Abstract
Background
This study assesses the behavioural and socio-economic factors associated with avoiding mosquitoes and preventing malaria in urban environments in Kenya.
Methods
Data from two cities in Kenya were gathered using a household survey and a two-stage cluster sample design. The cities were stratified based on planning and drainage observed across the urban areas. This helped control for the strong environmental and topographical variation that we assumed influences mosquito ecology. Individual interviews given to each household included questions on socio-economic status, education, housing type, water source, rubbish disposal, mosquito-prevention practices and knowledge of mosquitoes. In multivariate regression, factors measuring wealth, education level, and the communities' level of planning and drainage were used to estimate the probability that a household engages in multiple mosquito-avoidance activities, or has all members sleeping under a bed net.
Results
Our analysis shows that people from wealthier, more educated households were more likely to sleep under a net, in Kisumu (OR = 6.88; 95% CI = 2.56,18.49) and Malindi (OR = 3.80; 95% CI = 1.91,7.55). Similarly, the probability that households use several mosquito-prevention activities was highest among the wealthiest, best-educated households in Kisumu (OR = 5.15; 95% CI = 2.04,12.98), while in Malindi household wealth alone is the major determinant.
Conclusion
We demonstrate the importance of examining human-mosquito interaction in terms of how access to resources may enhance human activities. The findings illustrate that the poorest segments of society are already doing many things to protect themselves from being bitten, but they are doing less than their richer neighbours.
Background
Malaria remains an enormous public health problem in much of sub-Saharan Africa. In the past, malaria transmission was most notably associated with rural environments, as a result of the mosquito's affinity for clean, sunlit, temporary pools of water, which dominate rural landscapes in Africa [1,2]. There is however, evidence of urban malaria transmission [3,4]. Moreover, Robert et al. [5] identified market-garden wells as anopheline larval sites in Dakar, Senegal, and Trappe and Zoulani [6] found ditches, gutters and tyre tracks with anopheline larvae in Brazzaville. Urbanization is changing the context of human-mosquito interaction and subsequent disease transmission in Africa.
Typically, urbanization is defined as fundamental changes in occupation and land use at the community level [7,8]. However, in many peri-urban areas, populations are still actively engaged in rural-type activity. Although many individuals migrate to urban areas to increase educational and economic opportunities, rural lifestyles persist. Deteriorating infrastructure, poor access to, health and water and sanitation services, increasing population density, and widespread poverty contribute to conditions that modify the environment, which directly influences the risk of disease. These areas within and around urban areas are often considered "big villages" as a result of socio-economic, cultural, and physical conditions similar to contiguous rural areas. It is precisely this similarity that may contribute to human-mosquito contact and subsequent urban malaria transmission.
Despite evidence of the potential for rapid increases in urban malaria transmission [9-12], vector control programmes and mosquito-prevention programmes are still largely focused on rural areas [13]. To address the epidemiological consequences of human behaviour in urban and peri-urban areas, research must consider the scale at which human and mosquito populations are interacting. Such studies have important policy implications, since this information could assist policy makers and public health practitioners prevent epidemic urban malaria, and assist agencies in developing important information for populations most at risk. Moreover, results from such studies can help identify populations doing little, or nothing at all, to avoid being bitten by mosquitoes.
This paper explores the interactions between mosquitoes and humans in two cities, Kisumu and Malindi, Kenya. Descriptions of what people say they are doing to avoid being bitten are presented. Household wealth, education level, and the community's level of planning and drainage were used to estimate the probability that a household engages in multiple mosquito-avoidance activities, or has all members sleeping under a bednet. The first part of this paper describes the importance of understanding what people are doing to avoid being bitten, while the second presents findings, and discusses policy implications for malaria transmission control in urban areas.
The health belief model (HBM), which has driven so much of public health programming in the past decade, is predicated on the idea that individuals or their carers must first perceive the health issue as a problem, and then understand its origins and causes [14]. The HBM is driven by the premise that behaviour change must be preceded by knowledge change. In the case of malaria prevention, the use of bednets or curtains should be accompanied by commensurate knowledge of the pathogen transmission process. However, there is evidence to suggest that education levels and explicit knowledge of transmission may not be prerequisites to the uptake of mosquito- or malaria-prevention activity. Aygepong and Manderson [15] showed that households in Accra were engaged in mosquito prevention regardless of whether they had correct knowledge about transmission. The term "nuisance avoidance" was used to describe this behaviour. Another premise that underscores many programmes is that increased education levels means that people are more likely to understand the transmission cycle, and that this factor alone can lead to behaviour change. Although health education may be an important component, the toxic irritant in the saliva of the mosquito may be the only stimulus needed for people to modify their behaviour. There is evidence that many communities employ multiple methods to avoid being bitten. The use of animals as decoys is a strategy in some pastoralist and agriculturalist communities in East and West Africa [16-19]. Shutters, doors, screens, or windows are commonly used as barriers against mosquitoes in many areas across Africa. In Kenya, people have reported using sisal bundles stuffed into cracks to keep out mosquitoes [19]. Throughout Africa, communities report burning organic material, such as dung, wheat, wood from the Neem tree, and leaves to produce smoke, on the grounds that smoke repels mosquitoes [20]. Other communities have reported using permethrin-impregnated sisal curtains to protect themselves [21]. Semi-nomadic Samburu herdsmen reportedly cover themselves in the sand of dry riverbeds at night, while travelling through areas where the abundance of mosquitoes is particularly bothersome (M. Lochigan Pers. Comm. 2000). In short, communities have been practicing mosquito-avoidance long before they comprehend links between malaria and mosquitoes.
The positive relationship between economic resources and high health status has often been noted in many public health problems. Economic resources, whether measured by income levels or by asset accumulation, may be proxies for many other pathways to improved health. This may occur directly as economic resources affect access to health care or the ability to purchase medicines, or indirectly as more efficient use of prophylactics or prevention measures is associated with higher education levels or improved environmental conditions. However, whether this relationship holds at the household level in the context of mosquito-avoidance and prevention behaviours has rarely been measured. One study of urban malaria behaviours does suggest that poorer households are less likely to be using protection against mosquito bites [15]. But this study used location alone as a proxy for wealth. There has been little work in urban Africa that investigates the relationship between wealth and mosquito-avoidance behaviours as practised within households.
Given that humans desire to sleep peacefully and not be bitten, it is worth examining factors that determine the use of mosquito-avoidance measures. We hypothesize that at the household level important factors may include house type, household wealth, household density, and house location. Safe water access, the existence of engineered water delivery and drainage systems, the presence or absence of mosquitoes, and topography may also be important.
Methods
Study sites
Kisumu is Kenya's third largest city, has approximately 315,000 inhabitants, and is located about 10 km south of the equator on Lake Victoria in Nyanza Province. Kisumu is made up of industrial, commercial, and residential areas, with patches of agricultural land, gardens, tall grass, and a swamp which maintains the riparian and marine ecology along the lakeshore. Industries include, fishing, beer-brewing, air, marine and rail transport. Most of the population is occupied in informal activities such as produce markets, bicycle- and car-repair, car-washing, although a formal sector also exists and consists of banking, teaching, commercial, the public and civil service [22]. Important vectors of malaria in this region include Anopheles gambiae, An. arabiensis, and An. funestus [23,24], although nuisance-biting Culex, Mansonia and Aedes species are common.
Malindi is Kenya's tenth largest urban centre, has approximately 80,500 inhabitants, and is located on the Indian Ocean in Coast Province. Urban Malindi is made up of commercial and residential areas, with most residents engaged in fishing, tourism, trading, and informal service-type economic activities [22]. The major malaria transmitting mosquitoes along the coast include An. gambiae, An. arabiensis, An. merus, and An. funestus [1]. Culicine are also present in rural and urban areas. Adjacent rural sites were also included in the sample frame to serve as a basis for ecological comparisons. We defined the comparison areas as "rural" for both cities, as most of the livelihoods of those living in these areas were clearly related to agriculture.
Data collection
In May, 2001, household surveys were administered to 412 households in urban Kisumu, and 100 households in an adjacent rural area (Tiengre), and 380 households in Malindi, and 100 households in an adjacent rural area. Keating et al. [25] describe the integrated sampling strategy that provided the foundation for the sampling strategy employed in this cross-sectional study. Briefly, the goal was to develop a random sampling scheme that captured both the human-ecological and biological effect of human-mosquito interaction in urban environments. Global positioning system (GPS) units were used to collect latitude and longitude coordinates for all major roads, water-ways and significant landmarks. These coordinates, which were linked to existing georeferenced administrative data, were used to develop base-maps for Kisumu and Malindi in ArcView 3.2®, a Geographic Information System (GIS). The sample frame was constructed through the overlay of a measured grid, consisting of 270 × 270 meter cells, on each site. The study area was stratified based on the level of planning and drainage present within each grid cell. This resulted in 5 strata for each study site: 1) planned, well drained; 2) planned, poorly drained; 3) unplanned, well drained; 4) unplanned, poorly drained, and 5) rural. A systematic random sampling strategy was then used to select a proportionate number of grid cells from each stratum. Twenty grid cells were selected in Kisumu and 28 grid cells in Malindi. Grid cell boundaries were located using compasses, base maps, and existing landmarks [25]. Figure 1 illustrates the base maps for the two cities.
Figure 1.
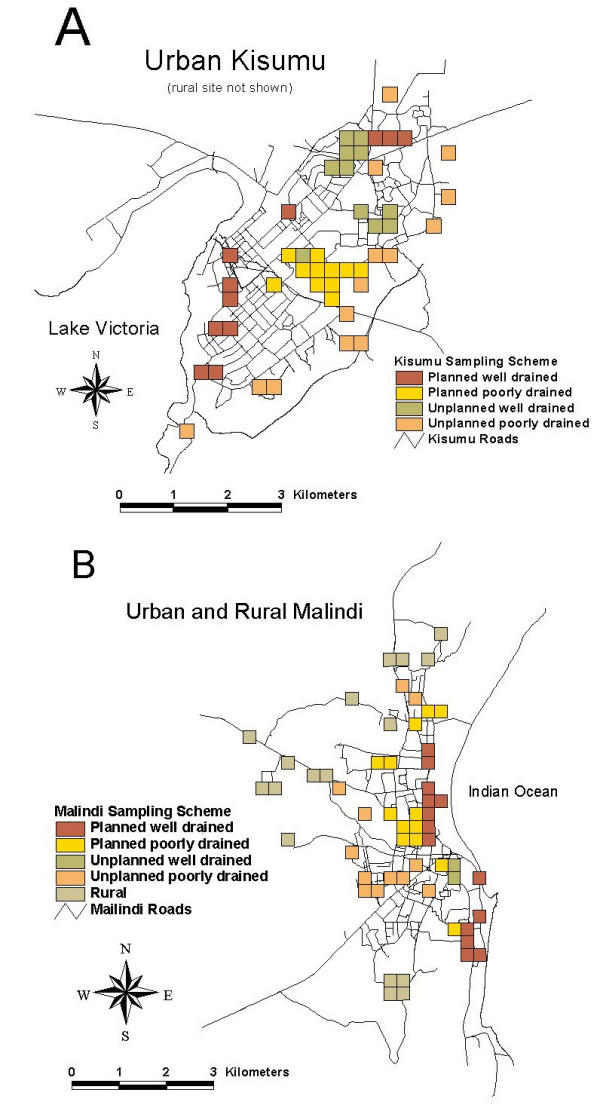
A: Map showing stratified, sampling scheme for Kisumu B: Map showing stratified, sampling scheme for Malindi
Households were selected from within the randomly selected grid cells, and about 100 surveys were completed in each stratum for both cities. Random direction was used to approach ten houses from each selected grid cell. In strata containing fewer than 10 grid cells, the 100 households to be surveyed were divided equally among the total number of selected grid cells falling within the stratum. In grid cells where houses were absent or inaccessible, questionnaires were administered to randomly selected households in adjacent grid cells of the same stratification type.
Interviews completed with one adult per household included questions about socio-economic status, education, housing type, domestic water-source, rubbish disposal and basic demographic information. Questions about mosquito-prevention practices and knowledge of mosquitoes were also asked. These included questions about what methods the household used, and who slept under nets.
Data analysis
Wealth, education, housing density, and planning and drainage data were analysed using chi-square analysis. Household density did not test significant as a categorical or continuous variable and was not considered further in this analysis. The controlled effects of the covariates household wealth, education, and the community effect of the strata's underlying planning and drainage were tested against the two research questions using logistic regression. The research questions were as follows: Are the proportions of households engaged in multiple mosquito-avoidance measures different among strata, wealth groups, and education groups? If so, what is the effect of this difference on the probability that a household will engage in multiple mosquito-avoidance efforts? Secondly, are the proportions of households where all occupants sleep under a bednet different among wealth groups, educational levels, and planning and drainage? If so, is the probability that all members of a household sleep under a bednet a function of these same factors?
The dependent variable in model one was whether or not the household engaged in multiple mosquito protection measures. Households were considered to have engaged in multiple mosquito protection measures if at least three of the following measures were reportedly used: coils, bednets, screening of windows and eaves, repellents, clearing debris from drains and ditches, burning of organic material, or insecticides. The dependent variable in model two was whether or not it was reported that everyone in the household sleeps under a bednet every night.
Independent variables were wealth, education, and the area's levels of planning and drainage. A high, medium, and low wealth index was created using factor analysis techniques based on reported household ownership of various items. Households were considered high income if an occupant owned a car or satellite dish. The medium income group included households owning at least a bicycle or radio, and either a television, electricity, or telephone. Low income was defined as ownership of nothing listed on the questionnaire, or ownership of only a bicycle or radio. The education variable was created by assigning households to low, medium, or high education groups, based on the reported highest level of education completed by any household member. High education was equal to Form 4 secondary through college or university. Medium education was equal to Standard 7/8 through Form 3. Low education was equal to no education through Standard 6. The planning and drainage variable was created by categorizing the stratification type of each randomly selected grid cell and assigning that value (1–5) to households falling within each respective strata.
Logistic regression was used to determine the relationship between households using multiple mosquito-avoidance techniques, and wealth, education, and the areas level of planning and drainage. An alpha level of 0.05 was chosen to indicate the significance of the independent variables. Wald's statistics and log-likelihood ratios of the models were used to identify variable significance and model fit. Data analysis was done using SPSS version 10.0.
Results
In Kisumu, 512 households completed a socio-economic questionnaire. One hundred and thirty seven (26.8%) households reported all occupants using a bednet, and 277 (54%) households reported using multiple mosquito-avoidance measures. The proportion of households falling within the high, medium, and low-income group was 13.1%, 6.3%, and 80.7%, respectively. Forty-six percent of the households sampled in Kisumu had access to electricity, and 12.6% reported owning a car. The proportion of households occupying the high, medium, and low education groups was equal to 10%, 35.4%, and 54.6%, respectively. The proportion of houses sampled occupying the various planning and drainage strata was approximately even. Table 1 provides survey summary statistics for the various strata in Kisumu study area. In general, the trends are in the expected direction. For example, the planned, well-drained stratum (Strata 1) had the highest proportion of residents with access to the main sewer and stratum 5, the rural comparison area, had the least. The unplanned poorly drained and rural stratas (Strata 4 and 5, respectively) had the highest number of reported malaria cases, and the two planned strata (Strata 1 and 2) had the least.
Table 1.
Summary household statistics for Kisumu by planning and drainage strata
| Strata | |||||
| Planning & drainage | 1 | 2 | 3 | 4 | 5 |
| Number of HHs | 103 | 100 | 113 | 95 | 101 |
| Average # of people per HH | 5.4 | 5.7 | 5.8 | 4.7 | 4.4 |
| % HH with electricity | 67.3 | 76.0 | 64.0 | 11.5 | 6.0 |
| % HH with access to main sewer | 49.0 | 76.1 | 26.7 | 9.7 | 0.0 |
| % HH harbouring livestock** | 30.9 | 25.5 | 29.6 | 28.3 | 63.0 |
| % HH using bednets | 71.8 | 60.0 | 54.0 | 54.7 | 39.0 |
| % HH with screens | 65.0 | 64.0 | 60.2 | 21.0 | 15.8 |
** With livestock present in household or within compound. 1 = Planned, 2 = Planned, poorly-drained 3 = Unplanned, well-drained 4 = Unplanned, poorly-drained well-drained 5 = Rural
In Malindi, 480 households completed the questionnaire: 64% of them reported using multiple mosquito-avoidance measures, and 52 % of households reported all occupants use a bednet. The proportion of households within the high, medium, and low-income groups was 19.4%, 9.8%, and 70.8%, respectively. In Malindi, 52.7% of all households sampled reported having access to electricity, and 14.4% reported car ownership. The proportion of households within the high, medium, and low-education groups were 37.9%, 31.9%, and 30.2%, respectively. Again, the proportion of households within each planning and drainage stratum was approximately equal. Selected summary statistics for Malindi (see Table 2) show trends in the expected directions. For example, 72% of the households in stratum 1 reported using bednets, whereas 39% reported using bednets in the rural stratum.
Table 2.
Summary household statistics for Malindi by planning and drainage strata
| Strata | |||||
| Planning & drainage | 1 | 2 | 3 | 4 | 5 |
| Number of HHs | 100 | 100 | 80 | 100 | 100 |
| Average # of people per HH | 4.1 | 4.1 | 6.0 | 5.9 | 6.2 |
| % HH with electricity | 83.0 | 88.0 | 55.0 | 27.0 | 11.0 |
| % HH with access to main sewer | 15.0 | 8.0 | 2.5 | 3.0 | 1.0 |
| % HH harbouring livestock** | 32.0 | 24.0 | 16.3 | 29.0 | 61.0 |
| % HH using bednets | 82.0 | 75.0 | 75.0 | 69.0 | 46.0 |
| % HH with screens | 71.0 | 79.0 | 57.5 | 59.0 | 28.0 |
** With livestock present in household or within compound. 1 = Planned, well-drained 2 = Planned, poorly-drained 3 = Unplanned, well-drained 4 = Unplanned, poorly-drained 5 = Rural
Table 3 lists the number of households reporting various methods of mosquito-avoidance in both Kisumu and Malindi. In general, bednets and mosquito coils were the most reported mosquito-prevention activity. Two and 15 households in Kisumu and Malindi, respectively reported burning of organic material to repel mosquitoes. In both cities, bednets and coils in combination were reported more often than other combinations of mosquito-avoidance activity. In Kisumu, 18.6% said they did nothing to prevent being bitten, whereas only 2.3% of the households in Malindi reported doing nothing. In Malindi, 8 of the 11 households that reported no form of preventive action were from the rural area. In Kisumu, the planned well-drained stratum had the least number of households doing nothing and the unplanned, poorly-drained stratum and the rural area had the most. Moreover, 73% of the households in wealthiest group in Malindi reported using bednets versus only 44% of the households occupying the lowest wealth group. Similarly, 51% in Kisumu's richest wealth group reported using bednets compared to 22% of the households occupying the lowest wealth group.
Table 3.
Number of households reporting mosquito-avoidance activity in Kisumu and Malindi, Kenya (% of total)
| Mosquito-avoidance Activity | Kisumu | Malindi |
| Bednets | 287 (56%) | 332 (69) |
| Mosquito coils | 207 (40%) | 257 (54%) |
| Screens on doors & windows | 27 (5%) | 153 (32%) |
| Burning organic material | 2 (.004%) | 15 (3%) |
| Mosquito sprays | 69 (13%) | 128 (27%) |
| Mosquito repellents | 4 (.008%) | 25 (5%) |
| No reported mosquito-avoidance activity | 95 (18.6%) | 11 (2.3%) |
| Bednets & coils | 101 (20%) | 154 (32%) |
| Bednets & sprays | 48 (9%) | 101 (20%) |
| Bednets & screens | 21 (4%) | 117 (24%) |
| Sprays & coils | 19 (4%) | 58 (12%) |
| Coils & repellants | 1 (.002%) | 14 (3%) |
| Total Responses | 512 (100%) | 480 (100%) |
The questionnaire attempted to gauge whether respondents had correct knowledge regarding mosquito habitat and behaviour. The results were varied. In Malindi, 77.8% of the respondents correctly reported mosquito habitat as stagnant water, inside dark houses, or vegetation. Seventeen percent reported not knowing. When asked why mosquitoes are sometimes found inside the house, 30% reported that the mosquitoes were either resting or feeding, whereas 40% reported not knowing and 28% reported incorrect answers. In Kisumu, 75% correctly reported mosquito habitat as vegetation, stagnant water, and inside dark houses and 8% reported that they did not know. When asked as to why mosquitoes are sometimes found inside houses, 85% reported that mosquitoes were either resting or hiding from the light, and 8% reported not knowing. Bivariate results reveal that the proportion of households engaged in multiple mosquito-prevention efforts differ for households occupying areas of different planning and drainage levels (p < 0.001), different wealth groups (p < 0.001), and different education groups (p < 0.001) in both cities (Table 4). The proportion of households with all occupants sleeping under bednets is also statistically different for households among strata, among wealth groups, and among the defined education groups (Table 5).
Table 4.
Proportion of households engaged in multiple mosquito-avoidance behaviours by wealth, education, and planning and drainage variables (# of households interviewed).
| Variables | Kisumu (n = 512) | Malindi (n = 480) | ||
| Wealth | ||||
| • Low | 47.2 | 86.0 | ||
| • Medium | 87.5 | 74.5 | ||
| • High | 80.6 | *p < 0.001 | 56.5 | *p < 0.001 |
| Education | ||||
| • Low | 39.2 | 72.5 | ||
| • Medium | 35.4 | 51.0 | ||
| • High | 68.8 | *p < 0.001 | 66.9 | *p < 0.001 |
| Planning and Drainage | ||||
| 1. Planned well drained | 71.8 | 70.0 | ||
| 2. Planned poorly drained | 71.0 | 71.0 | ||
| 3. Unplanned well drained | 65.2 | 80.0 | ||
| 4. Unplanned poorly drained | 35.8 | 57.0 | ||
| 5. Rural | 24.8 | *p < 0.001 | 45.0 | *p < 0.001 |
*Chi-square analysis within variables
Table 5.
Proportion of households reporting all occupants sleeping under bednets by wealth, education, and planning and drainage variables (# of households interviewed).
| Variables | Kisumu (n = 512) | Malindi (n = 480) | ||
| Wealth | ||||
| • Low | 21.8 | 43.5 | ||
| • Medium | 40.6 | 72.3 | ||
| • High | 50.7 | *p < 0.001 | 73.1 | *p < 0.001 |
| Education | ||||
| • Low | 15.7 | 43.4 | ||
| • Medium | 13.3 | 47.1 | ||
| • High | 37.3 | *p < 0.001 | 63.2 | *p < 0.001 |
| Planning and Drainage | ||||
| 1. Planned well drained | 45.6 | 71.0 | ||
| 2. Planned poorly drained | 32.0 | 61.0 | ||
| 3. Unplanned well drained | 24.1 | 57.5 | ||
| 4. Unplanned poorly drained | 18.9 | 45.0 | ||
| 5. Rural | 12.9 | *p < 0.001 | 27.0 | *p < 0.001 |
*Chi-square analysis within variables
Results from the multivariate analysis in Kisumu indicate that the probability of multiple mosquito-avoidance efforts being used in a household is a function of household wealth, education, and level of planning and drainage (Table 6). Controlling for planning and drainage, the wealthiest, best educated households were five times more likely that households in the lowest wealth and education categories to adopt multiple mosquito-avoidance activities in the family compound (OR = 5.15; 95% CI = 2.04,12.98). A positive relationship exists between the probability of the outcome occurring and the level of planning and drainage of the community; the planned well-drained, planned undrained, and unplanned well-drained strata are all significantly associated with the practice of multiple mosquito-prevention measures at the household level. However, caution should be used when interpreting this result given that it is unclear to what extent household wealth and a strata's level of planning/drainage are confounded. Thus, it is difficult to determine if this variable reflects the adult or larval mosquito habitat, or simply higher socio-economic levels.
Table 6.
Summary statistics for logistic model predicting odds that a household engages in multiple mosquito-avoidance behaviours.
| Variables | Kisumu Odds Ratio | 95% CI | Malindi Odds Ratio | 95% CI |
| Wealth | ||||
| • Low | 1.00 | Ref. group | 1.00 | Ref. group |
| • Medium | 4.07* | (1.36, 12.17) | 1.54 | (0.73, 3.24) |
| • High | 2.39* | (1.21, 4.71) | 3.79* | (1.92, 7.45) |
| Education | ||||
| • Low | 1.00 | Ref. group | 1.00 | Ref. group |
| • Medium | 0.81 | (0.40, 1.63) | 0.523* | (0.32, 0.86) |
| • High | 2.16* | (1.09, 4.30) | 1.08 | (0.65, 1.79) |
| Planning and Drainage | ||||
| • Rural (Strata 5) | 1.00 | Ref. group | 1.00 | Ref. group |
| • Planned well drained (Strata 1) | 4.79** | (2.48, 9.23) | 1.71 | (0.91, 3.23) |
| • Planned poorly drained (Strata 2) | 4.94** | (2.56, 9.53) | 1.89* | (1.01, 3.56) |
| • Unplanned well drained (Strata 3) | 3.31** | (1.74, 6.3)) | 3.98** | (1.98, 7.99) |
| • Unplanned poorly drained (Strata 4) | 1.53 | (0.81, 2.91) | 1.48 | (0.83, 2.62) |
*p < .05, **p < .001
Results from Malindi differed somewhat from those of Kisumu with respect to the practice of multiple mosquito-prevention measures. While the wealthiest households were significantly more likely than the poorest households to practice multiple mosquito-prevention measures (OR = 3.79; 95% CI = 1.93, 7.45), a household's education level was not associated with the outcome (Table 6).
The model for Malindi testing the probability that everyone in a household sleeps under a bednet indicates that higher levels of wealth and education were associated with bednet usage (Table 7). Again, the wealthiest and best educated households were almost four times as likely as the poorest, least educated households to have reported that all household members sleep under a bednet (OR = 3.80; 95% CI = 1.91, 7.55). The level of planning and drainage also tested significant, suggesting that in Malindi, community factors are related to mosquito control as well as household factors. With respect to wealth and education, the results were similar in Kisumu. The wealthiest and best educated households were again more likely than the poorest, least educated households to report bednet use (OR = 6.88; 95% CI = 2.56,18.49: see Table 7).
Table 7.
Summary statistics for logistic model predicting the odds that everyone in a house sleeps under a bednet.
| Variables | Kisumu Odds Ratio | 95% CI | Malindi Odds Ratio | 95% CI |
| Wealth | ||||
| • Low | 1.00 | Ref. Group | 1.00 | Ref. group |
| • Medium | 1.78 | (0.81, 3.92) | 2.10* | (1.03, 4.29)) |
| • High | 2.38** | (1.33, 4.25) | 2.15* | (1.23, 3.75) |
| Education | ||||
| • Low | 1.00 | Ref. Group | 1.00 | Ref. group |
| • Medium | 0.96 | (0.39, 2.38) | 1.25 | (0.77, 2.02) |
| • High | 2.90* | (1.25, 6.74) | 1.78* | (1.10, 2.86) |
| Planning and Drainage | ||||
| • Rural (Strata 5) | 1.00 | Ref. group | 1.00 | Ref. group |
| • Planned well drained (Strata 1) | 3.36** | (1.6, 7.05) | 4.50** | (2.34, 8.63) |
| • Planned poorly drained (Strata 2) | 1.91 | (0.90, 4.09) | 2.95** | (1.56, 5.57) |
| • Unplanned well drained (Strata 3) | 1.09 | (0.50, 2.4) | 3.12** | (1.63, 5.97) |
| • Unplanned poorly drained (Strata 4) | 1.38 | (0.62, 3.07) | 2.10* | (1.15, 3.83) |
*p < .05, **p < .001
Discussion
Three main findings emerge from this analysis. First is the almost ubiquitous nature of the efforts: virtually every household sampled report using some form of protection. However, the data do not suggest that individuals are knowledgeable about vector-borne parasite transmission or necessarily acting to prevent malaria. It may be simply that individuals are avoiding nuisance mosquito contact. This is good news for international public health. Most public health programmes struggle to find a population-based impetus for raising enthusiasm. In this situation, people do not want to be bitten, irrespective of their knowledge of the transmission mechanism. Health educators, working on mosquito-prevention programmes, should be able to build on these activities.
Second, some of the poorest households in our sample reported using some of the most expensive methods available on the market (i.e., they are burning coils and using sprays). Although it is not known how frequently these measures are employed, the repeated purchase of coils and sprays could be costly. Pricing of personal protection methods in Kenya suggests that a packet of 10 coils cost KSH 30.00 (equivalent to US$.38 cents), and a coil is available singly at KSH3.50 each. Aerosol sprays range between KSH120 and 220 (US$1.50 to 2.82), while bednets cost between from KSH350.00 to 750.00 (US$4.50 to $10.00). Thus, while poor households may actually be spending more on coils or sprays, the richer households are, according to these results, much more likely to use bednets. As such, household wealth is a good predictor of whether the inhabitants of a household engage in mosquito-prevention activities. When a good is valued and provides a major public service, through protection at a population level, it is often considered for subsidization. Although this fact is not new, as evidenced by the increase in social marketing of bednets in Africa [26], it does provide more evidence that even among the least educated, living in very degraded slums, people avoid mosquitoes if they can afford it. More attention is needed from the international health community emphasizing the need to get bednets and other protective methods subsidized by local and national governments or by other donors and NGOs.
Third, in parallel with Manderson and Aygepong's work in Ghana [15], who found that knowledge of malaria was not a necessary prerequisite for mosquito-avoidance behaviour, we also found that many inhabitants are actively trying to avoid being bitten, even if knowledge of how malaria is transmitted is incorrect or lacking. Despite this, the level of education within Kisumu households was an important predictor of whether the household used multiple methods of protection or whether everyone in the house slept under a net.
Kisumu and Malindi are very different cities, differing across ecology, culture, history and economics. In common, however, they are both rapidly growing urban centres in malaria endemic areas and both cities report malaria transmission with varying degrees of severity throughout the year. As such, it is not surprising that both of these urban areas have high proportions of the population doing something to avoid mosquitoes. However, mosquito-avoidance behaviours differ between the two cities. The higher bednet use in Malindi as compared to Kisumu, and higher multiple bednet use in these households, may be a consequence of increased social marketing of bednets and intense community-based programme activity in the area in recent years. Since 1995 there has been increased awareness of using insecticide treated bednets in Malindi through social marketing strategies conducted by PopulationServices International, a international NGO with a country office in Kenya. Secondly, this awareness enabled the formation of many community groups involved in environmental management such as tree planting, drainage, and mosquito control. A few of these are also involved in the manufacturing and treating bednets for sale. Thus, knowledge of the advantages of bednets may have spread through family or community networks, and availability (either through large subsidization or through free distribution) and may have been the partial cause of increased access in Malindi. There are far fewer community-based programmes in Kisumu.
The categorizing of urban areas into strata reflects a compilation of ecological factors such as the topographical slope and drainage facilities in the area, the condition of roads, the state of drains and sewerage systems, rubbish collection and other factors. This is essentially a community level measure of wealth. This contrasts to wealth as measured at the household level. Community-level stratification captures factors that are difficult to control for, such as quality and condition of households in the area, variation in how much a community takes care of its immediate environment (civic pride or responsibility), and resources the community can access, such as municipal vector control, municipal maintenance of drains and water mains and paved roads. Our analysis suggests that these unmeasured community level differences are significant for the most affluent, and poorest communities in both cities. Policy makers should consider that in the poorer areas, where the great majority of people live, even those who are relatively better off, need help as there are factors operating beyond their immediate control at the community level that influence their ability to share resources and protect themselves from mosquitoes.
The results of this study demonstrate the importance of examining human-mosquito interaction in terms of how access to resources, including education and financial resources, may enhance human activities and help determine if and how they subsequently protect themselves from mosquito bites. The findings illustrate that the poorest segments of society are already doing many things to protect themselves from being bitten, but they are doing less than their richer neighbours. Gallop and Sachs [27] discuss the thesis that malaria in a country not only reflects considerable poverty, but the disease may actually be a cause of that poverty. Certainly, our results could be interpreted as contributing to this thesis. If the poorer households, motivated by the similar urge for a peaceful nights sleep as their richer counterparts, insist on paying out of pocket for the relatively more expensive protective methods, then it is easy to see that just the act of attempting to prevent mosquitoes from biting may be helping to keep these households from improving their well-being as well as their health status.
Authors' contributions
KM helped conceive of the study and led the drafting of this manuscript; JK supervised data collection, helped analyze the data and co-wrote the paper; SS helped analyze data, LK helped collect and analyze data; CM, AG and JB all conceived of the study, and helped in the write up of this paper. JB is the principal investigator of the study. All authors read and approved the final manuscript
Financial Support
This research was supported by NIH ICIDE and ABC Training grant numbers: D43 TW01142 and U19 AI45511 and NSF Grant DEB-0083602.
Acknowledgments
Acknowledgements
We are grateful for the assistance of Maurice Ombok, Richard Amimo, Francies Atieli, and Bryson Ndenga at the KEMRI-Center for Vector Biology and Control Research, Kisian, Kenya; and, Nellie Njoki, Samuel Kahindi, Salim Omar, and Mtawali Chai at the Center for Geographic Medicine Research-Coast, Kilifi, Kenya. We also wish to thank John I. Githure, James L. Regens, Chris Swalm, and Laura J. Steinberg. This paper is published with the permission of the Directors of the Kenya Medical Research Institute and ICIPE.
Contributor Information
Kate Macintyre, Email: kmacint@tulane.edu.
Joseph Keating, Email: jkeating@tulane.edu.
Stephen Sosler, Email: ssosler@tulane.edu.
Lydiah Kibe, Email: lkibe@hotmail.com.
Charles M Mbogo, Email: Cmbogo@kilifi.mimcom.net.
Andrew K Githeko, Email: AGitheko@kisian.mimcom.net.
John C Beier, Email: jbeier@tulane.edu.
References
- Mbogo CM, Snow RW, Khamala CP, Kabiru EW, Ouma JH, Githure JI, March K, Beier JC. Relationships between Plasmodium falciparum transmission by vector populations and the incidence of severe disease at nine sites on the Kenyan coast. Am J Trop Med Hyg. 1995;52:201–206. doi: 10.4269/ajtmh.1995.52.201. [DOI] [PubMed] [Google Scholar]
- Elissa N, Karch S, Bureau P, Ollomo B, Lawoko M, Yangari P, Ebang B, George AJ. Malaria transmission in a region of savanna-forest mosaic, Haut-Ogooué, Gabon. J Am Mosq Control Assoc. 1999;15:15–23. [PubMed] [Google Scholar]
- Barbazan P, Baldet T, Darriet F, Escaffre H, DH H, Hougard JM. Impact of treatments with Bacillus sphaericus on Anopheles populations and the transmission of malaria in Maroua, a large city in a savannha region of Cameroon. J Am Mosq Control Assoc. 1998;14:33–39. [PubMed] [Google Scholar]
- Khaemba BM, Mutani A, Bett MK. Studies on the anopheline mosquitoes transmitting malaria in a newly developed highland urban area: a case study of Moi University and its environs. East Afr Med J. 1994;71:159–164. [PubMed] [Google Scholar]
- Robert V, Gazon P, Ouedraogo V, Carnevale P. Ecology of larval mosquito, with special reference to Anopheles arabiensis (Diptera: Culicidae) in market-garden wells in the urban area of Dakar, Senegal. J Med Entomol. 1998;35:948–955. doi: 10.1093/jmedent/35.6.948. [DOI] [PubMed] [Google Scholar]
- Trape JF, Zoulani A. Malaria and urbanization in central Africa: the example of Brazzville Part II: results of entomological surveys and epidemiological analysis. Trans R Soc Trop Med Hyg. 1987;81:10–18. doi: 10.1016/0035-9203(87)90472-x. [DOI] [PubMed] [Google Scholar]
- Grimm NB, Grove JM, Pickett ST, Redman CL. Integrated approaches to long term studies of urban ecological systems. Bioscience. 2000;50:571–583. [Google Scholar]
- Nichter M, Kendall C. Beyond child survival: anthropology and international health in the 1990's. Med Anthro Q. 1991;5 [Google Scholar]
- Coene J. Malaria in urban and rural Kinshasa: the entomological input. Med Vet Ento. 1993;7:127–137. doi: 10.1111/j.1365-2915.1993.tb00665.x. [DOI] [PubMed] [Google Scholar]
- Dossou-yovo J, Doannio J, Rivière F, Duval J. Rice cultivation and malaria transmission in Bouaké city (Côte d'Ivoire). Acta Trop. 1994;57:91–94. doi: 10.1016/0001-706X(94)90097-3. [DOI] [PubMed] [Google Scholar]
- Robert V, Gazin P, Ouedraogo V, Carnevale P. Le paludisme urbain à Bobo-Dioulasso1 Etude entomologique de la transmission ORSTOM. 1986.
- El Sayed BB, Arnot DE, Mukhtar MM, Baraka OZ, Dafalla AA, Elnaiem DE, Nugud AH. A study of the urban malaria transmission problem in Khartoum. Acta Trop. 2000;25:163–171. doi: 10.1016/S0001-706X(99)00098-4. [DOI] [PubMed] [Google Scholar]
- WHO 1998 Roll Back Malaria. 1998.
- Janz N, Becker MH. The Health Belief Model: A Decade Later. Health Edu Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Agyepong IA, Manderson L. Mosquito avoidance and bed net use in the greater Accra region, Ghana. J Biosocial Sci. 1999;31:79–92. doi: 10.1017/S0021932099000796. [DOI] [PubMed] [Google Scholar]
- Bruce-Chwatt L. Essential Malariology. London: Heinemann Medical Books; 1980. [Google Scholar]
- Little MA, Leslie PW. Turkana herders of the dry savanna: ecology and biobehavioral response of nomads to an uncertain environment. New York: Oxford University Press; 1999. [Google Scholar]
- Hill AG. Population, health and nutrition in the Sahel: issues in the welfare of selected West African communities. London: Kegan Paul International; 1985. [Google Scholar]
- MacCormack CP. Human ecology and behavior in malaria control in tropical Africa. Bull World Health Organ. 1984;62:81–87. [PMC free article] [PubMed] [Google Scholar]
- Robert EK, Weller SC, Zeissig R, Richards FO, Ruebush TK., II Knowledge, beliefs, and practices in relation to malaria transmission and vector control in Guatemala. Am J Trop Med Hyg. 1995;52:383–388. doi: 10.4269/ajtmh.1995.52.383. [DOI] [PubMed] [Google Scholar]
- Karanja DMS, Alaii J, Abok K, Adungo NI, Githeko AK, Seroney I, Vulule JM, Odada P, Oloo JA. Knowledge and attitudes to malaria control and acceptability of permethrin impregnated sisal curtains. East Afr Med J. 1999;76:42–46. [PubMed] [Google Scholar]
- Book 1999 Housing and Population Census of Kenya. Nairobi: National Bureau of Statistics; 1999. 1999 Housing and Population Census of Kenya. [Google Scholar]
- Petrarca V, Beier JC. Intraspecific chromosomal polymorphism in the Anopheles gambiae complex as a factor affecting malaria transmission in the Kisumu area of Kenya. Am J Trop Med Hyg. 1992;46:229–237. doi: 10.4269/ajtmh.1992.46.229. [DOI] [PubMed] [Google Scholar]
- Githeko AK, Service MW, Mbogo CM, Atieli F, Juma FO. Plasmodium falciparum sporozoite and entomological inoculation rates at the Ahero rice irrigation scheme and the Miwani sugar-belt in western Kenya. Ann Trop Med Parasitol. 1993;87:379–391. doi: 10.1080/00034983.1993.11812782. [DOI] [PubMed] [Google Scholar]
- Keating J, Macintyre K, Mbogo CM, Githeko AK, Regens JL, Swalm C, Ndenga B, Steinberg LJ, Kibe L, Githure JI, Beier JC. Relationships between house density and the abundance of larval habitats for Anopheles mosquitoes in Kisumu and Malindi, Kenya. Am J Trop Med Hyg. 2002.
- Armstrong-Schellenberg JRM, Abdulla S, Nathan R, Mukasa O, Marchant TJ. Effect of large scale social marketing of insecticide-treated nets on child survival in rural Tanzania. Lancet. 2001;357:1241–1247. doi: 10.1016/S0140-6736(00)04404-4. [DOI] [PubMed] [Google Scholar]
- Gallup JL, Sachs J. The economic burden of malaria. Am J Trop Med Hyg. 2001;64:85–96. doi: 10.4269/ajtmh.2001.64.85. [DOI] [PubMed] [Google Scholar]


