Abstract
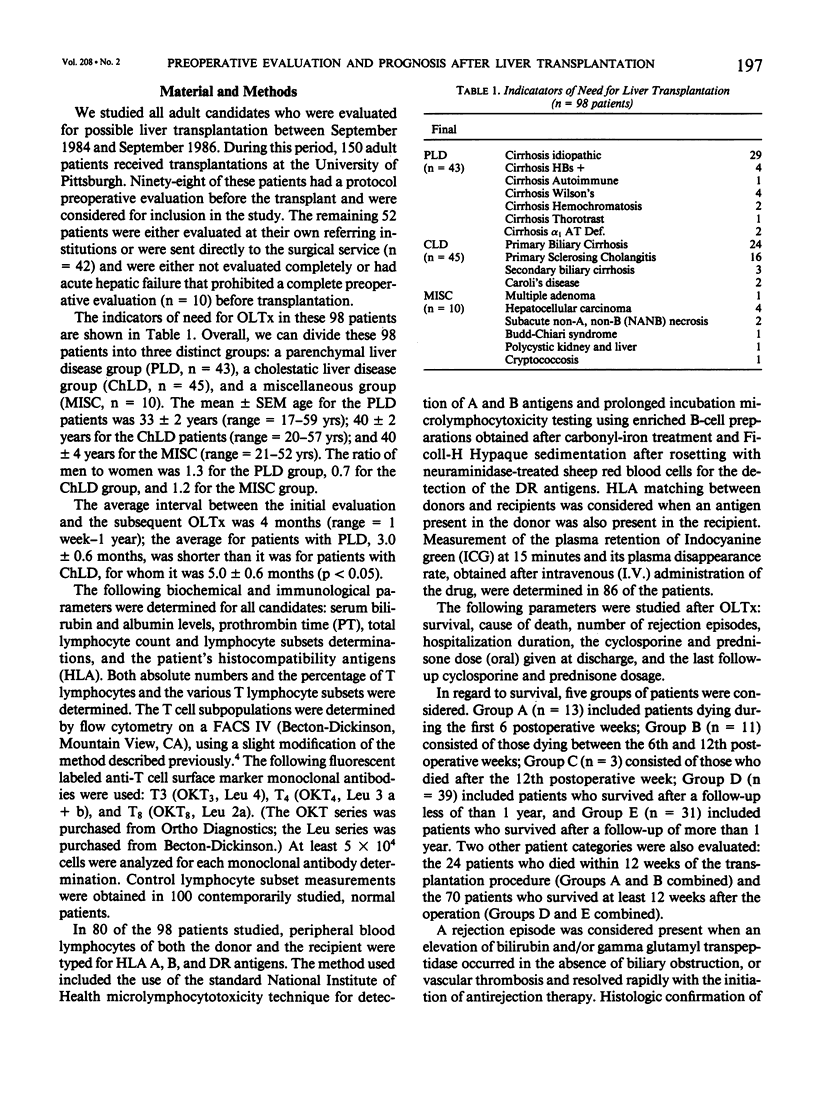
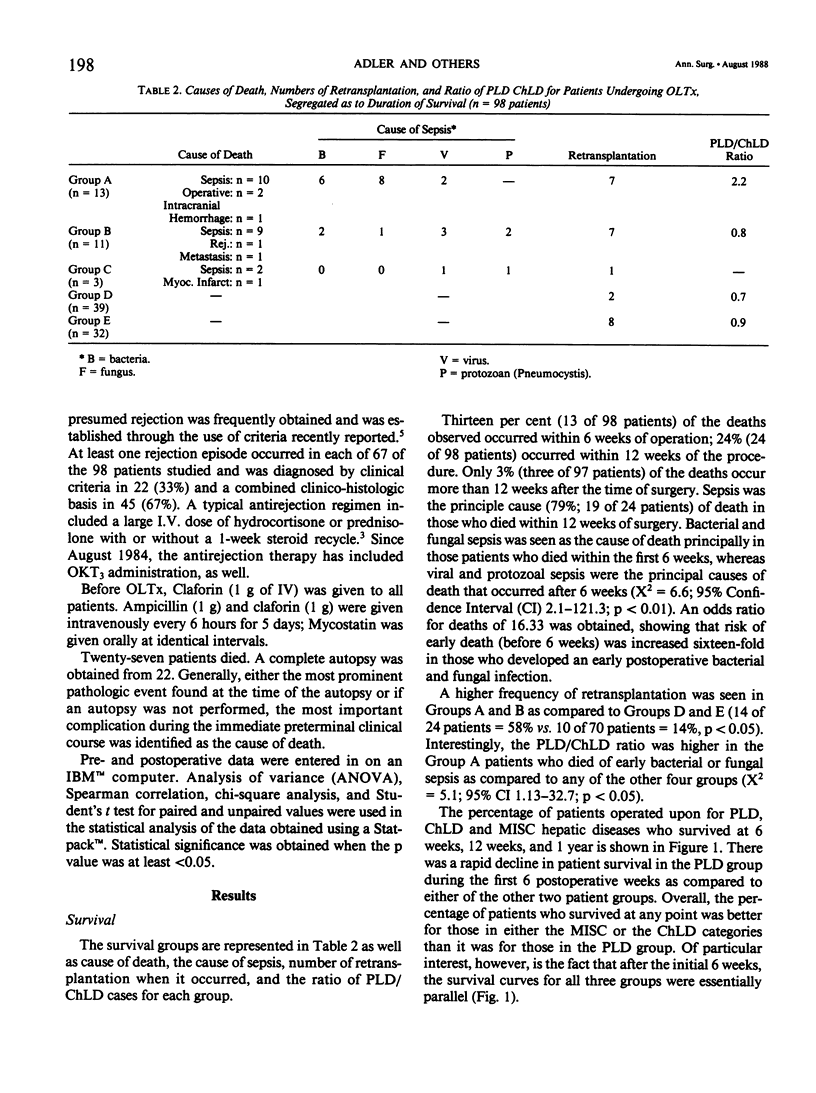
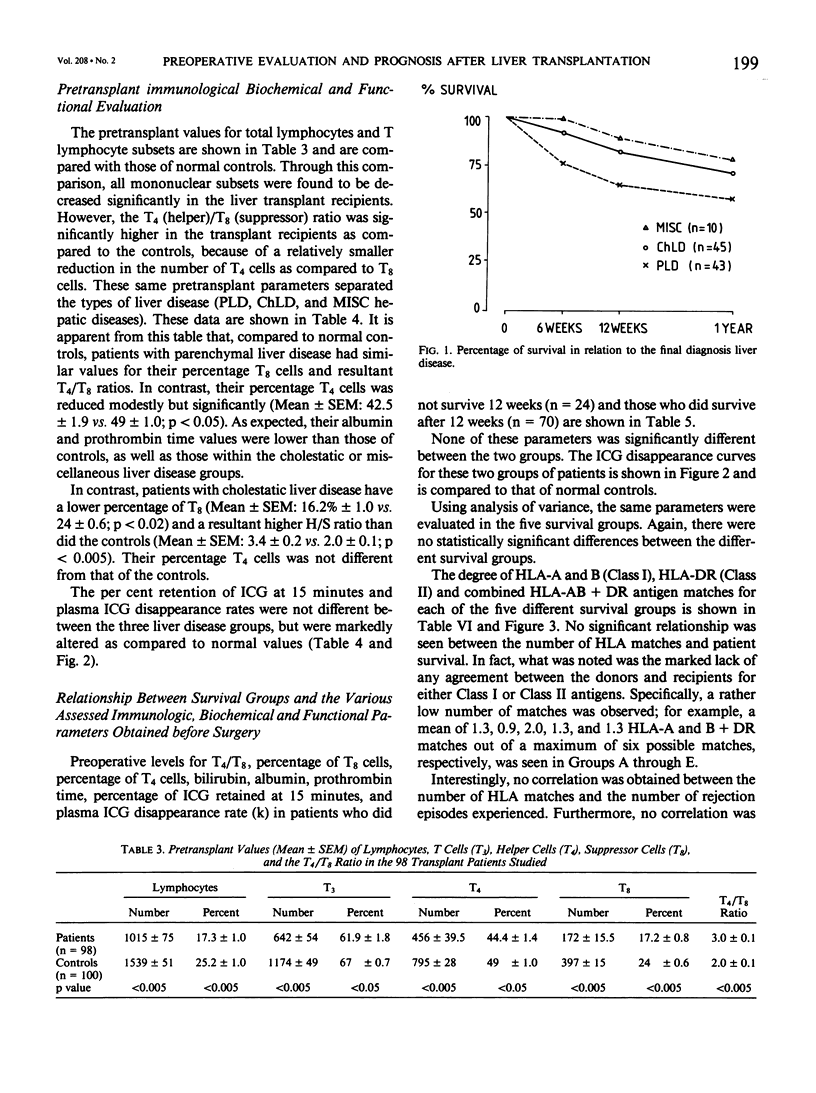
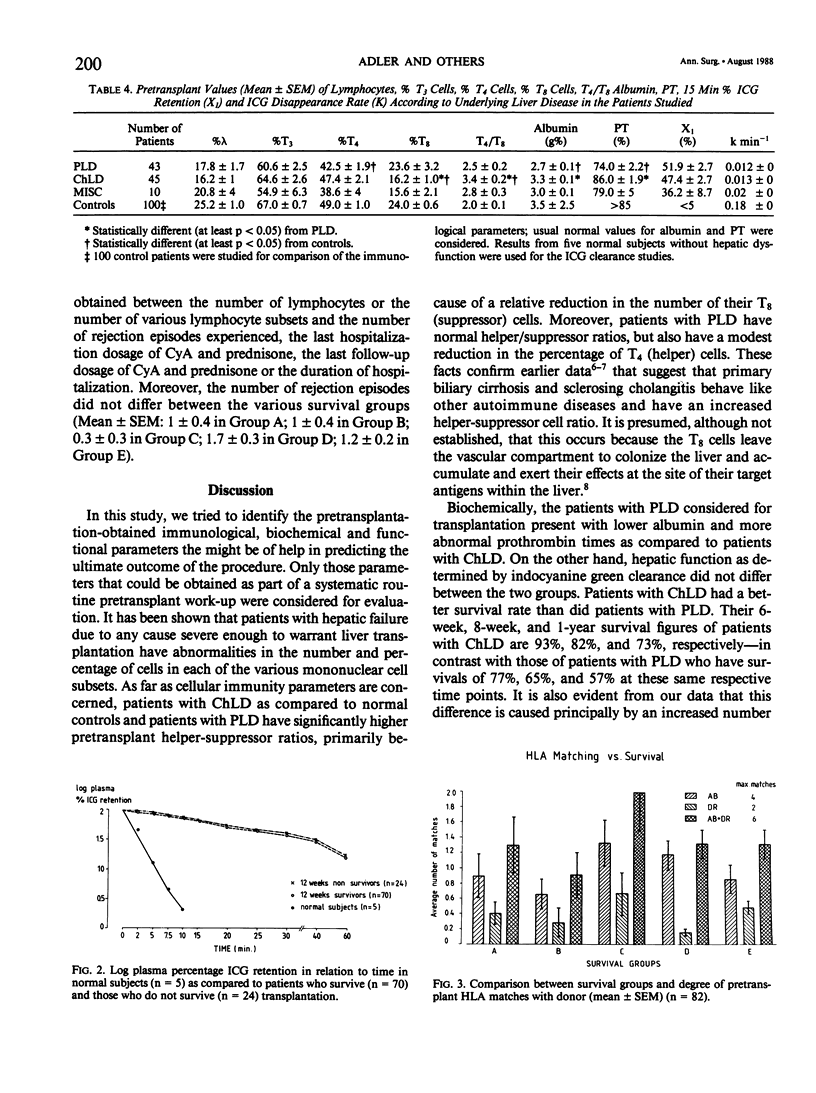
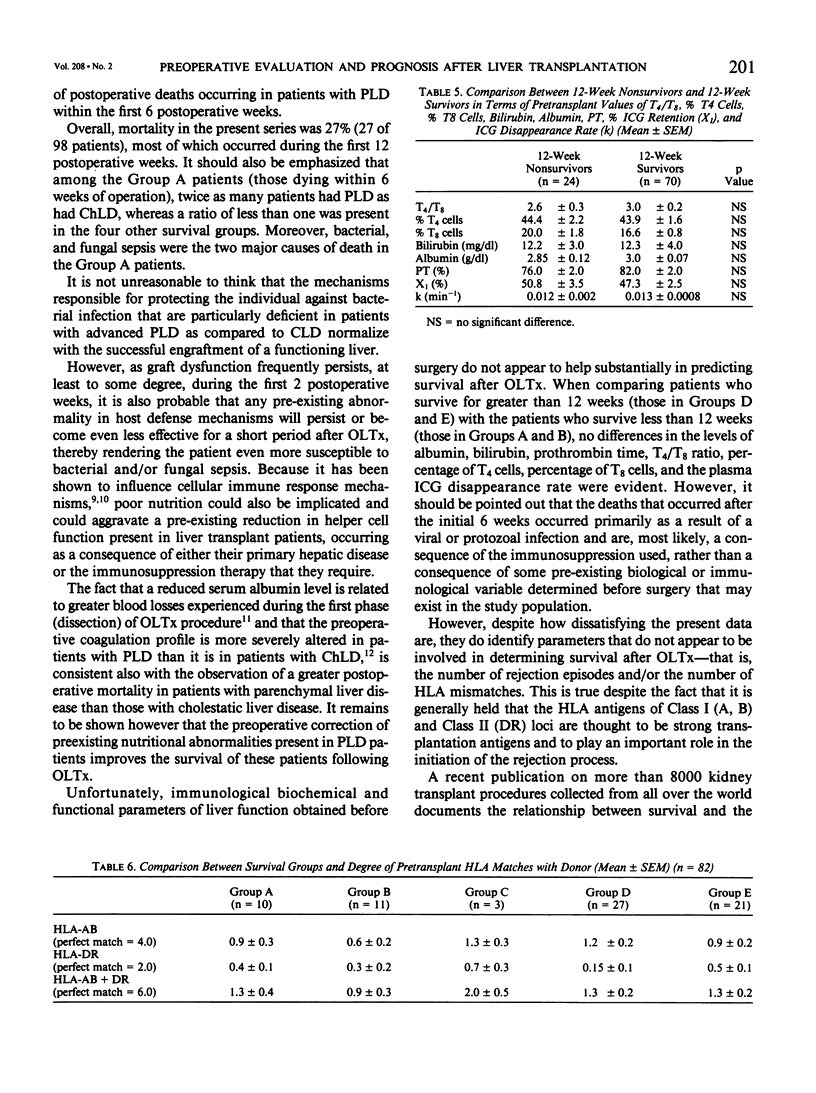
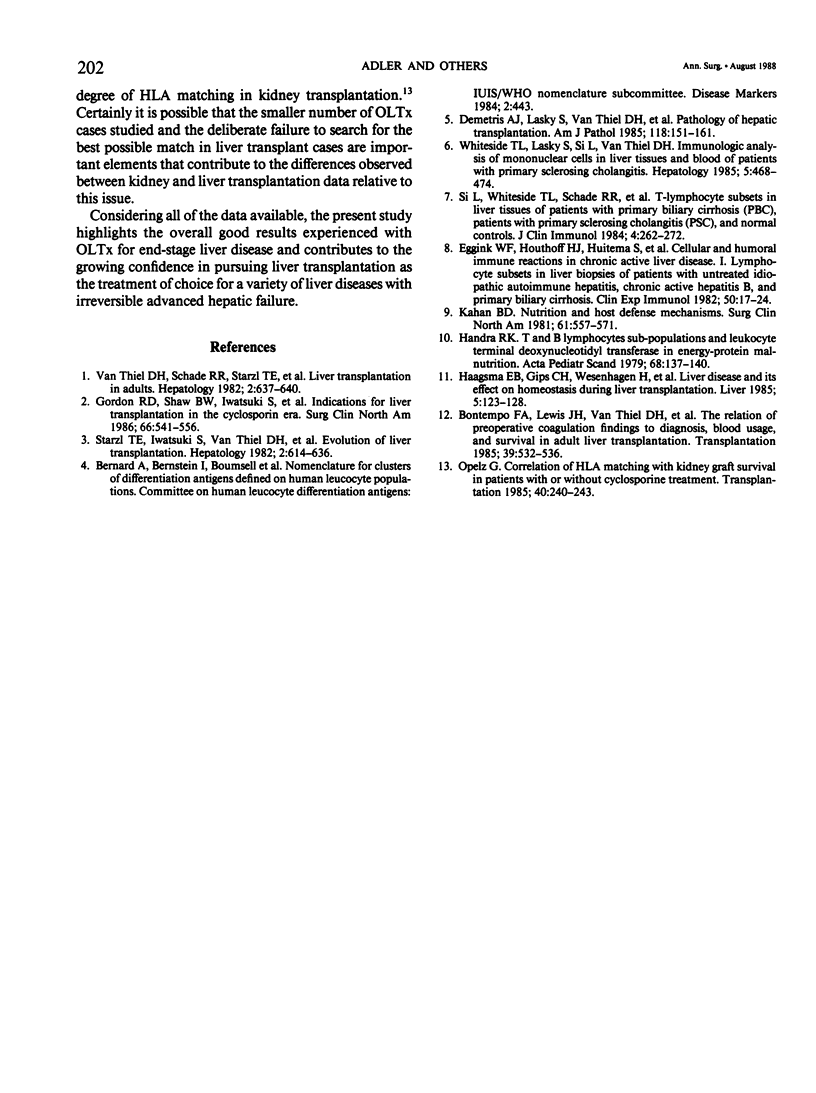
The purpose of this study was to identify which of the biochemical, immunological, or functional parameters derived before surgery as part of a systemic evaluation were helpful in predicting the frequency of rejection episodes, the chance of survival, and the cause risk of death (should death occur) of patients after orthotopic liver transplantation (OLTx). Ninety-eight adult patients who had an extensive preoperative protocol evaluation were studied before OLTx. The biochemical parameters assessed were albumin, prothrombin time, bilirubin, and ICG clearance. The immunologic parameters assessed included total lymphocytes, T3 cells, T4 cells, T8 cells, and the T4/T8 ratio. The degree of histocompatibility antigen (HLA) matching between the donor and the recipient was also evaluated in 80 of the 98 patients studied. Most postoperative deaths occurred within 12 weeks of the procedure (24%; 24 of 98 patients); 13 patients (13%) died within the first 6 postoperative weeks, of either bacterial or fungal sepsis. An additional 14 patients (14%) died after the initial 6 postoperative weeks due, primarily of an acquired viral and/or protozoan infection (p less than 0.01). During the first 6 weeks, survival was better for patients with cholestatic liver disease (ChLD, 93%, n = 45) and miscellaneous liver diseases (MISC, 100%, n = 10) than it was for those with parenchymal liver diseases (PLD, 77%, n = 43). Although albumin, prothrombin time, T4/T8 ratios, and per cent T8 cells were statistically different in patients with PLD as compared with those with ChLD, these parameters, as well as the per cent T4 cells, serum bilirubin level, per cent retention of ICG at 15 minutes, and the plasma ICG disappearance rate were not found to be of substantial help in predicting patient survival or non-survival. Moreover, neither the degree of HLA matching nor the number of rejection episodes differed between surviving and nonsurviving patients. The results of this study suggest that patients with PLD are at increased risk of early postoperative death after OLTx because of bacterial and/or fungal sepsis, as compared with patients operated upon for ChLD. Better pre-, intra-, and postoperative predictors of risk of death and complications are needed to reduce the early mortality observed after orthotopic liver transplantation.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bontempo F. A., Lewis J. H., Van Thiel D. H., Spero J. A., Ragni M. V., Butler P., Israel L., Starzl T. E. The relation of preoperative coagulation findings to diagnosis, blood usage, and survival in adult liver transplantation. Transplantation. 1985 May;39(5):532–536. doi: 10.1097/00007890-198505000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demetris A. J., Lasky S., Van Thiel D. H., Starzl T. E., Dekker A. Pathology of hepatic transplantation: A review of 62 adult allograft recipients immunosuppressed with a cyclosporine/steroid regimen. Am J Pathol. 1985 Jan;118(1):151–161. [PMC free article] [PubMed] [Google Scholar]
- Eggink H. F., Houthoff H. J., Huitema S., Gips C. H., Poppema S. Cellular and humoral immune reactions in chronic active liver disease. I. Lymphocyte subsets in liver biopsies of patients with untreated idiopathic autoimmune hepatitis, chronic active hepatitis B and primary biliary cirrhosis. Clin Exp Immunol. 1982 Oct;50(1):17–24. [PMC free article] [PubMed] [Google Scholar]
- Gordon R. D., Shaw B. W., Jr, Iwatsuki S., Esquivel C. O., Starzl T. E. Indications for liver transplantation in the cyclosporine era. Surg Clin North Am. 1986 Jun;66(3):541–556. doi: 10.1016/s0039-6109(16)43939-3. [DOI] [PubMed] [Google Scholar]
- Haagsma E. B., Gips C. H., Wesenhagen H., Van Imhoff G. W., Krom R. A. Liver disease and its effect on haemostasis during liver transplantation. Liver. 1985 Jun;5(3):123–128. doi: 10.1111/j.1600-0676.1985.tb00226.x. [DOI] [PubMed] [Google Scholar]
- Kahan B. D. Nutrition and host defense mechanisms. Surg Clin North Am. 1981 Jun;61(3):557–570. doi: 10.1016/s0039-6109(16)42437-0. [DOI] [PubMed] [Google Scholar]
- Opelz G. Correlation of HLA matching with kidney graft survival in patients with or without cyclosporine treatment. Transplantation. 1985 Sep;40(3):240–243. doi: 10.1097/00007890-198509000-00003. [DOI] [PubMed] [Google Scholar]
- Si L., Whiteside T. L., Schade R. R., Starzl T. E., Van Thiel D. H. T-lymphocyte subsets in liver tissues of patients with primary biliary cirrhosis (PBC), patients with primary sclerosing cholangitis (PSC), and normal controls. J Clin Immunol. 1984 Jul;4(4):262–272. doi: 10.1007/BF00915293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starzl T. E., Iwatsuki S., Van Thiel D. H., Gartner J. C., Zitelli B. J., Malatack J. J., Schade R. R., Shaw B. W., Jr, Hakala T. R., Rosenthal J. T. Evolution of liver transplantation. Hepatology. 1982 Sep-Oct;2(5):614–636. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Thiel D. H., Schade R. R., Starzl T. E., Iwatsuki S., Shaw B. W., Jr, Gavaler J. S., Dugas M. Liver transplantation in adults. Hepatology. 1982 Sep-Oct;2(5):637–640. doi: 10.1002/hep.1840020517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside T. L., Lasky S., Si L., Van Thiel D. H. Immunologic analysis of mononuclear cells in liver tissues and blood of patients with primary sclerosing cholangitis. Hepatology. 1985 May-Jun;5(3):468–474. doi: 10.1002/hep.1840050321. [DOI] [PubMed] [Google Scholar]


