Abstract
Background
Few assessments of the costs and benefits of reducing acute cardiorespiratory morbidity related to air pollution have employed a comprehensive, explicit approach to capturing the full societal value of reduced morbidity.
Methods
We used empirical data on the duration and severity of episodes of cardiorespiratory disease as inputs to complementary models of cost of treatment, lost productivity, and willingness to pay to avoid acute cardiorespiratory morbidity outcomes linked to air pollution in epidemiological studies. A Monte Carlo estimation procedure was utilized to propagate uncertainty in key inputs and model parameters.
Results
Valuation estimates ranged from $13 (1997, Canadian) (95% confidence interval, $0–28) for avoidance of an acute respiratory symptom day to $5,200 ($4,000–$6,400) for avoidance of a cardiac hospital admission. Cost of treatment accounted for the majority of the overall value of cardiac and respiratory hospital admissions as well as cardiac emergency department visits, while lost productivity generally represented a small proportion of overall value. Valuation estimates for days of restricted activity, asthma symptoms and acute respiratory symptoms were sensitive to alternative assumptions about level of activity restriction. As an example of the application of these values, we estimated that the observed decrease in particulate sulfate concentrations in Toronto between 1984 and 1999 resulted in annual benefits of $1.4 million (95% confidence interval $0.91–1.8 million) in relation to reduced emergency department visits and hospital admissions for cardiorespiratory disease.
Conclusion
Our approach to estimating the value of avoiding a range of acute morbidity effects of air pollution addresses a number of limitations of the current literature, and is applicable to future assessments of the benefits of improving air quality.
Background
Numerous assessments have been conducted around the world of the costs and/or benefits of interventions to improve air quality [1-7]. Benefits assessments typically employ the damage function approach, consisting of estimating changes in air pollution emissions and resultant changes in ambient air quality; calculating the number of avoided adverse health and environmental outcomes using concentration-response functions; and applying economic value measures to avoided outcomes [8], often extrapolating valuation estimates from the original context in which data were collected [9]. The majority of benefits generally derive from improved human health, including both reduced mortality and morbidity. Benefits of reduced mortality and chronic morbidity tend to dominate these assessments, accounting for over 90 percent of benefits in most instances [1,7]. Nonetheless, acute morbidity is still viewed as an important component of the broad public health burden associated with air pollution [10], and benefits assessments will undoubtedly continue to include acute morbidity effects. Thus, future assessments will need to address deficiencies in past work dealing with acute morbidity, including failure to consistently employ a comprehensive, explicit approach to capturing all components of the societal value of reduced morbidity and differing levels of severity of symptoms and activity restrictions.
In earlier analyses [3,5], consideration of morbidity effects of air pollution was restricted to a limited range of symptoms and activity restrictions as observed in clinical and epidemiological studies. These assessments, as well as more recent ones [2], relied heavily on contingent valuation studies [11-13] in which individual willingness to pay (WTP) to avoid a variety of symptoms of varying duration was evaluated. In more recent assessments, there has been a greater reliance on cost of illness (COI) data, comprising medical costs and lost production experienced by society as a result of a health effect. However, these measures represent at best a lower bound on the total societal value of avoiding these health outcomes [14], since they reflect only one element of this value. In some assessments, no adjustments have been made to correct for this bias [6,7], while in others, empirical evidence from studies which simultaneously measured COI and individual WTP have been used to derive adjustment factors [1,4,15-17]. Such adjustments recognize deficiencies in available estimates, but applying them uniformly to a variety of cardiorespiratory conditions could introduce error in benefits assessments. An additional issue is that most previous assessments have relied heavily upon valuation estimates derived from U.S. data, the applicability of which outside the U.S. can be questioned.
In the present study, our objective was to estimate the benefits of avoiding a variety of acute cardiorespiratory morbidity outcomes which have been linked epidemiologically to air pollution, using complementary data on COI and individual WTP. In contrast to the lack of a consistent, comprehensive approach in earlier studies, particular features of our approach include application to all outcomes of: a consistent conceptual model of the nature of acute episodes of cardiorespiratory disease, including differing levels of severity of symptoms and activity restrictions; a comprehensive valuation framework encompassing all aspects of the value of avoided morbidity and a recognition of the perspective (societal versus individual) from which primary data were collected; a common source of inputs based on empirical data on the duration and severity of episodes of cardiorespiratory disease; and an estimation procedure which propagates uncertainty in key inputs.
Methods
Conceptual model of acute cardiorespiratory morbidity
We identified several types of acute cardiorespiratory morbidity which have been linked with air pollution in epidemiological studies: respiratory and cardiac hospital admissions and emergency department visits, restricted activity days, asthma symptom days, and acute respiratory symptom days [18-21]. Based on this literature, we identified asthma, chronic obstructive pulmonary disease (COPD), respiratory infections, congestive heart failure, cardiac dysrhythmias, and myocardial infarction/angina, as well as mild non-specific respiratory symptoms, as the principal conditions of interest [18-22].
As a general framework, we viewed these conditions as occurring in the form of acute episodes superimposed upon the underlying baseline health state. The extent to which health status departed from its premorbid level could be expected to vary during the course of the episode, so that the episode of illness could be characterized as the sum of several periods, each of which is associated with a given decrement from baseline health status. Depending on the nature of the morbidity outcome, these periods might include periods spent in or out of hospital, and in various states of restriction of activity.
Valuation framework
Reduced morbidity due to cleaner ambient air represents real economic value to individuals and society, measured most appropriately in a welfare economic framework by WTP to improve health or willingness to accept compensation (WTA) to worsen it [23]. Measures such as quality- or disability-adjusted life years (QALYs or DALYs) represent an alternative measure which generically reflects preferences among health states involving loss of quality and/or quantity of life [24]. However, experience with application to acute effects of air pollution is limited [25], and unlike dollar valuation of health outcomes, these measures do not permit direct comparisons to costs. WTP (and WTA) are generally regarded as comprising several components: expenditures related to medical treatment of adverse health effects, including costs of treatment as well as related out of pocket expenditures (for example, for assistance in completing usual unpaid chores that the individual is unable to undertake as a result of ill health); the dollar value of interruption in work duties, which can range from decreased productivity to absence from the workplace; expenditures to avert or mitigate future occurrences of the effect (eg. purchasing an air conditioning unit as a means of reducing the chances of an asthma attack associated with outdoor air pollution); and the dollar value of pain and suffering, inconvenience, restrictions and reduced enjoyment of leisure activities, anxiety about the future, and concern and inconvenience to family members and others [14]. The perspective of the analysis (societal versus individual) is clearly an important consideration, in that individual WTP will not reflect medical expenditures and lost productivity where there is third party payment of medical expenditures or paid sick leave [8,14,26].
A comprehensive measure of the total value, from a societal perspective, of avoiding the acute cardio-respiratory morbidity effects of air pollution can therefore be expressed as follows:
VT = VAE + VPS + VCOT + VLP (1)
where,
VAE = value of reduced averting expenditures;
VPS = value of reduced pain and suffering;
VCOT = cost of treatment including reduced expenditures on mitigation of the illness; and
VLP = value of lost productivity.
Sources of empirical data
We used empirical results from two recent studies in order to generate estimates of VT. Both studies have been described in detail elsewhere [27-29], but are summarized briefly below.
In the first study, joint estimates were constructed of individual WTP to reduce acute episodes of respiratory and cardiovascular ill health based on graded-pairs and choice-based stated preference survey responses among 399 randomly selected subjects in Toronto in 1997 [28,30]. The survey instrument employed health-state descriptions based on the Quality of Well Being (QWB) index [31,32], with attributes comprising symptoms, motor function, and ability to fulfill roles and expectations. The scope of symptoms was selected to correspond to the cardiorespiratory conditions of policy interest as described above. Four levels of activity restriction were considered (Table 1). The payment vehicle employed in this survey was described as illness related costs not covered by the government health system or a company insurance plan. Because pre-testing revealed that respondents with and without paid sick leave interpreted costs differently and this led to ambiguity in interpretation of their WTP, respondents were instructed to assume that they had paid sick leave. By combining results from graded-pairs and choice formats, the resulting estimates from this study are more robust than estimates based on a single format. In addition, relative to other studies in the WTP literature in this area, estimates from this study were based on comprehensive multi-attribute health state descriptions which ensured that key attributes were clearly and consistently presented to respondents, for the wide range of symptoms and severity levels covered in the study. Estimates from this study were not systematically smaller or larger than other literature and varied logically with duration and severity of outcomes. However, given the payment vehicle and the instructions regarding sick leave, we determined that individual WTP estimated in this study would not reflect VLP or that portion of VCOT covered by public health care system or third party insurance. We obtained these data from the following study.
Table 1.
Description of symptoms and activity restrictions
| Type of symptom/activity restriction | Description |
| Upper Respiratory | Stuffy or runny nose and sore throat. |
| Eye Irritation | Eye irritation. |
| Asthma/COPDa | Coughing, wheezing, shortness of breath. |
| Respiratory Infection | Coughing or wheezing with fever, chills, aching all over. |
| Dysrhythmia | Fluttering in chest and feeling light-headed |
| Congestive Heart Failure | Shortness of breath, and swelling in ankles and feet. |
| Myocardial Infarction/Angina | Pain in chest or arm. |
| Mild Limitationsb | Can go to work, go to school, do housework, and participate in social or recreational activities, but have some physicial limitations (trouble bending, stooping, or doing vigorous activities because of this health condition). |
| Can go to work, go to school, do housework, but have some physical limitations (trouble bending, stooping, or doing vigorous activities), and cannot participate in social or recreational activities because of this health condition. | |
| Housebound | Cannot leave house, go to work, go to school, do housework, participate in social or recreational activities, and have some physical limitations (trouble bending, stooping, or doing vigorous activities) because of this health condition, but can care for self. |
| Help caring for Self | Cannot leave house, go to work, go to school, do housework, participate in social or recreational activities, and need help caring for self (feeding, bathing, dressing, toilet). |
| In Hospital | In hospital and need help caring for self (feeding, bathing, dressing, toilet) |
achronic obstructive pulmonary disease bcollapsed into a single level corresponding to mild restrictions, for the purposes of the final model used to generate WTP estimates.
In the second study, data were collected prospectively on individuals visiting emergency departments for cardiorespiratory conditions, as part of an epidemiological study of air pollution in Saint John, Canada between 1992 and 1996 [29,33]. A random sample of those agreeing to follow-up was contacted two weeks after their visit and asked to complete a structured telephone interview, in which information was collected on the duration of the disease episode which prompted their visit, disposition of their visit (whether they were admitted or discharged), and the occurrence of various outcomes including restricted activity days, days of missed work for the patient, parent, or other care giver, health care utilization and illness-related expenses, from the onset of their earliest symptoms until the follow-up interview. Data were obtained for 1,772 individuals. Inpatient utilization data were also abstracted from the clinical records of 393 randomly selected patients representing the same groups of cardiorespiratory conditions, and cost of illness estimates were generated which included fully allocated costs related to hospital utilization and emergency department visits, as well as costs of physician visits, medication use, equipment, and out-of-pocket expenses [27]. We analyzed these data using stepwise ordinary least squares regression. Selection of the final multi-variate model was based on minimization of Akaike's Information Criterion, the deviance penalized for the number of parameters being estimated [34]. Compared to other literature in this area, this study has the advantage of having been designed specifically to prospectively quantify the broad quality of life impacts and COI associated with episodes of cardiorespiratory disease, thus ensuring that the required data elements were collected in a consistent, coordinated fashion. Cost analysis was carried out in a manner consistent with current methodological standards.
Estimation procedure
Based on these two studies, we calculated VT according to Equation (1) as follows:
VPS + VAE = value from stated preference survey = VSP(SiAjDk) [28,30]
where Si, Aj, and Dk are the symptom complex, level of activity restriction and duration of the illness episode respectively (See [28] for details of the stated preference valuation estimation procedure).
VCOT = f (diagnosis, duration, admission to critical care/non critical care) (See results section below for model specification);
VLP = DLP × WD
where DLP = duration of lost productivity in days; and WD is the average daily wage for Canada in 1997 of $119.60 [35].
While recent recommendations note the friction cost method as an alternative to the conventional human capital approach as potentially more accurately reflecting the ability to replace disabled workers, thus minimizing societal productivity losses [26,36], we assumed that this was not applicable in the current context, where illness episodes are of short duration. We did not attempt to value productivity losses not resulting in lost time (i.e. reduced work capacity), but we did capture time lost by parents and other care givers.
In estimating VSP, we mapped symptoms and activity restrictions to the various health outcomes identifed in epidemiolgical and clinical studies as shown in Table 2. Some outcomes were mapped to time periods both in and out of hospital, in keeping with the expected natural history of an acute episode of cardiorespiratory morbidity. Hospital admissions, for example, were considered to occur following a period over which symptoms and activity restrictions began and worsened to the point that hospital admission was required, and in turn, to be followed by a period of recovery out of hospital before returning to the baseline health state. Similarly, a proportion of emergency department visits was expected to result in eventual admission to hospital, with accompanying periods of symptom onset and recovery. While, a priori, both asthma symptom days and restricted activity days would include days in hospital, on the basis of population-based data, we estimated that the latter would account for a very small proportion of these less severe outcomes [1,22,37]. We therefore did not map these outcomes to the in-hospital level of activity restriction in generating our estimates.
Table 2.
Mapping of symptoms and activity restrictions to health outcomes examined in epidemiological studies
| ARSa | RAD | ASD | REDV | RHA | CEDV | CHA | |
| Symptom Weightings (proportions) | |||||||
| Upper Respiratory | 0.70 | 0.40 | |||||
| Eye irritation | 0.30 | 0.15 | |||||
| Asthma/COPDb | 0.15 | 1.00 | 0.44 | 0.60 | |||
| Respiratory Infection | 0.15 | 0.56 | 0.40 | ||||
| Dysrhythmia | 0.05 | 0.23 | 0.13 | ||||
| Congestive Heart Failure | 0.05 | 0.27 | 0.28 | ||||
| Myocardial Infarction/Angina | 0.05 | 0.50 | 0.59 | ||||
| Activity Level Weightings (proportions) | |||||||
| Mild limitations | 0.90 | 0.80 | 0.90 | 0.74 | 0.50 | 0.41 | 0.34 |
| Housebound | 0.10 | 0.15 | 0.10 | 0.14 | 0.09 | 0.08 | 0.06 |
| Need help caring for self | 0.05 | 0.05 | 0.03 | 0.03 | 0.02 | ||
| In hospital | 0.07 | 0.37 | 0.48 | 0.57 | |||
aARS = Acute Respiratory Symptom Day ASD = Asthma Symptom Day RAD = Restricted Activity Day REDV = Respiratory Emergency Department Visit RHA = Respiratory Hospital Admission CEDV = Cardiac Emergency Department Visit CHA = Cardiac Hospital Admission bchronic obstructive pulmonary disease
Mapping of symptoms and levels of activity restrictions to a given outcome was derived from empirical data from our own emergency department study [29], and from a population-based survey in Strasbourg, France on the prevalence of minor respiratory symptoms [38]. Adjustments were made, where applicable, to shift the distribution towards the mild end of the spectrum to reflect those individuals who do not visit the emergency department and whose symptoms are presumably less severe on average.
The definitions of a number of health outcomes as examined in the air pollution epidemiology literature overlap with one another (e.g. hospital admissions and emergency department visits, restricted activity days and acute respiratory symptoms), and this is reflected in our mapping of these outcomes as shown in Table 2. This needs to be considered in order to avoid double counting of benefits among these health outcomes. Procedures have been suggested to deal with this, for instance by subtracting occurrences of restricted activity days, from those related to acute respiratory symptom days, prior to applying valuation estimates [1].
All inputs to our estimates pertaining to the duration of time in and out of hospital and of lost work days, and the probability of requiring inpatient care at the ward or critical care level (Table 3), were derived from Stieb et al. [29]. Based on data from the U.S. National Health Interview Survey, it was determined that work loss days comprise 21 percent of restricted activity days (standard error = 1.07%) [39] and we applied this factor in estimating lost productivity costs associated with restricted activity days. This is consistent with our mapping to the three levels of activity restriction, where 20% fell into the housebound or need help category. We assumed that 10 percent of asthma symptom days and acute respiratory symptom days were work loss days, based on the evidence described earlier.
Table 3.
Inputs on duration and disposition for valuation calculations
| Condition | Admitted to: | Number of days: | ||||||||
| Critical Care | Non-critical Care | In Hospital | Out of Hospital | Lost Work | ||||||
| Percent | Standard Error | Percent | Standard Error | Mean | Standard Error | Mean | Standard Error | Mean | Standard Error | |
| Individuals admitted to hospital | ||||||||||
| Asthma | 23.1% | 4.8% | 76.9% | 4.8% | 4.4 | 0.3 | 9.3 | 1.1 | 2.8 | 0.5 |
| Chronic Obstructive Pulmonary Disease | 0.0% | 0.0% | 100.0% | 0.0% | 7.9 | 0.7 | 9.4 | 2.6 | 0.8 | 0.6 |
| Respiratory Infection | 11.3% | 3.4% | 88.7% | 3.4% | 5.1 | 0.4 | 8.7 | 1.4 | 3.3 | 0.6 |
| Congestive Heart Failure | 12.9% | 6.0% | 87.1% | 6.0% | 7.2 | 0.7 | 8.9 | 2.4 | 1.2 | 0.6 |
| Dysrhythmia | 27.8% | 10.6% | 72.2% | 10.6% | 5.6 | 0.8 | 6.5 | 2.3 | 3.5 | 1.5 |
| Myocardial infarction/angina | 65.0% | 3.8% | 35.0% | 3.8% | 6.0 | 0.3 | 3.2 | 0.8 | 2.4 | 0.4 |
| Individuals visiting emergency department | ||||||||||
| Asthma | 2.6% | 0.6% | 8.5% | 1.1% | 0.6 | 0.1 | 12.9 | 0.5 | 1.2 | 0.1 |
| Chronic Obstructive Pulmonary Disease | 0.0% | 0.0% | 38.5% | 5.5% | 3.9 | 0.6 | 14.0 | 1.7 | 0.7 | 0.3 |
| Respiratory Infection | 1.5% | 0.5% | 12.1% | 1.3% | 0.9 | 0.1 | 14.3 | 0.5 | 1.5 | 0.1 |
| Congestive Heart Failure | 8.9% | 4.2% | 60.0% | 7.3% | 4.8 | 0.7 | 8.5 | 1.8 | 0.8 | 0.4 |
| Dysrhythmia | 9.6% | 4.1% | 25.0% | 6.0% | 1.9 | 0.5 | 5.3 | 1.0 | 1.7 | 0.6 |
| Myocardial infarction/angina | 61.8% | 3.8% | 33.3% | 3.7% | 5.8 | 0.3 | 3.1 | 0.8 | 2.3 | 0.4 |
Valuation estimates for cardiac and respiratory hospital admissions and emergency department visits were calculated as the weighted average among specific cardiac and respiratory conditions, with the weights based on the proportion of hospital admissions and emergency department visits accounted for by these conditions as reported in Burnett et al. [22] and Stieb et al. [33].
We obtained Monte Carlo estimates for each morbidity outcome by iteratively calculating its components (n = 1000), sampling from the observed distributions of model parameters, accounting for correlation among parameters, and from the observed distributions of input values. We report a central estimate which reflects model results evaluated at the mean of input values, and a 95% confidence interval bounded by the 2.5th and 97.5th percentiles of the output distribution. Where demographic information (age, education, income) and population health status were employed as independent variables in calculating stated-preference values, we conducted a sensitivity analysis by employing both the values of these variables in the original survey sample, as well as values based on the 1996 Canadian census and the 1996 National Population Health Survey [40]. While specific subgroups of those experiencing acute episodes of cardiorespiratory disease may be more specifically susceptible to air pollution as a trigger, and the severity of their disease episodes may differ from others, it is not possible to identify these groups with confidence. In order to deal with uncertainty generated by this issue, we also conducted a sensitivity analysis by varying the weight given to the least versus most severe levels of activity restriction and symptoms. When comparing our results with those from earlier studies, we converted values from other countries to the same year in Canadian dollars using purchasing power parity [41]. They were adjusted to 1997 Canadian dollars using the consumer price index for Canada for either all goods and services (WTP based estimates) or for health care (cost of treatment based estimates) [42]. While caution should be exercised in transferring our estimates to other countries, a similar procedure would be employed to do this, by applying the 1997 purchasing power parity between Canada and the target country, and adjusting to the currency year of interest using the country specific consumer price index for all goods and services.
Results
Cost of treatment model
Results from our analysis of cost of treatment data are presented in Table 4. The largest coefficients were associated with a diagnosis of congestive heart failure, and admission to critical care or non-critical care units. As reflected in the interaction terms, critical-care (CC) costs for respiratory infections (RI) and dysrhythmias (DYS) were considerably lower (RI*CC and DYS*CC), as were non critical-care (NCC) costs for asthma (AS*NCC). However, non critical-care costs were higher for those with a diagnosis of myocardial infarction/angina (MIA*NCC). Duration was associated with a coefficient of approximately $30 per day, but interaction terms essentially eliminated this effect for some diagnoses.
Table 4.
Parameter estimates for cost of treatment model
| Variable Name | Variable Description | Parameter Estimate ($) | Standard Error ($) |
| VCOT = α + βASAS + βCHFCHF + βDD + βCCCC + βNCCNCC + βAS*DAS*D + βRI*DRI*D + βMIA*DMIA*D + βRI*CCRI*CC + βDYS*CCDYS*CC | |||
| Intercept | Intercept term | 348.58 | 90.71 |
| AS | Dummy variable for diagnosis of asthma (0,1) | 440.33 | 125.97 |
| CHF | Dummy variable for diagnosis of congestive heart failure (0,1) | 1680.09 | 406.92 |
| D | Total duration of disease episode (days) | 31.70 | 7.85 |
| CC | Dummy variable for admission to hospital in critical care unit (0,1) | 4530.36 | 176.20 |
| NCC | Dummy variable for admission to hospital in non-critical care unit (0,1) | 1977.94 | 163.67 |
| AS*D | Interaction term (see variable definitions above) | -27.71 | 9.17 |
| RI*D | Interaction term where RI is a dummy variable for diagnosis of respiratory infection (0,1) | -29.02 | 8.07 |
| MIA*D | Interaction term where MIA is a dummy variable for diagnosis of myocardial infarction/angina (0,1) | -30.54 | 14.50 |
| RI*CC | Interaction term (see variable definitions above) | -1544.58 | 538.12 |
| DYS*CC | Interaction term where DYS is a dummy variable for diagnosis of dysrhythmia (0,1) | -2402.73 | 906.97 |
| AS*NCC | Interaction term (see variable definitions above) | -431.01 | 272.89 |
| MIA*NCC | Interaction term (see variable definitions above) | 1180.79 | 301.74 |
| CHF*NCC | Interaction term (see variable definitions above) | -2158.82 | 539.88 |
Comprehensive valuation estimates
Results of our calculations of overall valuation for each endpoint are presented in Table 5. Cost of treatment accounted for the majority of the overall value in the case of respiratory and cardiac hospital admissions, as well as cardiac emergency department visits. In the case of respiratory emergency department visits, cost of treatment accounted for approximately forty-five percent of the overall value. Lost productivity costs represented a small proportion of the overall value, although the proportion was greater for those endpoints which do not include a cost of treatment component. For both hospital admissions and emergency department visits, the overall value was larger for cardiac compared to respiratory conditions. This is primarily attributable to the larger cost of treatment for cardiac versus respiratory conditions. The ratio between total value and COI (i.e. cost of treatment plus lost productivity), ranged from 1.3 to 1.9 for those endpoints with a cost of treatment component, while the ratio tended to be larger for those endpoints without a cost of treatment component.
Table 5.
Valuation estimatesa and ratio of total value to cost of illness, by endpoint and component
| Endpoint | Cost of Treatment (CoT) | Lost Productivity (LP) | Pain, Suffering and Averting Expenditures | Total | Total Value/(CoT + LP) | ||
| In Hospital | Out of Hospital |
Point Estimate |
95% CI | ||||
| Respiratory Hospital Admission | $2,800 | $300 | $670 | $410 | $4,200 | ($3,400, $5,000) | 1.3 |
| Cardiac Hospital Admission | $3,800 | $270 | $760 | $340 | $5,200 | ($4,000, $6,400) | 1.3 |
| Respiratory Emergency Department Visit | $930 | $160 | $430 | $520 | $2,000 | ($1,700, $2,500) | 1.9 |
| Cardiac Emergency Department Visit | $3,200 | $210 | $680 | $330 | $4,400 | ($3,300, $5,600) | 1.3 |
| Restricted Activity Day | $25 | $23 | $48 | ($13, $82) | 1.9 | ||
| Asthma Symptom Day | $12 | $16 | $28 | ($11, $71) | 2.3 | ||
| Acute Respiratory Symptom Day | $12 | $1 | $13 | ($0, $28) | 1.1 | ||
aestimates rounded to two significant figures
Results were not sensitive to choice of input values for demographic and health status characteristics (original survey sample characteristics versus nationally representative values for Canada). Sensitivity to the weighting given to the levels of activity restriction differed among the endpoints. The total value of avoiding respiratory and cardiac hospital admissions and emergency department visits varied by less than 10% from base estimates when we varied the weighting given to least versus most restrictive health states based on empirical data as described earlier. Relative to the base values, the total value of avoiding restricted activity days and asthma symptom days was respectively 54 and 57% lower and 65 and 104% higher when weighting of the different health states was varied. In all of the sensitivity analyses for restricted activity days and asthma symptom days, point estimates fell within the 95% confidence intervals on the base case estimates. However, the 95% confidence interval on the valuation estimate for asthma symptom days with less severe activity restrictions overlapped 0. For acute respiratory symptom days, valuation estimates for less and greater activity restrictions were respectively $12 and $28, both of which were within the 95% confidence interval on the base case estimate. In all cases the 95% confidence interval overlapped 0.
Discussion
Our estimates of the value of avoiding a range of acute effects of air pollution on cardiorespiratory morbidity are generally consistent with expectation in terms of the magnitude of values relative to severity and duration. The higher valuation of avoiding cardiac compared to respiratory disease episodes is driven mainly by the much higher proportion of cardiac conditions requiring admission to hospital, critical care, and invasive procedures [29]. Valuation for emergency department visits for both types of conditions includes cost of treatment related to hospital admission for those patients who were ultimately admitted. Because cardiac patients were much more likely to be admitted, this is reflected in a much larger cost of treatment value for cardiac compared to respiratory emergency department visits. While this would result in double counting of benefits where both hospital admissions and emergency visits are assessed and monetized in a benefits analysis, this approach was considered appropriate because concentration-response relationships for air pollution and emergency department visits are based on all those who visit the emergency department, including those who are ultimately admitted to hospital. Where both types of outcomes are being considered in benefits analysis, double counting can be avoided by using concentration-response relationships for emergency department visits to capture both types of effects, either by using relationships taken directly from epidemiological studies of air pollution and emergency department visits, or scaling up concentration response relationships from studies of hospital admissions, based on the expected ratio between hospital admissions and emergency department visits [1]. (See illustrative example below.)
Comparison with existing estimates
We present a comparison of our estimates with those from earlier studies [1-7,43,44] in figures 1,2,3 and Table 6 (see additional file 1). We have categorized estimates from earlier studies based on the authors' description of the health state, and the primary sources cited. It is difficult to make precise comparisons, however, because many other studies do not specify the level of activity limitation associated with the condition being valued, and our estimates pertaining to emergency department visits differ from earlier estimates in that they also capture costs for those patients who were ultimately admitted.
Figure 1.
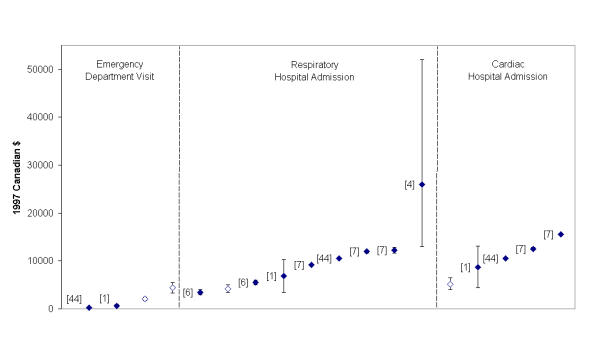
Comparison of valuation estimates for hospital admissions and emergency department visits with earlier studies. Legend: Labels denote reference number. Open symbols denote estimates from the present study. See Table 6 (additional file 1) for additional details on individual estimates.
Figure 2.
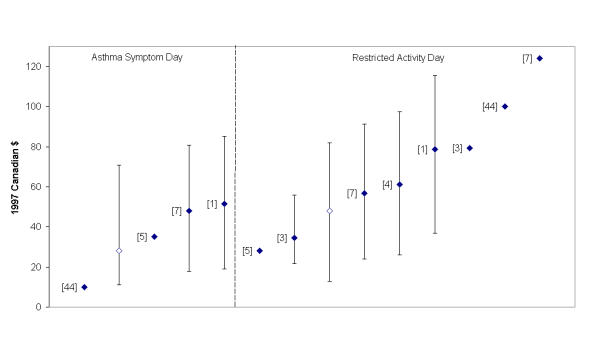
Comparison of valuation estimates for restricted activity days and asthma symptom days with earlier studies. Legend: Labels denote reference number. Open symbols denote estimates from the present study. See Table 6 (additional file 1) for additional details on individual estimates.
Figure 3.
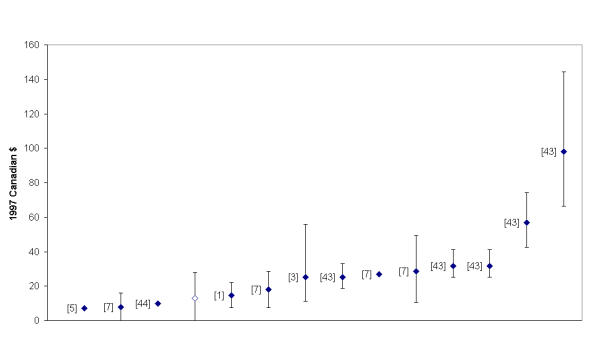
Comparison of valuation estimates for acute respiratory symptom days with earlier studies. Legend: Labels denote reference number. Open symbols denote estimates from the present study. See Table 6 (additional file 1) for additional details on individual estimates.
Nonetheless, in general, our estimates are comparable in magnitude to those from earlier studies in this area. A priori, we might have expected that our more comprehensive approach would have resulted in somewhat higher estimates compared to earlier studies. We observed that valuation estimates for the less severe outcomes were sensitive to specification of severity level, such that specifying a higher level of severity produced estimates at the higher end of those reported in earlier studies. It is also possible that in the context of the less severe outcomes which are associated with relatively low valuation, our approach, though more comprehensive, adds only small increments which do not result in a substantial change in magnitude of the overall estimate
Our estimates for hospital admissions are less than in most earlier studies. With respect to the cost of treatment component for this outcome, compared to the Anis et al. study [27], two studies based on U.S. data reported higher costs for pneumonia [45] and congestive heart failure [46], while another from Canada revealed similar costs for asthma hospital admissions [[47], personal communication, Dr. W. Ungar, November 2002]. Estimates from the U.K. were also similar to those derived here [6]. The estimates advanced by Chestnut et al. [1], though developed for Canada, are also based partially on U.S. data [48]. These findings may reflect true systematic differences in costs of treatment in the U.S. compared to Canada and the U.K.. It has been documented that intensity of care for some conditions is greater in the United States than Canada [49], and that administrative/overhead costs are significantly higher in the U.S. than in Canada in relation to the multiple versus single payer systems in the two countries [50,51]. Given that the ratios we observed for total value to COI were generally similar to (or indeed at the lower end of) those reported previously [1,4,15-17], this indicates that the component of valuation related to avoided pain and suffering and averting expenditures is also lower than earlier estimates. This may suggest that WTP to avoid health outcomes associated with significant health care costs may be lower in the context of a publicly funded universal health care system, possibly because of lower perceived risks of catastrophic financial consequences. Thus it appears that in the case of hospital admissions, the impact of our more comprehensive approach to valuation is overshadowed by lower costs of treatment in Canada compared to the U.S., which has been the predominant source of earlier such estimates.
Limitations of our approach
While we believe our results represent an advance over earlier estimates, there are several limitations which could be addressed in future work in this area. The model we employed for stated preference values was non-linear with respect to duration of the illness episode, implying diminishing marginal utility for reduced morbidity with respect to duration [28]. However, we assumed simple additivity of the individual blocks of time constituting each segment of activity restriction of varying severity in the context of an illness episode. This was necessitated by the finding in the context of the original stated preference survey, that presenting individuals with illness episode scenarios involving an evolution of level of activity restriction was overly burdensome for respondents. Our assumption of simple additivity is likely to lead to overestimates of total value relative to the observation in the original study of diminishing marginal utility with respect to duration [28]. The extent of bias requires further empirical evaluation. Additional development work would be needed to determine how best to communicate this information to respondents in a straightforward yet accurate way, and to elicit valuation information appropriately.
Our analysis relied on data from two studies carried out in single centres (Saint John and Toronto). While we found that our results were not sensitive to demographic and health status differences between the original stated preference survey sample and Canada as a whole, repeating the survey in multiple centres would nevertheless be desirable, as would collecting illness episode, cost of treatment, and stated preference information from the same sample of respondents.
Response rate is a potential concern for both the cost of illness study and the stated preference survey. Response rates to the emergency department follow-up survey were greater than 80% for individuals with asthma and respiratory infections, but only 50% and 67% for those with COPD and cardiac conditions respectively. Those with cardiac conditions who completed follow-up interviews were younger (and possibly healthier) than those who did not [29]. Cost of treatment estimates may therefore be conservative relative to a fully representative population of patients of all degrees of severity. Lower and upper bounds on the response rate for the stated preference survey were 22 and 63 percent, assuming that respectively all or none of the telephone numbers which could not be contacted or verified as households were included in the denominator [30]. Of prospective subjects who completed the screening telephone survey, 45 percent agreed to take the in-person survey, while 72 percent of those who scheduled an appointment actually completed the in-person survey [30]. Thus, a substantial portion of the sample did not complete the in-person survey. While a low response rate would raise concerns about the representativeness of the sample, no major differences were observed with respect to demographic characteristics or health status characteristics which were found to influence WTP in this study.
An additional potential limitation of our results is the possibility of double counting of out of pocket expenditures, which could potentially have been captured by both the cost of treatment study and the stated preference willingness to pay study. Ungar et al. [47] found that out of pocket expenses accounted for only 1 per cent of annual per patient treatment costs for asthma, which suggests that this is probably not an important issue.
An illustrative example
We illustrate the application of our approach by examining the benefits associated with reduced cardiorespiratory emergency department visits and hospital admissions attributable to the decline in particulate sulfate concentrations observed in Toronto from the mid 1980s to the late 1990s. Average particulate sulfate concentrations in the Toronto Census Metropolitan Area (CMA) declined from 5.0 μg/m3 (1984–1986 average) to 3.8 μg/m3 (1997–1999 average) during this period. We estimated the benefits in 2000 when the estimated population was 4.771 million, using results from an epidemiological study examining the association of air pollution with hospital admissions for respiratory and cardiac disease in southern Ontario [22]. We used this study rather than more recent work because of recently identified problems with the statistical analysis software which has become the standard over the past 5 to 6 years in the analysis of time-series data [52], the full impact of which is still being evaluated. The rates of admission reported in the study translate into 25,000 cardiac and 28,000 respiratory hospital admissions in the Toronto CMA in 2000. Applying the proportion of cardiac and respiratory emergency department visits resulting in admission to hospital from the Saint John study (76% and 20%), [29,33] the numbers of hospital admissions correspond to 33,000 cardiac and 140,000 respiratory emergency department visits in 2000. Based on this study, we estimated that a 1.2 μg/m3 decrease in sulfate concentration would respectively result in a 0.30 % decrease in cardiac hospital admissions/emergency department visits (95% CI 0.16–0.45) and a 0.32% decrease in respiratory hospital admissions/emergency department visits (95% CI 0.21–0.43), accounting for the simultaneous effects of ozone and temperature. The proportional reduction is the same for admissions and emergency visits because in this example the concentration response function is simply scaled based on the relative frequency of the two types of outcome.
We estimated the benefits of the observed changes in sulfate concentration, specifying both the concentration response relationship and the valuation estimates generated above as normal distributions based on the point estimate and standard error, using a Monte Carlo simulation with 1,000 iterations implemented using Analytica software [53]. It was estimated that the benefits of reduced emergency department visits for respiratory and cardiac disease were respectively $910,000 and $440,000, while the benefits of reduced respiratory and cardiac hospital admissions were $380,000 and $390,000. However, because essentially all non-elective hospital admissions occur through the emergency department, and the valuation estimates generated above for emergency department visits reflect the probability and valuation of subsequent admission to hospital, the total benefits are simply the sum of those related to emergency department visits or $1.4 million (95% CI 0.91–1.8 million). We emphasize that this estimate does not reflect the much larger benefits attributable to reduced mortality and chronic morbidity.
Conclusions
We believe our overall approach addresses a number of the limitations of the current literature and is widely applicable to future assessments of the benefits of improved air quality. However, because we have noted potentially significant differences between the U.S. and Canada in valuation of certain outcomes, the revised morbidity valuation estimates presented here are most suitable for use in assessing the benefits of air pollution mitigation initiatives in Canada. We recommend employing sensitivity analyses with respect to severity of activity limitation, for those health outcomes where we observed significant sensitivity to this factor.
Abbreviations
COI – cost of illness
COPD – chronic obstructive pulmonary disease
COT – cost of treatment
LP – lost productivity
WTP – willingness to pay
WTA – willingness to accept compensation
Competing interests
None declared.
Authors' Contributions
All authors contributed to drafting of the manuscript and approved the final version. DMS conceived of the study design and contributed to the statistical analysis. PD conceived of the study design. FRJ participated in study design and supervised the statistical analysis. MPM programmed the statistical analysis. AHA participated in study design and the statistical analysis. RCB participated in study design. SJ contributed to the statistical analysis.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/content/backmatter/1476-069X-1-7-b1.pdf
Supplementary Material
See additional file 1, an Adobe Acrobat file, which contains a tabular summary of the properties of valuation estimates utilized in recent benefits assessment studies, as shown graphically in figures 1 to 3.
Acknowledgments
Acknowledgments
The authors are grateful to Curt Rabon for programming assistance and to Tom Dann of Environment Canada for providing historical air quality data. Funding was provided by Health Canada.
Contributor Information
David M Stieb, Email: dave_stieb@hc-sc.gc.ca.
Paul De Civita, Email: paul_decivita@hc-sc.gc.ca.
F Reed Johnson, Email: frjohnson@rti.org.
Matthew P Manary, Email: matthewmanary@yahoo.com.
Aslam H Anis, Email: anis@hivnet.ubc.ca.
Robert C Beveridge, Email: drbob_beveridge@bigfoot.com.
Stan Judek, Email: stan_judek@hc-sc.gc.ca.
References
- Health and Environmental Impact Assessment Panel Report on Sulphur in Gasoline and Diesel Fuels. Ottawa, Canada, Joint Industry/Government Study. 1997.
- Desvousges WH, Johnson FR, Banzhaf HS, Russell RR, Fries EE, Dietz KJ, Helms SC, Keen D, Snyder J, Valentine H, et al. Assessing environmental externality costs for electricity generation. Durham, NC, Triangle Economic Research. 1995.
- Hall JV, Winer WM, Kleinman MT, Lurmann FW, Brajer V, Colome SD. Valuing the Health Benefits of Clean Air. Science. 1992;255:812–817. doi: 10.1126/science.1536006. [DOI] [PubMed] [Google Scholar]
- Levy JI, Carrothers TJ, Tuomisto JT, Hammitt JK, Evans JS. Assessing the public health benefits of reduced ozone concentrations. Environ Health Perspect. 2001;109:1215–26. doi: 10.1289/ehp.011091215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupnick AJ, Portney PR. Controlling Urban Air Pollution: A Benefit-Cost Assessment. Science. 1991;252:522–528. doi: 10.1126/science.1902322. [DOI] [PubMed] [Google Scholar]
- United Kingdom Department of Health, Adhoc Group on the Economic Appraisal of the Health Effects of Air Pollutants. http://www.doh.gov.uk/hef/airpol/eareport.htm#details 19 April 2000.
- United States Environmental Protection Agency The Benefits and Costs of the Clean Air Act, 1970 to 1990. EPA 410-R-97-002 Washington, DC. 1997.
- Freeman AM., III The Measurement of Environmental and Resource Values: Theory and Methods. Washington, DC, Resources for the Future. 1993.
- Bergstrom JC, De Civita P. Status of Benefits Transfer in the United States and Canada: A Review. Can J Agric Econ. 1989;47:79–87. [Google Scholar]
- European Centre for Environment and Health Quantification of the Health Effects of Exposure to Air Pollution. Bitlhoven, the Netherlands, World Health Organization. 2000.
- Dickie M, Gerking S, Brookshire D, Coursey D, Schulze W, Coulson A, Tashkin D. Reconciling averting behavior and contingent valuation benefit estimates of reducing symptoms of ozone exposure. Improving accuracy and reducing costs of environmental benefit assessment. Washington, DC: U.S. Environmental Protection Agency. 1987.
- Loehman ET, Berg SV, Arroyo AA, Hedinger RA, Schwartz JM, Shaw ME, Fahien RW, De VH, Fishe RP, Rio DE, et al. Distributional analysis of regional benefits and cost of air quality control. J Environ Econ Manage. 1979;6:222–243. [Google Scholar]
- Tolley G, Babcock L, Berger M, Bilotti A, Blomquist G, Brien M, Fabian R, Fishelson G, Kahn C, Kelly A, et al. Valuation of reductions in human health symptoms and risk. Contingent valuation study of light symptoms and angina, Final report prepared for U.S. Environmental Protection Agency. Washington, DC. 1986;3 [Google Scholar]
- Kenkel D. Cost of Illness Approach. In: Tolley G, Kenkel D, Fabian R, editor. Valuing Health for Policy: An Economic Approach. Chicago, IL, University of Chicago Press; 1994. pp. 42–71. [Google Scholar]
- Chestnut LG, Colome SD, Keller LR, Lambert WE, Ostro B, Rowe RD, Wojciechowski SL. Heart Disease Patients' Averting Behavior, Costs of Illness and Willingness to Pay to Avoid Angina Episodes. EPA-230-10-88-042 Washington, U S Environmental Protection Agency. 1988.
- Chestnut LG, Keller LR, Lambert WE, Rowe RD. Measuring Heart Patients' Willingness to Pay for Changes in Angina Symptoms. Med Decis Making. 1996;16:65–77. doi: 10.1177/0272989X9601600115. [DOI] [PubMed] [Google Scholar]
- Rowe RD, Chestnut LG. Oxidants and Asthmatics in Los Angeles: A Benefits Analysis. Boulder, CO, Energy and Resource Consultants. 1986.
- Canadian Environmental Protection Act Federal – Provincial Advisory Committee Working Group on Air Quality Objectives and Guidelines National Ambient Air Quality Objectives for Ground-Level Ozone, Science Assessment Document. Ottawa, Canada, Health Canada and Environment Canada. 1999.
- Canadian Environmental Protection Act Federal – Provincial Advisory Committee Working Group on Air Quality Objectives and Guidelines National Ambient Air Quality Objectives for Particulate Matter, Science Assessment Document. Ottawa, Canada, Health Canada and Environment Canada. 1999.
- United States Environmental Protection Agency Office of Research and Development Air Quality Criteria for Particulate Matter. Washington, DC. 1996.
- World Health Organization Guidelines for Air Quality. Geneva, Switzerland. 1999.
- Burnett RT, Dales R, Krewski D, Vincent R, Dann T, Brook JR. Associations between Ambient Particulate Sulfate and Admissions to Ontario Hospitals for Cardiac and Respiratory Diseases. Am J Epidemiol. 1995;142:15–22. doi: 10.1093/oxfordjournals.aje.a117540. [DOI] [PubMed] [Google Scholar]
- Mitchell RC, Carson RT. Using Surveys to Value Public Goods: The Contingent Valuation Method. Washington, DC, Resources for the Future. 1989.
- Gold MR, Stephenson D, Fryback DG. HALYs and QALYs and DALYs, My Oh: Similarities and Differences in Summary Measures of Population Health. Annu Rev Public Health. 2002;23:115–134. doi: 10.1146/annurev.publhealth.23.100901.140513. [DOI] [PubMed] [Google Scholar]
- de Hollander AEM, Melse JM, Lebret E, Kramers PGN. An Aggregate Public Health Indicator to Represent the Impact of Multiple Environmental Exposures. Epidemiol. 1999;10:606–617. [PubMed] [Google Scholar]
- Brouwer WBF, Koopmanschap MA, Rutten FFH. Productivity Costs Measurement through Quality of Life? A Response to the Recommendation of the Washington Panel. Health Econ. 1997;6:253–259. doi: 10.1002/(SICI)1099-1050(199705)6:3<253::AID-HEC266>3.3.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- Anis AH, Guh D, Stieb D, Leon H, Beveridge RC, Burnett RT, Dales RE. The Costs of Cardiorespiratory Disease Episodes in a Study of Emergency Department Use. Can J Public Health. 2000;91:103–106. doi: 10.1007/BF03404920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson FR, Ruby Banzhaf M, Desvousges WH. Willingness to pay for improved respiratory and cardiovascular health: a multiple-format stated-preference approach. Health Econ. 2000;9:295–317. doi: 10.1002/1099-1050(200006)9:4<295::AID-HEC520>3.3.CO;2-4. [DOI] [PubMed] [Google Scholar]
- Stieb DM, Beveridge RC, Smith-Doiron M, Burnett RT, Judek S, Dales RE, Anis AH. Beyond Administrative Data: Characterizing Cardiorespiratory Disease Episodes Among Patients Visiting the Emergency Department. Can J Public Health. 2000;91:107–112. doi: 10.1007/BF03404921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson FR, Ruby MC, Desvousges WH, King JR. Using Stated Preferences and Health-State Classifications to Estimate the Value of Health Effects of Air Pollution. Durham, NC, Triangle Economic Research. 1998.
- Kaplan RM, Bush JW. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1:61–80. doi: 10.1037//0278-6133.1.1.61. [DOI] [Google Scholar]
- Fanshel S, Bush JW. A health-status index and its application to health-services outcome. Oper Res. 1970;18:1021–1066. [Google Scholar]
- Stieb DM, Beveridge RC, Brook JR, Smith-Doiron M, Burnett RT, Dales RE, Beaulieu S, Judek S, Mamedov A. Air pollution, aeroallergens and cardiorespiratory emergency department visits in Saint John, Canada. J Expo Anal Environ Epidemiol. 2000;10:461–477. doi: 10.1038/sj.jea.7500112. [DOI] [PubMed] [Google Scholar]
- Hastie T, Tibshirani R. Generalized Additive Models. London, UK Chapman and Hall. 1990.
- Canadian Socioeconomic Information Management system Matrix 4468. Statistics Canada, Labour Division. Average Weekly Earnings (Incl.Overtime), of All Employees, Firms of All Sizes, by Industry, 1980 SIC, Annual Averages, Canada. Ottawa, Canada.
- Canadian Coordinating Office for Health Technology Assessment . Ottawa, Canada. 2. 1997. Guidelines for economic evaluation of pharmaceuticals: Canada. [DOI] [PubMed] [Google Scholar]
- Stieb DM, Smith-Doiron M, Brook JR, Burnett RT, Dann T, Mamedov A, Chen Y. Air Pollution and Disability Days in Toronto: Results from the National Population Health Survey. Environ Res. 2002;89:210–219. doi: 10.1006/enrs.2002.4373. [DOI] [PubMed] [Google Scholar]
- Rozan A. Air pollution: a valuation of morbidity. Pollution Atmosphérique. 2001. pp. 105–119.
- Collins JG, LeClere FB. Health and selected socioeconomic characteristics of the family: United States, 1988–90. Vital Health Stat. 1996;10:1–94. [PubMed] [Google Scholar]
- Tambay J-L, Catlin G. Sample Design of the National Population Health Survey. Health Rep. 1995;7:29–38. [PubMed] [Google Scholar]
- Organization for Economic Cooperation and Development. Main Economic Indicators: Purchasing Power Parities. http://www.oecd.org/std/nadata.htm accessed 1 May 2001.
- Canadian Socioeconomic Information Management system Matrix 9957. Statistics Canada, Prices Division. Consumer Price Indexes for Canada, Annual, 1996 Classification. Ottawa, Canada.
- Johnson FR, Fries EE, Banzhaf HS. Valuing Morbidity: An Integration of the Willingness-to-Pay and Health-Status Index Literatures. J Health Econ. 1997;16:641–665. doi: 10.1016/S0167-6296(97)00012-X. [DOI] [PubMed] [Google Scholar]
- Holland M, Berry J, Forster D. Externalities of Energy: Methodology 1998 Update Brussels, Belgium, European Commission. 1999.
- Lave JR, Fine MJ, Sankey SS, Hanusa BH, Weissfeld LA, Kapoor WN. Hospitalized Pneumonia: Outcomes, Treatment Patterns, and Costs in Urban and Rural Areas. J Gen Intern Med. 1996;11:415–421. doi: 10.1007/BF02600189. [DOI] [PubMed] [Google Scholar]
- Funk M, Krumholz HM. Epidemiologic and economic impact of advanced heart failure. J Cardiovasc Nurs. 1996;10:1–10. doi: 10.1097/00005082-199601000-00002. [DOI] [PubMed] [Google Scholar]
- Ungar WJ, Coyte PC, Chapman KR, MacKeigan L. The patient level cost of asthma in adults in south central Ontario. Can Respir J. 1998;5:463–471. doi: 10.1155/1998/362797. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information Resource Intensity Weights: Summary of Methodology 1994/5. Toronto, Canada. 1995.
- Mark DB, Naylor CD, Hlatky MA, Califf RM, Tool EJ, Granger CB, Knight JD, Nelson CL, Lee KL, Clapp-Channing NE, et al. Use of medical resources and quality of life after acute myocardial infarction in Canada and the United States. N Engl J Med. 1994;331:1130–1135. doi: 10.1056/NEJM199410273311706. [DOI] [PubMed] [Google Scholar]
- Woolhandler S, Himmelstein DU. The deteriorating administrative efficiency of the U.S. health care system. N Engl J Med. 1991;324:1253–1258. doi: 10.1056/NEJM199105023241805. [DOI] [PubMed] [Google Scholar]
- Woolhandler S, Himmelstein DU. Costs of care and administration at for-profit and other hospitals in the United States. N Engl J Med. 1997;336:769–774. doi: 10.1056/NEJM199703133361106. [DOI] [PubMed] [Google Scholar]
- Health Effects Institute letter regarding generalized additive models: http://www.healtheffects.org/Pubs/NMMAPSletter.pdf 10 June 2002.
- Analytica A Software Tool for Uncertainty Analysis and Model Communication: http://www.lumina.com/software/ch10.9.PDF 28 June 2002.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
See additional file 1, an Adobe Acrobat file, which contains a tabular summary of the properties of valuation estimates utilized in recent benefits assessment studies, as shown graphically in figures 1 to 3.


