb;10(1):53–63. doi: 10.1007/BF01656090. [DOI] [PubMed] [Google Scholar]
- Pettigrew R. A., Hill G. L. Indicators of surgical risk and clinical judgement. Br J Surg. 1986 Jan;73(1):47–51. doi: 10.1002/bjs.1800730121. [DOI] [PubMed] [Google Scholar]
- STEIN M., KOOTA G. M., SIMON M., FRANK H. A. Pulmonary evaluation of surgical patients. JAMA. 1962 Sep 1;181:765–770. doi: 10.1001/jama.1962.03050350027006. [DOI] [PubMed] [Google Scholar]
- TAYLOR H. L., KEYS A. Criteria for fitness and comments on negative nitrogen balance. Ann N Y Acad Sci. 1958 Sep 10;73(2):465–475. doi: 10.1111/j.1749-6632.1959.tb40819.x. [DOI] [PubMed] [Google Scholar]



